Abstract
Objective:
To report the distribution and types of injuries in victims of suicide bombing attacks and to identify external signs that would guide triage and initial management.
Summary Background Data:
There is a need for information on the degree to which external injuries indicate internal injuries requiring emergency triage.
Methods:
The medical charts and the trauma registry database of all patients who were admitted to the Hadassah Hospital in Jerusalem from August 2001 to August 2004 following a suicide bombing attack were reviewed and analyzed for injury characteristics, number of body areas injured, presence of blast lung injury (BLI), and need for therapeutic laparotomy. Logistic analysis was performed to identify predictors of BLI and intra-abdominal injury.
Results:
The study population consisted of 154 patients who were injured as a result of 17 attacks. Twenty-eight patients suffered from BLI (18.2%) and 13 patients (8.4%) underwent therapeutic laparotomy. Patients with penetrating head injury and those with ≥4 body areas injured were significantly more likely to suffer from BLI (odds ratio, 3.47 and 4.12, respectively, P < 0.05). Patients with penetrating torso injury and those with ≥4 body areas injured were significantly more likely to suffer from intra-abdominal injury (odds ratio, 22.27 and 4.89, respectively, P < 0.05).
Conclusion:
Easily recognizable external signs of trauma can be used to predict the occurrence of BLI and intra-abdominal injury. The importance of these signs needs to be incorporated into triage protocols and used to direct victims to the appropriate level of care both from the scene and in the hospital.
Following a suicide bombing attack, scores of casualties suffering from complex injuries are examined by paramedical and medical crews. External signs such as penetrating injury to the head and torso and the presence of injury to four or more body areas are predictors of blast lung injury and intra-abdominal injury and should be used to direct patients to the appropriate level of care.
Suicide bombing attacks have become a threat to civilians all over the world, and physicians treating trauma victims need to have the training and preparation to handle casualties of such attacks.1 To better deal with the influx of numerous severely injured victims and the chaos that ensues, victims need to be directed to the appropriate level of care, and life-threatening injuries need to be swiftly recognized and treated. In these circumstances, early diagnosis depends on focused physical examination and on limited imaging studies.
Blast lung injury (BLI) is diagnosed in up to 45% of fatalities of an explosion and is caused by the rapid expansion of the blast wave, a phenomenon that is exacerbated in confined spaces.2–4 Victims of suicide bombing attacks inside buses have been shown to suffer from diffuse alveolar injury, pneumothoraces, and bronchopleural fistulas. Timely initiation of therapy including unconventional methods such as high-frequency jet ventilation, independent lung ventilation, and nitric oxide may improve survival.5
Intra-abdominal injury is seen less frequently in victims of explosions compared with BLI.6 The mechanisms of injury are the rapid expansion of the blast wave, which results in pressure differentials at the interface between tissues of varying densities, and penetrating injury from shrapnel and other debris.7 Early recognition of BLI and intra-abdominal injury, 2 of the leading causes of in-hospital mortality, may improve outcome by directing patients to the appropriate level of care and initiating early treatment.5
Jerusalem was the target of 17 of the 59 suicide bombing attacks that took place in Israel from August 2001 to August 2004.8 The Hadassah University Hospital Ein-Kerem Campus is the only level I trauma center in Jerusalem. We have recently analyzed the experience acquired at our hospital in managing and treating survivors of suicide bombing attacks.9 The primary objective of this work was to study the frequency and pattern of injuries associated with BLI and intra-abdominal injury, 2 of the leading causes of morbidity and mortality following a suicide bombing attack.5,9 The secondary objective was to identify external signs of trauma that will serve as predictors of BLI and intra-abdominal injury.
METHODS
We retrospectively reviewed the records of all victims of suicide bombing attacks who were admitted to the Hadassah University Hospital, Ein Kerem Campus, in Jerusalem between August 2001 and August 2004. Data were retrieved from medical records and the trauma registry database. The trauma registry is a prospectively collected database that is updated daily by dedicated personnel. The charts of all patients admitted to the hospital with the diagnosis of trauma are reviewed and demographic data such as gender, age, cause of trauma, and types of injuries and their location and severity are recorded. The registry is updated daily for diagnostic and surgical procedures that were performed and patient outcome.
