Abstract
Objectives. I studied the extent to which maternal deaths are underreported on death certificates.
Methods. We collected data on maternal deaths from death certificates, linkage of death certificates with birth and fetal death records, and review of medical examiner records.
Results. Thirty-eight percent of maternal deaths were unreported on death certificates. Half or more deaths were unreported for women who were undelivered at the time of death, experienced a fetal death or therapeutic abortion, died more than a week after delivery, or died as a result of a cardiovascular disorder.
Conclusions. The number of maternal deaths is substantially underestimated when death certificates alone are used to identify deaths, and it is unlikely that the Healthy People 2010 objective of reducing the maternal mortality rate to no more than 3.3 deaths per 100000 live births by 2010 can be achieved. Increasing numbers of births to older women and multiple-gestation pregnancies are likely to complicate efforts to reduce maternal mortality.
The magnitude of the problem of maternal mortality is underestimated when mortality rates are based only on maternal deaths reported on death certificates. Studies have shown that physicians completing death certificates after a maternal death fail to report that the woman was pregnant or had a recent pregnancy in 50% or more of these cases.1–3 Because a history of pregnancy must be recorded on a death certificate for a death to be coded as resulting from a maternal cause, these deaths are not included in the calculation of maternal mortality rates. This leads to an underestimation of the problem of maternal mortality on both the state and national levels because death certificate data collected by states are used to compute maternal mortality rates for the nation.
Previous research has shown that the completeness of reporting of deaths related to pregnancy can be improved by linking death records of women of reproductive ages with birth and fetal death records2,4–6 and through the use of a check box on the death certificate to indicate that a decedent was pregnant at the time of death or had recently been pregnant.7 Other studies have shown that review of medical examiner records is successful in identifying deaths that were not ascertained through other sources, particularly those among women who were pregnant at the time of death.8,9 Studies that have used medical examiner records to study pregnancy mortality have focused on pregnancy-associated deaths, defined as deaths from any cause during pregnancy or within 1 calendar year of delivery or pregnancy termination.10 Because maternal deaths, as defined below, are a subset of pregnancy-associated deaths, review of medical examiner records to identify maternal deaths should also improve the completeness of maternal death reporting.
The purpose of this study was to determine the extent to which maternal deaths are un-derreported on death certificates by using both linkage of records and review of medical examiner records to identify unreported maternal deaths. The overall undercount of maternal deaths was estimated, sources of identification of deaths were reported, and the degree of underreporting among subgroups of the population was described.
METHODS
The World Health Organization (WHO) definition of a maternal death was used to identify deaths for inclusion in this study because this is the definition used by the National Center for Health Statistics (NCHS) to compile national maternal mortality statistics. WHO defines a maternal death as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.”11 This definition includes deaths assigned to the cause “complication of pregnancy, childbirth and the puerperium” (International Classification of Diseases, Ninth Revision [ICD-9] codes 630–67611 and Tenth Revision [ICD-10] codes O00–O95, O98–O99, and A34).12
Data were collected from 3 sources: (1) review of death certificates to identify those records on which a complication of pregnancy, childbirth, or the puerperium was listed as an underlying or contributing cause of death; (2) linkage of death certificates of reproductive-age women with live birth and fetal death records to identify a delivery within 42 days of death; and (3) review of medical examiner records for evidence that a woman was pregnant at the time of death or experienced a recent pregnancy. Data were collected for all maternal deaths occurring during the years 1993 through 2000.
Vital records data were obtained from the Vital Statistics Administration of the Maryland Department of Health and Mental Hygiene. Death records were identified by searching for records on which a complication of pregnancy, childbirth, or the puerperium was listed as an underlying or contributing cause of death. For the years 1993 through 1998, this included all deaths with ICD-9 codes 630 through 676. Because Maryland and the remainder of states began using ICD-10 codes beginning with 1999 mortality data,13 all deaths with ICD-10 codes O00 to O95, O98 to O99, or A34 were included for the years 1999 and 2000.
Changes were made in the classification of maternal deaths between ICD-9 and ICD-10. ICD-9 classified a death as having a maternal cause only if pregnancy was reported as part of the sequence of events leading to death. These deaths are classified as maternal in ICD-10 as well. However, the coding rules for ICD-10, unlike the rules for ICD-9, classify deaths aggravated by pregnancy as maternal deaths. This includes deaths from previously existing diseases and deaths from nonobstetric conditions that developed during pregnancy and were aggravated by physiological effects of pregnancy.13 To account for this discontinuity in the rules for classifying deaths as having a maternal cause, records for all deaths occurring before 1999 were recoded using ICD-10 rules. The study group therefore includes 16 deaths occurring between 1993 and 1998 that would not have been classified as maternal deaths using ICD-9 rules. Late maternal deaths (deaths occurring 43 days through 1 year after termination of pregnancy) were not included in the study group.
