Abstract
Poliomyelitis has gone from being one of the worst scourges of the 20th century to nearing eradication in the 21st. This success is well known to be attributable to the Salk inactivated and Sabin attenuated poliovirus vaccines.
However, before introduction of these vaccines, William McDowall Hammon of the University of Pittsburgh Graduate School of Public Health led the first major breakthrough in prevention of the disease by using passive immunization in one of the earliest double-blind, placebo-controlled clinical trials. This study provided the first evidence that antibodies to poliovirus could prevent the disease in humans.
POLIOMYELITIS, OR POLIO, IS a modern saga. The poliovirus has likely been in the human population for thousands of years. However, before the late 1800s, paralytic disease attributable to poliovirus was sporadic and endemic, not epidemic. As an enterovirus, it is predominantly spread via the fecal–oral route and is stable in the environment. Thus, conditions of poor sanitation and crowding common before the 20th century led to widespread infection at early ages. Improved hygienic standards opened the portal for poliovirus to cause more serious disease in an epidemic form. Children lost their passive maternal antibody as they aged, leaving them vulnerable to infection and, for reasons still unclear, to the more severe, paralytic manifestations of polio.
Annual, seasonal polio epidemics first became commonplace in the United States and Western Europe in the late 19th century. In the summer of 1916, North America underwent a horrifying polio epidemic reportedly claiming more than 7000 lives in 20 states.1 The peak of the US epidemic occurred in 1952: almost 57 000 cases, more than 21000 of them paralytic. Similar epidemic trends were occurring all over the Western world.
Clearly there was a desperate need for a way to prevent poliomyelitis, preferably through a vaccine such as that developed for childhood whooping cough (pertussis) and diphtheria early in the 20th century. Thus, the best scientific and medical minds of the 1930s, 1940s, and 1950s focused on polio. We all know of Jonas Salk of the University of Pittsburgh and Albert Sabin of the University of Cincinnati for their polio vaccines. However, many other prominent figures were involved in the development of the poliovirus vaccine, particularly William McDowall Hammon, also of the University of Pittsburgh. Here I present a historical review of Hammon’s development of passive immunization in the prevention of poliomyelitis, which was one of the key advances leading to the Salk vaccine.2–5
HAMMON’S BASIS FOR POLIO PREVENTION BY PASSIVE IMMUNIZATION
Pittsburgh was the Steel City in 1949, covered with smoke and soot, with a postwar, civic push to rid the city of its dirty image. It was “a city on the rise,” according to the Pittsburgh Press. At the University of Pittsburgh in the city’s historic Oakland section, there was an unremarkable School of Medicine and a brand new Graduate School of Public Health, both endowed by wealthy Pittsburgh families, the Scaifes and Mellons. The first dean of the Graduate School of Public Health was Thomas Parran, a world-renowned physician and former US surgeon general. He recruited the cream of public health leaders to head 6 new departments. Among these individuals was the eminent 45-year-old William Hammon, tapped to chair the Department of Epidemiology and Microbiology. Hammon was born in Ohio in 1904, and his family settled in Conneautville, 60 miles (96 km) north of Pittsburgh, so this appointment meant a return to his roots. Salk later professed his strong desire for this chairmanship, having been appointed to the School of Medicine 2 years earlier, and expressed his disappointment that Parran recruited Hammon instead.5,6
Hammon was married with 2 children by the time he graduated from medical school.7 He was an ordained Methodist minister who, after completing undergraduate work at Allegheny College in 1931, served as a missionary in the Belgian Congo. Upon returning, he was admitted to Harvard Medical School and joined the laboratory of Hans Zinsser, the famous bacteriologist and epidemiologist. He received his medical degree in 1936, a master’s of public health degree in 1938, and a doctor of philosophy degree in 1939. He excelled under Zinsser’s guidance, developing the first vaccine for feline panleukopenia in collaboration with John Enders.8 In 1940, Hammon was recruited by the University of California at Berkeley.
About the time Hammon was learning virology at Harvard, the National Foundation for Infantile Paralysis (NFIP) was established by President Franklin Roosevelt, a famous polio victim, and his former law partner Basil O’Connor.9 This private organization depended on public donations. Its well-known publicity theme was small contributions, or the “March of Dimes,” which became the organization’s formal name in 1979. NFIP funded the research that eventually led to the prevention of polio.
Hammon laid out his future approach to preventing poliomyelitis in an address delivered at the annual meeting of the American Academy of Pediatrics in November 1949.10 It revealed the strengths and flaws in his reasoning, based on his scientific orthodoxy, that would lead him and most others in the field to reject Salk’s views on an inactivated polio vaccine. He stressed the use of passive immunization to prevent the infection temporarily during the polio season. Passive immunization refers to injection of blood gamma globulins that transfer specific antibodies to the virus, in contrast to active immunization, in which an antigenic substance is injected that induces specific antibodies to the virus. Hammon believed that gamma globulin obtained from pooled plasma with known neutralizing activity for neurotropic strains of poliovirus held the best promise for protecting against natural infection.
Hammon believed that gamma globulin obtained from pooled plasma with known neutralizing activity for neurotropic strains of poliovirus held the best promise for protecting against natural infection.
Hammon did not necessarily hope to prevent infection with this approach; the goal was to prevent the virus’s pathogenic effects on the nervous system. There were already tantalizing data, although from poorly controlled human trials conducted in the 1920s and 1930s, suggesting that paralysis could be prevented by passive administration of whole blood or convalescent serum.4 There was also evidence that mass immunization with plasma could prevent the spread of measles virus.11 Hammon based much of his reasoning that antibody was protective against polio on his postwar research in Guam.10 He noted that the last reported polio outbreak in Guam was in 1899. An outbreak in 1948 was restricted to Americans. He found that serum from indigenous Guamanians had neutralizing antibodies to poliovirus, probably as a result of the natural infection with the virus that persisted on the island.
Hammon emphasized that the role of antibody in immunity to poliovirus was still uncertain. It was only 2 years earlier that Isabel Morgan and David Bodian of Johns Hopkins University had shown that neutralizing antibody protected against virus challenge in monkeys.12 How long neutralizing antibodies endured in the blood was still unknown. Morgan and Bodian also showed that there were 3 poliovirus serotypes,13 a number later confirmed by the NFIP Virus Typing Committee, of which Hammon was a member.14 This “problem of multiple immunologic types”10(p700) was one of Hammon’s arguments against the use of active vaccination for polio prevention.