Data Collection
The trauma registry database was screened for patients who were physically injured and admitted to the hospital following a suicide bombing attack. Data were collected from medical charts and the trauma registry for demographic characteristics, the presence and location of penetrating wounds, location and type of fractures (open versus closed), the presence of burns, ear-drum perforation, BLI, intra-abdominal trauma, and injury severity score (ISS). The severity of BLI, the need and duration of mechanical ventilation, and the surgical procedure were recorded. The diagnosis of BLI was determined based on previously published criteria, briefly, pO2/FIO2 < 200 and the presence of typical imaging findings.5,10 The severity of BLI injury was defined according to the degree of hypoxemia, whether the contusion was unilateral or bilateral, and the presence of a bronchial pleural fistula.5 A therapeutic laparotomy was defined as previously published.11
Data Analysis
For the purpose of mapping external injuries the body was divided into 9 areas (head, neck, cervical spine, chest, upper back, abdomen, lower back, legs, and arms) and the presence of visible injury to each area such as penetrating wounds and burns was retrieved from the trauma registry database (Fig. 1). To quantify the extent of external injury, we added the sum of injured areas and defined it as the “number of areas injured” (range, 1–9). There were 110 patients who sustained injuries to 1 to 3 body areas and 44 patients who sustained injuries to ≥4 body areas (median number of body areas injured, 3; interquartile range [IQR], 2–4). We therefore used the cutoff of ≥4 body areas injured and defined it as “injury to multiple areas.” To analyze the distribution and importance of penetrating injury, the 9 areas of the body were grouped into 3 zones: head (head, neck and cervical spine), torso (chest, abdomen, and upper and lower back), and extremities (legs and arms).
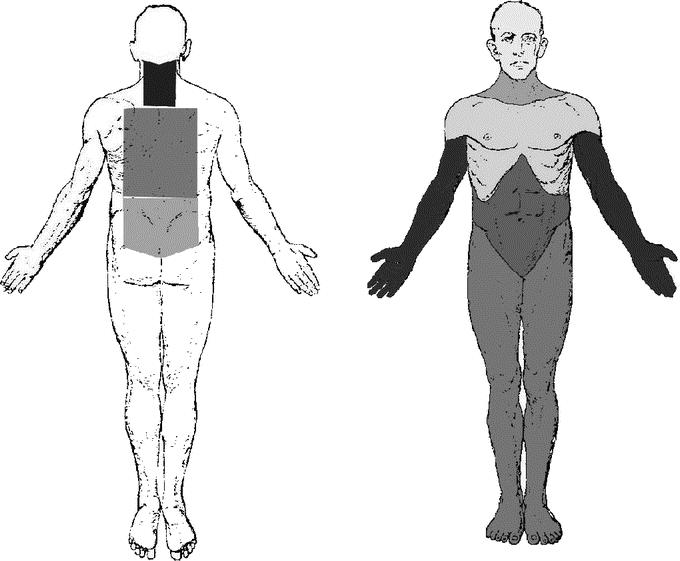
FIGURE 1. Graphic illustration of the 9 body areas. Right: anterior view showing the head, neck, chest, abdomen, arms, and legs. Left: posterior view showing the cervical spine, upper back, and lower back. Details of injury to each area were retrieved from the trauma registry database and recorded.
Statistical Analysis
Data are presented as median and IQR. The χ2 test and Fisher exact test were used to compare proportions and the Mann-Whitney U test was used to compare continuous variables. The odds ratio as well as its 95% confidence interval was calculated for each of the injury types studied. Multivariate logistic regression analysis was performed to analyze external predictors of BLI and intra-abdominal injury. A P value of 0.05 or less was considered statistically significant. Statistical analysis was performed using SPSS version 11.5 (Statistical Package for Social Science, Chicago, IL).
RESULTS
Patient Population
From August 2001 to August 2004, there were 17 suicide bombing attacks in Jerusalem. As a result of these attacks, 430 patients were examined in the Emergency Department of the Hadassah University Hospital, Ein Kerem Campus and 157 patients (36.5%) were admitted. Three patients were transferred from other hospitals and were excluded from the study. The study population consisted of 75 males and 79 females with a median age of 24.5 years (IQR, 17.25–34.75 years) (Table 1). There were 10 in-hospital deaths: 5 patients died of severe intracranial injury (median 8 days after admission), 2 patients died of penetrating intrathoracic injury (both on the day of admission), 2 patients died of uncontrollable retroperitoneal and intra-abdominal hemorrhage (both on the day of admission), and 1 patient died of severe BLI (day 4).