Identification of maternal deaths through linkage of vital records was performed by matching death certificates for all women of reproductive age against live birth and fetal death records to identify pregnancies occurring within 42 days of death. Records were linked by matching either the mother’s social security number or the mother’s name and date of birth on the death record with corresponding information on live birth and fetal death records. All linked records were manually reviewed to ensure accurate matching.
Medical examiner records were reviewed for all women aged 10 through 50 years who died between 1993 and 2000. Death certificates were obtained for all women for whom medical examiner records identified an undelivered or recent pregnancy.
All death certificates that were identified through linkage of records or review of medical examiner records were reviewed by a team of 3 board-certified obstetrician-gynecologists and 2 trained nosologists to determine the underlying cause of death that would have been assigned if a history of pregnancy had been reported on the death certificate. All records meeting the WHO definition of a maternal death were included in the study population.
The distribution of maternal deaths identified through death records alone, and deaths identified from all sources, were compared by outcome of pregnancy, time of death, cause of death, maternal race, age, education and marital status, parity, and plurality.
RESULTS
A total of 129 maternal deaths occurring between 1993 and 2000 were identified from the 3 data sources. Only 80 of these deaths (62.0%) were identified through cause-of-death information obtained from death records (Figure 1 ▶). Inclusion of all 129 identified maternal deaths resulted in a maternal mortality rate of 22.2 per 100 000 live births for the years 1993 through 2000, substantially higher than the rate of 13.8 per 100 000 live births based on information reported on death records alone.
FIGURE 1—
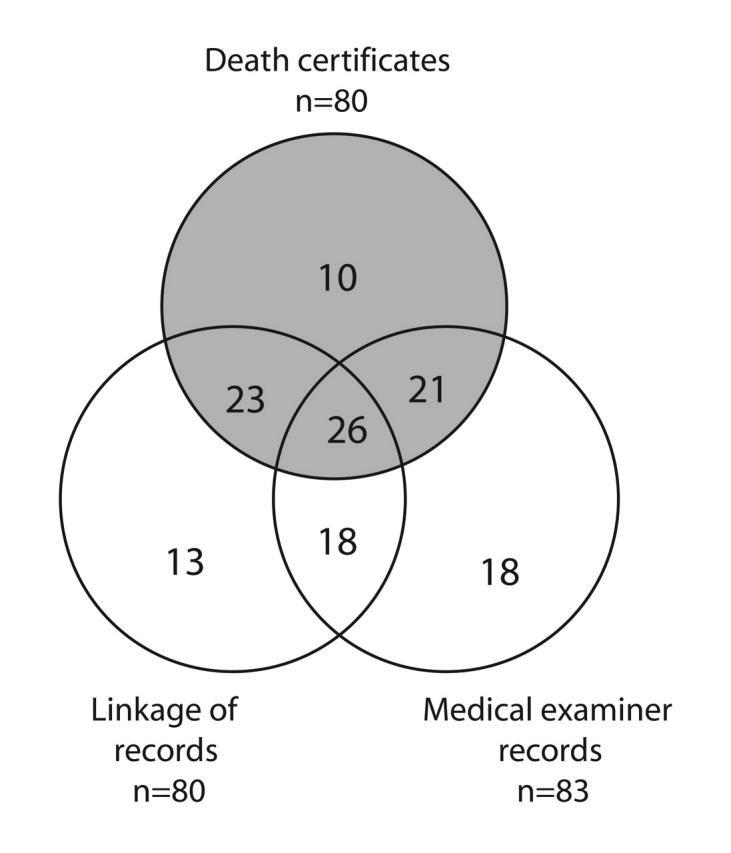
Number of maternal deaths, by source of identification, Maryland, 1993–2000. Note. The gray area highlights the number of maternal deaths that were identified through death records. The nonshaded areas show the cases that were missed.
A similar number of maternal deaths were identified from each of the 3 data sources (Figure 1 ▶). Eighty deaths (62.0%) were identified through death records, 80 (62.0%) through linkage of records, and 83 (64.3%) through review of medical examiner records (Figure 1 ▶). Although most deaths were identified through more than 1 source, 41 deaths (31.8%) were identified through only a single data source. These included 10 deaths (7.8%) identified through death records, 13 deaths (10.1%) identified through linkage of records, and 18 deaths (14.0%) identified through review of medical examiner records.
