Abstract
We compared levels of geographic access to prenatal clinics in Brooklyn, NY, between immigrant and US-born mothers and among immigrant groups by country of birth. We used birth data to characterize the spatial distribution of mothers and kernel estimation to measure clinic density within a 2-mile radius of each mother. Results showed that geographic access to clinics differs substantially by country of birth. Certain groups (e.g., Pakistani, Bangladeshi) have relatively poor geographic access despite a high need for prenatal care.
Accessible and effective prenatal care is critically important for improving reproductive health outcomes in the United States. In the past 2 decades, efforts have been made to enhance access to prenatal care by expanding Medicaid coverage for pregnant women and by providing prenatal services for low-income women. These efforts have significantly increased the proportion of pregnant women who receive early and regular prenatal care, although the proportion remains below the target specified in Healthy People 2010: Understanding and Improving Health.1,2
A major challenge in improving prenatal care is to respond to shifting patterns of ethnic diversity in the population that result from immigration. Women from different ethnic backgrounds have not only diverse needs, expectations, and resources but also different residential location patterns that affect their geographic access to prenatal care. Geographic access describes distance, transportation, and mobility factors that influence people’s ability to use services when and where they are needed. Distance is a critical factor in the use of health and prenatal care services, affecting both the choice of service providers and the intensity of utilization.3–5 Travel time, cost, and effort increase with distance, creating barriers to service use.6–11 We analyzed how the uneven residential location patterns of immigrant women are related to their geographic access to prenatal care clinics provided by public and voluntary agencies in Brooklyn, NY.
METHODS
The data consisted of birth records for the year 2000 for mothers whose residential address was Brooklyn, NY (roughly 39 000 mothers). Brooklyn has a large and diverse immigrant population: 52% of the mothers in our data set were born outside the United States. Mothers’ residential locations were recorded at the census tract level. Census tracts are small areas that represent well the detailed locational patterns of immigrant groups. Immigrant groups were defined according to country of birth. To assess differences among immigrant groups in prenatal care need, we examined several indicators: low-birthweight percentage; percentage of mothers whose primary financial coverage was Medicaid; and percentage of self-pay, uninsured mothers.12
We used geographic information systems technology to assign prenatal clinics to point locations on the basis of street address. All clinics in New York City were included to allow for travel to clinics outside Brooklyn. The clinics are operated by public and voluntary agencies and primarily serve low-and middle-income mothers. Of the clinics, 30% are located in hospitals, and the rest are freestanding.
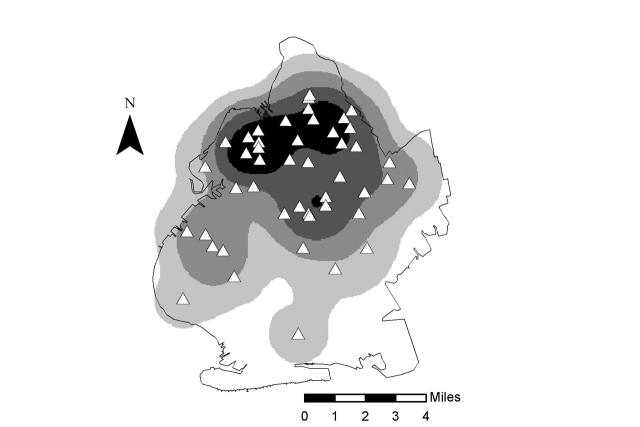
To measure geographic availability of clinics, we used kernel estimation.13–16 Kernel estimation depicts the density of points (clinics) as a spatially continuous variable that can be represented as a smooth contour map. Peaks on the map show areas of high clinic density, and valleys show areas of low clinic density. In computing density, a circle, centered at small, evenly spaced grid cells, is moved over the study area. The density of clinic locations (clinics per square mile) is computed within each circle according to a kernel function.13 A critical issue is the choice of circle radius. We used a radius of 2 miles to reflect the localized nature of primary health care use in New York City. To check the sensitivity of results to the choice of radius, we repeated the analysis with values of 1.5 and 3 miles; results were very consistent. Figure 1 ▶ depicts a map of the density of prenatal clinics in Brooklyn according to kernel estimation. High densities indicate high geographic access to services.
FIGURE 1—
Density of prenatal clinics (clinics per square mile) according to kernel estimation: Brooklyn, NY, 2000. The locations of prenatal clinics are marked by white triangles.