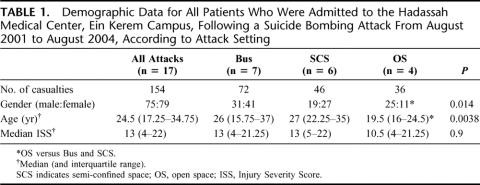
TABLE 1. Demographic Data for All Patients Who Were Admitted to the Hadassah Medical Center, Ein Kerem Campus, Following a Suicide Bombing Attack From August 2001 to August 2004, According to Attack Setting
Attack Setting
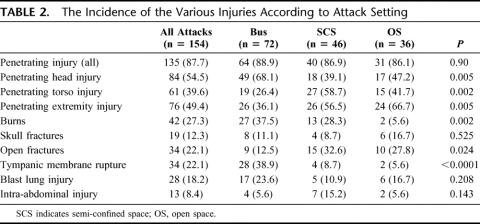
Three settings were targeted: buses, semi-confined spaces such as covered open markets, restaurants and indoor cafés, and open spaces such as outdoor cafés and bus stops. In open spaces, there were more males and the patients were younger compared with buses and semi-confined spaces (Table 1). The median number of casualties admitted to the hospital per attack and the median number of severely injured casualties (ISS ≥ 16) per attack did not differ significantly between the various settings (Fig. 2). Patients injured in open spaces were more likely to suffer from penetrating extremity injury and less likely to suffer from the effects of the blast wave (burns and tympanic membrane rupture) compared with patients injured in semi-confined spaces and buses (Table 2).
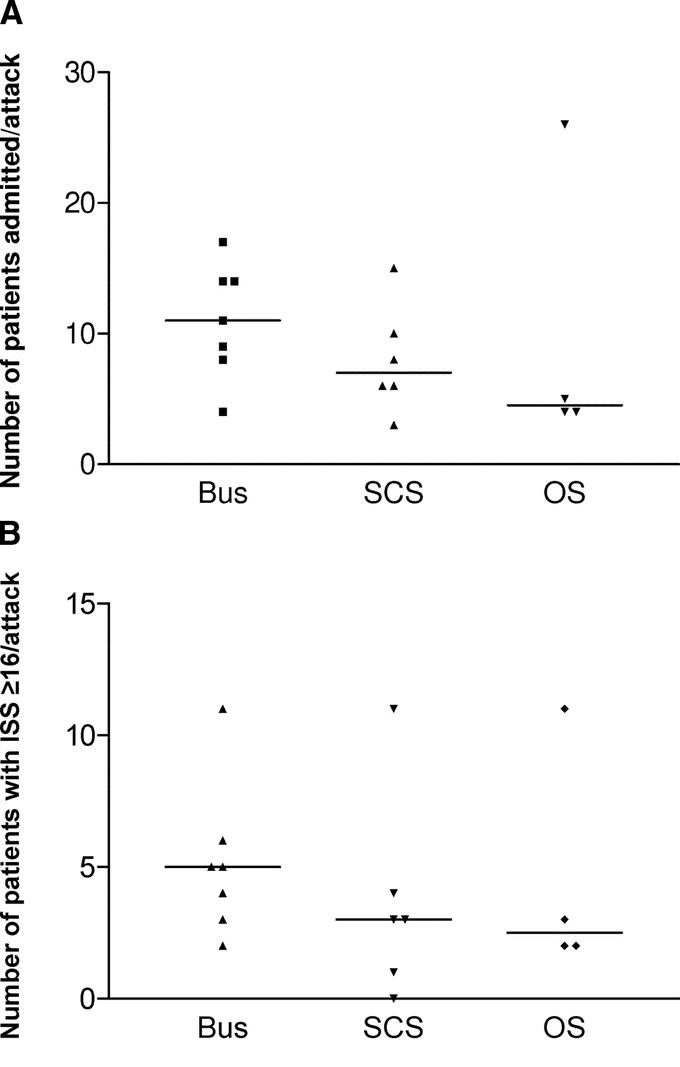
FIGURE 2. A, The number of casualties per suicide bombing attack who were admitted to the Hadassah Medical Center. B, The number of casualties with ISS ≥ 16 per suicide bombing attack who were admitted to the Hadassah Medical Center, August 2001 to August 2004. Medians are not significantly different. SCS, semi-confined space; OS, open space.