The number of maternal deaths following a live birth increased from 50 to 80 and the number of deaths following a fetal death increased from 4 to 8 when multiple data sources were used to identify maternal deaths. Death records identified all 8 deaths that occurred as a result of an ectopic pregnancy and the single death that occurred as a result of a molar pregnancy but neither of the 2 deaths that followed a therapeutic abortion. Death records identified only 10 of the remaining 23 deaths among women who were pregnant at the time of death (Table 1 ▶).
TABLE 1—
Number of Maternal Deaths, by Source of Identification, Outcome of Pregnancy, Time of Death, and Cause of Death: Maryland, 1993–2000
| Source of Identification | |||
| Death Records | All Sourcesa | Maternal Deaths Unreported on Death Records (%) | |
| Total deaths | 80 | 129 | 38.0 |
| Outcome of pregnancy | |||
| Live birth | 50 | 80 | 37.5 |
| Fetal death | 4 | 8 | 50.0 |
| Therapeutic abortion | 0 | 2 | 100.0 |
| Ectopic pregnancy | 8 | 8 | 0.0 |
| Molar pregnancy | 1 | 1 | 0.0 |
| All other undelivered | 10 | 23 | 56.5 |
| Unknown | 7 | 7 | 0.0 |
| Days from delivery to death | |||
| Undelivered | 16 | 28b | 42.9 |
| 0–1 day | 22 | 28 | 21.4 |
| 2–7 days | 18 | 24 | 25.0 |
| 8–14 days | 8 | 16 | 50.0 |
| 15–21 days | 3 | 8 | 62.5 |
| 22–30 days | 3 | 7 | 57.1 |
| 31–42 days | 2 | 8 | 75.0 |
| Unknown | 9 | 10 | 10.0 |
| Cause of death | |||
| Cardiovascular disordersc | 17 | 39 | 56.4 |
| Embolism | 15 | 24 | 37.5 |
| Hemorrhage | 15 | 17 | 11.8 |
| Hypertensive disorders | 15 | 19 | 21.1 |
| Infection | 5 | 8 | 37.5 |
| Other | 13 | 22 | 40.9 |
aIncludes death records, linkage of records, and medical examiner records.
bIncludes 5 deaths resulting from ectopic pregnancies, 1 death resulting from a molar pregnancy, and 22 deaths among other women who were undelivered at the time of death.
cIncludes cardiomyopathy, congenital heart disease, pulmonary hypertension, endocarditis, valvular dysfunction, and other cardiac conditions related to or aggravated by pregnancy.
Among women who were no longer pregnant at the time of death, the percentage of unreported deaths increased with the length of time between delivery or pregnancy termination and death. Six of 28 deaths (21.4%) occurring within 1 day of delivery or pregnancy termination and 6 of 24 deaths (25.0%) occurring 2 through 7 days after delivery were not reported on death records. The percentage of unreported maternal deaths rose to 75.0% for deaths occurring 31 to 42 days after delivery or termination. Twelve of the 28 deaths (42.8%) that occurred among women who were pregnant at the time of death were not reported on death records. This figure included 5 deaths resulting from ectopic pregnancies, 1 death resulting from a molar pregnancy, and 22 deaths among other women who were undelivered at the time of death.
Deaths were underreported on death records for all leading causes of maternal death. The percentage of unreported deaths was highest for cardiovascular disorders (56.4%), followed by embolism and infection (37.5% each), hypertensive disorders of pregnancy (21.1%), and hemorrhage (11.8%).
On the basis of information reported on death certificates, it appeared that cardiovascular disorders, embolism, hemorrhage, and hypertensive disorders of pregnancy were each responsible for a similar proportion of maternal deaths. However, when previously unreported deaths were included, cardiovascular disorders were clearly the leading cause of maternal death, responsible for 39 of 129 deaths (30.2%). Embolism, the second leading cause of death, was responsible for 18.6% of deaths, whereas hypertensive disorders of pregnancy, the third leading cause, were responsible for 14.7% of deaths.
Maternal deaths were underreported for all categories of maternal race, age, education, marital status, parity, and plurality (Table 2 ▶). The percentage of unreported deaths was particularly high for women at the extremes of the maternal age distribution; half of all maternal deaths among teenagers and more than half of all maternal deaths among women aged 40 and above were unreported.
