Abstract
Objectives. We evaluated the effectiveness of an intervention designed to increase preventive health care seeking among adolescents.
Methods. Adolescents and young adults aged 12 to 21 years, recruited from community-based organizations in 2 different communities, were randomized into either a 3-session intervention or a control condition. We estimated outcomes from 3-month follow-up data using logistic and ordinary least squares regression.
Results. Female intervention participants were significantly more likely than female control participants to have scheduled a health care appointment (odds ratio [OR]=3.04), undergone a checkup (OR=2.87), and discussed with friends or family members the importance of undergoing a checkup (OR=4.5). There were no differences between male intervention and male control participants in terms of outcomes.
Conclusions. This theory-driven, community-based group intervention significantly increased preventive health care seeking among female adolescents. Further research is needed, however, to identify interventions that will produce successful outcomes among male adolescents.
Sexually active adolescents and young adults have the highest rates of sexually transmitted diseases (STDs) in the United States, yet they are less likely to seek and receive health care than any other age group.1–3 If young people delay or avoid seeking health care, they may be at increased risk of transmitting infections to sexual partners and experiencing long-term negative sequelae such as infertility, chronic pelvic pain, and cancer.4 Even when adolescents seek care, they are much less likely to undergo comprehensive preventive health assessments that include screening for STDs. Here we describe the outcomes of an intervention designed to increase health care seeking behaviors among adolescents and young adults in 2 communities with high rates of STD endemicity.
There are many benefits associated with increasing preventive health care seeking on the part of adolescents, including early diagnosis and treatment of illness and the opportunity for preventive health education. Adolescents who use preventive health services have been shown to engage in fewer risk behaviors and more health promoting behaviors and to be in better health.2,5–7 In addition, establishing the habit of seeking preventive health services during this age period can build health behaviors that may continue throughout adulthood.
Adolescents may face structural, social, or psychological barriers to seeking health care. Family income and access to health insurance are consistently related to use of preventive health care in this age group.7–10 However, even adolescents with health insurance coverage seek preventive health care less frequently than adults.11 Psychosocial barriers to seeking care include concerns about confidentiality, a sense of invulnerability, and, among adolescent girls, embarrassment and not wanting their parents to know they are seeking sexual health care.7,9
Despite the public health benefits of use of periodic preventive services, minimal attention has been directed at community-based interventions designed to promote preventive health care seeking behaviors among adolescents.12 A recent school-based intervention was found to have produced no significant increases in health care seeking among an intervention group relative to a control group, and almost 50% of participants in both groups reported not having received needed care. Thus, there is a critical need for effective interventions designed to increase health care use among this vulnerable population.
The present study involved a randomized controlled trial of a skill-building intervention intended to increase preventive health care seeking among adolescents. The intervention, offered through the facilities of community-based organizations (CBOs) providing after-school educational and sports programs, promoted positive beliefs and attitudes regarding preventive health care visits, skills and self-efficacy in regard to seeking health care, and communication with others regarding the importance of undergoing checkups. The study was conducted as part of a larger project—the Gonorrhea Community Action Project—involving complementary interventions targeting health care providers, STD clinic patients, and community awareness in 3 communities with high rates of STDs. The interventions shared a common theoretical framework and common measures of key constructs (M. Hogben, N. VanDevanter, C. K. Malotte, et al., unpublished data, 2003).
METHODS
Participants and Recruitment
Adolescents and young adults between the ages of 12 and 21 years were recruited at CBOs located in central Harlem, NY, and Prince George’s County (PGC), Maryland, from January 2000 to June 2001. Age and geographic location were the only inclusion criteria. Male adolescents and young adults were not recruited in PGC because no easily accessible public health clinic targeted toward male patients existed when the study began.
Project staff and peer educators approached potential participants at collaborating CBOs, explaining the project and distributing informational flyers. Parental consent forms were given to participants younger than 18 years to be signed and returned before initiation of baseline data collection, and contact information for reminder telephone calls was collected. Participants received $10 for attending each intervention session, $45 for completion of the 3 study surveys, $3 transportation vouchers for each workshop session, and a $25 gift certificate for completion of the workshops.
