Abstract
Increases in obesity, hypercholesterolemia, and diabetes may be under way in Europe. We have reported the only data available from the 1990s for continuous monitoring of chronic disease risk factors in random samples of a general European population. In random surveys (1993–2003) of 6164 men and 6107 women in Geneva, overweight and obesity combined increased in both men and women; hypercholesterolemia prevalence also rose; diabetes treatment increased in men. Only population-based interventions can prevent the impending epidemic of obesity-related disorders.
Increasing relative weight trends in populations have caused much concern among health care providers.1,2 Prevalence rates of obesity and sedentary life have been escalating in the United States, where the National Health and Nutrition Examination Surveys, performed about every 10 years since 1960, showed obesity rates doubling between 1976 through 1980 and 1990 through 2000.3 Increased relative weight coincides with lipid and glucose metabolism disruptions, which translate into higher hypercholesterolemia and diabetes prevalence rates.4–6 However, very little evidence has been reported that similar trends are under way in Europe.7 In Geneva, smoking, obesity, high blood pressure, and physical inactivity are more prevalent among persons of low socioeconomic status, and most socioeconomic risk factor differences remained stable in the 1990s.8
A wider epidemic of metabolic disorders may be under way in Geneva, characterized by concurrent, parallel trends in obesity, hypercholesterolemia, and diabetes. Geneva has a relatively low prevalence of obesity,9 so the situation may be worse in other European populations.
METHODS
A risk factor surveillance system (Bus Santé) has been collecting information continuously from nonoverlapping random samples of adults aged 35 to 74, representative of the Geneva (city and canton) general population, since 1993. Through 2003, 12271 subjects (6164 men and 6107 women) have been interviewed and examined. Sampling methods, questionnaires, and examination techniques have been standardized and are described in detail elsewhere.8 Annual response rates were 57% to 65%. These are accurate participation estimates because the target population is well defined and enumerated. Residents unable to participate because they either worked outside the canton, were too sick to come, or did not understand French well enough to respond to the questionnaires were counted as refusals.
On the day of the mobile clinic appointment, each participant undergoes a physical examination. Weight and standing height are measured in subjects who are dressed but not wearing shoes (medical scale, precision=0.5 kg; medical gauge, precision=1 cm). Until 1998, total cholesterol was measured in plasma from capillary blood taken from the fingertip of nonfasting subjects with dry chemistry analyzers (Reflotron, Roche Diagnostic, Basel, Switzerland). Thereafter, it was assayed in fasting venous blood (Bayer Technicon Diagnostics, Brussels, Belgium) because substantial progressive underestimation in Reflotron capillary total cholesterol compared with the nondry chemistry laboratory measurement was observed (biases +0.08, −0.17, −0.27, and −0.60 mmol/L in 1999–200210). Overall, 57% of the Reflotron capillary total cholesterol measurements for 894 hypercholesterolemic (see next paragraph) patients underestimated laboratory venous total cholesterol (2%, 57%, 71%, and 98% in 1999–200210). Monthly quality controls for both methods were performed by the Swiss Center for Quality Control in Clinical Chemistry and Hematology.
The risk factors were defined as follows: (1) relative weight in terms of body mass index (BMI, kg/m2)—overweight=25 ≤ BMI<30, obese=BMI ≥ 30; and (2) hypercholesterolemia: total plasma cholesterol ≥ 6.5 mmol/L (approximately 250 mg/dL) or self-report of taking medication for high cholesterol. Participants also were asked if they were receiving a drug therapy for diabetes.
Risk factor prevalence trends (individual-level data, mean age adjusted) were assessed with both quarterly (44 time points) and annual (11 time points) linear regression models. The results were very similar, so annual trends are reported here. The linear regression slope represented the annual change in prevalence, and the associated (2-tailed) P value tested the null hypothesis that the slope was 0 (no trend). In addition, annual, mean age-adjusted prevalences (aggregated data) provided some idea of background sampling fluctuations.11
Six gender-specific prevalence rates of being at risk due to having (1) both high relative weight (i.e., being either overweight (only), obese, or overweight/obese) and hypercholesterolemia or (2) high relative weight or hypercholesterolemia were compared between the diabetes treatment (no or yes) subgroups with Fisher exact tests.
