Abstract
Objective:
A retrospective study was designed to evaluate the results of surgical treatment and follow-up data in thyroid cancer patients less than 15 years old at the time of surgery.
Summary Background Data:
Pediatric thyroid carcinomas have a high rate of lymph nodal and distant metastases. Risk factors for recurrences and postoperative morbidity have not been assessed yet in a representative series.
Methods:
The group included 740 pediatric patients with thyroid cancer. Total thyroidectomy was performed in 426 (57.6%), lobectomy in 248 (33.5%), subtotal thyroidectomy in 58 (7.8%) cases, and 8 patients (1.1%) underwent partial lobectomy.
Results:
The mean follow-up period was 115.8 months (range, 1.5–236.4 months). Recurrence was diagnosed in 204 cases (27.6%), including 73 local relapses (9.9%), 90 distant metastases (12.2%), and a combination of local and distant recurrences in 41 (5.5%) patients. Multivariate statistical assessment revealed the following independent parameters significantly associated with the risk of recurrent nodal disease: a young age at diagnosis, multifocal carcinomas, N1 status, and lack of neck lymph node dissection. For lung metastases, the significant risk factors were female gender, young age at diagnosis, and presence of symptoms. The observed 5- and 10-year survival for the entire group was 99.5% and 98.8%, respectively. Postoperative hypoparathyroidism was significantly associated with multifocal tumors, central compartment removal, and ipsilateral dissection.
Conclusions:
Total thyroidectomy followed by radioiodine therapy is an optimal treatment strategy that makes it possible to achieve a cure in a vast majority of pediatric patients with differentiated thyroid carcinomas. Risk of recurrence is strongly associated with tumor stage, extent of surgery, the young patient's age, and presence of symptoms at diagnosis.
A retrospective analysis of the results of surgical treatment of 740 cases of childhood thyroid cancer was carried out with the purpose of identifying risk factors for recurrence and postoperative morbidity. The data obtained confirm favorable prognosis for survival and support total thyroidectomy with appropriate neck lymph node dissection followed by radioiodine therapy as an optimal treatment strategy.
Childhood thyroid malignancies are very uncommon with diagnostic rate ranging from 0.2 to 2.2 per 1 million children.1 Only a few institutions worldwide have reported a series comprising more than 100 patients.2–5 The accident at the Chernobyl nuclear power station in April 1986 resulted in a dramatic increase in thyroid cancer incidence, especially in young residents of the contaminated territories in Belarus, Ukraine, and Russia, which led to a uniquely rapid accumulation of experience in the treatment of this otherwise rare human malignancy. According to published observations, post-Chernobyl pediatric thyroid cancer is almost exclusively presented by papillary carcinomas with frequent lymph node involvement at diagnosis and a high incidence of recurrence after treatment.4,5 At the same time, apart from its peculiar etiology and pathogenesis, there is no evidence of pediatric post-Chernobyl thyroid cancer being principally different from sporadic thyroid cancer in terms of clinical manifestations;6 therefore, the data obtained in our series may be projected on any childhood thyroid cancer study.
Thyroid cancer in children usually has a favorable prognosis. The stepwise combination of surgery and radioiodine therapy is curative with an overall survival rate ranging from 86% to 100%.6 Although treatment results are good on the whole, there still remain controversies concerning treatment strategy, and surgical options in particular. Hitherto the opinion existed that thyroid-preserving procedures were preferable while total thyroidectomy could be recommended only for advanced disease.7–11 An opposite standpoint advocated total or near-total thyroidectomy with central neck lymph node dissection as a procedure of choice with appropriate lateral dissections depending on the nodal status.12–19 The indications for preventive removal of jugular-carotid chain lymph nodes have not been clearly formulated, although some reports have demonstrated high incidence of neck lymph node metastases not detectable by palpation.20,21
The purpose of this study is to evaluate the results of surgical treatment and follow-up data in the group of thyroid cancer patients younger than 15 years of age at the time of diagnosis. Based on our data on more than 700 post-Chernobyl thyroid cancer cases, the largest series in the world to our knowledge, we have assessed recurrence risk, postoperative morbidity, and survival rate to the effect of establishing a rationale for treatment strategy in childhood patients.
MATERIALS AND METHODS
During 1985 to 2003, 740 children (279 male and 461 female patients; sex ratio, 1:1.6) were treated for thyroid cancer and followed up in the Thyroid Cancer Center (Minsk, Belarus). The mean age of patients was 11.7 years (range, 4.2–14.9 years) with the majority of cases (76.1%) belonging to the 10- to 15-year-old age group. Only 8 children (1.1%) were younger than 5 years at the time of surgery. Nine patients with papillary cancer had a family history of thyroid malignancies and 2 cases of MEN2A and MEN2B syndrome were registered in female patients with medullary carcinoma. Prior to the diagnosis of a thyroid tumor, 2 children had undergone chemotherapy and radiotherapy for Hodgkin disease; 1 patient had been treated for non-Hodgkin lymphoma and 1 for acute lymphoblastic leukemia. Exposure to radionuclides at the time of Chernobyl disaster was proved in 681 cases (92.0%). In 10 patients (1.4%), no history of radioactive exposure was available and 49 (6.6%) children were recognized as sporadic nonmedullary thyroid cancer cases.