Initially, potential participants were recruited by study staff at several CBOs. The intervention was offered as an addition to the organizations’ ongoing schedule of programs, often requiring participants to travel to another agency. Because the initial turnout for workshops was sporadic, an alternative recruitment approach was developed. In New York, project staff worked with several CBOs to incorporate the workshops into their existing programming, allowing participants to remain at the CBO while taking part in the intervention. In PGC, the staff members of a single, large CBO were trained by the researchers to deliver the intervention. The integrated organizational approach greatly facilitated recruitment efforts, leading to a nearly 100% response rate.
Randomization Procedure
Within each agency, participants were randomly assigned to intervention and control groups. Participants were enrolled into new cohorts on a monthly basis. In Harlem, after completion of the baseline questionnaire, groups were randomized into intervention workshops or a 1-session self-esteem-building intervention. All groups randomized to the control condition were offered the opportunity to participate in the intervention workshops after completion of the 3-month follow-up survey. In PGC, after completing the baseline questionnaire, young women were randomized to either the intervention or a 3-session self-esteem-building intervention.
Intervention
The goal of the intervention, labeled “Check Out That Body” (COTB), was to increase health care seeking among adolescents and young adults in the 2 study communities. The intervention comprised 3 interactive skill-building workshops each 1.5 hours in duration. Adolescents and young adults from both communities were involved in the development and tailoring of the intervention workshops during the formative phase of the research.
In Harlem, an adult community advisory board was instrumental in focusing the intervention on encouraging participants to undergo comprehensive checkups that included STD testing. The members of the advisory board believed that this approach would be less stigmatizing and would have the added benefit of creating a norm for preventive health care seeking in adulthood.
Gender-specific sessions were facilitated by gender-matched health educator and peer leaders. Group sizes in these sessions ranged from 3 to 14 participants (median: 9).
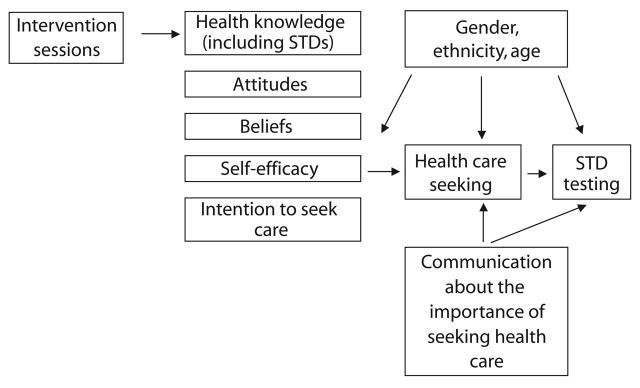
An integrated health behavior model including constructs from the theory of reasoned action, social cognitive theory, and psychological empowerment theory provided the theoretical framework for the intervention.13,14 Each session was designed to increase knowledge, positive beliefs, and attitudes regarding the benefits of preventive primary care visits (Harlem) or reproductive health visits (PGC), as well as to increase skills, self-efficacy, and intentions in regard to seeking health care. Figure 1 ▶ demonstrates the intervention logic model (for a more fully developed description of the theoretical framework and test of the model, see Hogben et al.15).
FIGURE 1—
Intervention logic model used in the “Check Out That Body” intervention.
Intervention sessions were highly interactive, involving discussions, brainstorming, games, and role-play activities. Participants learned communication skills in the first session, and their homework assignment was to talk with a friend or parent about the importance of preventive health visits. Session 2 focused on confidentiality laws, insurance eligibility, what to expect at a preventive health visit, and provision of information about STDs, mental health, and substance use. During session 3, a local physician led a discussion based on questions anonymously submitted by participants, reviewed what to expect in a preventive health visit, and conducted role-play exercises. Finally, participants formulated a detailed plan for scheduling checkups and received graduation certificates.
Quality Assurance
All health/peer educators participated in a standardized curriculum training program. Each intervention session was videotaped, and a subset of the sessions were randomly selected to be independently reviewed by 2 investigators. Throughout the project, facilitators received ongoing supervision and feedback regarding delivery of the intervention.
Sample
Table 1 ▶ describes the 313 adolescents and young adults recruited for the study from Harlem (n=226; 114 female and 108 male participants) and PGC (n=91; all female). The mean age of the sample was 15.8 years; male participants were slightly older than female participants. Most participants were Black; 12.3% were Latinas. Approximately 88% were enrolled in school. More than half of the participants were not employed, but 41.3% reported part-time work. Approximately one third lived with both parents, and slightly more than half (51.6%) lived with one parent.