TABLE 2. The Incidence of the Various Injuries According to Attack Setting
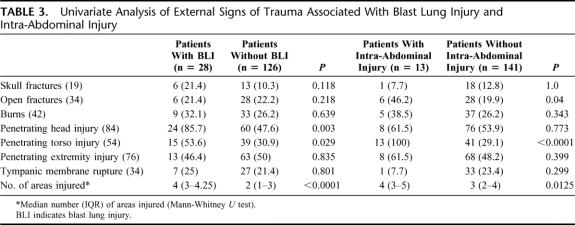
BLI
Twenty-eight of the 154 patients (18.2%) suffered from BLI. Three patients had severe lung injury (10.7%), 17 had moderate injury (60.7%), and 8 had mild injury (28.6%). One patient with severe BLI died of respiratory failure 4 days after admission. Associated injuries are shown in Table 3. Median ISS for patients with BLI was 21 (IQR, 17–34.5) and 23 of the 28 patients (82.1%) had an ISS ≥ 16. Patients with BLI were mechanically ventilated for a median of 1 day (IQR, 0–5 days) and the median intensive care unit length of stay was 4 days (IQR, 1–7 days). The median overall length of stay for patients with BLI was 10 days (IQR, 6.75–20.25 days).
TABLE 3. Univariate Analysis of External Signs of Trauma Associated With Blast Lung Injury and Intra-Abdominal Injury
The incidence of all degrees of BLI did not differ significantly between the various settings. Of the 28 patients with BLI, 20 (71.4%) suffered moderate to severe injury. The incidence of moderate and severe BLI in semi-confined and confined (bus) spaces was significantly higher compared with open spaces. Of the 22 patients with BLI who were injured inside buses and semi-confined spaces, 18 (81.8%) developed moderate to severe BLI compared with 2 of the 6 patients (33%) who were injured in open spaces (P < 0.05).
Predictors of BLI
Multivariate regression analysis was performed to identify external predictors of BLI. Attack setting, penetrating injury to head and torso, skull fracture, and the presence of 4 or more body areas injured (“injury to multiple areas”) were entered into a backward stepwise regression model. Penetrating injury to the head (odds ratio, 3.47; 95% confidence interval, 1.01–12.13, P = 0.049) and injury to 4 or more areas (odds ratio, 4.12; 95% confidence interval 1.54–11.03, P = 0.005) were found to be independent predictors of BLI.
Intra-abdominal Injury
Fifteen patients underwent laparotomy for the following findings: hemodynamic instability in the presence of penetrating torso injuries (n = 4), penetrating abdominal injury and a positive sonogram (n = 3) and penetrating abdominal injury and findings on computerized tomography scan (CT) revealing intra-abdominal injury (n = 8). The indication for surgery for the 2 patients with negative explorations was hemodynamic instability. Thirteen of the 154 patients (8.4%) underwent a therapeutic laparotomy for one or more of the following injuries: small bowel (n = 7), colon (n = 5), spleen (n = 4), liver (n = 3), stomach (n = 3), and rectum (n = 1). Associated injuries are shown in Table 3. Four of the 13 patients with intra-abdominal injury also suffered from BLI, all 4 with moderate to severe BLI.
Median ISS for patients with intra-abdominal injury was 26 (IQR, 22–34) and 11 of the 13 patients (84.6%) had an ISS ≥ 16. Penetrating trauma was the cause of all abdominal injuries. Laparotomy was performed in all cases within 6 hours of admission. Patients with intra-abdominal injury were admitted to the intensive care unit for a median of 5 days (IQR, 2–12 days) and their median overall length of stay was 21 days (IQR, 13–29 days).