Another barrier was making commercial-scale virus preparations. Work on polio was greatly hampered by the fact that the virus could not be grown efficiently in tissue culture. Wild-type virus grew preferentially in primates and had to be adapted to nonprimate species through passage in cells or animals. Sabin and colleagues had tried unsuccessfully to grow the virus in different tissue types, being able to replicate their monkey brain–passaged strain only in nervous system tissue.15 They did not realize that this strain had adapted to the tissue, making it less virulent for cells derived from other tissues. In his presentation, Hammon acknowledged only in passing the recent findings of Enders, Weller, and Robbins on the growth of poliovirus in human extraneural cell cultures.16 This achievement was in fact of such magnitude that it would result in their receiving the Nobel Prize in 1954. Hammon maintained that brain tissue was still “the only present source of even moderately large supplies of virus.”10(p700) The dangers of such multiple inoculations of brain tissue had been well documented4 and had hampered the development of a poliovirus vaccine for years.
Hammon cautioned about using either killed or live virus as a vaccine, given the failures of earlier, relatively crude clinical trials. Such fear was a common theme voiced by Sabin and most leaders in the field. In the mid-1930s, Maurice Brodie of New York University, William Park of the New York City Health Laboratory, and John Kolmer of Temple University, tested inactivated and live attenuated poliovirus vaccines, respectively.17,18 These vaccines proved ineffective, with the killed vaccine causing allergic reactions and the live vaccine resulting in several cases of paralysis and death. It was unclear how much poliovirus “inactivation” would be enough to prevent its replication yet retain immunogenicity. Even if a superior killed vaccine became available, Hammon was adamant that multiple, annual inoculations would be necessary to maintain immunity. In support of this view, Morgan had shown that repeated, large doses of formalin-inactivated virus induced only temporary immunity in monkeys.19 It was apparent then, and is now well established,20 that these different forms of vaccines involve several advantages and disadvantages.
These risks led Hammon to an ultimately incorrect supposition based on the relatively low morbidity and mortality of poliovirus infections: he questioned the effort, expense, and “risk for accident” to thousands of children involved in developing a vaccine to protect a relatively few individuals from paralysis caused by poliomyelitis relative to efforts to prevent other important diseases.10 Hammon also cited the availability of gamma globulin as a plus for its use, not recognizing that his future clinical trial alone would seriously deplete the nation’s reserves of gamma globulin. High-quality gamma globulin had been available in sufficient quantity for such treatment only since the late 1940s. Cohn and Oncley of Harvard had perfected multistep fractionation processing of blood during World War II.21
Soon after this accomplishment, Enders and others proved that gamma globulin contained antibodies to infectious agents, particularly measles and polio. Clinical trials had shown that gamma globulin was effective against measles virus,11 and Bloxsom22 had reported a decrease in the expected number of paralytic polio cases in an uncontrolled gamma globulin trial involving more than 800 cases in Texas in 1949. Finally, much of the impetus for Hammon’s gamma globulin trials came from his collaborator, Joseph Stokes Jr, a renowned pediatrician at Children’s Hospital of Philadelphia. Stokes, an early proponent of passive immunization, had conducted human prophylaxis trials with whole blood for poliomyelitis in the 1930s23 and, with the prominent virologist Werner Henle, had proposed a large trial of gamma globulin immunization to the NFIP in the mid-1940s. The proposal was rejected as a result of the cost and lack of sufficient supply of gamma globulin.
Hammon stated the basic rationale for his passive immunization approach: “gamma globulin would only be given at times of probable unusual exposure, ordinarily during the early phase of the epidemic.”10(p702) Interestingly, he was critical of the likely requirement of multiple injections for primary, active immunization: “Its [gamma globulin] effect would be immediate and would represent no danger to any child.”10(p702) He did not acknowledge that passive immunization would require up to 10 cc of gamma globulin given in the buttocks, a painful and involved undertaking. Moreover, there was concern, based on accounts of such problems after parenteral inoculations, that “localized irritation” at the injection site could promote paralysis attributable to poliovirus.4,9,24
Hammon noted that passive immunization might not prevent infection but would be expected to prevent clinical disease.10 This could lead to permanent immunity through inapparent infection with wild-type strains. Hammon called for a controlled trial of gamma globulin to address his hypothesis.
THE HAMMON GAMMA GLOBULIN CLINICAL TRIALS
After arriving in Pittsburgh, Hammon proceeded with his plans for a massive field trial of immune globulin in the prevention of polio. This was not a simple process. In February 1950, he failed to gain support for the trial from a group of his peers that included Sabin, Enders, and Salk, under the auspices of NFIP. They wanted to see more animal and human data before embarking on an expensive, complicated, and potentially harmful clinical trial. Much of the opposition came from Thomas Rivers, a prominent virologist and director of the Rockefeller Institute (now Rockefeller University). He and others were concerned about Hammon’s insistence on using placebo controls, based on their fear of the injections provoking paralysis, and negative reactions from the parents of trial control participants who did not receive gamma globulin.
More than a year later, in July 1951, studies conducted by Dorothy Horstmann of Yale and Bodian provided critical proof that passively transferred antibodies protected against lethal poliovirus infections in monkeys.25,26 Bodian also reported that human gamma globulin protected monkeys against immediate intramuscular challenge with all 3 poliovirus strains.27 This was enough evidence to convince the panel, now formally established as the Committee on Immunization, to unanimously recommend that NFIP fund a pilot study of 5000 children. Notably, panel members realized that a trial of this size would not yield statistically significant results. Rather, the study’s purpose was to gain experience in organization and administration, as well as to evaluate the public’s and medical profession’s reaction to such a trial.
Hammon worked rapidly to mount the trial. Most important, he finally convinced the committee to use a 1-to-1 match of vaccine to placebo control. In Hammon’s words, “Only this type of test would withstand critical scientific scrutiny and be accepted universally as a final evaluation.”28(p741) This reflected an evolving appreciation since the 1930s that clinical trials must include control participants who do not receive the experimental drug.29 Investigators were also coming to realize that the control group should receive a placebo, a substance with no therapeutic benefit that mimicked the test drug in size, shape, color, and taste, to control for potential bias introduced by the “placebo effect,” wherein such mock treatment nonspecifically relieves a disease symptom.30 The most powerful “double-blind,” placebo-controlled clinical trials, those wherein neither the participant nor the clinician was aware of whether drug or placebo was being administered, were almost unheard of at that time. Hammon’s study on passive immunity to poliovirus would be one of the first major double-blind, placebo-controlled clinical trials. The trial ultimately would cost NFIP $1 million, an extraordinary amount at the time that reflected both interest and desperation.