TABLE 1—
Baseline Demographic Characteristics of Study Participants, by Site and Gender: Gonorrhea Community Action Project, 2000–2001
| Site | |||||
| Characteristic | Female PGC (n = 91) | Female NYC (n = 114) | Male NYC (n = 108) | Total (n = 313) | Site Difference Statistica (P) |
| Age, y, mean (SD) | 15.6 (2.3) | 15.9 (1.8) | 15.9 (1.8) | 15.8 (1.9) | 0.72 (.49) |
| Race/ethnicity, % | |||||
| Black | 89.0 | 72.6 | 81.9 | 80.8 | |
| Hispanic | 5.5 | 17.9 | 12.4 | 12.3 | 9.27 (.06) |
| Other | 5.5 | 9.5 | 5.7 | 6.9 | |
| Education, % | |||||
| Less than/some high school | 74.7 | 82.2 | 85.0 | 81.0 | |
| High school diploma | 19.8 | 13.1 | 13.1 | 15.1 | 4.45 (.35) |
| Other | 5.5 | 4.7 | 1.9 | 3.9 | |
| Currently in school | 74.7 | 94.7 | 91.6 | 87.8 | 0.0001 (.23) |
| Employment status, % | |||||
| Not employed | 56.0 | 46.4 | 55.1 | 52.3 | |
| Employed part time | 28.6 | 51.8 | 41.1 | 41.3 | 23.96 (.000) |
| Employed full time | 15.4 | 1.8 | 3.7 | 6.5 | |
| Living situation, % | |||||
| Lives with both parents | 40.7 | 27.9 | 29.6 | 32.3 | |
| Lives with one parent | 44.0 | 53.2 | 56.5 | 51.6 | 5.56 (.47) |
| Lives with relatives | 11.0 | 12.6 | 10.2 | 11.3 | |
| Other | 4.4 | 6.3 | 3.7 | 4.8 | |
aWith the exception of age, all statistics are χ2 values.
PGC participants were more likely to be Black, less likely to be enrolled in school, and more likely to be working full time than Harlem participants. At baseline, there were no differences between intervention and control participants in regard to age, ethnicity, education, employment, or living situation. However, higher proportions of participants still in high school and Latina participants were lost to follow-up (data not presented). The present analyses were limited to the 153 female and 69 male adolescents who completed all surveys (response rate: 71%).
Data Collection and Measures
Data from 3 rounds of self-administered questionnaires were collected. Baseline data were collected immediately before randomization and the initial intervention session. Follow-up interviews were conducted directly after completion of the intervention and 3 months after initiation of the intervention. In these interviews, data were gathered on demographic characteristics and on psychosocial factors underlying health seeking behaviors. In addition, questions were asked regarding intention to undergo a checkup, scheduling of a checkup, and actual visits to health care providers.14 Participants were also asked about patient–provider interactions and STD testing at their most recent visit.
The primary endpoints examined were as follows: (1) scheduling an appointment for a checkup, (2) undergoing a checkup, and (3) talking about the importance of undergoing a checkup with a friend or family member. As a means of assessing patterns of health care seeking, participants were asked whether they had seen a doctor or made an appointment to see a doctor for a checkup in the 3 months subsequent to the intervention. As a means of assessing behavioral outcomes related to the empowerment activity included in session 1, participants were asked “In the last 60 days have you talked to anyone about how important it is for people your age to go for a health checkup?”
We also gathered information, using 7-point scales ranging from negative to positive responses, on the intervention’s effects in regard to psychosocial variables involved in seeking health care and talking to physicians. In addition, a 3-item scale was constructed to measure attitudes toward undergoing a checkup (e.g., “How much would you like or dislike going for a checkup at least once a year?”). The Cronbach α coefficient for this scale was 0.71.
We measured beliefs about having a checkup once a year by asking participants the extent to which they agreed or disagreed with 20 statements, originally identified through elicitation research, that focused on yearly health care checkups. Half of these belief statements were framed as benefits, such as “Going for a checkup at least once a year would help me find out I am healthy” and “Going for a checkup at least once a year would help me get cured if I had gonorrhea or chlamydia” (Cronbach α = 0.75). The other half were framed as costs, such as “Going for a checkup at least once a year would be scary for me” and “Going for a checkup at least once a year would cause me problems with my family” (Cronbach α = 0.78).