Predictors of Intra-abdominal Injury
Multivariate regression analysis was performed to identify external predictors of intra-abdominal injury. Attack setting, penetrating torso injury, open fractures, and the number of areas injured were entered into a backward stepwise regression model. As expected, the presence of penetrating torso injury was found to be an independent predictor of intra-abdominal injury (odds ratio, 22.27; 95% confidence interval, 2.58–192.62, P = 0.005). After removal of penetrating torso injuries, intuitively an important predictor of intra-abdominal injury, injury to 4 or more areas (odds ratio, 4.89; 95% confidence interval, 1.83–13.1, P = 0.001) was found to be an independent predictor of intra-abdominal injury.
DISCUSSION
Following a suicide bombing attack, there is an influx of a large number of patients suffering from complex injuries over a short time period.9 Victims suffer from a combination of blast injury, penetrating wounds, and burns.12 Triage performed at the scene and in the hospital will determine the distribution of casualties to the different medical and trauma centers, and the distribution of patients within a medical facility to the different levels of care. During these chaotic stages, guidelines are needed to improve triage, delivery of care, and utilization of resources.
The concept of a level I trauma center was introduced to improve delivery of care and outcome for severely injured trauma patients.13,14 Einav et al, however, have shown that only 48% of severely injured victims of terror attacks in Israel are brought to level I trauma centers.15 A possible explanation for those findings is the difficulty in recognizing the signs of BLI and intra-abdominal injuries, particularly when EMS crews are flooded with numerous victims with complex injuries. The cardinal finding of this study is that selection of the majority of victims with BLI and intra-abdominal injury can be performed based on easily recognizable external signs such as the number of areas injured and the presence of penetrating head and torso wounds. Patients suffering from BLI and intra-abdominal injury will often require sophisticated ventilatory support, well-equipped intensive care units, well-trained personnel, and a multidisciplinary approach, resources that are usually limited to level I trauma centers. Our data suggest that patients with injuries to 4 or more body areas and those with penetrating head and torso wounds should be brought to level I trauma centers, which are able to provide such superior care.
Because of the mayhem and the large number of victims, triage following suicide bombing attacks cannot be performed according to conventional scoring systems.16–19 Thus, there is a need for a simple, quick, and intuitive method for determining the presence of internal injuries in mass casualty events. The number of areas with external injuries is intuitively, yet thus far unrecognized, predictor of the severity of injury. Our data show that external injury to 4 or more body areas is a predictor of BLI and intra-abdominal injury. Indeed, there was good correlation between ISS and the number of areas injured (Spearman's coefficient, 0.525; P < 0.0001). A probable explanation for this finding is that victims in proximity to an explosive device, which is accompanied by a large amount of shrapnel, are more likely to suffer from the effects of the blast wave and from multiple penetrating wounds.
Isolated head injury has been shown to be associated with BLI and the adult respiratory distress syndrome.20,21 Following isolated traumatic brain injury in rats ultrastructural changes, such as intracellular edema and dilatation of the smooth endoplasmic reticulum, have been recognized in type II pneumocytes as early as 2 hours after injury.22 These findings and the findings of others may be consistent with our data showing that penetrating head injury is an independent predictor of BLI, and suggests that part of the pulmonary injury following a blast is caused by release of neurotransmitters, cytokines, and free radicals.
The Emergency Department at Hadassah Hospital is composed of an admitting area and a trauma unit. During mass casualty events, our setup is such that a team of surgeons is assigned to each bed in the trauma unit, whereas in the admitting area each team is responsible for 3 or 4 patients.9 The most experienced surgeons are allocated to the trauma unit and as a result many of the casualties in the admitting area will be initially managed by surgeons and physicians who are not necessarily experienced in trauma. Thus, in the initial phases of treatment, patients directed to a trauma unit setting will receive more attention by better trained physicians compared with patients directed to the admitting area. The decisions made by the surgeon-in-charge as he or she examines the patients being brought to the hospital by EMS crews and other nonmedical personnel is pivotal to their immediate management.9 By defining and stressing the relevance of visible signs of trauma, we are able to provide the surgeon-in-charge with better tools for triaging victims (Fig. 3).