Hammon and the committee addressed other factors,28 including how to blind the injection vials, type of control inoculum (autoclaved Knox gelatin), source and dosage of gamma globulin (0.14 cc per pound of body weight of Red Cross pooled gamma globulin, as Bodian had shown it to have neutralizing antibodies to polioviruses), types of syringes (disposable syringes were not yet widely available and thus were not used), venue (public schools, to allow for large numbers of participants), injection administration site (right buttock), legal aspects such as written informed consent (a half-page document!), selection of geographical area undergoing a polio epidemic of a suitable magnitude, approval by the local population (including medical groups), publicity and preparation of clinics, and follow-up studies (including gathering of stool and blood samples from incident case patients and their close contacts). Most critical was the definition of the severity of the paralytic disease, for which they used a carefully graded scale of muscle function loss.
Hammon chose to conduct the initial pilot trial in Provo, Utah, and the surrounding Utah County south of Salt Lake City.28 This choice was based on the need for an epidemic area predicted to involve a morbidity rate of 100 per 100 000, with 70% to 80% of paralytic cases occurring among children in the 1- to 12-year age range. The team of investigators calculated that at least 36 cases (24 in the control group and 12 in the treatment group) were required within the study population of 5000 to allow determination of whether the gamma globulin was protective (i.e., whether it resulted in at least a 50% reduction of cases in the treated group). By the end of August 1951, they had recorded 38 cases of paralytic poliomyelitis in Utah County for the year, with most occurring that month. The epidemic was taking off. On August 30, the study plans were presented to the Utah Medical Society and unanimously accepted with “unexpected enthusiasm.” Hammon started the trial on September 4, 1951.
Problems included such issues as lack of large autoclaves to sterilize the syringes and needles, the investigators driving 50 miles to Salt Lake City each night to use hospital autoclaves.28 However, the amount of public support was incredible. Within 3 days, the team had enrolled and inoculated 5768 children (aged 2–8 years) at 5 locations. The investigators stopped enrollment after the gamma globulin supply had been exhausted, turning hundreds away on day 4.
The results were encouraging.31,32 In the 84 days following the trial, there was 1 case of paralytic polio in the gamma globulin group (n = 2871), along with 5 cases in the placebo group (n = 2860) and 12 in the remainder of the sample (n = 6800). As anticipated by Hammon and the committee, given the small number of cases, this result was not statistically significant. The team did, however, achieve the study’s primary goal of gaining experience in administering gamma globulin to children in a large clinical trial, with no major adverse outcomes. Moreover, there was tantalizing if not conclusive evidence that gamma globulin modified the severity of paralysis, even if administered late in the incubation period.
This positive experience led to rapid approval of a larger trial that required a similar poliomyelitis rate in an area of greater population density. Hammon and colleagues found such a setting in Houston and the surrounding Harris County, Texas.31 By late June 1952, the rate of poliomyelitis cases in the area was 27 per 100 000, and half of the patients were in the 1- to 6-year age range. The double-blind trial was put into action, with enough gamma globulin available from the Red Cross to inoculate about 28% of the children in this age group (Figure 1 ▶). A New York Times editorial published on the eve of the trial expressed great hope that “poliomyelitis could eventually be as readily controlled as measles or smallpox.”33(p20)
FIGURE 1—
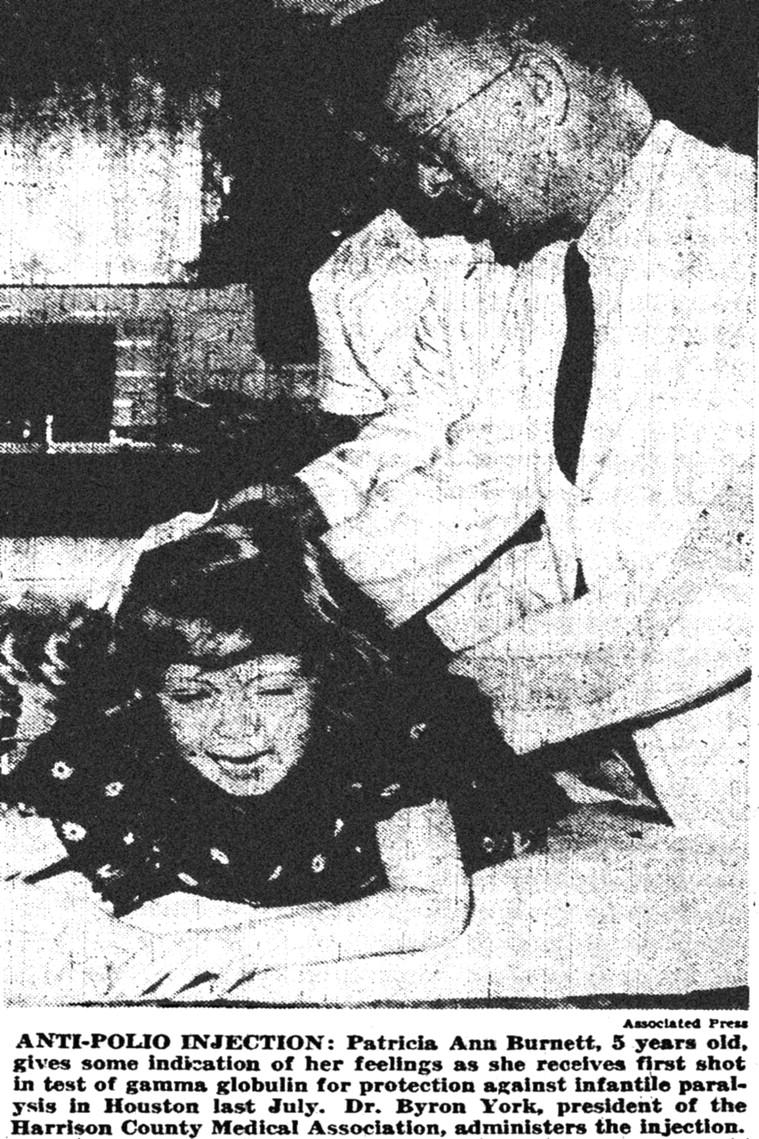
Injection of 10 cc of gamma globulin was a painful experience, as shown here in an Associated Press photograph that appeared with the October 23, 1952, New York Times article describing the Hammon clinical trials in Houston.
