As we look to advance the public’s health and eliminate health disparities through programs and policies, one issue that surfaces repeatedly is which racial/ethnic group we should focus on. One group that calls for attention is the Hispanic population. The Hispanic population, the fastest growing subgroup of the US population, is heterogeneous and comprises people from at least 25 countries with the Spanish language as the common identifier. As of 2002, there were 37.4 million Hispanics in the United States, representing 13.3% of the total mainland population.1 Mexican Americans represent 66.9% of the total Hispanic population, followed by Central and South Americans (14.3%), Puerto Ricans (8.6%), Cubans (3.7%), and other Hispanics (6.5%). Compared with Whites, Hispanics are younger, have a lower proportion of people aged 25 years and older with at least a high school diploma, are more likely to be unemployed, are less likely to earn $35000 or more, are more likely to live in poverty, and are less likely to have health insurance.1,2
Figure 2.
Rufina Tinoco, 59, does not have health insurance and would have gone blind from glaucoma had not the Open Door Health Center in Florida found an eye surgeon willing to operate on her for free. (IPNSTOCK/Ed Kashi)
There is significant variability among Hispanic subgroups. Mexican Americans are the youngest, the least educated, and the least likely to have health insurance, while Puerto Ricans are the least likely to be uninsured but have the highest proportion of unemployed people and are the most likely to live below poverty level. Cubans are the oldest, the most educated, and the least likely to be unemployed, while Central and South Americans are the least likely to live below poverty level. Finally, compared with non-Hispanic Whites, Puerto Ricans fare similar to or worse than non-Hispanic Blacks with regard to income, education, unemployment status, and poverty.
LOOKING BEYOND THE HISPANIC PARADOX
Despite their low socioeconomic position and lack of health insurance coverage, Hispanics as a group are often omitted from the health disparities discourse because they are believed to fare similar to if not better than non-Hispanic Whites with regard to mortality outcomes. This similarity to non-Hispanic Whites often shifts attention to the dichotomy of non-Hispanic White and Black. However, recent studies provide evidence to counter the so-called Hispanic health advantage or Hispanic paradox.3–5 These studies suggest that the Hispanic paradox, which might be attributed to a healthy migrant effect, healthy behaviors, cultural traditions, or some combination of these, does not apply to all Hispanic subgroups. In fact, the paradox is relevant only to recent foreign-born Mexican immigrants.3
For example, although Hispanics as a group have lower age-adjusted all-cause death rates per 100 000 (629.3) than non-Hispanics (856.5), variability across Hispanic subgroups is usually ignored and data are presented on the group as a whole.6 Puerto Ricans have higher age-adjusted all-cause death rates per 100 000 (766.2) than Mexican Americans (612.8), Cubans (524.1) and other Hispanics (761.8). The heterogeneity among Hispanic subgroups in terms of sociodemographic and health status is often lost owing to data aggregation. Therefore, to move forward our efforts to eliminate health disparities, the health of Hispanics deserves a look beyond the paradox. It is essential to explore the complexities of the sociodemographic dynamics operating within the different Hispanic subgroups and how these dynamics interact with social relationships in the United States to influence the life chances, health, and well-being of Hispanics.
IMPLICATIONS OF RACIAL IDENTITY FOR HEALTH AND WELL-BEING
Although race and ethnicity are used interchangeably, they have different meanings. In the case of Hispanics, for example, ethnicity refers to the array of values, cultural norms, and behaviors the different subgroups share. In contrast, race represents categorization of individuals on the basis of skin color, both by self-identification and by the eye of the beholder. Thus, given the heterogeneity of Hispanics, we have individuals fitting the White or Black racial taxonomy as defined by the individual’s perception and reinforced by society.
Although evidence suggests that the majority of Hispanics do not identify with the existing Year 2000 US Census racial categories,7–9 they were nonetheless asked to choose the best fit among the existing racial categories in the decennial census. (During the 2000 Census, 47.9% of Hispanics indicated they were White, 2% reported they were Black, 42.2% chose the “Some Other Race” category,” 1.2% said they were American Indian, and less than 1% said they were Asian, Native Hawaiian, or Other Pacific Islander.) It is possible that categorizing Hispanics into the US Census racial categories channels them toward or away from opportunities and resources that may influence their life chances and, further, their health status. Thus, categorizing Hispanics within the racial categories Black or White could confer on them social-patterned experiences and exposures similar to those of non-Hispanic Blacks, thus affecting their health negatively and leading to disease, disability, and death. This could well be true for Puerto Ricans and Dominicans, Hispanic subgroups with strong African ancestry who are more likely to be identified as Black in everyday life in US society. Interestingly, disaggregate data show that Puerto Ricans exhibited the worst health profiles among Hispanics. Similarly, among Mexican Americans, those with dark skin or American Indian physical appearance are more likely to be discriminated against, receive less education, and hold occupations with lower prestige than their counterparts with lighter skin or a more European appearance.10
Moreover, racial categorization among Hispanics could depend on nativity status (US- vs foreign-born), length of stay in the United States, and language spoken. Hispanics who were born in the United States and those who were born outside the United States but who have been in the United States for a long time and who have a good command of the English language could be more likely to categorize themselves into the US racial categories because of their acculturation or assimilation into the mainstream society. Therefore, the idealized health advantage or so-called Hispanic paradox for certain health outcomes and mortality could be related to their racial categorization and the opportunities attached to race in our society.