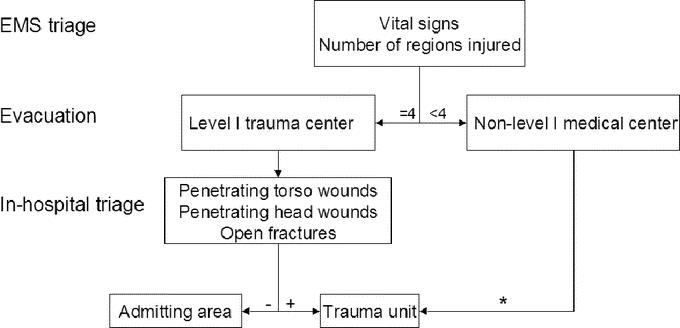
FIGURE 3. Proposed protocol for determining evacuation and triage preferences. *, secondary transfers; EMS, emergency medical services.
Our data show that attack setting has implications on the composition and number of casualties, and on their injuries. Injuries caused by the blast wave and the heat wave that ensues, ie, BLI, tympanic membrane rupture and burns, become increasingly more common as the setting changes from open spaces to semi-confined and confined spaces (buses). Specifically, the severity of BLI becomes progressively worse in buses and semi-confined spaces compared with open spaces. This has implications on the scope of injuries that is to be expected depending on the attack setting and on hospital preparedness, particularly the need for intensive care unit beds and advanced ventilatory therapies.5
Katz et al have reported on 29 hospitalized victims of an explosion inside a bus who were treated at 2 medical centers.6 Diagnosis of bowel perforation was late, and both patients underwent laparotomy 3 and 7 days following the blast. The current cycle of violence has unfortunately given us the possibility to reexamine the incidence and factors associated with intra-abdominal injury in these circumstances. Our data, based on 154 hospitalized victims of 17 suicide bombing attacks who were treated in our hospital, show that intra-abdominal injury is caused by penetrating shrapnel and not by the blast wave. Our results demonstrate that intra-abdominal injury can be suspected based on the presence of penetrating torso wounds and the presence of injuries to ≥4 body areas. Diagnosis can be established within 6 hours of injury based on sonogram and CT. The disparity between our results and previous reports can be explained by changes that have taken place in regards to the type and mass of explosive material and shrapnel and the location of the explosive device. The explosive material has changed from low to military-grade, shrapnel has changed from low- to high-mass, and the location of the explosive device, which was concealed under the seats, is now carried at chest height. Thus, victims in proximity to the explosive device absorb higher levels of energy and are less likely to survive and develop bowel perforation; and correspondingly, the severity of penetrating injuries among survivors is intensified.
The approach to each victim of a mass casualty event is based on conventional guidelines. Since penetrating injury to the torso is highly sensitive (100%) of clinically significant abdominal trauma but lacks specificity (71%), we recommend that all patients with penetrating abdominal trauma who are hemodynamically stable undergo imaging studies to rule out intra-abdominal injury. A focused abdominal sonogram for trauma should be performed in each and every case. In hemodynamically stable patients without signs of peritonitis, CT should be performed after the initial chaotic state has settled down, ie, within 4 to 6 hours of admission.23
Adjustments to our protocol were introduced gradually as our experience accumulated. This was not a prospective randomized study, and it is therefore impossible to declare that by implementing any of our findings we were able to deliver better care. Based on our experience, we believe that adopting these broad guidelines for triage and immediate management will assist physicians in treating victims of suicide bombing attacks.
CONCLUSION
Our results show that external signs of trauma such as penetrating head and torso injury and the number of body areas injured can serve as surrogates of severe trauma. We recommend that the relevance of these external signs be incorporated into the protocols for trauma triage both at the scene and in the hospital.
Footnotes
Reprints: Gidon Almogy, MD, Department of Surgery and Trauma Unit, Hadassah Medical Center, P.O. Box 12000, Jerusalem, 91120, Israel. E-mail: galmogy@Hadassah.org.il.
