Abstract
Objectives. I examined trends in and epidemiological and clinical characteristics of tuberculosis (TB) within the American Indian/Alaska Native (AIAN) population of the United States and compared TB trends and characteristics in that population with TB trends and characteristics within other racial/ethnic groups.
Methods. I analyzed all verified cases of TB reported to the US National Tuberculosis Surveillance System from January 1, 1993, to December 31, 2002.
Results. From 1993 through 2002, 196133 TB cases were reported, 2612 (1.3%) of which were in the AIAN population. During this period, TB case rates declined 40.4% among AIAN peoples, the smallest decrease among any US-born racial/ethnic group. In 2002, 15075 TB cases (5.2 per 100000 population) were reported, 180 of which were in the AIAN population (8.4 per 100000 population)—almost 6 times the rate for non-Hispanic Whites (1.5 per 100000 population).
Conclusions. TB continues to be a significant health problem for the AIAN population. Vigilance and collaboration among local, state, federal, AIAN, and tribal TB control programs are essential to TB elimination among the AIAN population.
Tuberculosis (TB) continues to be a major health problem within the American Indian/Alaska Native (AIAN) population. Indeed, the incidence patterns of this disease could be said to exemplify the health disparities currently observed in the United States along racial/ethnic lines.1–5 In 2002, an estimated 4.3 million US residents (1.5% of the total population) identified themselves as AIAN, alone or in combination with another race.6 The majority of the approximately 560 federally recognized tribes are located in the West, Southwest, and Midwest.7,8
Eliminating racial and ethnic health disparities is a primary focus for many organizations9–13 and is the goal of several federal initiatives, including Healthy People 201014 and Racial and Ethnic Approaches to Community Health (REACH 2010).15 Although Healthy People 2000 documented reductions in health disparities among many races, the AIAN population demonstrated the smallest improvement.14,16 An assessment of 17 health status indicators, developed in conjunction with Healthy People 2000, revealed that TB case rates among American Indians/Alaska Natives had the highest index of disparity.1
The 2001 AIAN TB case rate was twice the national rate, and the 1997 age-adjusted AIAN TB mortality rate was 5 times greater than the national rate.17 Several TB outbreaks involving American Indians/Alaska Natives have occurred, both on and off reservations.18–22 To better understand TB epidemiology among American Indians/Alaska Natives relative to other racial/ethnic groups, I analyzed national TB surveillance data obtained from 1993 through 2002.
METHODS
I obtained data on all newly diagnosed TB cases reported to the National Tuberculosis Surveillance System (NTSS) from January 1, 1993, to December 31, 2002. I used reports that were up to date on March 28, 2003. TB is a reportable disease in every state.23 The NTSS collects data on TB cases that have been verified and meet the Centers for Disease Control and Prevention (CDC) public health surveillance case definition for TB.24,25 In addition, the NTSS collects data on TB cases verified by health care providers and reporting areas (usually states), without a requirement that cases meet the public health case definition.24 Although the CDC performs periodic data quality checks, reporting completeness throughout the system has not been evaluated. However, a multistate study estimated reporting completeness to be more than 95%.26 Other studies using other methodologies have estimated reporting completeness to be 82%–98% (average of these estimates = 91%).27–29
All 50 states and the District of Columbia report TB cases to the NTSS with a standardized case report form that records information on TB patient demographic, clinical, and laboratory characteristics.30 The instructions for reporting cases to the NTSS state that race and ethnicity information for each patient comes from the patient’s self-identity and self-reporting. Historically, almost all AIAN TB patients with case reports in the NTSS have been US born, with only 2%–3% reported as foreign born. Of the TB patients coded as foreign-born AIAN, the majority ( > 80%) were born in countries outside North, South, and Central America (e.g., India, Bangladesh) and therefore are probably miscoded. The US Census Bureau defines the AIAN population as “people having origins in any of the original peoples of North and South America (including Central America), and who maintain tribal affiliation or community attachment.”31(p2) For the purposes of this analysis, (1) AIAN TB case patients include only those persons born in the United States, unless otherwise specified; (2) race and ethnicity are characterized as either Hispanic or belonging to a non-Hispanic racial group (i.e., non-Hispanic White, non-Hispanic Black, non-Hispanic AIAN, non-Hispanic Asian/Pacific Islander); and (3) non-Hispanic American Indians/Alaska Natives and non-Hispanic Asian/Pacific Islanders are referred to as American Indians/Alaska Natives and Asian/Pacific Islanders, respectively.