Global self-efficacy regarding seeking preventive health care was assessed with a single item: “How sure are you that you can go for a checkup at least once a year?” Also, we created a situation-specific scale (Cronbach α = 0.87) composed of 7 self-efficacy items (e.g., “I can go for a health checkup in the next year if I have no symptoms” and “I can go for a checkup in the next year if I have to make an appointment”). Intention to undergo a checkup was assessed with the question “How likely is it that you will go for a checkup at least once a year?” In addition, participants were asked “How much do you agree or disagree that it is appropriate for a doctor to talk to you about each of the following issues (nutrition, sex, drugs and alcohol, emotional concerns) at a health checkup?” and “How comfortable would you be talking to a doctor about each of the following (nutrition, sex, drugs and alcohol, emotional concerns)?”
To assess replication costs associated with the COTB intervention, we collected cost information on materials, labor, and refreshments. Average commercial lease rates for the study metropolitan areas were used to calculate costs related to facility usage.16 Utility costs were approximated on the basis of average costs per square foot for commercial buildings in the appropriate regions.17 Participant costs were attributed as the sum of incentives paid for session attendance and gift certificates awarded at study completion. Because they were study related and would not have been incurred otherwise, incentives paid for completion of the surveys were not included in the analyses described here. The “all urban consumers” version of the consumer price index was used in adjusting costs to 2001 dollars.18
Data Analysis
The effects of the intervention on study outcomes, measured at the 3-month follow-up survey, were estimated via logistic regression and ordinary least squares analyses. The independent variables included terms coded for participation in either the experimental condition or the control condition to assess the impact of the intervention. To adjust for non-equivalencies between the samples in the 2 study conditions and to further strengthen the power of our statistical tests focusing on intervention effects, we included the following covariates: baseline outcome, site (Harlem or PGC), and gender.
As a result of the gender differences that have been observed in patterns of health care seeking, and because male and female sessions were conducted separately, we estimated intervention effects among male and female participants separately. Since participants were assigned to the study and control conditions as groups rather than individuals, we used the robust variance estimator option available in Stata version 7.0 (Stata Corp, College Station, Tex) to adjust standard errors for non-independence of individuals within assignment groups.
RESULTS
At the 3-month follow-up, female intervention participants were significantly more likely than female control group participants to have made an appointment for a checkup (odds ratio [OR] = 3.04; 95% confidence interval [CI] = 1.81, 5.11; P < .001) and to have undergone a checkup (OR = 2.87; 95% CI = 1.39, 5.93; P = .004) (see Table 2 ▶). However, there were no differences between male participants in the intervention and control groups in regard to scheduling an appointment (OR = 0.84; 95% CI = 0.39, 1.81) or undergoing a checkup (OR = 0.74; 95% CI = 0.29, 1.89). Female participants in the intervention group were significantly more likely than female control participants to have spoken to friends or family members about the importance of undergoing a checkup (OR = 4.5; 95% CI = 2.25, 8.99; P < .001), but there were no differences between male intervention and control participants.
TABLE 2—
Results of Gender-Specific Logistic Regression Analyses of Behavioral Outcomes at 3-Month Follow-Up: Gonorrhea Community Action Project, 2000–2001
| Outcome | Baseline, % | 3-Month Follow-Up, % | Odds Ratioa (95% Confidence Interval) | P |
| Made appointment for checkupb | ||||
| Female | ||||
| Intervention (n = 95) | 30.5 | 50.5 | 3.04 | |
| Control (n = 51) | 39.2 | 25.5 | (1.81, 5.11) | <.001 |
| Male | ||||
| Intervention (n = 41) | 19.5 | 24.4 | 0.84 | .65 |
| Control (n = 25) | 24.0 | 28.0 | (0.39, 1.81) | |
| Underwent health checkup in past 3 monthsc | ||||
| Female | ||||
| Intervention (n = 88) | 35.2 | 63.6 | 2.87 | |
| Control (n = 45) | 48.9 | 44.4 | (1.39, 5.93) | .004 |
| Male | ||||
| Intervention (n = 41) | 26.8 | 39.0 | 0.74 | .53 |
| Control (n = 23) | 34.8 | 47.8 | (0.29, 1.89) | |
| Talked to friends/family about importance of undergoing health checkup | ||||
| Female | ||||
| Intervention (n = 94) | 35.1 | 73.4 | 4.50 | |
| Control (n = 52) | 44.2 | 46.2 | (2.25, 8.98) | <.001 |
| Male | ||||
| Intervention (n = 38) | 31.6 | 39.5 | 1.13 | |
| Control (n = 26) | 23.1 | 34.6 | (0.56, 2.28) | .73 |
aAdjusted for baseline score and site.