Papillary, follicular, and medullary carcinomas were diagnosed in 702 (94.9%), 35 (4.7%), and 3 (0.4%) cases, respectively. Tumor size varied from 2 mm to 60 mm (15 mm, mean). In 273 patients (36.9%), primary lesions were ≤10 mm in the largest dimension. Nine children had tumors exceeding 40 mm in diameter.
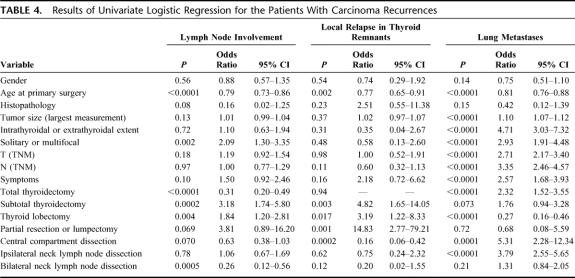
A total of 738 tumor cases were staged according to the TNM Classification of Malignant Tumours, 6th edition22 (in 2 of 22 patients having undergone primary thyroid-preserving surgery in hospitals other than the Thyroid Cancer Center, the information was not available). As shown in Table 1, the majority of carcinomas were pT1; lymph node involvement was proved in 513 cases (69.3%); tumors extending to tracheal wall, larynx, esophagus, or recurrent laryngeal nerve (pT4) occurred in 3 patients (0.4%). Pulmonary foci were detected by routine x-ray only in 17 cases (2.3%) before the surgical treatment. Most of the tumors were confined to the thyroid. Postoperative pathologic investigation revealed extrathyroidal invasion in 121 (16.3%) cases and multifocal lesions in 146 (19.7%) cases.
TABLE 1. pTNM Distribution in 738 Children
Primary surgical procedures were performed in 718 (97.0%) children. Twenty-two patients (3.0%) underwent completion thyroid surgery for proven relapse or suspicion of recurrence after the initial treatment.
Choice of the primary surgical procedure depended on tumor size and its extent. In the early 1990s, surgeons preferred thyroid lobectomy or subtotal thyroidectomy. Neck lymph node dissection was performed only in cases when preoperative ultrasound neck examination and biopsy revealed lymph node involvement. Since 1998, the strategy has switched to a more aggressive approach. Total thyroidectomy and neck lymph node dissection became more frequent, whereas conservative surgery was done only in cases of very small solitary intrathyroidal nodules with no evidence of metastases.
In our group of patients, total thyroidectomy was performed in 426 (57.6%) cases, lobectomy in 248 (33.5%), and subtotal thyroidectomy in 58 (7.8%) cases. Eight (1.1%) patients underwent partial lobectomy or lumpectomy. Classic radical neck lymph node dissection was performed in 10 (1.4%) children with multiple neck metastases invading the internal jugular vein. The most common surgical procedure for lymph node removal included modified or selective lateral dissection, performed bilaterally in 164 (22.2%) patients. All in all, neck lymph node dissection was performed in 607 (82.0%) of cases.
During the period from 1986 to 1992, adjuvant external beam therapy in a total dose of 30 to 40 Gy was administered to 28 (3.8%) patients with advanced disease. Since February 1993, this therapy was administered only to 2 children with medullary carcinomas.
Radioiodine treatment was used for ablation of thyroid remnants and/or lung metastases in 464 (62.7%) patients, including 193 children who were receiving this therapy in the Clinics for Nuclear Medicine in Essen and Würzburg, Germany. 131I administration was performed in patients with papillary or follicular carcinomas after total or subtotal thyroidectomy and induced postoperative hypothyroidism with serum TSH levels exceeding 30 mU/L. The dose of 50 and 100 MBq/kg of body weight of 131I was administered with the purpose of ablation of the thyroid tissue remnants and recurrences, respectively. On the fifth or the sixth day after radioiodine administration, a whole body scan was performed for staging. All patients were maintained on l-thyroxine suppressive therapy with the mean dose of 2.5 μg/kg of body weight starting 2 days after the onset of radioiodine therapy.
The follow-up protocol included clinical examination, neck ultrasonography, chest x-ray, and measurement of blood cell count and serum levels of thyroglobulin, calcium, phosphate, and free T3 and T4 every 3 months during the first year after surgery and once in 6 months from the second year on.
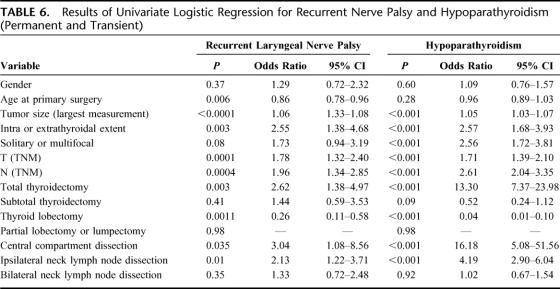
For the evaluation of prognostic variables, 23 clinical parameters were selected for the univariate and multivariate analyses (Table 2). The rates of recurrence and patients’ survival were estimated using the Kaplan-Meier method.
TABLE 2. Variables Selected for Univariate and Multivariate Analysis
Multivariate analyses included the logistic stepwise regression method (SAS/STAT software package; SAS Institute, Inc., Cary, NC).23 A P value not exceeding 0.05 was considered statistically significant.