Nationally, HIV test results are requested for each person diagnosed with TB. California does not report HIV test results, but reports persons with TB found in the California AIDS Registry who have a positive test result for HIV infection. In this study, all other persons in California with TB were designated as having an unknown HIV infection status.
Annual population estimates from the 1990 US Census were used to calculate TB case rates for 1993–1999, and annual population estimates from the 2000 US Census were used to calculate TB case rates for 2000–2002.32 When I calculated 2000–2002 TB case rates, the annual population estimates for persons who reported their race as exclusively AIAN, rather than in combination with 1 or more races, were used. I used the direct method and the 2000 US population as a reference to calculate age-adjusted rates. I used the Mantel–Haenszel χ2 test to calculate 2-tailed P values and the χ2 test to test for linear trends. Statistical significance was set at P < .05. Epi Info (version 6.04d; CDC, Atlanta, Ga) and SAS (version 8.02; SAS Institute Inc, Cary, NC) were used for analysis.
RESULTS
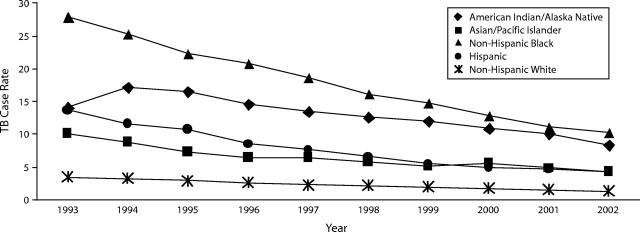
From 1993 through 2002, 196 133 TB cases were reported to the NTSS; of these, 2612 (1.3%) occurred among the AIAN population (US-born and foreign-born combined). In 2002, 15 075 TB cases (crude rate = 5.2 per 100,000 population; age-adjusted rate = 5.2 per 100 000 population) were reported in the United States; of these, 180 were in the AIAN population (1.2%; crude rate = 8.4 per 100 000 population; age-adjusted rate = 10.6 per 100 000 population) (Table 1 ▶). Overall (among US-born and foreign-born populations combined), TB case rates declined between 1993 and 2002; TB case rates decreased less steeply among Asian/Pacific Islanders (36.9%) and American Indians/Alaska Natives (39.6%) than among Hispanics (49.7%), non-Hispanic Blacks (56.6%), and non-Hispanic Whites (58.3%). However, among all segments of the US-born TB population, rates decreased less steeply among American Indians/Alaska Natives (40.4%) than among other racial/ethnic groups (Asian/Pacific Islanders, 57.4%; non-Hispanic Whites, 61.8%; non-Hispanic Blacks, 63.6%; and Hispanics, 69.3%) (Figure 1 ▶).