TABLE 2—
Number of Maternal Deaths, by Source of Identification and Selected Maternal and Pregnancy Characteristics: Maryland, 1993–2000
| Source of Identification | |||
| Maternal and Pregnancy Characteristics | Death Records | All Sourcesa | Maternal Deaths Unreported on Death Records (%) |
| Maternal race | |||
| White | 37 | 60 | 38.3 |
| African American | 42 | 67 | 37.3 |
| All other races | 1 | 2 | 50.0 |
| Maternal age, y | |||
| < 20 | 5 | 10 | 50.0 |
| 20–24 | 12 | 19 | 36.8 |
| 25–29 | 16 | 28 | 42.9 |
| 30–34 | 23 | 37 | 37.8 |
| 35–39 | 19 | 23 | 17.4 |
| > 39 | 5 | 12 | 58.3 |
| Maternal education (aged ≥20 y)b | |||
| < 12 y | 10 | 15 | 33.3 |
| 12 y | 29 | 52 | 44.2 |
| Some college | 13 | 21 | 38.1 |
| College graduate/graduate school | 16 | 23 | 30.4 |
| Marital status | |||
| Married | 37 | 58 | 36.2 |
| Unmarried | 43 | 70 | 38.6 |
| Not stated | 0 | 1 | … |
| Live birth order | |||
| 1st child | 20 | 30 | 33.3 |
| 2nd child | 15 | 25 | 40.0 |
| 3rd child | 8 | 15 | 46.7 |
| 4th child and over | 8 | 14 | 42.9 |
| Not stated | 29 | 45 | … |
| Pluralityc | |||
| Singleton | 53 | 87 | 39.1 |
| Twin or multiple | 4 | 7 | 42.9 |
| Unknown | 23 | 35 | … |
aIncludes deaths identified from death records, record linkage, and review of medical examiner records.
bFigures include data for women aged 20 years and older because younger women may not have completed their education at the time of death.
cNumber of fetuses in a pregnancy.
DISCUSSION
Today, maternal deaths are relatively rare events in developed countries. Nevertheless, maternal deaths still occur, frequently among young, apparently healthy women, and they have a devastating impact on the families left behind. Furthermore, for each woman who dies, many more experience life-threatening and often long-lasting complications.14
This study supports the findings of earlier studies that have shown that the number of maternal deaths is substantially underestimated when death certificates alone are used to identify deaths. In Maryland, collection of maternal death data from multiple sources showed that the maternal mortality rate in Maryland for the years 1993 through 2000 was 22.2 per 100000 live births, 60.9% higher than the rate of 13.8 per 100000 based only on information reported on death records. If maternal deaths are assumed to be underreported at the same level nationally as they are in Maryland, the maternal mortality rate for the United States for the year 2001 would have been 15.9 per 100000 live births, substantially higher than the reported figure of 9.9 per 100000.15 Because it is possible that not all maternal deaths were identified in this study even by using additional data sources, the adjusted rates of 15.9 per 100000 for the nation and 22.2 per 100000 for Maryland may also be underestimates of the true figures.
It is unlikely that the Healthy People 2010 objective of reducing the maternal mortality rate to no more than 3.3 deaths per 100 000 live births by 201016 can be achieved, especially because the number of women in 2 groups at increased risk of maternal death—women of advanced maternal age and women with multiple-gestation pregnancies—has been increasing. Between 1990 and 2001, the US birth rate increased by 47% for women aged 40 to 44 and tripled for women aged 45 to 49, whereas the twin birth rate increased by 33% and the rate of triplet and higher order births rose by nearly 300%.17 Both the increase in births among older women and the increase in multiple-gestation pregnancies are attributable in large part to the increased use of fertility-enhancing therapies. Data compiled in the current study showed that the maternal mortality rate for women aged 40 years and older was 84.5 per 100 000 live births, more than 4 times higher than the rate of 20.7 per 100 000 for all younger women. The maternal mortality rate for women experiencing multiple-gestation pregnancies was 38.5 per 100 000, more than double the rate of 15.5 per 100 000 for women with known singleton pregnancies. However, the true gap between maternal mortality rates for women with singleton and multiple-gestation pregnancies is not as large as these figures would suggest because most of the 35 pregnancies of unknown plurality were likely to have been singleton pregnancies. Nevertheless, even if all pregnancies of unknown plurality are assumed to have been singleton pregnancies, the recalculated maternal mortality rate of 21.4 per 100 000 for women with singleton pregnancies would remain substantially lower than the rate for women with multiple-gestation pregnancies. Although several studies based on international data have also shown that multiple gestation increases maternal mortality,18–20 this association has not previously been shown using US data. Additional study using US data is needed to further explore the association between multiple gestation and maternal mortality because the increasing number of multiple births is likely to complicate efforts to reduce maternal mortality.