RESULTS
Follow-up, Patterns of Failure, and Survival
The mean follow-up period was 115.8 months (range, 1.5–236.4 months); most of the patients (91.1%) were followed up for more than 5 years, and 362 children (48.9%) from among the patients defined the 10-year survival period.
Recurrence was diagnosed in 204 cases (27.6%), including 73 local relapses (9.9%), 90 distant metastases (12.2%), and a combination of local and distant metastases in 41 patients (5.5%) (Table 3). Neck lymph node metastases were a common type of relapse diagnosed solely or in combination with other recurrences in 105 (14.2%) patients. Lymphatic dissemination, mostly ipsilateral, was registered in 72 patients; contralateral or bilateral metastases were detected in 21 and 12 children, respectively. The mean disease-free interval for lymph node involvement was 27.2 months (SE 3.1 months; 95% confidence interval, 21.2–33.2). A total of 43 of 105 (40.9%) cases of relapse metastases were diagnosed during the first year after primary surgery. In 11 patients, positive lymph nodes appeared after more than 5 years after primary treatment.
TABLE 3. Sites of Carcinoma Recurrence
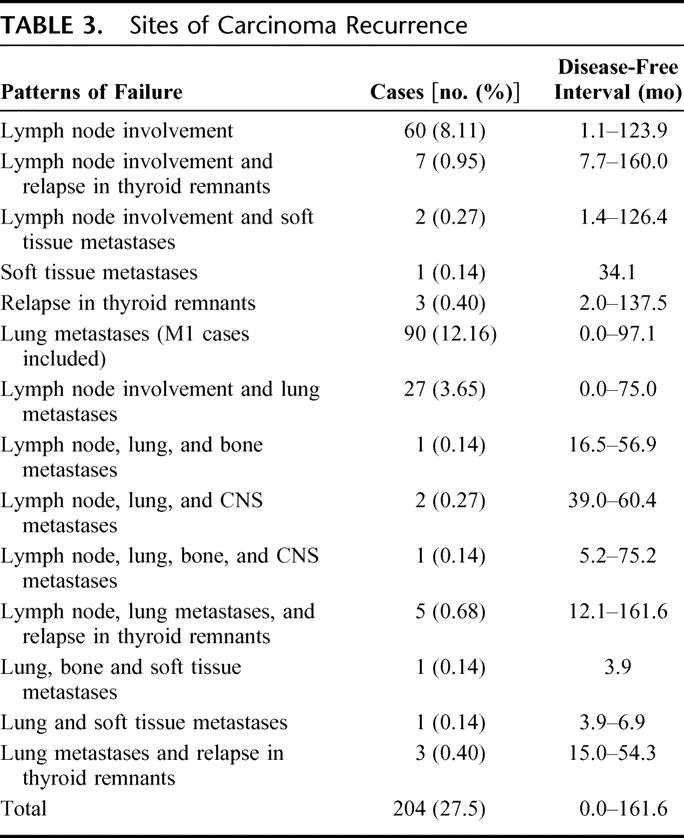
Relapses in thyroid remnants were detected in 18 cases (2.4%). This type of recurrence may also occur shortly or a long time after primary surgery. In 2 patients, relapses in thyroid remnants were detected in the 12th and in 1 case in the 15th year of follow-up.
The lungs were the main site of metastases diagnosed in 131 (17.7%) cases. Other sites of distant spread (such as the bones and central nervous system) in children were uncommon and, once occurred, were strongly associated with the presence of pulmonary lesions. The mean pulmonary metastases-free interval was 19.9 months (SE 2.2 months; 95% confidence interval, 15.6–24.1). In 76 patients, metastatic foci were detected during the first year of follow-up on the first post-therapeutic radioiodine scan. In contrast, in 3 children, lung metastases were diagnosed more than 5 years after surgery.
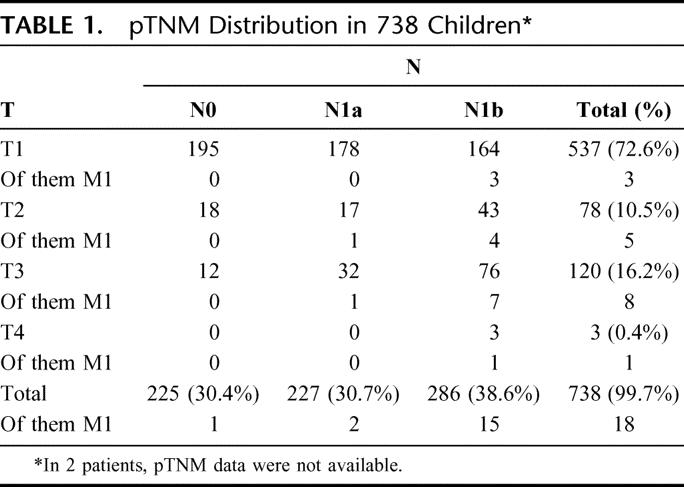
Univariate analysis (Table 4) has proved the following parameters to be significantly associated with lymphatic spread of thyroid carcinomas: young age at diagnosis, multifocality, subtotal thyroidectomy, and thyroid lobectomy. On the other hand, total thyroidectomy and bilateral neck lymph node dissection conferred a lower risk of subsequent lymph node involvement. For recurrences in thyroid remnants, the reliable risk factors were subtotal thyroidectomy, thyroid lobectomy, or lesser resection. It is interesting to note that none of the parameters except age and tumor size was significantly associated with the risk of this type of failure. Risk of lung metastases was extremely significantly associated with the young age at diagnosis, extrathyroidal extent, multifocality, advanced T- and N-status, presence of symptoms, and extended surgical procedures. The latter interdependence should be interpreted in the way that advanced tumors usually require aggressive surgery.