bNonequivalence at baseline between intervention and control groups significant at P < .1.
cNonequivalence at baseline between intervention and control groups significant at P < .05.
We conducted a multivariate analysis to assess the value of theoretically derived mediating variables in explaining immediate postintervention changes between the intervention and control groups (Table 3 ▶). Female intervention participants reported a greater increase in positive beliefs about undergoing a checkup than did female control participants (b=0.41, SE=0.10, P<.001). There were no differences between male intervention and control participants in regard to positive beliefs, nor were there differences in negative beliefs regarding undergoing a checkup among male or female participants in either condition. Female intervention participants exhibited a significant increase in positive attitudes toward undergoing a checkup relative to female control participants (b=0.47, SE=0.16, P=.007). There were no significant differences between male intervention and control participants in terms of positive attitudes.
TABLE 3—
Results of Gender-Specific Ordinary Least Squares Regression Analyses of Posttest Psychosocial Outcomes: Gonorrhea Community Action Project, 2000–2001
| Outcome | Baseline Mean (SD) | Posttest Mean (SD) | Unstandardized Coefficient (SE) | P |
| Positive beliefs about undergoing a health checkup at least once a year | ||||
| Female | ||||
| Intervention (n = 112) | 5.86 (.82) | 6.17 (.68) | ||
| Control (n = 63) | 5.84 (.91) | 5.74 (.83) | 0.41 (0.10) | <.001 |
| Male | ||||
| Intervention (n = 52) | 5.25 (.96) | 5.56 (1.0) | ||
| Control (n = 34) | 5.78 (.83) | 5.62 (.82) | 0.12 (0.10) | .24 |
| Negative beliefs about undergoing a health checkup at least once a year | ||||
| Female | ||||
| Intervention (n = 112) | 2.46 (.90) | 2.64 (1.1) | ||
| Control (n = 63) | 2.45 (1.0) | 2.47 (1.1) | 0.10 (0.20) | .61 |
| Male | ||||
| Intervention (n = 52) | 2.93 (1.1) | 3.30 (1.4) | ||
| Control (n = 34) | 2.60 (.82) | 2.77 (1.1) | 0.43 (0.35) | .26 |
| Attitudes toward undergoing a health checkup at least once a year | ||||
| Female | ||||
| Intervention (n = 111) | 5.64 (1.2) | 6.16 (.88) | ||
| Control (n = 63) | 6.02 (1.0) | 5.84 (.96) | 0.47 (0.16) | .01 |
| Male | ||||
| Intervention (n = 50) | 5.49 (1.2) | 5.37 (1.1) | ||
| Control (n = 34) | 5.56 (1.1) | 5.47 (1.3) | −0.07 (0.23) | .77 |
| Intentions regarding undergoing a health checkup at least once a year a | ||||
| Female | ||||
| Intervention (n = 112) | 5.77 (1.4) | 6.27 (1.1) | ||
| Control (n = 63) | 6.21 (1.0) | 6.06 (1.2) | 0.32 (0.18) | .10 |
| Male | ||||
| Intervention (n = 49) | 5.35 (1.6) | 5.51 (1.2) | ||
| Control (n = 34) | 5.94 (1.1) | 5.88 (1.3) | −0.37 (0.37) | .34 |
| Self-efficacy regarding undergoing a health checkup at least once a year | ||||
| Female | ||||
| Intervention (n = 111) | 5.86 (1.4) | 6.22 (.96) | ||
| Control (n = 63) | 6.23 (1.1) | 6.05 (1.4) | 0.20 (0.21) | .35 |
| Male | ||||
| Intervention (n = 50) | 5.71 (1.1) | 5.34 (1.3) | ||
| Control (n = 34) | 5.61 (1.4) | 5.82 (1.6) | −0.44 (0.35) | .23 |
| Appropriate to discuss sex with physician at health checkupb | ||||
| Female | ||||
| Intervention (n = 117) | 5.82 (1.5) | 6.14 (1.3) | ||
| Control (n = 62) | 5.94 (1.6) | 5.69 (1.8) | 0.53 (0.25) | .04 |
| Male | ||||
| Intervention (n = 51) | 5.60 (1.7) | 5.47 (1.4) | ||
| Control (n = 33) | 6.24 (1.3) | 5.70 (1.3) | −0.07 (0.27) | .80 |
| Comfortable talking with physician regarding sex | ||||
| Female | ||||
| Intervention (n = 117) | 4.85 (1.8) | 5.61 (1.7) | ||
| Control (n = 61) | 4.59 (2.1) | 4.75 (2.0) | 0.83 (0.28) | .01 |
| Male | ||||
| Intervention (n = 51) | 4.47 (2.1) | 4.88 (1.6) | ||
| Control (n = 33) | 5.76 (1.6) | 5.42 (1.5) | −0.17 (0.32) | .60 |
Note. Outcomes were assessed on scales ranging from 1 (negative) to 7 (positive). All regression equations were adjusted for baseline score and site.
aNonequivalence at baseline between intervention and control groups significant at P < .01.