Source. McLafferty and Grady.17
To analyze differences in clinic density by immigrant group, we assigned each mother the density value for the corresponding census tract of residence. The density value for a tract was computed as the average density value for all grid cells in the tract. Unpopulated coastal and park areas were clipped from the census tracts and thus removed from the average density calculations. To compare clinic density levels among immigrant groups, we analyzed descriptive statistics for mothers belonging to a specific group.
RESULTS
Prenatal clinics are unevenly distributed across Brooklyn, with higher densities in north and central regions of the borough (Figure 1 ▶). Immigrant and US-born mothers had similar geographic access to clinics, as reflected in median density values (0.855 US-born; 0.729 immigrant). Among US-born mothers, those covered by Medicaid had the highest median density (1.107), compared with 0.826 for uninsured mothers and 0.632 for mothers with third-party insurance coverage. For immigrant mothers, median density was highest for the Medicaid group (0.801) and lowest for uninsured mothers (0.461). The poor geographic access to clinics for uninsured immigrant mothers is noteworthy.
Geographic access to clinics differs substantially among immigrant mothers according to country of birth (Table 1 ▶). In general, we found the highest density values for certain Caribbean and Central American immigrant groups, which shows that prenatal clinics are relatively well located in relation to the residential locations of these groups. Many of these immigrant groups have high need for services, as evidenced by high rates of low-birthweight infants and high percentages of women covered by Medicaid. Overall, median clinic density was positively correlated with low birthweight (Spearman R = 0.52; P = .004) and inversely associated with percentage of self-pay mothers (R = −0.40; P = .06).
TABLE 1—
Density of Prenatal Clinics and Need Indicators for Immigrant Mothers, by Country of Birth
| Clinic Density (Clinics/Sq Mile) | Need Indicators | |||||
| Country of Birth | n | Mean (95% CI) | Median | Medicaid, % | Self-Pay, % | Low Birthweight, % |
| Bangladesh | 304 | 0.48 (0.43, 0.54) | 0.42 | 87.2 | 4.6 | 7.9 |
| Barbados | 257 | 1.04 (0.98, 1.09) | 1.22 | 52.5 | 3.9 | 13.2 |
| China | 1753 | 0.58 (0.55, 0.59) | 0.64 | 65.0 | 8.5 | 5.0 |
| Dominican Republic | 1461 | 0.99 (0.96, 1.01) | 0.96 | 83.4 | 2.4 | 6.2 |
| Ecuador | 497 | 0.92 (0.87, 0.97) | 0.87 | 83.1 | 4.6 | 5.2 |
| Egypt | 206 | 0.37 (0.33, 0.41) | 0.28 | 51.5 | 14.6 | 7.2 |
| Grenada | 414 | 1.02 (0.98, 1.06) | 1.15 | 61.4 | 6.3 | 10.4 |
| Guyana | 919 | 0.88 (0.85, 0.91) | 0.88 | 56.0 | 2.2 | 11.0 |
| Haiti | 1349 | 0.78 (0.76, 0.81) | 0.73 | 62.8 | 3.5 | 13.0 |
| Honduras | 242 | 0.91 (0.84, 0.97) | 0.81 | 83.5 | 5.0 | 3.3 |
| Israel | 570 | 0.61 (0.57, 0.65) | 0.47 | 48.6 | 5.1 | 2.8 |
| Jamaica | 1641 | 0.92 (0.89, 0.94) | 0.97 | 59.5 | 3.4 | 10.1 |
| Mexico | 2067 | 0.79 (0.76, 0.81) | 0.76 | 93.6 | 4.0 | 5.9 |
| Nigeria | 205 | 0.84 (0.76, 0.91) | 0.88 | 60.7 | 7.8 | 9.0 |
| Pakistan | 611 | 0.31 (0.28, 0.33) | 0.21 | 84.3 | 3.8 | 9.8 |
| Panama | 222 | 0.93 (0.87, 0.99) | 0.96 | 57.7 | 2.7 | 12.5 |
| Poland | 334 | 0.48 (0.44, 0.51) | 0.40 | 53.6 | 7.8 | 4.5 |
| Russia | 541 | 0.27 (0.24, 0.30) | 0.17 | 31.1 | 12.6 | 4.7 |
| St. Vincent and Grenadines | 259 | 1.05 (1.00, 1.09) | 1.17 | 65.6 | 5.0 | 13.3 |
| Syria | 213 | 0.27 (0.23, 0.30) | 0.19 | 55.4 | 4.2 | 6.9 |
| Trinidad | 1077 | 1.01 (0.99, 1.04) | 1.15 | 61.2 | 5.2 | 9.0 |
| Ukraine | 391 | 0.20 (0.17, 0.22) | 0.14 | 23.0 | 12.5 | 5.3 |
Note. CI = confidence interval.