In the span of 10 days during July 1952, the team inoculated 33 137 children in 8 clinics. This was still not a large enough sample to achieve the most accurate, statistically significant results possible. As the trial was closing, an advance team found 2 other suitable locations: Sioux City and surrounding Woodbury County, Iowa, and nearby Dakota County, Nebraska. By mid-July 1952, the incidence of poliomyelitis in this area was 100 per 100 000 population, much higher than the rate at the Texas location. Hammon’s team quickly established its trial at this site and inoculated 15868 children aged 1 to 11 years in 6 days.
Thus, in 3 clinical trials held in less than a year, the team had inoculated 54 772 children. The procedure was safe, with very few adverse outcomes (e.g., hyperreactivity to the inoculum) and no associated paralysis. After the epidemics had waned and the cases had been tabulated, data from the combined 3 trials revealed 26 cases of paralytic polio in the group receiving gamma globulin compared with 64 cases in the controls by 10 weeks after injection.31,32 No statistical analysis was available at that time, but the results were considered “conclusive evidence of a very significant reduction in the total number of cases of paralytic poliomyelitis”32(p758) owing to the gamma globulin.
Hammon presented the trial results at the American Public Health Association’s annual meeting in Cleveland on October 22, 1952. The work was hailed in the news media across the country as the first time polio could be checked, albeit temporarily (Figure 2 ▶). In his report, Hammon stated: “If it is found that gamma globulin has not interfered with inapparent infection and the development of active immunity during the period of protection against clinical disease, this will have a wide field usefulness.”32(p759)
FIGURE 2—
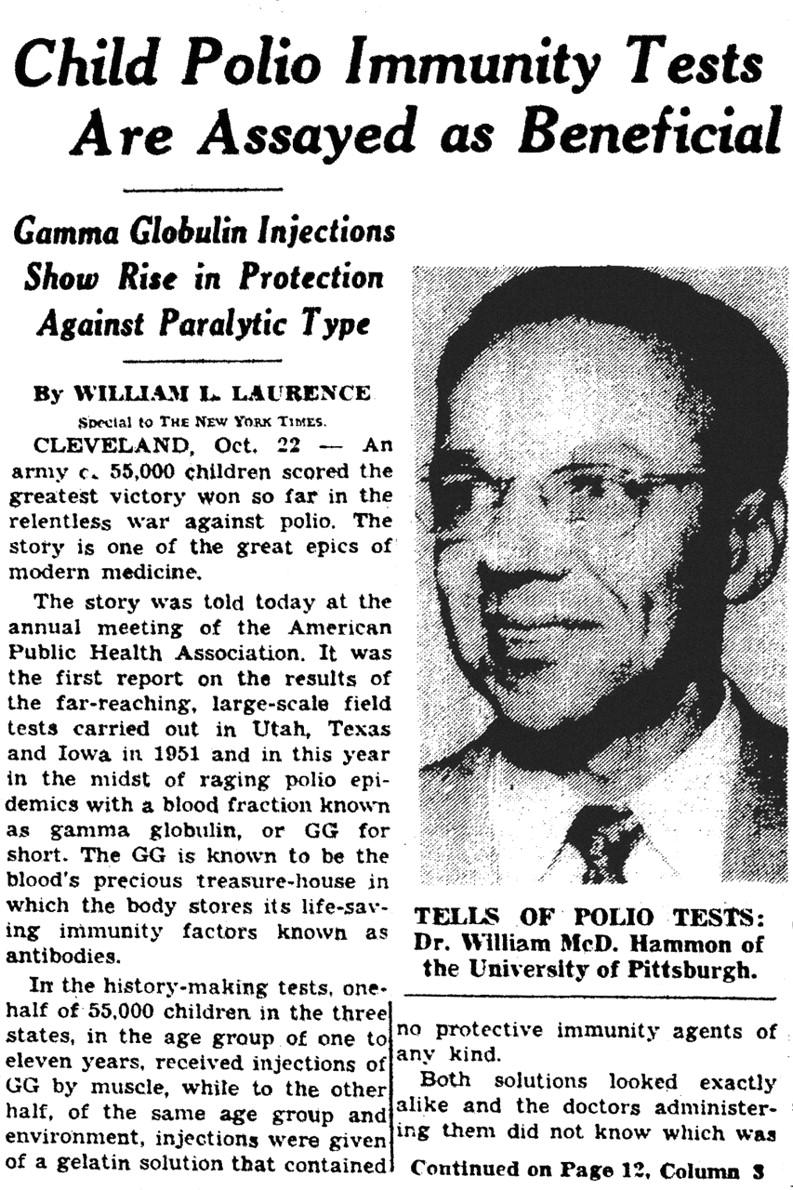
October 23, 1952, New York Times article on the report presented at the annual meeting of the American Public Health Association in Cleveland on the effectiveness of gamma globulin in the 1952 Hammon clinical trials. The photograph of Hammon is modified from an October 23 Pittsburgh Post-Gazette article.
The study results were published in 3 back-to-back articles in the October 25, 1952, issue of the Journal of the American Medical Association (JAMA).28,31,32 The accompanying editorial praised the work for the “philosophy of the experiment” as well as the “encouraging” evidence for protection from paralytic polio.34 The authors cautioned, however, that longer follow-up and final evaluation of the trial were needed before more definitive conclusions could be drawn. The “first successful prevention of paralytic poliomyelitis” was lauded by Basil O’Connor as NFIP’s scientific highlight of 1952 and the greatest step yet taken toward ultimate control of the disease.35 Hammon had impressed upon the medical community that something could finally be done to prevent the dreaded disease, although the solution was not perfect.
As anticipated, the limited availability of gamma globulin restricted its use. O’Connor warned that there was not enough to provide “even temporary protection to the 46,000,000 children and adolescents most susceptible to poliomyelitis.”35(p32) Each lot of gamma globulin was obtained from fractionation of a pool of at least 1000 units of blood plasma or serum, an expensive and time-consuming process. In the case of the largest supplier, the Red Cross, the amount of gamma globulin produced depended on voluntary blood donations. The product also contained antibodies to measles and infectious hepatitis and was needed to prevent these infections as well. The Korean War and routine hospital needs were another major drain on the gamma globulin supply. Finally, until 1955, the lots were not standardized as to amount of antibody to poliovirus, so it was unclear which lots were more potent against poliomyelitis.