TABLE 4. Results of Univariate Logistic Regression for the Patients With Carcinoma Recurrences
Multivariate logistic regression (Table 5) revealed the following parameters significantly associated with the risk of recurrent nodal disease: young age at diagnosis, multifocal carcinomas, N1 status, and lack of ipsilateral or bilateral neck lymph node dissection. None of these factors was significantly associated with the risk of recurrence in thyroid remnants. Perhaps the frequency of the latter events was relatively small for the declared set of independent variables.
TABLE 5. Results of Multivariate Logistic Regression Analysis in the Patients With Recurrent Nodal Disease and Lung Metastases
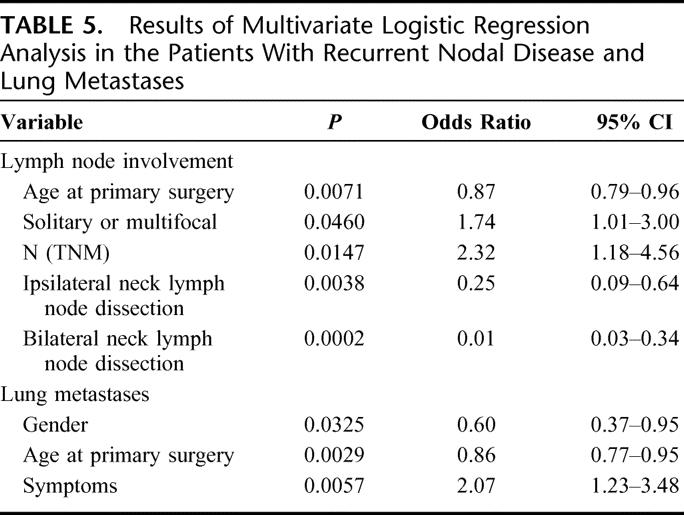
For lung metastases, significant risk factors were female gender, a young age at diagnosis, and presence of clinical symptoms.
The observed 5- and 10-year survival rate for the entire group was 99.5% and 98.8%, respectively. There was no 30-day operative mortality. Eight (1.1%) patients died during the study period. In 3 cases, the cause of death was other than thyroid cancer. The remaining 5 patients died of distant metastases, including all 3 patients with medullary carcinoma and 1 with advanced (M1) follicular carcinoma. Only 1 girl with multiple lung metastases of papillary carcinoma died of this type of cancer. The cause-specific 5- and 10-year survival rate was 99.7 and 99.2%, respectively.
Results of Radioiodine Therapy
Of the total number of 464 patients treated with 131I, 336 children (72.4%) underwent ablation of thyroid remnants and 128 (27.6%) received radioiodine therapy for distant metastases. The complete response (no evidence of 131I accumulation on the whole body scan and thyroglobulin levels <1 ng/L) was achieved in 271 (58.4%) of cases. In 159 (34.3%) cases, stable partial response (no evidence of 131I uptake on the whole body scan and thyroglobulin levels between 1 and 10 ng/L) was observed, and 34 (7.3%) patients were recognized as nonresponders with 131I still in visible accumulation and increased serum thyroglobulin levels.
Of the 128 cases with lung metastases, complete, stable partial, and partial response was registered in 37 (28.9%), 61 (47.7%), and 30 patients (23.4%), respectively. Children with incomplete remission are still maintained on radioiodine therapy.
Surgical Complications
A total of 242 complications specific to thyroid surgery were registered in 214 patients. In the entire group of cases, permanent recurrent laryngeal nerve palsy occurred in 46 children (6.2%), including 38 unilateral (5.1%) and 8 bilateral injuries (1.1%). Thirteen patients (1.8%) developed transient recurrent laryngeal nerve palsy. It is noteworthy that 6 children with an advanced disease had hoarseness at diagnosis and in 4 patients recurrent laryngeal nerve was encased by the tumor. Obviously, avoiding surgical morbidity in such cases was not possible. On the other hand, several patients developed vocal cord palsy after an apparently accurate nerve separation. Tracheostomy was performed in 4 patients with bilateral nerve injuries. Subsequently, in all these cases, tracheal wall reconstruction was performed by means of plastic surgery within 1 year after primary surgery.
Permanent hypoparathyroidism was the most frequent complication detected in 91 patients (12.3%). Eighty (10.8%) children developed transient hypocalcaemia. In our opinion, difficulties of parathyroid gland identification accounted for hypoparathyroidism in cases of advanced tumor, in those with lymph node metastases in particular. In such patients, distinguishing between a positive lymph node and glandular tissue is often impossible. In children with central compartment metastases, surgeons frequently sacrifice the lower parathyroid glands to ensure complete malignancy removal.