RESULTS
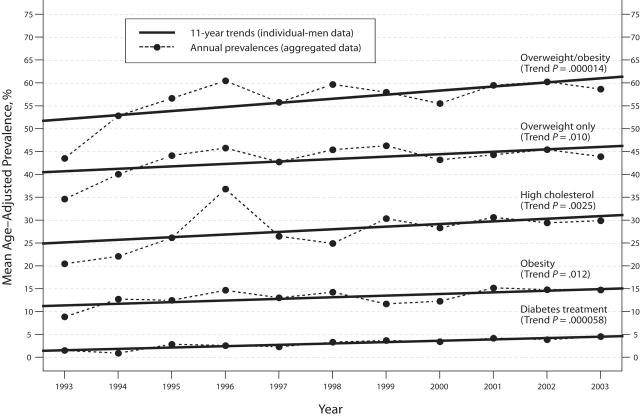
Among men, respective overweight (only) and obesity prevalence rates increased significantly—from 35% and 9%, respectively, in 1993 to 44% and 15%, respectively, in 2003 (trend P < .02; Figure 1 ▶). Likewise, the combined prevalence of overweight and obesity increased significantly (from 44% to 59%; trend P < .001).
FIGURE 1—
Eleven-year trends (1993–2003, mean age-adjusted linear regression) in overweight (only), obesity, overweight and obesity combined, hypercholesterolemia, and diabetes treatment among a random sample of 6164 male residents of Geneva, Switzerland, aged 35 to 74 years. Note. Overweight = 25 ≤ body mass index (BMI) < 30 kg/m2; obese = BMI ≥ 30 kg/m2; hypercholesterolemia = total plasma cholesterol ≥ 6.5 mmol/L (approximately 250 mg/dL) or self-report of taking medication for high cholesterol; diabetes treatment: self-reported.
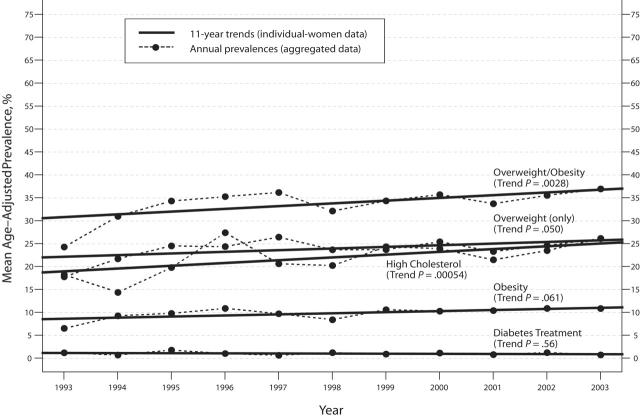
Among women, borderline trends in overweight (only) (from 18% to 26%; trend P < .06) and obesity (from 7% to 11%; trend P < .07; Figure 2 ▶) were seen. However, the increase in overweight and obesity combined was statistically significant (from 24% to 37%; trend P < .01).
FIGURE 2—
Eleven-year trends (1993–2003, mean age-adjusted linear regression) in overweight (only), obesity, overweight and obesity combined, hypercholesterolemia, and diabetes treatment among a random sample of 6107 female residents of Geneva, Switzerland, aged 35 to 74 years. Note. Overweight = 25 ≤ body mass index (BMI) < 30 kg/m2; obese = BMI ≥ 30 kg/m2; hypercholesterolemia = total plasma cholesterol ≥ 6.5 mmol/L (approximately 250 mg/dL) or self-report of taking medication for high cholesterol; diabetes treatment: self-reported.
Hypercholesterolemia increased significantly in both genders (men: from 21% to 30%; trend P < .01; women: from 18% to 26%; trend P < .001).
Among men, diabetes treatment prevalence increased significantly (from 2% to 5%; trend P < .001). Among women, there was no evidence of a sustained increase in diabetes treatment prevalence (all prevalence rates = 1%; trend P = .56).
The small fraction of either gender receiving treatment for diabetes was significantly more likely to have at least 1 of the other 2 risk factors (high relative weight, high cholesterol) compared with their nontreated counterparts (men: P<.05 for all 6 comparisons; women: P<.01 for 5 of 6 comparisons; not shown otherwise).