bDifferential attrition between intervention and control groups significant at P < .1.
The intervention had no measurable effect on self-efficacy, social norms (data not shown), or intention to undergo a checkup. Female intervention participants were significantly more likely than female control participants to show an increase in regard to the perception that it is appropriate to discuss sexual issues with a physician during a health care visit (b = 0.53, SE = 0.25, P = .04). However, there were no differences between male intervention and control participants on this variable, nor were there differences between male and female participants in the intervention and control groups in regard to comfort in discussing sex with a doctor.
We conducted an additional analysis involving a Gender × Study Condition interaction term to formally assess the potential moderating effects of gender. Interaction terms between gender and the study condition variables were statistically significant in the case of (1) making an appointment in the past 3 months (OR=0.28; 95% CI=0.18, 0.66; P=.004), (2) undergoing a checkup in the past 3 months (OR=0.27; 95% CI=0.08, 0.90; P=.033); (3) talking to friends and family members about the importance of undergoing a checkup (OR=0.25; 95% CI=0.10, 0.67; P=.006) (data not shown), and (4) having positive beliefs regarding undergoing a checkup (b= −0.28, SE=0.13, P=.04).
DISCUSSION
Among adolescent and young adult women, participation in the COTB workshops was associated with increases in all 3 of the major outcomes examined—scheduling a checkup, undergoing a checkup, and talking with family and friends about the importance of checkups—along with attitudes and beliefs regarding undergoing a checkup and appropriateness of discussing sexual issues with a physician. In stark contrast, the COTB intervention had no discernible effect on male participants. Workshop facilitators noted that male adolescents took an active role in the workshop sessions and found the sessions enjoyable. However, feedback from session leaders revealed that although male participants did not perceive any particular barriers to accessing health care, nor did they perceive any benefits to doing so. A larger sample size may be needed to detect small effects such as those found here among the male participants; however, we found no effect on the mediating variables that would support such a claim.
While the intervention approach was effective in the case of the female participants, a different approach tailored to males seems a logical next step. Because Harlem is a community in which significant health disparities exist, especially among male residents, future interventions targeting male adolescents might focus on increasing the salience of interventions by raising awareness of these disparities and the potential benefits of preventive health care in reducing them.19 Future interventions should also consider a community-wide mass media approach targeting both adolescent and adult males to increase preventive health care seeking norms in these groups.
The success of this CBO-based intervention is important for several reasons. First, CBOs often interact with youths who may be at high risk for health problems. Second, there is increased potential for an intervention to be sustained when it is integrated into an agency’s ongoing programming schedule. Finally, COTB represents a “real-world” (i.e., relatively low cost, modest intensity) intervention that can be replicated in a variety of settings, including schools.
The availability of health services for members of the age group assessed here could influence the outcomes they experience in regard to seeking health care. Related to this fact, COTB provided information to intervention participants about the availability of low-and no-cost, adolescent-friendly health care services available in each community. However, it is interesting to note that, for the most part, participants in Harlem did not seek care at the suggested referral sites but sought care where they had previously done so.