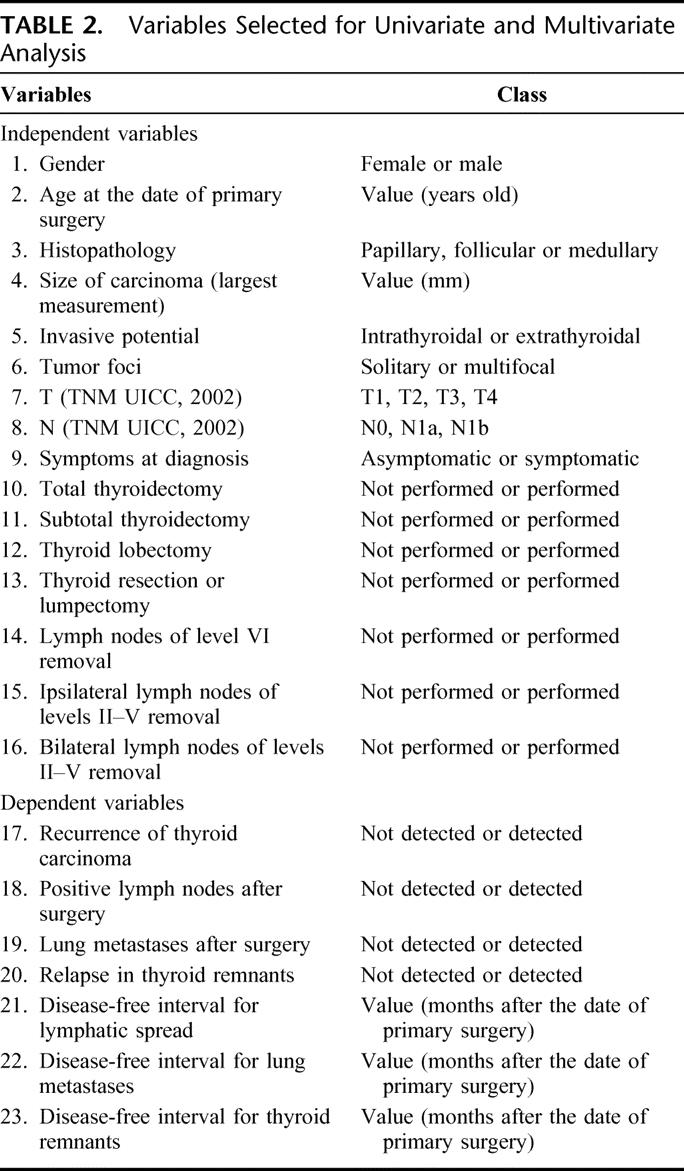
According to the univariate analysis data, the following factors were associated with high risk of recurrent nerve palsy (Table 6): extrathyroidal tumor, large tumor size, T3–T4, N1, total thyroidectomy, central compartment dissection, and ipsilateral nodal removal. Favorable results correlated with older age and thyroid lobectomy.
TABLE 6. Results of Univariate Logistic Regression for Recurrent Nerve Palsy and Hypoparathyroidism (Permanent and Transient)
Risk of permanent hypoparathyroidism and transient hypocalcemia was associated with large tumor size, extrathyroidal invasion, multifocality, T3–T4, N1, total thyroidectomy, central compartment dissection, and ipsilateral nodal removal. Thyroid lobectomy significantly correlated with a lower incidence of hypoparathyroidism.
Multivariate logistic regression did not reveal statistically significant risk factors for the recurrent laryngeal nerve palsy. On the contrary, postoperative hypoparathyroidism was strongly associated with multifocal tumors, central compartment removal, and ipsilateral dissection.
Besides these 2 major surgical complications, other types of morbidity were diagnosed in a few instances. Three patients (0.4%) had wound bleeding, 4 (0.5%) developed lymph leakage, Horner syndrome was diagnosed in 3 (0.4%) cases, 1 (0.1%) patient had glossopharyngeal nerve injury, 1 (0.1%) had pneumonia, and 1 (0.1%) had wound infection.
Repeated Surgery
Preliminary interim result evaluation, in particular, the high frequency of lung metastases, toughened our approach to surgical treatment and led us to strictly recommending complete thyroid removal in all cases of childhood locally extended thyroid carcinoma. Such tactics were imposed by the necessity to detect metastatic spread using the whole body scan and thyroglobulin measurement. On the whole, 172 repeated surgical procedures were performed for carcinoma recurrence or substantiated suspicion of the disease relapse in 139 patients.
The choice of surgery was determined by recurrence localization and its extension to the neck. Reoperations were performed by skilled surgeons because of the technical difficulties of careful separation of the tracheal wall, parathyroid glands, recurrent laryngeal and cranial nerves, jugular veins, and carotid arteries during the removal of relapse, which in a large proportion of cases was encased by a rough fibrous tissue knitted with the said anatomic structures.
Neck lymph node dissection was performed in 144 of 172 repeated surgical procedures (83.7%). In 124 cases, this type of surgery was performed for proved or suspected metastases, and 20 children were subjected to preventive lymph node removal during the intervention for the relapse in thyroid remnants or metastases in the soft tissues of the neck.
All in all, thyroid remnant removal was performed in 83 of 314 patients (26.4%) having undergone a primary safe operation. Thus, in more than one fourth of cases, subtotal thyroidectomy, lobectomy, or lesser resection had proved inadequate since such procedures did not result in an accurate tumor staging. The majority of local relapses may be qualified as residual disease.