The findings of this report show that cardiovascular disorders, which include conditions such as cardiomyopathy, congenital heart disease, pulmonary hypertension, endocarditis, valvular dysfunction, and other cardiac conditions related to or aggravated by pregnancy, are the leading cause of maternal death in Maryland. This is in contrast to national death data compiled by the NCHS, which show the leading causes of maternal death to be hypertensive disorders of pregnancy, hemorrhage, and embolism.15 The Centers for Disease Control and Prevention’s Pregnancy-Related Mortality Surveillance System (PMSS), which compiles national data on pregnancy-related deaths, has historically identified the same 3 leading causes of death.21–23 The PMSS data on pregnancy-related deaths, which are defined as all deaths causally related to pregnancy, are based largely on death certificate data provided by state vital records offices. It is likely that cardiovascular disorders have not been identified as a leading cause of maternal death in either NCHS or PMSS data because death records of women dying as a result of this cause frequently do not indicate that they were pregnant or had recently been pregnant. Fewer than half of all deaths resulting from cardiovascular disorders were identified from death records in the present study.
It is critical that physicians who care for pregnant woman are aware that a pregnant patient or a patient who has recently given birth is more likely to die as a result of a cardiovascular disorder than from any other cause. Cardiovascular disorders may be of particular concern for adolescents; this cause was responsible for 6 of the 10 deaths among 14- to 19-year-olds in this study.
This study has also shown that a larger proportion of maternal deaths occur among undelivered women than previously reported. Although deaths resulting from an ectopic or molar pregnancy were well-reported on Maryland death certificates, more than half of the deaths that occurred among other undelivered women were unreported. Deaths among this subgroup of undelivered women represented 19.3% of all maternal deaths for which the time of death was known, compared with a figure of 11.7% in a recent PMSS report.24
The lack of complete reporting of maternal deaths has led to misconceptions regarding the magnitude of the problem of maternal deaths, the leading cause of death, and the timing of maternal deaths. Death records are an important source of data on pregnancy mortality, but death records alone identify only a fraction of all maternal deaths. New York City and 17 states have attempted to improve ascertainment of pregnancy on death records by including a pregnancy check box or asking about pregnancy status on their death records. In Maryland, questions about pregnancy status in the 12 months preceding death, the outcome of pregnancy, and the date of delivery were added to the Certificate of Death in 2001. The NCHS has recommended use of a single pregnancy question by all states on the revised US Standard Certificate of Death, but it is likely to be a number of years before all states begin using the revised certificate. Currently, comprehensive identification of maternal deaths can be accomplished only by collecting information from multiple data sources. Both data linkage and review of medical examiner records contributed substantially to identification of maternal deaths in Maryland. Linkage of records identified 13 deaths that were not identified through death records or review of medical examiner records. Review of medical examiner records identified 18 deaths that could not be identified through death records or linkage of records, including 56% of all deaths among women who were undelivered at the time of death, 21% of embolism deaths, 18% of cardiovascular deaths, and both deaths that followed therapeutic abortions. Review of paper copies of medical examiner records to identify maternal deaths can be a labor-intensive process. Fortunately, medical examiner records are increasingly becoming computerized, which will make the identification of women who were pregnant at the time of death or were recently pregnant a far less time-consuming process. We hope that this will encourage the use of medical examiner records for routine surveillance of deaths related to pregnancy.
Comprehensive identification of maternal deaths is necessary to determine the magnitude of maternal mortality, identify the major causes of death, and identify groups at increased risk of death. Without a clear understanding of these factors, it is not possible to develop comprehensive strategies to prevent this devastating pregnancy outcome.
Acknowledgments
The author gratefully acknowledges Dr Diana Cheng for her guidance, support, and thoughtful review of this article, and Dr Robert Hayman for assistance with linkage of data.
Human Participant Protection No protocol approval was needed for this study.