Only countries of birth with 200 or more births are listed. Mothers came from more than 160 countries, but sample sizes for most countries were too small for statistical comparisons.
From a policy perspective, it is important to identify groups that have a high need for clinic-based services but poor geographic access. Immigrant mothers from Pakistan and Bangladesh fit this pattern. More than 80% of Pakistani and Bangladeshi mothers rely on Medicaid, and their rates of low-birthweight infants are high, especially for Pakistani mothers. For both groups, the density of prenatal clinics in nearby areas is relatively low. Median clinic densities for Pakistani and Bangladeshi mothers are 0.21 and 0.42, respectively, well below the corresponding values for all immigrant and US-born mothers. Several other groups (e.g., Egyptians, Russians, and Ukrainians) also have a low density of prenatal clinics nearby. However, these groups have relatively low indicators of need for prenatal services.
DISCUSSION
Differences in geographic access among immigrant groups reflect their uneven residential location patterns in the study area. Many immigrant groups cluster in space as a result of the economic, social, and political forces that shape their settlement patterns. Each group has a unique residential geography that constrains its spatial access to health care. Recent research highlights the diversity among immigrant groups in reproductive health outcomes and access to prenatal care.2,18–22
Our study emphasized the importance of geographic diversity in addition to diversity in culture, resources, and behaviors. In Brooklyn, some immigrant groups have relatively high levels of geographic access to prenatal clinics, whereas others are less well served by the current configuration of clinics. Groups with higher rates of low-birthweight infants tend to have a greater density of clinics nearby, which indicates that clinic locations are sensitive to prenatal care need; however, some groups do not fit this trend. We found that Pakistani and Bangladeshi mothers have a high need for prenatal care services but poor geographic access. Other studies point to low use of prenatal care among Asian immigrant women as an important public health concern.21,23
The need for health services varies in complex geographic patterns, and such patterns provide an important foundation for planning.17,24–28 Kernel estimation, combined with small-area population health data, is useful for quickly evaluating the geographic correspondence between population needs and health service locations. Public health departments can use the methods discussed here to assess this correspondence and explore how it changes in response to demographic transitions.29 As immigration reshapes health care needs in US cities, such information is crucial for developing health service networks that are responsive and effective for improving population health.
Acknowledgments
We thank the New York City Department of Health for providing the birth data and the data on prenatal clinics. We also thank Kluwer Academic Publishers, Springer Science and Business Media, and the editor of the Journal of Medical Systems for granting copyright permission for Figure 1 ▶.
Human Participant Protection The institutional review boards of the New York City Department of Health and Mental Hygiene and the City University of New York, Hunter College, approved this study.
Peer Reviewed
Contributors S. McLafferty originated the study and participated in planning of the study, analysis of the data, and writing of the brief. S. Grady contributed to preparation of data, analysis of the data, and writing of the brief.
References
- 1.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2001. Also available at: http://web.health.gov/healthypeople/document.
- 2.Alexander GR, Kogan MD, Nabukera S. Racial differences in prenatal care use in the United States: are disparities decreasing? Am J Public Health. 2002; 92:1970–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gesler W, Meade M. Locational and population factors in health care-seeking behavior in Savanah, Georgia. Health Serv Res. 1988;23:443–462. [PMC free article] [PubMed] [Google Scholar]
- 4.Haynes R, Bentham G, Lovett A, Gale S. Effects of distances to hospital and GP surgery on hospital in-patient episodes, controlling for needs and provision. Soc Sci Med. 2002;49:425–433. [DOI] [PubMed] [Google Scholar]
- 5.Joseph A, Phillips D. Accessibility and Utilization: Geographical Perspectives on Health Care Delivery. New York, NY: Harper & Row; 1984.
- 6.Brown SS, ed. Prenatal Care: Reaching Mothers Reaching Children. Washington, DC: National Academy Press; 1998.