TABLE 1—
Characteristics of Tuberculosis (TB) Cases, by Racial/Ethnic Group: United States, 1993–2002
| Non-Hispanic, No. (%) | |||||
| Characteristic | AIAN | White | Black | API | Hispanic, No. (%) |
| Age, y | 2540 (100.0) | 48 426 (100.0) | 64 276 (100.0) | 36 805 (100.0) | 43 441 (100.0) |
| < 5 | 133 (5.2) | 976 (2.0) | 2472 (3.8) | 738 (2.0) | 2967 (6.8) |
| 5–9 | 55 (2.2) | 330 (0.7) | 1045 (1.6) | 323 (0.9) | 1172 (2.7) |
| 10–14 | 39 (1.5) | 209 (0.4) | 801 (1.2) | 379 (1.0) | 755 (1.7) |
| 15–24 | 133 (5.2) | 1372 (2.8) | 4619 (7.2) | 4119 (11.2) | 6146 (14.1) |
| 25–44 | 756 (29.8) | 11 602 (24.0) | 27 160 (42.3) | 13 147 (35.7) | 17 263 (39.7) |
| 45–64 | 795 (31.3) | 13 978 (28.9) | 18 120 (28.2) | 9797 (26.6) | 9447 (21.7) |
| ≥ 65 | 628 (24.7) | 19 941 (41.2) | 10 043 (15.6) | 8295 (22.5) | 5686 (13.1) |
| Unknown | 1 (< 0.1) | 18 (< 0.1) | 16 (< 0.1) | 7 (< 0.1) | 5 (< 0.1) |
| Site of disease | 2540 (100.0) | 48 426 (100.0) | 64 276 (100.0) | 36 805 (100.0) | 43 441 (100.0) |
| Pulmonary only | 1784 (70.2) | 38 564 (79.6) | 47 510 (73.9) | 25 961 (70.5) | 32 015 (73.7) |
| Extrapulmonary only | 488 (19.2) | 7196 (14.9) | 11 064 (17.2) | 8723 (23.7) | 7785 (17.9) |
| Pulmonary and extrapulmonary | 267 (10.5) | 2640 (5.5) | 5681 (8.8) | 2110 (5.7) | 3630 (8.4) |
| Unknown | 1 (< 0.1) | 26 (0.1) | 21 (< 0.1) | 11 (< 0.1) | 11 (< 0.1) |
| TB case criteriaa | 2540 (100.0) | 48 426 (100.0) | 64 276 (100.0) | 36 805 (100.0) | 43 441 (100.0) |
| Culture-positive | 2059 (81.1) | 39 993 (82.6) | 52 683 (82.0) | 29 565 (80.3) | 32 911 (75.8) |
| Smear-positive | 17 (0.7) | 625 (1.3) | 375 (0.6) | 239 (0.6) | 288 (0.7) |
| Clinical diagnosis | 260 (10.2) | 4435 (9.2) | 7165 (11.1) | 5000 (13.6) | 6771 (15.6) |
| Provider diagnosis | 204 (8.0) | 3373 (7.0) | 4053 (6.3) | 2001 (5.4) | 3471 (8.0) |
| Sputum smear for acid fast bacillib (adultsc) | 1857 (100.0) | 40 029 (100.0) | 49 644 (100.0) | 26 930 (100.0) | 31 902 (100.0) |
| Positive | 966 (52.0) | 17 042 (42.6) | 25 449 (51.3) | 10 305 (38.3) | 16 324 (51.2) |
| Negative | 697 (37.5) | 15 520 (38.8) | 19 052 (38.4) | 14 228 (52.8) | 12 840 (40.2) |
| Not done/unknown | 194 (10.5) | 7467 (18.7) | 5143 (10.4) | 2397 (8.9) | 2738 (8.6) |
| Sputum cultureb (adultsc) | 1857 (100.0) | 40 029 (100.0) | 49 644 (100.0) | 26 930 (100.0) | 31 902 (100.0) |
| Mycobacterium tuberculosis positive | 1523 (82.0) | 27 391 (68.4) | 38 519 (77.6) | 19 682 (73.1) | 24 548 (76.9) |
| M. tuberculosis negative | 196 (10.6) | 5305 (13.3) | 6170 (12.4) | 4729 (17.6) | 4671 (14.6) |
| Not done/unknown | 138 (7.4) | 7333 (18.3) | 4955 (10.0) | 2519 (9.4) | 2683 (8.4) |
| HIV status among TB patients aged 25–44 yd | 652 (100.0) | 10 086 (100.0) | 23 641 (100.0) | 10 567 (100.0) | 14 140 (100.0) |
| Positive | 36 (5.5) | 2207 (21.9) | 8634 (36.5) | 189 (1.8) | 3217 (22.8) |
| Negative | 267 (41.0) | 3748 (37.2) | 7857 (33.2) | 2842 (26.9) | 3636 (25.7) |
| Unknown | 349 (53.5) | 4131 (41.0) | 7150 (30.2) | 7536 (71.3) | 7287 (51.5) |
| Crude TB case ratee,f | 8.4 | 1.5 | 12.6 | 28.6 | 10.3 |
| Age-adjusted TB case ratee,f,g | 10.6 | 1.4 | 13.7 | 30.3 | 12.3 |
Note. AIAN = American Indian/Alaska Native (includes only US-born AIAN persons); API = Asian/Pacific Islander; TB = tuberculosis.