Sixteen of 139 (11.5%) patients developed 20 postoperative complications after reoperations, among them 8 cases of permanent recurrent nerve palsy, 11 instances of hypoparathyroidism, and 1 case of pneumonia.
DISCUSSION
Despite the generally accepted standard treatment options for thyroid cancer, choice of specific surgical procedure in pediatric patients is still a matter of debate. Even the most comprehensive series comprises a relatively small number of enrolled cases. Indeed, surgical procedure adequacy is frequently left to the surgeon's discretion and may not necessarily have an objective basis.
To date, 2 opposite points of view on this problem exist. The most prevailing opinion calls for total thyroidectomy regardless of tumor size and histopathology.12–21,24,25 The rationale for this approach is that thyroid carcinomas are frequently disposed to intraglandular spreads or can be multifocal. Thus, thyroid remnants may become a factor conferring a very high risk of local relapse. Furthermore, residual thyroid tissue presents an obstacle for the diagnosis of distant spread, and for detection of the involvement of those neck and mediastinum lymph nodes that are inaccessible for routine x-ray. Only a radioiodine scan and thyroglobulin measurement after complete thyroidectomy can make recurrence detection possible.24,26,27 On the other hand, safe surgical procedures usually increase the quality of patients’ lives. Thyroid lobectomy, or subtotal thyroidectomy, virtually guarantees a low risk of operative morbidity. In addition, no clear evidence of the relationship between patients’ survival and type of surgical procedure has been demonstrated in childhood cases.7–11
Data obtained in our study confirm excellent survival rates in pediatric patients with thyroid carcinoma. Yet, besides acknowledging this well-known fact, analysis of a large series of eligible cases allowed us to evaluate the impact of patients’ demography, tumor characteristics, and surgical options on the treatment results and to draw evidence-based conclusions.
From the practical point of view, achieving a cure or at least a prolonged disease-free interval after primary surgery is highly desirable. Regarding these goals as our first priority, we attempted to identify the factors affecting disease relapse in the first place.
Multivariate logistic regression analysis demonstrated that such parameters as the young age of the patient, multifocality of the tumor, nodal status, and, remarkably, incomplete neck lymph node dissection independently contributed to local lymph node failure. In our estimation, if a recurrence appears in the neck within a short time after surgical treatment, the failure is likely due to the residuals of carcinoma foci or unnoticed lymph node metastases, which means that the primary tumor in such patients has not been appropriately staged at the time of the first operation.
Our results did not reveal parameters significantly associated with relapses in thyroid remnants. Perhaps the prognostic factors could not be identified because of a relatively small number of such cases. However, probability of this pattern of failure should be taken into account in patients selected for thyroid-preserving surgery as according to the published data, percentage of this type of relapse varies from 20% to 37% depending on the extent of thyroid-preserving surgical procedures.15,28 In our series, more than one-fourth of initial thyroid-preserving operations turned out to be insufficient.
A relatively high proportion of failure in cases when limited operation was performed indicates that extended primary surgery is preferable for childhood carcinomas. Our statistical findings are in accordance with a number of reports suggesting aggressive surgery as a method of choice improving the prognosis, especially in cases with lymph node metastases.13,15,16,18,19,29 Moreover, the complete removal of thyroid tissue allowed detection of pulmonary metastases in a proportion of cases after repeated surgical procedures.
Thus, although none of the fatal outcomes in this series of patients was due to local relapse as neck lymph nodes and recurrence in thyroid remnants were detected in proper time for repeated surgery, our results strongly argue in favor of total thyroidectomy with central and selective (or modified radical) bilateral neck lymph node dissection for the majority of childhood cases. This conclusion may be further strengthened if one takes into account the possible decline in patient's quality of life, treatment complications, and cosmetic defects after repeated surgical procedure(s). Lesser resections are only acceptable in exceptional cases of very small solitary intrathyroidal carcinomas without evidence of neck lymph node involvement on surgical revision.
Lung metastases present the highest potential threat for the patients’ lives. Multivariate analysis in our study identified the patient's age at diagnosis, female gender, and the presence of symptoms as risk factors for distant metastases. The younger age of patients has been associated previously with an elevated risk of dissemination,2,21,29,30 and our data support these claims. It is tempting to speculate that in younger patients cells may possess higher proliferative potential or have greater prevalence of thyroid cancer-specific mutations (and/or other (epi)genetic alterations) contributing to metastatic growth. However, such questions require further fundamental and laboratory investigations. The relation between female gender and a higher risk of lung metastases is also difficult to explain. It is worth noting that univariate analysis did not reveal association between these 2 parameters; therefore, just a simple numerical prevalence of girls in the patients’ cohort does not account for the findings of higher relapse incidence in them. Perhaps a specific sex hormone profile in combination with other factor(s) may favor progression of distant metastases in this subgroup of patients. As for the presence of clinical symptoms, though it could be expected that enlarged neck mass, the main clinical manifestation of thyroid carcinoma, would be linked with the T- and N-status of the disease, these 2 latter indices of tumor extension proved only marginally significant and, therefore, less important for the prognosis in comparison with symptoms at diagnosis. Our data demonstrate that symptomatic patients have a poorer prognosis as compared with asymptomatic ones. Therefore, enlarged lymph nodes and neck discomfort complaints at admission should be taken as a warning sign suggestive, firstly, of the necessity of a radical operation, and secondly, of possible lung metastases.