Despite these caveats, this was the only protection people had against the disease. On the basis of small studies22 and anecdotal information,4 many physicians were already using gamma globulin to prevent poliomyelitis. On December 9, 1952, the Red Cross announced plans to greatly increase the production of gamma globulin and distribute it to 150 areas around the country.36 This project would cost $7 million but would protect about 1 million children in the 1953 poliovirus season.
Follow-up information on the Hammon study was presented in the April 11, 1953, issue of JAMA.37 The analysis proved that Red Cross gamma globulin offered “highly significant protection against paralytic poliomyelitis.”37(p1284) In summary, it was about 80% effective for 5 weeks if given under these controlled circumstances. Later analysis by Hammon would prove that gamma globulin had not interfered with acquisition of the infection or development of active immunity.38 In the 1953 article,37 Hammon and coauthors Stokes, Lewis Coriell of the University of Pennsylvania, and Paul Wehrle of Pittsburgh were cautious, as was the accompanying editorial,39 listing several disadvantages of passive immunization and limitations of the study: immunity was of short duration, reinjection was required during each epidemic outbreak, the optimal time for administration was unknown, the study lacked control for preexisting immunity, and the protection offered was incomplete.
Hammon gave a balanced report of his data in an address delivered to the American Association of Physicians in May 1953 in which he summarized his concerns about the misinterpretation and misuse of the results of his clinical trials.40 He opened with a bold statement: “we find ourselves for the first time with an agent capable of preventing the paralytic disease.” However, he immediately warned that “the circumstances under which it [gamma globulin] is effective are definitely limited and not yet completely defined, and furthermore the agent is in short supply.” He argued strongly against the use of gamma globulin for mass, communitywide application in polio prevention, contending that it was a wasteful endeavor: “There is not enough gamma globulin for all children in all epidemic communities.” He stressed that gamma globulin should instead be used in “a few small groups,” particularly family contacts of individuals known to have the disease (a process labeled contact prophylaxis).
HOPE FOR THE SALK VACCINE, NO FAITH IN GAMMA GLOBULIN
Hammon undoubtedly knew that gamma globulin’s fate in polio prevention was taking a downward turn by April 1953. The previous month, JAMA had published Salk’s landmark article describing the first clinical immunization trial with inactivated polio vaccine, performed in mid-1952.41 These results were first presented at a meeting of the Immunization Committee in Hershey, Pa, in January 1953.5,6,42 A year earlier, Bodian and Horstmann had described viremia caused by poliovirus infection of primates prior to development of paralysis, implying that the virus traveled to the central nervous system via the blood.43,44 Until then, it was unclear that a bloodborne phase was required for infection of the nervous system.
Salk’s 1953 study showed that different types of poliovirus, including a highly virulent strain, could be inactivated by formaldehyde.41 Moreover, antibodies against the various types of poliovirus could be increased to relatively high titers in previously infected children. This appeared to be the breakthrough toward which the scientific field had been working.
In his April 1953 article, Hammon alluded to Salk’s work by stating that “[i]t must be obvious that a vaccine that can be given to small infants in a methodical way during nonepidemic seasons and confer more or less permanent immunity is much to be desired, and that when such a vaccine is available, it will largely replace gamma globulin.”37(p1283) He then offered what turned out to be the most significant reason his work should be considered important to the field of polio prevention: “Perhaps the greatest contribution of the gamma globulin field trials is the impact [they have] on the status of active immunization through the use of a vaccine. In these gamma globulin studies it has been demonstrated that a very low concentration of antibodies will protect man.”37(p1283) This was almost a verbatim version of what Salk had stated a month earlier in his JAMA article in reference to Hammon’s trials.41
The polio story was rapidly changing even as Hammon’s 1953 article was published. A week earlier, in the April 4, 1953, issue of JAMA, an editorial stated that Salk’s work implied that injection of the new vaccine “should be adequate to provide significant protection against the paralytic consequences of a natural infection with poliomyelitis virus.”45(p1198) A letter in the same issue written by Rivers described a meeting set up by NFIP to advise Salk on future clinical trials.46 A new Vaccine Advisory Committee led by Rivers and not including any of Salk’s detractors recommended that Salk conduct a limited clinical trial of his vaccine in Pittsburgh and that these investigations take place on an “ever increasing scale” in additional communities through the summer of 1954.
While these plans were being made, the epidemic raged throughout the summer of 1953. However, now there was something that could be done. In Montgomery, Ala, the outbreak was so severe that 30000 children were given gamma globulin. The attempts to use gamma globulin in multiple locations revealed the procedure’s basic shortcoming: there was not enough gamma globulin to go around. The national supply was protected by the Office of Defense Mobilization, with a third being reserved for the polio epidemic expected that year. Thus, supplies were clearly insufficient. In total, only 235 000 children received injections in 1953.
By December 1953, NFIP was preparing to triple the amount of gamma globulin available for polio prevention during the following season. They had spent $5.5 million that year and would need to spend $19 million in the next. NFIP was being stretched beyond its financial capacity while having to fulfill the great public hopes it had created for a cure for polio. However, 2 factors were about to change this situation dramatically.
NFIP convened a panel of 17 polio experts in January 1954 to review the results of the first widespread use of gamma globulin the previous year. In addition to Hammon, the panel included public health epidemiologists, clinicians, and experts such as Sabin, John Paul of Yale University, Thomas Francis of the University of Michigan, Alex Langmuir of the Centers for Disease Control, and Abraham Lilienfeld of Johns Hopkins. The panel’s report, released on February 22, 1954, and published in March,47 was devastating for Hammon and his work. The committee concluded that mass inoculations of 185 000 children in 23 areas the previous summer had failed to produce demonstrably beneficial results (Figure 3 ▶). Actually, the committee stated that, in most cities, the gamma globulin was given after the epidemic had peaked; thus, there was little chance to demonstrate an effect of gamma globulin in modifying the epidemic.