aDefinitions from the Centers for Disease Control and Prevention.24
bIncludes only persons with pulmonary TB.
cAdult is defined as a person 15 years or older.
dIncludes only TB cases reported from 1993 through 2000.
eIncludes only TB cases counted in 2002.
fTB case rate = TB cases per 100 000 population.
gAge-adjusted rates were calculated with the direct method, with the 2000 US population as reference.32
FIGURE 1—
US-born tuberculosis (TB) case rates, by race/ethnicity: United States, 1993–2002.
Note. TB case rate is per 100 000 population.
From 1993 through 2002, almost all AIAN TB patients were US-born (97.2%). Only 2.6% (n = 68) of AIAN TB patients were foreign-born, compared with 10.9% of non-Hispanic Whites, 13.6% of non-Hispanic Blacks, 65.5% of Hispanics, and 93.4% of Asian/Pacific Islanders. Of the 68 foreign-born AIAN TB patients reported from 1993 through 2002, 54 (79.4%) were born in countries outside North, South, and Central America (e.g., India, China) and were therefore probably miscoded.
During 1993–2002, the median age of AIAN TB patients (48.0 years) was higher than the median age of TB patients from other racial/ethnic groups (Asian/Pacific Islanders, 44.0 years; non-Hispanic Blacks, 42.0 years; and Hispanics, 36.0 years), with the exception of non-Hispanic Whites (58.0 years). In 2002, the proportion of TB cases in children younger than 5 years was greatest for Hispanics (6.3%), followed by non-Hispanic Blacks (4.0%), American Indians/Alaska Natives (3.3%), non-Hispanic Whites (2.1%), and Asian/Pacific Islanders (1.7%); however, TB rates (cases per 100 000 population) were highest for Asian/Pacific Islanders (7.3), followed by Hispanics (6.5), non-Hispanic Blacks (6.2), AIANs (3.5), and non-Hispanic Whites (0.6).
Geographic Location
All states except Delaware, Kentucky, Massachusetts, New Hampshire, and West Virginia reported at least 1 TB case in the AIAN population between 1993 and 2002. Among the 4 major US geographic regions,32 the majority of AIAN TB patients resided in the West (63.0%), followed by the South (22.8%), the Midwest (13.5%), and the Northeast (0.7%). AIAN TB cases made up more than 50% of the state total for 3 states: Alaska (64.0% [469]), South Dakota (65.3% [128], and Montana (51.6% [99]). In 2002, 27 states reported at least 1 TB case in the AIAN population; among states reporting at least 5 such cases, 7 states reported AIAN population TB rates higher than the national average of 8.4 cases per 100 000 population: Alaska (21.3, n = 21), South Dakota (17.7, n = 11), Washington (14.7, n = 13), Montana (14.2, n = 8), Arizona (13.8, n = 35), New Mexico (11.9, n = 20), and Oklahoma (10.4, n = 28). In 2002, of all TB cases among American Indians/Alaska Natives, 48.9% were reported for metropolitan statistical areas with populations of 50 000 or more, a smaller proportion than for other racial/ethnic groups (Asian/Pacific Islander, 97.2%; Hispanic, 91.8%; non-Hispanic Black, 89.3%; and non-Hispanic White, 78.9%). Only 9.4% of TB cases among American Indians/Alaska Natives were reported for a metropolitan statistical area with a population of 2.5 million or more persons, a much lower proportion than for other racial/ethnic groups (Asian Pacific Islander, 50.5%; Hispanic, 50.4%; non-Hispanic Black, 42.2%; and non-Hispanic White, 26.7%). The annual proportion of AIAN TB cases reported in metropolitan statistical areas with a population of 2.5 million or more persons remained relatively stable, with only minor fluctuations (range = 8.0%–12.2%; χ2 for trend, P > .05).