DISCUSSION
This is the first strong evidence of concurrent, increasing 11-year trends through 2003 in overweight and/or obesity, hypercholesterolemia, and diabetes treatment in a population of European general adult men. Among adult women in Geneva, an increasing trend in hypercholesterolemia was accompanied by an increase in being either overweight or obese, with no evidence of a change in diabetes treatment prevalence. The parallel rising trends are related because overweight or obesity and hypercholesterolemia occurred more frequently among subjects receiving a drug treatment for diabetes. The Geneva adult population is one of the leanest of those that participated in the EURALIM (EURope ALIMentation) project.9,12 Therefore, this evidence is also likely to be relevant for other European communities.
These trends might have been overlooked without the unique, ongoing system of continuous surveillance of health determinants in Geneva. Reports on trends normally rely on periodic local or national surveys, usually repeated within intervals of years.13 Because of random sampling variation in survey responses, reliance on data from a limited number of time points in a decade can be misleading. However, trends based on many more closely spaced time points can be identified clearly and interpreted with more confidence than if they were based on fewer time points spaced at much longer intervals.
The “obesity epidemic” might be a harbinger of a wider epidemic of metabolic disorders. The health effects of overweight and obesity on hypercholesterolemia, hypertension, and diabetes are well established.3 They incur increases in a wide range of chronic disorders and declines in life expectancy.
Feasible ways to combat the impending epidemic exist. It has been proposed that an excess intake of 420 kJ/day (100 kcal/day) is responsible for the increasing relative weight observed in many populations. The latter amount of energy can be expended, on average, only if the public health objective is to make populations become globally more active.14
Acknowledgments
This study was funded by the Swiss National Fund for Scientific Research (grants 32-31.326.91, 32-37986.93, 32-46142-95, 32-47219.96, 32-49847.96, 32-054097.98, 32-57104.99).
Human Participant Protection The study was approved by the Geneva University ethics committee.
Peer Reviewed
Contributors A. Morabia initiated and developed the study and has directed the Bus Santé survey since its inception in 1992. M. C. Costanza designed, performed, and interpreted the statistical analyses. Both authors contributed equally to the origination and writing of the brief.
References
- 1.Kelner K, Helmuth L. Obesity—what is to be done? Science. 2003;299:845. [Google Scholar]
- 2.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299:853–855. [DOI] [PubMed] [Google Scholar]
- 3.Manson JE, Skerrett PJ, Greenland P, VanItallie TB. The escalating pandemics of obesity and sedentary lifestyle: a call to action for clinicians. Arch Intern Med. 2004;164:249–258. [DOI] [PubMed] [Google Scholar]
- 4.Mokdad AH, Ford ES, Bowman BA, et al. Diabetes trends in the U.S.: 1990–1998. Diabetes Care. 2000;23:1278–1283. [DOI] [PubMed] [Google Scholar]
- 5.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999; 282:1519–1522. [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. [DOI] [PubMed] [Google Scholar]
- 7.Galobardes B, Costanza MC, Bernstein MS, Delhumeau CH, Morabia A. Trends in risk factors for the major “lifestyle-related diseases” in Geneva, Switzerland, 1993–2000. Ann Epidemiol. 2003;13:537–540. [DOI] [PubMed] [Google Scholar]
- 8.Galobardes B, Costanza MC, Bernstein MS, Delhumeau C, Morabia A. Trends in risk factors for lifestyle-related diseases by socioeconomic position in Geneva, Switzerland, 1993–2000: health inequalities persist. Am J Public Health. 2003;93:1302–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beer-Borst S, Morabia A, Hercberg S, et al. Obesity and other health determinants across Europe: the EURALIM project. J Epidemiol Community Health 2000;54:424–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costanza MC, Wolff H, James RW, Morabia A. Improving imprecise cholesterol monitoring and screening tests. J Clin Epidemiol. In press. [DOI] [PubMed]
- 11.Costanza MC. Estimating and approximating prevalence trends. Soz Praventivmed. 2004;49:224–226. [DOI] [PubMed] [Google Scholar]
- 12.Beer-Borst S, Hercberg S, Morabia A, et al. Dietary patterns in six European populations: results from EURALIM, a collaborative European data harmonization and information campaign. Eur J Clin Nutr. 2000; 54:253–262. [DOI] [PubMed] [Google Scholar]
- 13.Morabia A. Worldwide surveillance of risk factors to promote global health. Am J Public Health. 2000;90: 22–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morabia A, Costanza MC. Does walking 15 minutes per day keep the obesity epidemic away? Simulation of the efficacy of a populationwide campaign. Am J Public Health. 2004;94:437–440. [DOI] [PMC free article] [PubMed] [Google Scholar]