FIGURE 3—
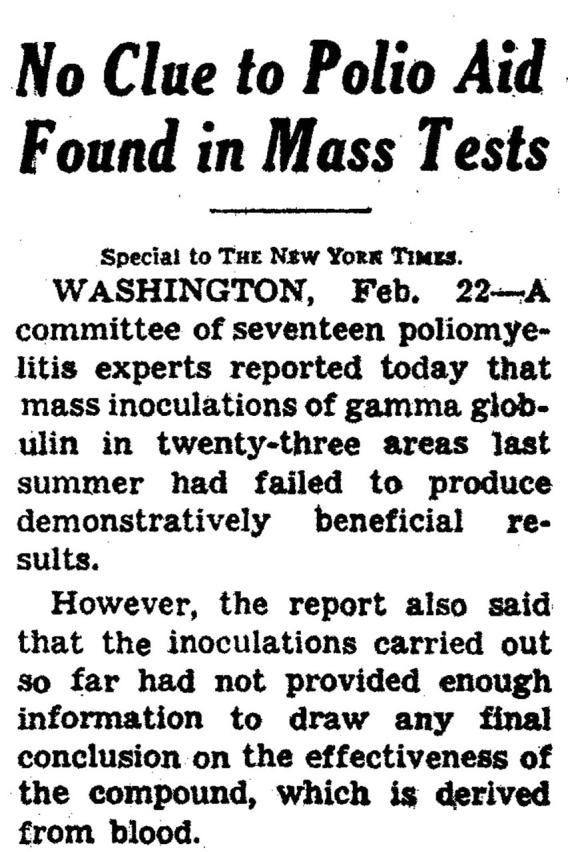
February 23, 1954, New York Times article on the report by the review committee of the “failure” of prevention of poliomyelitis by widespread use of gamma globulin in the summer of 1953.
Hammon strongly protested, filing a minority report.47 O’Connor tried to clear up the public fiasco the report created. He stated that the committee’s report did not indicate that gamma globulin was either effective or ineffective. Moreover, NFIP was still planning on tripling the gamma globulin supply for the upcoming season to 3 million doses.
Medical and public opinion were clearly marshaling against gamma globulin and in support of the Salk vaccine. Just 2 days after the 1954 report on the Hammon trial was issued, the beginning of Salk’s new clinical trial was announced nationally. By April, on the basis of safety results from use of the vaccine in 7500 children in Pittsburgh, NFIP approved the larger study. The resulting massive field trials of the Salk vaccine in 1954, and their associated controversies, have been described elsewhere.4,5,9 While dwarfing the Hammon trial in scope, the Salk project clearly incorporated major aspects of the Hammon trial design and rigid scientific method. The Vaccine Advisory Committee insisted that this large trial include placebo controls, in contrast to Salk’s preference for observed controls.5,9 Half a million children would receive the Salk vaccine, and an additional 300 000 would receive a placebo. The cost was estimated to be $7.5 million. As a means of avoiding potential complications in the Salk vaccine trial, use of gamma globulin for polio prevention was restricted in the 1954 season to geographical areas not included in the trial.48
These large field trials of the Salk vaccine were carried out against the protests of Sabin and others, who feared that the inactivated vaccine was unsafe and of low immunogenicity. The Salk vaccine, however, proved highly successful. The rate of poliomyelitis in the vaccinated group was 7 cases per 100000, compared with 35 among placebo controls.48 The vaccine was only 60% to 70% protective against paralysis caused by the more prevalent type 1 strain, but it was 90% effective against paralysis caused by the type 2 and type 3 strains. This did not represent total protection, but it was at least as good as passive immunization.
In September 1954, Hammon presented his final analysis of the 1952–1953 controlled trial at the Third International Poliomyelitis Conference in Rome, along with his reply to the NFIP committee’s report on the failure of the general use of gamma globulin in 1953.38 Reanalyses of his data using isolation of virus from feces and titration of neutralizing antibodies to poliovirus proved that gamma globulin prevented poliomyelitis in 77% to 88% of individuals exposed to the virus (Figure 4 ▶). He confirmed that, even when gamma globulin failed to prevent the disease, it significantly decreased its severity. Laboratory studies of blood obtained in the Hammon trial also proved his theory that gamma globulin did not interfere with the natural development of antibodies to poliovirus.38 Finally, he gave a highly learned yet scathing rebuttal of the 1954 committee report, insisting that the data from the uncontrolled use of gamma globulin in 1953 were overinterpreted.
FIGURE 4—
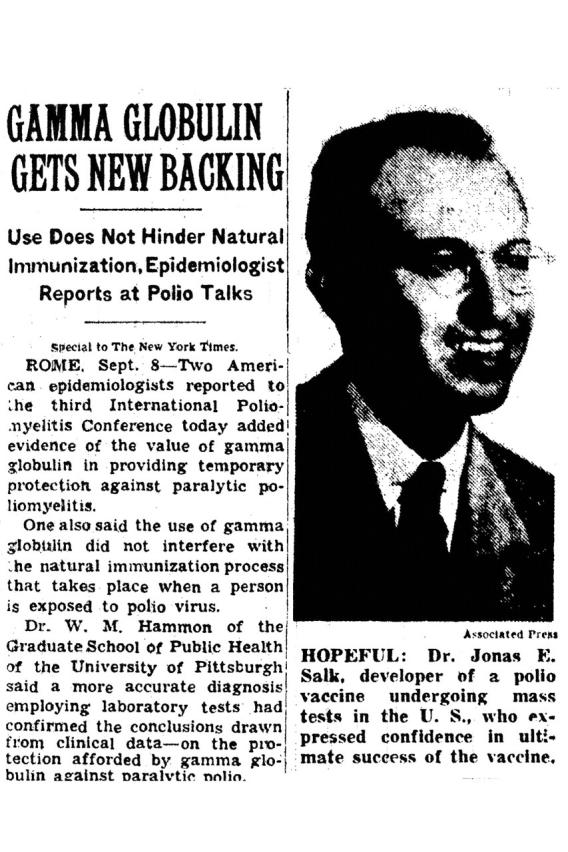
September 9, 1954, New York Times article on the Rome poliovirus conference, describing Hammon’s report that gamma globulin was effective in the 1953 epidemic and Salk’s report that the inactivated vaccine was proving effective in his 1954 trials. The article stressed that “[i]n contrast with gamma globulin, which gives temporary immunity . . . the Salk vaccine is designed as a permanent protection.”