Clinical Characteristics
Table 1 ▶ lists clinical characteristics by the racial/ethnic group; some variability is evident. For 1993 through 2002, 70.2% of all AIAN TB patients had pulmonary TB only, 19.2% had extrapulmonary TB only, and 10.5% had both pulmonary and extrapulmonary TB. The majority of AIAN TB patients (81.1%) had cultures positive for Mycobacterium tuberculosis. Among adult (i.e., older than 14 years) AIAN patients with pulmonary TB, 52.0% were sputum smear–positive for acid fast bacilli, 82.0% were sputum culture–positive for M. tuberculosis, and 90.4% had abnormal chest radiographs (Asian/Pacific Islanders, 96.0%; Hispanics, 94.0%; non-Hispanic Whites, 92.8%; and non-Hispanic Blacks, 92.4%). Of this last group, 26.3% had evidence of cavitary disease (Hispanics, 29.9%; non-Hispanic Blacks, 29.4%; non-Hispanic Whites, 26.7%; and Asian/Pacific Islanders, 21.0%).
For 1993 through 2000 (the most recent year with complete data), 5.5% of AIAN TB patients aged 25–44 years reported a positive HIV test result. However, HIV test results were not available for the majority of patients (53.5%) (Table 1 ▶). The rate of HIV infection among AIAN TB patients was comparatively low; only Asian/Pacific Islanders with TB had a lower HIV coinfection rate (1.8%). In2000, 3.3% of AIAN TB patients aged 25–44 years were coinfected with HIV, a lower rate than for most other racial/ethnic groups (Asian/Pacific Islanders, 1.2%; non-Hispanic Whites, 13.9%; Hispanics, 14.4%; and non-Hispanic Blacks, 31.2%). A positive tuberculin skin test at TB diagnosis was reported in 65.5% of Asian/Pacific Islander, 62.9% of Hispanic, 60.5% of AIAN, 54.6% of non-Hispanic Black, and 47.2% of non-Hispanic White TB patients. However, either a tuberculin skin test was not done or the result was unknown for a large proportion of TB patients (non-Hispanic Whites, 33.3%, non-Hispanic Blacks, 31.5%, American Indians/Alaska Natives, 27.5%, Asian/Pacific Islanders, 27.5%, and Hispanics, 24.5%). American Indians/Alaska Natives reported having a previous episode of TB slightly more often (7.2%) than did members of other racial/ethnic groups (Asian/Pacific Islanders, 6.6%; non-Hispanic Whites, 5.9%; non-Hispanic Blacks, 4.8%; and Hispanics, 4.1%).
Sociodemographic Characteristics
From 1998 through 2002, a greater proportion of 18- to 64-year-old AIAN TB patients than of similarly aged TB patients from other racial/ethnic groups reported being homeless (23.2%), using excess alcohol (49.8%) within the past year, or being unemployed during the 2 years (51.4%) before TB diagnosis (Table 2 ▶) (χ2, P < .001 for all 3 comparisons). From 1998 to 2002, trends for 18- to 64-year-old AIAN TB patients who reported being homeless, using excess alcohol within the past year, or being unemployed during the 2 years before TB diagnosis remained relatively stable (χ2 for trend, P > .05 for all 3 characteristics).