REFERENCES
- 1.Stein M, Hirshberg A. Medical consequences of terrorism: the conventional weapon threat. Surg Clin North Am. 1999;79:1537–1552. [DOI] [PubMed] [Google Scholar]
- 2.Philips YY. Primary blast injuries. Ann Emerg Med. 1986;15:1446–1450. [DOI] [PubMed] [Google Scholar]
- 3.Wightman JM, Gladish SL. Explosions and blast injuries. Ann Emerg Med. 2001;37:664–678. [DOI] [PubMed] [Google Scholar]
- 4.Leibovici D, Gofrit ON, Stein M, et al. Blast injuries in a bus versus open air bombings: a comparative study of injuries in survivors of open air versus confined space explosions. J Trauma. 1996;41:1030–1035. [DOI] [PubMed] [Google Scholar]
- 5.Pizov R, Oppenheim-Eden A, Matot I, et al. Blast lung injury from an explosion on a civilian bus. Chest. 1999;115:165–172. [DOI] [PubMed] [Google Scholar]
- 6.Katz E, Ofek B, Adler J, et al. Primary blast injury after a bomb explosion in a civilian bus. Ann Surg. 1989;209:484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper GJ, Maynard RL, Cross NL, et al. Casualties from terrorist bombings. J Trauma. 1983;23:955–967. [DOI] [PubMed] [Google Scholar]
- 8.Israel Ministry of Foreign Affairs. Available at http://www.mfa.gov.il/MFA/.
- 9.Almogy G, Belzberg H, Mintz Y, et al. Suicide bombing attacks: update and modifications to the protocol. Ann Surg. 2004;239:295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mellor SG. The relationship of blast loading to death and injury from explosion. World J Surg. 1992;16:893–898. [DOI] [PubMed] [Google Scholar]
- 11.Demetriades D, Velmahos G, Cornwell E, et al. Selective nonoperative management of gunshot wounds of the anterior abdomen. Arch Surg. 1997;132:178–183. [DOI] [PubMed] [Google Scholar]
- 12.Peleg K, Aharonson-Daniel L, Stein M, et al. Gunshot and explosion injuries: characteristics, outcomes, and implications for care of terror-related injuries in Israel. Ann Surg. 2004;239:311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiRusso S, Holly C, Kamath R, et al. Preparation and achievement of American College of Surgeons level I trauma verification raises hospital performance and improves patient out come. J Trauma. 2001;51:294–299. [DOI] [PubMed] [Google Scholar]
- 14.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. [DOI] [PubMed] [Google Scholar]
- 15.Einav S, Feigenberg Z, Weissman C, et al. Evacuation priorities in mass casualty terror-related events: implications for contingency planning. Ann Surg. 2004;239:304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker SP, O'Neill B, Haddon W Jr. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 17.Champion HR, Copes WS, Sacco WJ. A new characterization of injury severity. J Trauma. 1990;30:539–545. [DOI] [PubMed] [Google Scholar]
- 18.Kollef MH, Schuster DP. Predicting intensive care unit outcome with scoring systems: underlying concepts and principles. Crit Care Clin. 1994;10:1–18. [PubMed] [Google Scholar]
- 19.Sauaia A, Moore FA, Moore EE. Multiple organ failure can be predicted as early as 12 hours after injury. J Trauma. 1998;45:291–301. [DOI] [PubMed] [Google Scholar]
- 20.Fontes RB, Aguiar PH, Zanetti MV, et al. Acute neurogenic pulmonary edema: case reports and review of the literature. J Neurosurg Anesthesiol. 2003;15:144–150. [DOI] [PubMed] [Google Scholar]
- 21.Macmillan CS, Grant IS, Andrews PJ. Pulmonary and cardiac sequelae of subarachnoid haemorrhage: time for active management? Intensive Care Med. 2002;28:1012–1023. [DOI] [PubMed] [Google Scholar]
- 22.Yildirim E, Kaptanoglu E, Ozisik K, et al. Ultrastructural changes in pneumocyte type II cells following traumatic brain injury in rats. Eur J Cardiothorac Surg. 2004;25:523–529. [DOI] [PubMed] [Google Scholar]
- 23.Stein M, Hirshberg A. Limited mass casualties due to conventional weapons: the daily reality of a level I trauma center. In: Shemer J, Shoenfeld Y, eds. Terror and Medicine: Medical Aspects of Biological, Chemical and Radiological Terrorism. Lengerich: Pabst Science, 2003:378–393. [Google Scholar]