The vindication of the use of gamma globulin was not to matter. At the same Rome meeting, Salk offered his prediction that his vaccine would give permanent protection against poliomyelitis (Figure 4 ▶). By the next year, Hammon was stating that gamma globulin might be used too late to be effective in preventing disease in family contacts, and its only practical use was in limited circumstances such as quelling polio outbreaks in institutions and summer camps.49
THE WAR IS WON
The final report on the “Salk vaccine” trials was announced at the University of Michigan in Ann Arbor on April 12, 1955.48 According to Newsweek, “The Crippler has finally been defeated.” In the span of a few days, 6 firms were licensed to manufacture the vaccine. By the end of 1955, 10 million children in 5 countries had been vaccinated. By 1956, the number of polio cases in the United States had decreased to about 15 000, and by 1960 it had decreased to about 3000. Still, the inactivated vaccine was not as potent as hoped. In one 1959 analysis, it was shown that a number of children receiving the complete series of 3 Salk vaccine injections developed paralytic poliomyelitis.50
In 1961, the Sabin live attenuated oral vaccine was licensed.51 This vaccine was as effective as the Salk vaccine but also involved several advantages such as oral administration and induction of local immunity in the gut. We now know that the attenuation of the vaccine was attributable to natural selection of spontaneous mutations during propagation that eliminated neurovirulence while maintaining the virus’s replicative capacity.52 The number of polio cases eventually dropped to only 72 in 1965. Today, there are fewer than 5 cases a year in the United States, all owing to vaccine strain revertents and none causing paralysis.
Ironically, since 1999, the Centers for Disease Control and Prevention has halted use of the live attenuated vaccine to eliminate the risk of vaccine-associated paralytic polio.53 It was found that the type 3 strain of the Sabin vaccine could revert on rare occasion to a virulent, paralytic form.54 A new version of the inactivated vaccine that is more potent than the Salk version is now exclusively used for routine vaccination in the United States.
Since the early 1950s, the use of gamma globulin to fight infectious diseases has steadily increased. We now have a large armamentarium of licensed reagents that confer passive immunity to measles, hepatitis A and B, rabies, cytomegalovirus, varicella zoster virus, and other agents.55,56 Large double-blind, placebo-controlled trials are the norm for testing new vaccines and therapeutics,57 although there are strong arguments that such controls are unethical when known, effective therapy is available.58 This progress owes much to Hammon and his scientific excellence and foresight.
Acknowledgments
I thank Dr Margaret McDonald for superb editing of the article, Dr Paolo Piazza for assistance in preparing the images, Dr Monto Ho for helpful advice, and Dr Kirsten St. George for review of the article and encouragement.
Peer Reviewed
References
- 1.Rogers N. Dirt and Disease: Polio Before FDR. New Brunswick, NJ: Rutgers University Press; 1992.
- 2.Robbins FC. Polio—historical. In: Plotkin SA, Mortimer ER Jr, eds. Vaccines. 2nd ed. Philadelphia, Pa: WB Saunders Co; 1994:137–154.
- 3.Plotkin SA, Vidor E. Poliovirus vaccine—inactivated. In: Plotkin SA, Orenstein WA, eds. Vaccines. 4th ed. Philadelphia, Pa: WB Saunders Co; 2004:625–649.
- 4.Paul JR. A History of Poliomyelitis. New Haven, Conn: Yale University Press; 1971.
- 5.Carter R. Breakthrough: The Saga of Jonas Salk. New York, NY: Trident Press; 1966.
- 6.Smith JS. Patenting the Sun: The Polio Vaccine Controversy. New York, NY: Morrow; 1990.
- 7.Reeves WC. Regional oral history. Available at: http://ark.cdlib.org/ark:/13030/kt3j49n66k. Accessed February 26, 2005.
- 8.Enders JF, Hammon WM. Active and passive immunization against the virus of malignant pan leucopenia of cats. Proc Soc Exp Biol Med. 1940;48: 194–200. [Google Scholar]
- 9.Benison S. Tom Rivers: Reflections on a Life in Medicine and Science. Cambridge, Mass: MIT Press; 1967.
- 10.Hammon WM. Possibilities of specific prevention and treatment of poliomyelitis. Pediatrics. 1950;6:696–705. [PubMed] [Google Scholar]
- 11.Gamma globulin in prevention and attenuation of measles: report of subcommittee to the Blood Transfusion Committee of the Medical Research Council. Lancet. 1948;2:41–44. [PubMed] [Google Scholar]
- 12.Morgan IM, Howe HA, Bodian D. The role of antibody in experimental poliomyelitis: II. Production of intracerebral immunity in monkeys by vaccination. Am J Hyg. 1947;45:379–389. [DOI] [PubMed] [Google Scholar]
- 13.Bodian D, Morgan I, Howe H. Differentiation of types of poliomyelitis viruses: the grouping of fourteen strains into three basic immunologic types. Am J Hyg. 1947;49:234–245. [PubMed] [Google Scholar]
- 14.Bodian D. Neutralization of three immunological types of poliomyelitis virus by human gamma globulin. Proc Soc Exp Biol Med. 1949;72:259–261. [DOI] [PubMed] [Google Scholar]
- 15.Sabin AB, Olitsky PK. Cultivation of poliomyelitis virus in vitro in human embryonic nervous tissue. Proc Soc Exp Biol Med. 1936;31:357–359. [Google Scholar]
- 16.Enders JF, Weller TH, Robbins FC. Cultivation of the Lansing strain of poliomyelitis virus in cultures of various human embryonic tissues. Science. 1949;109:85–87. [DOI] [PubMed] [Google Scholar]
- 17.Brodie M, Park WH. Active immunization against poliomyelitis. Am J Public Health. 1936;26:119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kolmer JA. Vaccination against poliomyelitis. Am J Public Health. 1936; 26:126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morgan IM. Immunization of monkeys with formalin-inactivated poliomyelitis viruses. Am J Hyg. 1948;48: 394–410. [DOI] [PubMed] [Google Scholar]
- 20.Orenstein WA, Wharton M, Bart KJ, Hinman AR. Immunization. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas and Bennett’s Principles of Infectious Diseases. 5th ed. New York, NY: Churchill Livingstone; 2000: 3207–3234.