TABLE 2—
Sociodemographic Characteristics Among Tuberculosis (TB) Patients Aged 18–64 Years: United States, 1998–2002
| Non-Hispanic, No. (%) | |||||
| AIAN | White | Black | API | Hispanic No. (%) | |
| Correctional facility resident at diagnosis | |||||
| Yes | 27 (3.7) | 485 (4.6) | 1 227 (6.3) | 92 (0.7) | 881 (6.0) |
| No | 699 (95.9) | 10 147 (95.2) | 18 306 (93.5) | 12 733 (99.0) | 13 706 (93.7) |
| Unknown | 3 (0.4) | 24 (0.2) | 53 (0.3) | 40 (0.3) | 38 (0.3) |
| Pa | .33 | <.05 | <.001 | <.05 | |
| RR (95% CI)a | 0.82 (0.56,1.2) | 0.59 (0.41,0.86) | 5.2 (3.4,7.9) | 0.62 (0.42,0.90) | |
| Homeless within past year | |||||
| Yes | 169 (23.2) | 1417 (13.3) | 2 133 (10.9) | 118 (0.9) | 908 (6.2) |
| No | 556 (76.3) | 9073 (85.1) | 16 983 (86.7) | 12 505 (97.2) | 13 305 (91.0) |
| Unknown | 4 (0.5) | 166 (1.6) | 470 (2.4) | 242 (1.9) | 412 (2.8) |
| Pa | <.001 | <.001 | <.001 | <.001 | |
| RR (95% CI)a | 1.7 (1.5,2.0) | 2.1 (1.8,2.4) | 24.9 (20.0,31.2) | 3.7 (3.2,4.2) | |
| Injection drug use within past year | |||||
| Yes | 30 (4.1) | 427 (4.0) | 980 (5.0) | 16 (0.1) | 448 (3.1) |
| No | 646 (88.6) | 9533 (89.5) | 17 145 (87.5) | 12 289 (95.5) | 13 414 (91.7) |
| Unknown | 53 (7.3) | 696 (6.5) | 1461 (7.5) | 560 (4.4) | 763 (5.2) |
| Pa | =.93 | =.31 | <.001 | .11 | |
| RR (95% CI)a | 1.0 (0.72,1.5) | 0.82 (0.58,1.2) | 34.1 (18.7,62.3) | 1.4 (0.96,2.0) | |
| Noninjection drug use within past year | |||||
| Yes | 88 (12.1) | 1 043 (9.8) | 3247 (16.6) | 127 (1.0) | 1037 (7.1) |
| No | 578 (79.3) | 8843 (83.0) | 14 843 (75.8) | 12 145 (94.4) | 12 767 (87.3) |
| Unknown | 63 (8.6) | 770 (7.2) | 1496 (7.6) | 593 (4.6) | 821 (5.6) |
| Pa | <.05 | <.05 | <.001 | <.001 | |
| RR (95% CI)a | 1.3 (1.0,1.5) | 0.74 (0.60,0.90) | 12.8 (9.8,16.6) | 1.8 (1.4,2.2) | |
| Excess alcohol use within past year | |||||
| Yes | 363 (49.8) | 2826 (26.5) | 5036 (25.7) | 416 (3.2) | 2397 (16.4) |
| No | 337 (46.2) | 7228 (67.8) | 13 149 (67.1) | 11870 (92.3) | 11 491 (78.6) |
| Unknown | 29 (4.0) | 602 (5.6) | 1401 (7.2) | 579 (4.5) | 737 (5.0) |
| Pa | <.001 | <.001 | <.001 | <.001 | |
| RR (95% CI)a | 1.8 (1.7,2.0) | 1.9 (1.7,2.0) | 15.3 (13.6,17.2) | 3.0 (2.8,3.3) | |
| Occupation within past 2 years | |||||
| Not employed | 375 (51.4) | 4293 (40.3) | 9523 (48.6) | 4406 (34.2) | 5227 (35.7) |
| Health care worker | 13 (1.8) | 446 (4.2) | 794 (4.1) | 653 (5.1) | 231 (1.6) |
| Correctional employee | 0 (0.0) | 22 (0.2) | 43 (0.2) | 6 (< 0.1) | 13 (0.1) |
| Migratory/agriculture | 2 (0.3) | 26 (0.2) | 86 (0.4) | 25 (0.2) | 757 (5.2) |
| Other | 213 (29.2) | 5293 (49.7) | 7633 (39.0) | 6854 (53.3) | 7582 (51.8) |
| Multiple occupations | 1 (0.1) | 18 (0.2) | 40 (0.2) | 17 (0.1) | 26 (0.2) |
| Unknown | 125 (17.1) | 558 (5.2) | 1467 (7.5) | 904 (7.0) | 789 (5.4) |
| Pa | <.001 | <.001 | <.001 | <.001 | |
| RR (95% CI)a | 1.5 (1.4,1.6) | 1.2 (1.1,1.3) | 1.7 (1.6,1.8) | 1.6 (1.5,1.8) | |
| Total | 729 (100.0) | 10 656 (100.0) | 19 586 (100.0) | 12 865 (100.0) | 14 625 (100.0) |