Cost-Effectiveness
The average cost per participant was $305, including recruitment costs but excluding costs related to training recruiters and facilitators. This cost per participant was comparable to costs reported in 2 previous group HIV prevention interventions20,21; in comparison with COTB, these interventions consisted of more sessions (5 and 7, respectively) and involved higher per participant costs ($340 and $506, respectively). These estimates exclude costs associated with preintervention relationship building between members of the study staff and the community/CBO.
This study involved several limitations. First, there were baseline differences between female intervention and control participants in regard to previous health care seeking behaviors. At baseline, 53% of the female controls but only 34% of the female intervention participants reported having had a checkup within the previous 3 months. However, the higher proportion of controls who reported recent checkups did not appear to bias our findings greatly. In comparison with young women who had not reported a checkup at baseline (46%), those in both the control and intervention groups who reported having had a checkup at baseline were more likely to report having had one at the follow-up interview (74%). In addition, the intervention effect was somewhat stronger for participants who did not report a recent checkup (OR = 3.3; 95% CI = 1.17, 9.24) than for those who did (OR = 2.5; 95% CI = 0.75, 8.4).
A path analysis of mediating variables ruled out the alternative explanation that the increase in health care seeking among the intervention group participants was due to a propensity to seek health care and that the intervention cued them to seek it sooner. This analysis showed that the causal pathways linking COTB to behavioral change largely operated through beliefs regarding the benefits of seeking preventive health care, in turn creating a positive attitude toward undergoing a checkup. If there had been a propensity to seek care, we would not have expected to find significant differences between female intervention and control participants in regard to mediating variables related to the study outcomes.
The intervention had no direct effect on participants’ intentions to seek care. However, beliefs and attitudes had indirect effects on intentions. We found no intervention effect on self-efficacy despite the focus on skill building in the workshops, possibly because there were too few sessions and they were too brief.
Another limitation is that our findings are based on young people attending after-school programs and may not be representative of all adolescents residing in these communities. In addition, there was no external validation of participants’ self-reports. Finally, our findings could have been biased by participant attrition. Our analyses revealed higher rates of attrition among Latina participants and among participants enrolled in school. Although the potential for attrition bias did exist, we found no racial differences in previous health care seeking behaviors at baseline, and Latinas represented a relatively small percentage (12.3%) of the sample. One possibility is that the participants who were still in school were less likely to seek health care owing to time constraints or because they were still dependent on their parents.
Conclusion
Our study is noteworthy in that we employed a different approach to STD control by embedding this goal within a larger message about the importance of comprehensive preventive/reproductive health care among adolescents and young adults. Delays in this age group in regard to seeking care for STDs have been widely reported.22,23 COTB, by encouraging regular preventive health care visits that include STD screening, creates an expectation—and, potentially, a demand—for such screening, possibly increasing detection of asymptomatic STDs. This approach has the promise of increasing preventive health care seeking behaviors in adolescence that can carry over into adulthood.
Acknowledgments
This study was funded by the Centers for Disease Control and Prevention and the National Institute of Mental Health.
The authors would like to thank Deborah Levine, Sidney Moshette, and all of the members of the Gonorrhea Community Action Project Community Advisory Board in Harlem for their contributions to the intervention design and for the time, energy, and enthusiasm they brought to the study.
Human Participant Protection This study was approved by the institutional review boards of the Centers for Disease Control and Prevention; Columbia University; California State University, Long Beach; and the State of Maryland Department of Health and Mental Hygiene. Informed consent was obtained for participants 18 to 21 years old. Parental consent was obtained for participants younger than 18 years.
Peer Reviewed
Contributors N.L. VanDevanter designed the intervention curriculum and led the writing. P. Messeri led the study analyses. S.E. Middlestadt, C.R. Merzel, C.K. Malotte, M. Hogben, and R. Ledsky contributed to study design and implementation. A. Bleakley managed the project’s implementation and assisted with the study analyses. R.M. Cohall assisted in curriculum development and implementation. T.L. Gift helped write the article. J.S. St. Lawrence conceived the study and supervised all aspects of its implementation across all sites.
References
- 1.Sexually Transmitted Disease Surveillance 2001. Atlanta, Ga: Centers for Disease Control and Prevention; 2002.