As surgical treatment is inseparable from associated risk, we performed an analysis of the corresponding complications. According to previously published series, specific surgical morbidity varies widely from 0% to 30%, depending on the extent of initial surgery, with total thyroidectomy and neck lymph node dissections accounting for the highest morbidity rates.5,7,12,13,15,24,29,31 Extensive surgery is commonly suggested for advanced thyroid cancer; therefore, risk of complications may be associated not only with the tumor characteristics that require removal of adjacent tissues but also with the type of operation. From the technical point of view, recurrent nerves can be easily preserved, whereas preservation of the parathyroid glands is usually more difficult. Accordingly, using multivariate analysis, we have not revealed any parameters significantly associated with recurrent nerves palsy. On the contrary, risk of hypoparathyroidism appeared to be strongly dependent on the tumor extension and the degree of surgical aggressiveness. The relatively high frequency of such complications observed at the beginning of this series is worth emphasizing. From 1998 on, the number of adverse effects markedly decreased, and even surgical options switched to more extensive intervention did not lead to immediate result deterioration. Analysis of treatment results in a subgroup of patients operated on after 1998 demonstrates that there is no significant association between bilateral neck lymph node dissection and the risk of recurrent nerves palsy and hypoparathyroidism observed in the whole series (data not shown). Thus, better results of the treatment during the recent time may be directly linked with surgical experience and general improvement of the treatment strategy.
Results obtained in this work are also illustrative of the high efficacy of radioiodine therapy. In the majority of patients with distant metastases, a complete or stable partial response has been achieved. Of the total group, 1 patient with differentiated carcinoma and lung metastases in whom 131I administration was not performed (Results) died within 1 year, which suggests that the number of fatal outcomes in patients with distant recurrence might have been higher without radioiodine therapy.
CONCLUSION
Our work demonstrates that the risk of recurrence in childhood thyroid cancer is strongly associated with the extent of the primary tumor, the young age of the patient, presence of symptoms at diagnosis, and the aggressiveness of the primary surgery. Surgical decision-making is a balance between completeness of removal and quality of patient's life, so a variety of clinical parameters should be taken into account and special attention should be paid to tumor staging, careful separation of parathyroid glands, and recurrent laryngeal nerves at the time of surgery. According to the obtained results, total thyroidectomy with appropriate neck lymph node dissection followed by radioiodine therapy is an optimal treatment strategy that allows cure in most of pediatric patients with differentiated thyroid carcinoma.
Footnotes
Supported in part by Nagasaki University 21st Century COE Program, International Consortium for Medical Care of Hibakusha and Radiation Life Science (2002–2007).
Reprints: Shunichi Yamashita, MD, Department of Molecular Medicine, Atomic Bomb Disease Institute, Nagasaki University Graduate School of Biomedical Sciences, 1-12-4 Sakamoto, Nagasaki 852-8523. E-mail: shun@net.nagasaki-u.ac.jp.
REFERENCES
- 1.Parker DM, Kramarova E, Drapper GJ, eds. International Incidence of Childhood Cancer [IARC Scientific Publications No. 144]. Lyon, France: International Agency for Research on Cancer, 1998:11–15. [Google Scholar]
- 2.Welch Dinauer CA, Tuttle RM, Robie DK, et al. Clinical features associated with metastasis and recurrence of differentiated thyroid cancer in children, adolescents and young adults. Clin Endocrinol (Oxf). 1998;49:619–628. [DOI] [PubMed] [Google Scholar]
- 3.Farahati J, Parlowsky T, Mader U, et al. Differentiated thyroid cancer in children and adolescents. Langenbecks Arch Surg. 1998;383:235–239. [DOI] [PubMed] [Google Scholar]
- 4.Tronko MD, Bogdanova TI, Komissarenko IV, et al. Thyroid carcinoma in children and adolescents in Ukraine after the Chernobyl nuclear accident: statistical data and clinicomorphologic characteristics. Cancer. 1999;86:149–156. [DOI] [PubMed] [Google Scholar]
- 5.Rybakov SJ, Komissarenro IV, Tronko TB, et al. Thyroid cancer in children of Ukraine after the Chernobyl accident. World J Surg. 2000;24:1446–1449. [DOI] [PubMed] [Google Scholar]
- 6.Harness JK. Childhood thyroid carcinoma. In: Clark OH, Quan-Yang D, eds. Textbook of Endocrine Surgery. Philadelphia: Saunders, 1997:75–81. [Google Scholar]