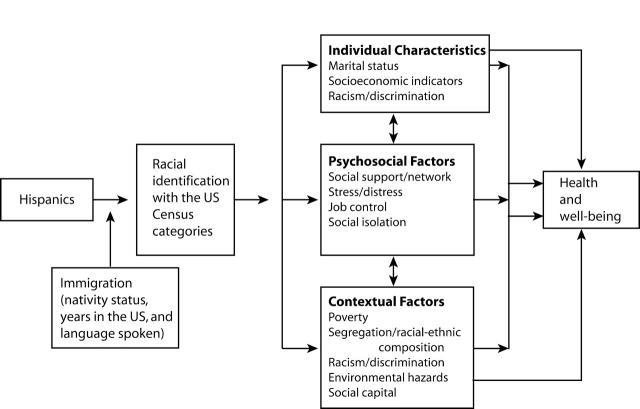
Figure 1 ▶ was developed as a conceptual framework to aid in understanding the effect of race on Hispanics and its implications for health and well-being. This model includes 3 domains: individual, psychosocial, and contextual-level characteristics. It postulates that Hispanics, although they do not favor the category options they are given, nevertheless categorize themselves into the US Census categories (Black, White, or Some Other Race) on the basis of their perception of how US society sees and identifies them9; however, this categorization will depend on their generation in the United States, nativity status, years in the United States, and language spoken. This racial categorization will channel Hispanics toward different opportunities and disadvantages at the personal, psychosocial, and contextual levels. For example, one’s categorization as Black or White will determine where one lives and one’s access to or lack of opportunities that may lead to health or disease.
FIGURE 1—
Framework for the effect of racial identity among Hispanics on health and well-being
At the contextual level, these characteristics will combine or interact with the social structures (e.g., segregation, educational equity or lack thereof owing to the quality of the schools, housing structures and environmental exposure, racism and discrimination) to influence one’s health and well-being. Thus, conditions at the individual and contextual levels will have effects on each other and will further interact, alone or in combination, with individual psychosocial status (e.g., social support, stress, social isolation). This process is not static but dynamic and can follow a life-course pattern of accumulated negative exposures that can be passed on through generations. For example, Hispanic Blacks would most likely reside in segregated areas with non-Hispanic Blacks or other Hispanic Blacks. In this setting, a Hispanic Black individual would be exposed to an array of risks and disadvantages, such as low quality of education, high level of unemployment, and greater possibility of exposure to environmental hazards. This could lead to the same health consequences faced by non-Hispanic Blacks. Therefore, racial categorization could be a significant predictor of health status and well-being.
A NEW LOOK AT HISPANICS’ HEALTH
For the past 20 years the discourse regarding Hispanic health has focused on the fact that Hispanics as a group have lower mortality outcomes than non-Hispanic Whites regardless of their low socioeconomic position and access to care. This finding, often referred to as an epidemiological or Hispanic paradox, does not apply to all Hispanic subgroups and therefore is spurious and misleading. It is evident that Hispanics are heterogeneous not only in health and mortality outcomes but also in sociodemographic characteristics. Racial categorization and its consequences for Hispanics deserve attention, especially now, since the US Census Bureau is proposing to eliminate the “Some Other Race” category for the 2010 US Census. This proposal, if approved, will force people to choose between the categories given, reinforcing social stratification. Therefore, to develop effective programs and policies to advance understanding of the health of this fastest growing segment of the population, we will need to look beyond Hispanics as a monolithic group and focus instead on the racial composition of the Hispanic group and the advantages and disadvantages associated with race in our society. This shift will not only contribute to a better understanding of the health of Hispanics but also will help to disentangle the role of race in the elimination of health disparities in the United States.
Acknowledgments
This work was supported by the National Institute of Dental and Craniofacial Research (grant K22DE15317) and by the Robert Wood Johnson Foundation Health and Society Scholars Program.
References
- 1.Ramirez R, De la Cruz GP. The Hispanic Population in the United States. Washington, DC: US Census Bureau; 2002. Current Population Reports, P20-545.
- 2.Freid VM, Prager K, Mackay AP, Xia H. Chartbook on Trends in the Health of Americans. Health, United States, 2003. Hyattsville, Md: National Center for Health Statistics; 2003.
- 3.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41(3): 385–415. [DOI] [PubMed] [Google Scholar]
- 4.Hunt KJ, Williams K, Resendez RG, Hazuda HP, Haffner SM, Stern MP. All-cause and cardiovascular mortality among diabetic participants in the San Antonio Heart Study: evidence against the “Hispanic Paradox.” Diabetes Care. 2002;25(9):1557–1563. [DOI] [PubMed] [Google Scholar]
- 5.Patel KV, Eschbach K, Ray LA, Markides KS. Evaluation of mortality data for older Mexican Americans: implications for the Hispanic paradox. Am J Epidemiol. 2004;159(7):707–715. [DOI] [PubMed] [Google Scholar]
- 6.Kochaneck KD, Murphy SL, Anderson RN. Deaths: final data for 2002. Natl Vital Stat Rep. October 12, 2004:53(5). [PubMed]
- 7.Rodriguez CE. Changing Race: Latinos, the Census, and the History of Ethnicity in the United States. New York, NY: New York University Press; 2000.
- 8.Rodriguez CE. Puerto Ricans: between black and white. New York Aff. 1974;1(4):92–101. [Google Scholar]
- 9.Rodriguez CE, Castro A, Garcia O, Torres A. Latino racial identity: in the eye of the beholder. Latino Stud J. 1991;2(3):33–48. [Google Scholar]
- 10.Arce CH, Murguia E, Frisbie WP. Phenotype and life chances among Chicanos. Hispanic J Behav Sci. 1987;9(1): 19–32. [Google Scholar]