- 7.Byrd TL, Mullen PD, Selwyn BJ, Lorimor R. Initiation of prenatal care by low-income Hispanic women in Houston. Public Health Rep. 1996;111: 536–540. [PMC free article] [PubMed] [Google Scholar]
- 8.Nothnagle M, Marchi K, Egerter S, Braveman P. Risk factors for late or no prenatal care following Medicaid expansions in California. Matern Child Health J. 2000;4:251–259. [DOI] [PubMed] [Google Scholar]
- 9.Mikhail BI. Perceived impediments to prenatal care among low-income women. West J Nurs Res. 1999;21:335–350. [DOI] [PubMed] [Google Scholar]
- 10.Dye TD, Wojtowycz MA. Organisational variation, satisfaction, and women’s time investment in prenatal care. Paediatr Perinat Epidemiol. 1999;13: 158–169. [DOI] [PubMed] [Google Scholar]
- 11.Heck K, Schoendorf K, Chavez G. The influence of proximity of prenatal services on small-for-gestational-age birth. J Community Health. 2002;27:15–31. [DOI] [PubMed] [Google Scholar]
- 12.Bachrach D, Lipson K, Tassi A. Expanding Access to Health Insurance Coverage for Low Income Immigrants in New York State. New York, NY: The Commonwealth Fund; 2001.
- 13.Bailey T, Gatrell A. Interactive Spatial Data Analysis. Essex, England: Addison Wesley Longman Limited; 1995.
- 14.Gatrell A, Bailey T, Diggle P, Rowlingson B. Spatial point pattern analysis and its application in medical geography. Trans Inst Br Geogr. 1996;21(1): 256–274. [Google Scholar]
- 15.Reader S. Detecting and analyzing clusters of low-birth weight incidence using exploratory spatial data analysis. GeoJournal. 2001;53:149–159. [Google Scholar]
- 16.Guagliardo M, Ronzio C, Cheung I, Chacko E, Joseph J. Physician accessibility: an urban case study of pediatric providers. Health Place. 2004;10: 273–284. [DOI] [PubMed] [Google Scholar]
- 17.McLafferty S, Grady S. Prenatal care need and access: a GIS analysis. J Med Syst. 2004;28:321–333. [DOI] [PubMed] [Google Scholar]
- 18.Gould JB, Madan A, Qin C, Chavez G. Perinatal outcomes in two dissimilar immigrant populations in the United States: a dual epidemiologic paradox. Pediatrics. 2003;111(6 pt 1):676–682. [DOI] [PubMed] [Google Scholar]
- 19.Kogan MD, Alexander GR, Mor JM, Kieffer EC. Ethnic-specific predictors of prenatal care utilisation in Hawaii. Paediatr Perinat Epidemiol. 1998;12:152–162. [DOI] [PubMed] [Google Scholar]
- 20.Center for Women in Government & Civil Society & Family Planning Advocates of New York State. Working Together to Increase Immigrant Women’s Access to Reproductive Health Care: Report on Statewide Roundtable. Available at: http://www.cwig.albany.edu/FinalReport_StatewideRoundtable.htm. Accessed December 2002.
- 21.Yu SM, Alexander GR, Schwalberg R, Kogan MD. Prenatal care use among selected Asian American groups. Am J Public Health. 2001;91:1865–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aizer A, Currie J. Networks or Neighborhoods? Correlations in the Use of Publicly-Funded Maternity Care in California. NBER Working Paper w9209. Available at: http://www.nber.org/papers/w9209. Accessed May 12, 2004.
- 23.Kieffer E, Alexander G, Lewis N, Mor J. Geographic patterns of low birthweight in Hawaii. Soc Sci Med. 1993;36:557–564. [DOI] [PubMed] [Google Scholar]
- 24.Andrews HF, Kerner JF, Zauber AG, Mandelblatt J, Pittman J, Streuning E. Using census and mortality data to target small areas for breast, colorectal and cervical cancer screening. Am J Public Health. 1994; 84:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gould JB, Herrchen B, Pham T, Bera S, Brindis C. Small-area analysis: targeting high-risk areas for adolescent pregnancy prevention programs. Fam Plann Perspect. 1998;30:173–176. [PubMed] [Google Scholar]
- 26.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the Public Health Disparities Geocoding Project. Am J Public Health. 2003;93:1655–1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Needle RH, Trotter RT, Singer M, et al. Rapid assessment of the HIV/AIDS crisis in racial and ethnic minority communities: an approach for timely community interventions. Am J Public Health. 2003; 93:970–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kirby RS. Toward congruence between theory and practice in small area analysis and local public health data. Stat Med. 1996;15:1859–1866. [DOI] [PubMed] [Google Scholar]
- 29.Rushton G. Improving the geographic basis of health surveillance using GIS. In: Gatrell A, Loytonen M, eds. GIS and Health. London, England: Taylor Francis, 1998:63–79.