Note. AIAN = American Indian/Alaska Native (includes only US-born AIAN persons); API = Asian/Pacific Islander; RR = relative risk; CI = confidence interval. Characteristics among TB patients determined with a combination of self-report and medical documentation.30
aComparison of AIAN vs other racial/ethnic group.
Drug Resistance
From 1993 through 2002, among TB culture-positive American Indians/Alaska Natives without a previous history of TB, the rate of drug resistance to at least isoniazid was 2.4%, to at least any first-line drug (i.e., isoniazid, rifampin, ethambutol, pyrazinamide, streptomycin), 6.2%, and to at least isoniazid and rifampin (i.e., multidrug resistance), 0.1%. Tuberculosis isolates from other racial/ethnic groups demonstrated higher rates of resistance to at least isoniazid (by a factor of 2 or more) (Asian/Pacific Islander, 13.1%; Hispanic, 8.7%; non-Hispanic Black, 5.9%; and non-Hispanic White, 4.8%); at least any first-line drug (by a factor of 1.3 or more) (Asian/Pacific Islander, 18.9%; Hispanic, 15.8%; non-Hispanic Black, 9.7%; and non-Hispanic White, 8.4%); and at least isoniazid and rifampin (by a factor of 9 or more) (Hispanic, 2.0%; Asian/Pacific Islander, 1.6%; non-Hispanic Black, 1.4%; and non-Hispanic White, 0.9%). Overall, trends for resistance to at least isoniazid (range = 0.9%–3.5%, median = 2.4%), resistance to at least any first-line drug (range = 4.4%–8.3%, median = 6.0%), and multidrug-resistant TB (range = 0.0%–0.6%, median = 0.0%) among AIAN TB patients without a previous history of TB were relatively stable from 1993 through 2002. In 2002, resistance decreased slightly (at least isoniazid, 0.9% ; n = 1; at least any first-line drug, 4.4%; n = 5).
Directly Observed Therapy and Treatment Outcome
Use of directly observed therapy during treatment among AIAN TB patients steadily increased, from 61.6% in 1993 to 90.4% in 2000 (χ2 for trend, P < .001). In 2000 (the most recent year with complete data), the AIAN population had the highest directly observed therapy rate (90.4%) of all racial/ethnic groups (Asian/Pacific Islander, 63.0%; non-Hispanic White, 72.6%; non-Hispanic Black, 83.5%; and Hispanic, 83.7%). In 2000, excluding patients who died during TB therapy, 95.9% of AIAN TB patients completed therapy, compared with 92.5% of non-Hispanic Whites, 92.3% of non-Hispanic Blacks, 90.6% of Asian/Pacific Islanders, and 89.1% of Hispanics. From 1993 through 2000, the proportion of patients reported to have died during TB therapy (any cause) varied among racial/ethnic groups (non-Hispanic White, 13.9%; non-Hispanic Black, 12.3%; AIAN, 10.5%; Hispanic, 7.4%; and Asian/Pacific Islander, 5.0%). Among those patients who died during TB treatment (any cause), 3.7% of AIAN patients had a positive HIV test result, compared with 4.1% of Asian/Pacific Islanders, 14.5% of non-Hispanic Whites, 40.5% of Hispanics, and 41.2% of non-Hispanic Blacks.