- 7.La Quaglia MP, Corbally MT, Heller G, et al. Recurrence and morbidity in differentiated thyroid carcinoma in children. Surgery. 1988;104:1149–1156. [PubMed] [Google Scholar]
- 8.Massimino M, Gasparini M, Ballerini E, et al. Primary thyroid carcinoma in children: a retrospective study of 20 patients. Med Pediatr Oncol. 1995;24:13–17. [DOI] [PubMed] [Google Scholar]
- 9.Chabot JA, Altman RP. Thyroid and parathyroid. In: Ashcraft KW, Thomas M, eds. Pediatric Surgery, 2nd ed. Philadelphia: Saunders, 1995:941–947. [Google Scholar]
- 10.Ben Arush MW, Stein ME, Perez NM, et al. Pediatric thyroid carcinoma: 22 years of experience at the Northern Israel Oncology Center (1973–1995). Pediatr Hematol Oncol. 2000;17:85–92. [DOI] [PubMed] [Google Scholar]
- 11.Brink JS, van Heerding JA, McIver B, et al. Papillary thyroid cancer with pulmonary metastases in children: long-term prognosis. Surgery. 2000;128:881–887. [DOI] [PubMed] [Google Scholar]
- 12.Ceccarelli C, Pacini F, Lippi F, et al. Thyroid cancer in children and adolescents. Surgery. 1988;104:1143–1148. [PubMed] [Google Scholar]
- 13.Harness JK, Thompson NW, McLeod MK, et al. Differentiated thyroid carcinoma in children and adolescents. World J Surg. 1992;16:547–553. [DOI] [PubMed] [Google Scholar]
- 14.Danese D, Gardini A, Farsetti A, et al. Thyroid carcinoma in children and adolescents. Eur J Pediatr. 1997;156:190–194. [DOI] [PubMed] [Google Scholar]
- 15.Segal K, Shvero J, Stern Y, et al. Surgery of thyroid cancer in children and adolescents. Head Neck. 1998;20:293–297. [DOI] [PubMed] [Google Scholar]
- 16.Hallwirth U, Flores J, Kaserer K, et al. Differentiated thyroid cancer in children and adolescents: the importance of adequate surgery and review of literature. Eur J Pediatr Surg. 1999;9:359–363. [DOI] [PubMed] [Google Scholar]
- 17.Arici C, Erdogan O, Altunbas H, et al. Differentiated thyroid carcinoma in children and adolescents: clinical characteristics, treatment and outcome of 15 patients. Horm Res. 2002;57:153–156. [DOI] [PubMed] [Google Scholar]
- 18.Giuffrida D, Scollo C, Pellegriti G, et al. Differentiated thyroid cancer in children and adolescents. J Endocrinol Invest. 2002;25:18–24. [DOI] [PubMed] [Google Scholar]
- 19.Haveman JW, Van Tol KM, Rouwe CW, et al. Surgical experience in children with differentiated thyroid carcinoma. Ann Surg Oncol. 2003;10:15–20. [DOI] [PubMed] [Google Scholar]
- 20.Schlumberger M, De Vathaire F, Travagli JP, et al. Differentiated thyroid carcinoma in childhood: long-term follow-up of 72 patients. J Clin Endocrinol Metab. 1987;65:1088–1094. [DOI] [PubMed] [Google Scholar]
- 21.Travagli JP, Schlumberger M, De Vathaire A, et al. Differentiated thyroid carcinoma in childhood. J Endocrinol Invest. 1995;18:161–164. [DOI] [PubMed] [Google Scholar]
- 22.Sobin LH, Wittekind C, eds. TNM Classification of Malignant Tumours, 6th ed. 2002.
- 23.SAS/STAT User's Guide, Version 8, Cary, NC: SAS Institute, 1999. [Google Scholar]
- 24.Fassina AS, Rupolo M, Pelizzo MR, et al. Thyroid cancer in children and adolescents. Tumori. 1994;80:257–262. [DOI] [PubMed] [Google Scholar]
- 25.Spinelli C, Bertocchini A, Antonelli A, et al. Surgical therapy of the thyroid papillary carcinoma in children: experience with 56 patients < or = 16 years old. J Pediatr Surg. 2004;39:1500–1505. [DOI] [PubMed] [Google Scholar]
- 26.Vassilopoulou-Sellin R, Klein MJ, Smith TH, et al. Pulmonary metastases in children and young adults with differentiated thyroid cancer. Cancer. 1993;71:1348–1352. [DOI] [PubMed] [Google Scholar]
- 27.La Quaglia MP, Black T, Holcomb GW, et al. Differentiated thyroid cancer: clinical characteristics, treatment, and outcome in patients under 21 years of age who present with distant metastases. A report from the Surgical Discipline Committee of the Children's Cancer Group. J Pediatr Surg. 2000;35:955–999. [DOI] [PubMed] [Google Scholar]
- 28.Landau D, Vini L, A'Hern R, et al. Thyroid cancer in children: the Royal Marsden Hospital experience. Eur J Cancer. 2000;36:214–220. [DOI] [PubMed] [Google Scholar]
- 29.Grigsby PW, Gal-or A, Michalski JM, et al. Childhood and adolescent thyroid carcinoma. Cancer. 2002;95:724–729. [DOI] [PubMed] [Google Scholar]
- 30.Alessandri AJ, Goddard KJ, Blair GK, et al. Age is the major determinant of recurrence in pediatric differentiated thyroid carcinoma. Med Pediatr Oncol. 2000;35:41–46. [DOI] [PubMed] [Google Scholar]
- 31.van Santen HM, Aronson DC, Vulsma T, et al. Frequent adverse events after treatment for childhood-onset differentiated thyroid carcinoma: a single institute experience. Eur J Cancer. 2004;40:1743–1751. [DOI] [PubMed] [Google Scholar]