Peer Reviewed
References
- 1.Dye TD, Gordon H, Held B, Tolliver NJ, Holmes AP. Retrospective maternal mortality case ascertainment in West Virginia, 1985 to 1989. Am J Obstet Gynecol. 1992;167:72–76. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Pregnancy-related mortality: Georgia, 1990–1992. MMWR Morb Mortal Wkly Rep. 1995;44:93–96. [PubMed] [Google Scholar]
- 3.Atrash HK, Alexander S, Berg CJ. Maternal mortality in developed countries: not just a concern of the past. Obstet Gynecol. 1995;86:700–705. [DOI] [PubMed] [Google Scholar]
- 4.Starzyk P, Frost F, Kobayashi JM. Misclassification of maternal deaths: Washington State. MMWR Morb Mortal Wkly Rep. 1986;35:621–623. [PubMed] [Google Scholar]
- 5.Jocums SB, Berg CJ, Entman SS, Mitchell EF. Post-delivery mortality in Tennessee, 1989–91. Obstet Gynecol. 1998;91:767–770. [DOI] [PubMed] [Google Scholar]
- 6.Floyd V, Hadley C, Lavoie M, Toomey K. Pregnancy-related mortality: Georgia, 1990–92. MMWR Morb Mortal Wkly Rep. 1995;44:93–97. [PubMed] [Google Scholar]
- 7.Comas A, Navarro A, Carrera A, et al. Maternal mortality surveillance: Puerto Rico, 1989. MMWR Morb Mortal Wkly Rep. 1991;40:521–523. [PubMed] [Google Scholar]
- 8.Allen MH, Chavkin W, Jarinoff J. Ascertainment of maternal deaths in New York City. Am J Public Health. 1991;81:382–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horon IL, Cheng D. Enhanced surveillance for pregnancy-associated mortality: Maryland, 1993–1998. JAMA. 2001;285:1455–1459. [DOI] [PubMed] [Google Scholar]
- 10.Atrash HK, Rowley D, Hogue CJR. Maternal and perinatal mortality. Curr Opin Obstet Gynecol. 1992;4: 61–71. [PubMed] [Google Scholar]
- 11.Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death. Geneva, Switzerland: World Health Organization; 1977.
- 12.International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD10). Geneva, Switzerland: World Health Organization; 1992. [PubMed]
- 13.Hoyert DL, Arias E, Smith BL, Murphy SL, Kochanek KD. Deaths: final data for 1999. Natl Vital Stat Rep. September 21, 2001;49(8). [PubMed]
- 14.Hebert PR, Reed G, Entman SS, Mitchel EF Jr, Berg C, Griffin MR. Serious maternal morbidity after childbirth: prolonged hospital stays and readmissions. Obstet Gynecol. 1999;94:942–947. [DOI] [PubMed] [Google Scholar]
- 15.Arias E, Anderson RN, Hsiang-Ching K, Murphy SL, Kochanek KD. Deaths: final data for 2001. Natl Vital Stat Rep. September 18, 2003:52. [PubMed]
- 16.Healthy People 2010 Volume II: Objectives for Improving Health. Washington, DC: US Government Printing Office; 2000.
- 17.Martin JA, Hamilton BE, Ventura SJ, Menaker F, Park MM, Sutton PD. Births: final data for 2001. Natl Vital Stat Rep. December 18, 2002:51. [PubMed]
- 18.McDermott JM, Steketee R, Wirima J. Mortality associated with multiple gestation in Malawi. Int J Epidemiol. 1995;24:413–419. [DOI] [PubMed] [Google Scholar]
- 19.Blickstein I. Maternal mortality in twin gestations. J Reprod Med. 1997;42:680–684. [PubMed] [Google Scholar]
- 20.Conde-Agudelo A, Belizan JM, Linkmark G. Maternal morbidity and mortality associated with multiple gestations. Obstet Gynecol. 2000;95:899–904. [PubMed] [Google Scholar]
- 21.Atrash HK, Koonin LA, Lawson HW, Franks AL, Smith JC. Maternal mortality in the United States, 1970–1986. Obstet Gynecol. 1990;76:1055–1060. [PubMed] [Google Scholar]
- 22.Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987–1990. Obstet Gynecol. 1996;88:161–167. [DOI] [PubMed] [Google Scholar]
- 23.Chang J, Elam-Evans LD, Berg CJ, et al. Pregnancy-related mortality surveillance: United States, 1991–1999. MMWR Surveill Summ. 2003;52:1–8. [PubMed] [Google Scholar]
- 24.Berg CJ, Chang J, Callaghan WM, Whitehead SJ. Pregnancy-related mortality in the United States, 1991–1997. Obstet Gynecol. 2003;101:289–296. [DOI] [PubMed] [Google Scholar]