- 21.Berger M. A history of immune globulin therapy, from the Harvard crash program to monoclonal antibodies. Curr Allergy Asthma Rep. 2002;2: 368–378. [DOI] [PubMed] [Google Scholar]
- 22.Bloxsom A. Use of immune serum globulin (human) as prophylaxis against poliomyelitis. Texas State J Med. 1949; 75:468–470. [PubMed] [Google Scholar]
- 23.Stokes J Jr, Wolman IJ, Carpenter HC, Margolis J. Prophylactic use of parents’ whole blood in anterior poliomyelitis: Philadelphia epidemic of 1932. Am J Dis Child. 1935;50:581–595. [Google Scholar]
- 24.Korns RF, Albrecht RM, Locke FB. The association of parenteral injections with poliomyelitis. Am J Public Health. 1952;42:153–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horstmann DM. Poliomyelitis virus in blood of orally infected monkeys and chimpanzees. Proc Soc Exp Biol Med. 1952;79:417–419. [DOI] [PubMed] [Google Scholar]
- 26.Bodian D. Experimental studies on passive immunizations against poliomyelitis: II. The prophylactic effect of human gamma globulin on paralytic poliomyelitis in cynomolgus monkeys after virus feeding. Am J Hyg. 1952;56:78–89. [PubMed] [Google Scholar]
- 27.Bodian D. Experimental studies on passive immunization against poliomyelitis: I. Protection with gamma globulin against intramuscular inoculation and combined passive and active immunization. Am J Hyg. 1951;54:132–143. [DOI] [PubMed] [Google Scholar]
- 28.Hammon WM, Coriell LL, Stokes J Jr. Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis: 1. Plan of controlled field tests and results of the 1951 pilot study in Utah. JAMA. 1952;150:739–749. [DOI] [PubMed] [Google Scholar]
- 29.Shapiro AK, Shapiro E. The Powerful Placebo: From Ancient Priest to Modern Physician. Baltimore, Md: Johns Hopkins University Press; 1997.
- 30.Medical Research Council. The prevention of whooping-cough by vaccination. BMJ. 1951;1:1463–1471. [PMC free article] [PubMed] [Google Scholar]
- 31.Hammon WM, Corriell LL, Stokes J Jr. Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis: 2. Conduct and early followup of 1952 Texas and Iowa-Nebraska studies. JAMA. 1952;150:750–756. [DOI] [PubMed] [Google Scholar]
- 32.Hammon WM, Coriell LL, Wehrle PF, Klimt CR, Stokes J Jr. Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis: 3. Preliminary report of results based on clinical diagnoses. JAMA. 1952;150:739–749. [DOI] [PubMed] [Google Scholar]
- 33.The Texas polio experiment. New York Times. July 7, 1952:20.
- 34.Gamma globulin as a prophylactic in poliomyelitis [editorial]. JAMA. 1952; 150:796. [DOI] [PubMed] [Google Scholar]
- 35.O’Connor reviews anti-polio strides. New York Times. November 11, 1952:32.
- 36.Red Cross polio plan to immunize young. New York Times. December 9, 1952:1.
- 37.Hammon WM, Coriell LL, Wehrle PF, Stokes J Jr. Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis: 4. Final report of results based on clinical diagnoses. JAMA. 1953;151:1272–1285. [PubMed] [Google Scholar]
- 38.Hammon WM, Coriell LL, Ludwig EH, et al. Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis: 5. Reanalysis of results based on laboratory-confirmed cases. JAMA. 1954;156:21–27. [DOI] [PubMed] [Google Scholar]
- 39.Gamma globulin in the prevention of poliomyelitis [editorial]. JAMA. 1953; 151:1292–1293. [Google Scholar]
- 40.Hammon WM. Limitations on the use of gamma globulin in poliomyelitis. Am J Med Sci. 1953;226:125–130. [PubMed] [Google Scholar]
- 41.Salk JE. Studies in human subjects on active immunization against poliomyelitis: 1. A preliminary report of experiments in progress. JAMA. 1953;151: 1081–1098. [PubMed] [Google Scholar]
- 42.Klein AE. Trial by Fury: The Polio Vaccine Controversy. New York, NY: Doubleday; 1972.
- 43.Bodian D. Experimental studies on passive immunizations against poliomyelitis: III. Passive-active immunization and pathogenesis after virus feeding in chimpanzees. Am J Hyg. 1953;58: 87–100. [DOI] [PubMed] [Google Scholar]
- 44.Horstmann DM, McCollum RW. Poliomyelitis virus in human blood during the minor illness and the asymptomatic infection. Proc Soc Exp Biol Med. 1953;82:434–437. [DOI] [PubMed] [Google Scholar]
- 45.Research on a vaccine for the prevention of poliomyelitis [editorial]. JAMA. 1953;151:1198. [DOI] [PubMed] [Google Scholar]
- 46.Rivers TM. Vaccine for poliomyelitis [letter]. JAMA. 1953;151:1224. [Google Scholar]
- 47.Evaluation of gamma globulin in prophylaxis of paralytic poliomyelitis in 1953: summary of the report of the National Advisory Committee for evaluation of gamma globulin. JAMA. 1954; 154:1086–1090. [PubMed] [Google Scholar]
- 48.Francis T, Napier JA, Voight RB, et al. Evaluation of the 1954 Field Trial of Poliomyelitis Vaccine: Final Report. Ann Arbor, Mich: Poliomyelitis Vaccine Evaluation Center, University of Michigan; 1957.
- 49.Hammon WM. Passive immunization against poliomyelitis. Monogr Ser World Health Organ. 1955;26: 357–370. [PubMed] [Google Scholar]
- 50.Berkovich S, Pickering JE, Kibrick S. Paralytic poliomyelitis in Massachusetts, 1959: a study of the disease in a well vaccinated population. N Engl J Med. 1961;264:1323–1329. [Google Scholar]
- 51.Sabin AB. Oral poliovirus vaccine: history of its development and prospects for eradication of poliomyelitis. JAMA. 1965;194:130–134. [DOI] [PubMed] [Google Scholar]
- 52.Pallansch MA, Roos RP. Entero-viruses: polioviruses, Coxsackieviruses, echoviruses, and newer enteroviruses. In: Knipe DM, Howley PM, Griffin DE, et al., eds. Fields Virology. 4th ed. Philadelphia, Pa: Williams & Wilkins; 2001:723–775.
- 53.Centers for Disease Control and Prevention. Poliomyelitis prevention in the United States: updated recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2000;49(RR-5): 1–22. [PubMed] [Google Scholar]
- 54.Racaniello VR. Poliovirus neurovirulence. Adv Virus Res. 1988;34: 217–246. [DOI] [PubMed] [Google Scholar]
- 55.Sawyer LA. Antibodies for the prevention and treatment of viral diseases. Antiviral Res. 2000;47:57–77. [DOI] [PubMed] [Google Scholar]
- 56.Keller MA, Stiehm ER. Passive immunity in prevention and treatment of infectious diseases. Clin Microbiol Rev. 2000;13:602–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Friedman LM, Furberg CD, DeMets DL. Fundamentals of Clinical Trials. New York, NY: Springer-Verlag; 1998.
- 58.Temple R, Ellenberg SE. Placebo-controlled trials and active-control trials in the evaluation of new treatments: I. Ethical and scientific issues. Ann Intern Med. 2000;133:455–463. [DOI] [PubMed] [Google Scholar]