- 2.Prevention and Women’s Health: A Shared Responsibility. New York, NY: Commonwealth Fund; 1996.
- 3.Britto MT, Klostermann BK, Bonny AE, Altum SA, Hornung RW. Impact of a school-based intervention on access to healthcare for underserved youth. J Adolesc Health. 2001;29:116–124. [DOI] [PubMed] [Google Scholar]
- 4.Braverman PK. Sexually transmitted diseases in adolescents. Adolesc Med. 2000;84:869–889. [DOI] [PubMed] [Google Scholar]
- 5.Irwin C, Millstein S. Biopsychosocial correlates of risk taking behaviors during adolescence. J Adolesc Health. 1992;13:162–170. [PubMed] [Google Scholar]
- 6.Klein JD, Slap GB, Elster AB, Schonberg SK. Access to health care for adolescents. J Adolesc Health. 1992;3:162–170. [DOI] [PubMed] [Google Scholar]
- 7.Klein JD, Wilson KM, McNulty M, Kapphahn C, Collins KS. Access to medical care for adolescents: results from the 1997 Commonwealth Fund survey of the health of adolescent girls. J Adolesc Health. 1999; 25:120–130. [DOI] [PubMed] [Google Scholar]
- 8.Newacheck PW, Brindis CD, Cart CU, Marchi K, Irwin CE. Adolescent health insurance coverage: recent changes and access to care. Pediatrics. 1999;104:195–202. [DOI] [PubMed] [Google Scholar]
- 9.Samet JH, Winter MR, Grant L, Hingson R. Factors associated with HIV testing among sexually active adolescents: Massachusetts survey. Pediatrics. 1997; 100:371–377. [DOI] [PubMed] [Google Scholar]
- 10.Yu SM, Bellamy HA, Schwalberg RH, Drum MA. Factors associated with use of preventive dental and health services among US adolescents. J Adolesc Health. 2001;29:395–405. [DOI] [PubMed] [Google Scholar]
- 11.Lafferty WE, Downey L, Shields AW, Holan CM, Lind A. Adolescent enrollees in Medicaid managed care: the provision of well care and sexual health assessment. J Adolesc Health. 2000;28:497–508. [DOI] [PubMed] [Google Scholar]
- 12.Guidelines for Adolescent Preventive Services. Chicago, Ill: American Medical Association; 1992.
- 13.Fishbein M, Ajzen I. Beliefs, Attitudes, Intentions, and Behavior: An Introduction to Theory and Research. Reading, Mass: Addison-Wesley; 1975.
- 14.Chinman MJ, Linney JA. Toward a model of adolescent empowerment: theoretical and empirical evidence. J Primary Prev. 1998;18:393–413. [Google Scholar]
- 15.Hogben M, Ledsky R, Middlestadt S, et al. Psychological mediating factors in an intervention to promote adolescent health care–seeking. Psychol Health Med. In press.
- 16.CoStar Group. Market trends. Available at: http://www.costar.com/trends. Accessed May 5, 2002.
- 17.Statistical Abstract of the United States. Washington, DC: US Bureau of the Census; 2001.
- 18.Bureau of Labor Statistics. Consumer price index—all urban consumers. Available at: http://www.bls.gov/cpihome.htm. Accessed May 5, 2002.
- 19.Fullilove RE, Fullilove MT, Northridge ME, et al. Risk factors for excess mortality in Harlem: findings from the Harlem Household Survey. Am J Prev Med. 1999;16:22–28. [DOI] [PubMed] [Google Scholar]
- 20.Holtgrave DR, Kelly JA. Preventing HIV/AIDS among high-risk urban women: the cost-effectiveness of a behavioral group intervention. Am J Public Health. 1996;86:1442–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pinkerton SD, Holtgrave DR, Johnson-Masotti AP, et al. Cost-effectiveness of the NIMH multisite HIV prevention intervention. AIDS Behav. 2002;6:83–96. [Google Scholar]
- 22.Fortenberry JD. Health care seeking behaviors related to sexually transmitted diseases among adolescents. Am J Public Health. 1997;87:417–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Institute of Medicine. The Hidden Epidemic: Confronting Sexually Transmitted Diseases. Washington, DC: National Academy Press; 1997.