DISCUSSION
This article is the first published comprehensive analysis of national TB surveillance data for American Indians/Alaska Natives in more than a decade.34,35 TB continues to be a significant preventable disease within the AIAN population and demonstrates a racial/ethnic distribution pattern that is typical of many health disparities seen in the United States. In 2002, the age-adjusted TB case rate in American Indians/Alaska Natives was more than 7 times higher than the TB case rate in non-Hispanic Whites and double the national TB rate. From 1993 through 2002, among US-born populations, TB rates decreased less among American Indians/Alaska Natives than among any other racial/ethnic group. It is unclear why TB rates remain elevated among American Indians/Alaska Natives; this finding may result from poor access to care, missed opportunities for latent TB infection screening and case finding, lower socioeconomic status,36 and more frequent progression to disease from latent infection with M. tuberculosis. The majority of TB cases within the AIAN population were reported in states in the West and in less populated MSAs. In addition, American Indians/Alaska Natives were the majority racial/ethnic group for reported TB cases in several states. Low rates of drug resistance among AIAN TB patients compared with TB patients from other racial/ethnic groups were consistently found and may be partly a result of high rates of directly observed therapy and completion of therapy, low reported rates of HIV coinfection, and the drug resistance levels found among the prevalent TB strains in the communities. TB disease in a child is considered a sentinel event, because it usually represents recent transmission from an adult with infectious pulmonary TB.37 Recent TB transmission may occur more frequently among racial/ethnic groups other than non-Hispanic Whites, explaining the elevated TB rates and the larger proportion of reported TB cases among children younger than 5 years.
Specific clinical conditions (e.g., diabetes mellitus) and factors (e.g., clinical, patient, microbiological) have been associated with an increased risk for progression from latent TB infection to TB disease.33,38 Diabetes mellitus is a commonly reported condition within the AIAN population39,40; as a comorbid condition in TB patients, diabetes mellitus also can affect case management. Currently, the NTSS does not collect information on diabetes mellitus. However, to help identify TB patients with diabetes mellitus, a working group of local, state, and national TB surveillance experts has proposed a revision of the National Tuberculosis Surveillance System’s standardized case report form to include whether a TB patient has diabetes mellitus. In addition, specific risk factors, such as homelessness, excess alcohol use, and unemployment were more likely to be reported by AIAN TB patients than by TB patients from other racial/ethnic groups. Awareness of these risk factors is important in TB diagnosis and case management. Screening high-risk groups for latent TB infection (i.e., targeted tuberculin testing) is a strategic component of TB control. Testing those who are at an increased risk for progression from latent TB infection to TB (e.g., patients with diabetes mellitus) and ensuring that patients not only start treatment for latent TB infection but also complete it are essential for TB control and elimination.33,41
HIV coinfection was more commonly reported in non-Hispanic Black, Hispanic, and non-Hispanic White TB patients than in AIAN TB patients. However, HIV test results were not reported to the NTSS for a large proportion of TB patients, regardless of racial/ethnic classification and despite the CDC recommendation that all TB patients, independent of risk factors, should be advised to undergo HIV counseling, testing, and referral.41–43 Although American Indians/Alaska Natives accounted for fewer than 1% of HIV infections reported in the US general population through 2001 and HIV infection rates among American Indians/Alaska Natives have been low, the estimated AIDS incidence among adult and adolescent American Indians/Alaska Natives increased between 1998 and 2001.44 Low HIV and AIDS infection rates among American Indians/Alaska Natives should not deter health care providers from providing TB patients with HIV counseling, testing, and referral. A recent TB outbreak in Seattle–King County, Wash, highlighted the need for HIV testing. An investigation revealed that 55% of outbreak-associated cases were in the AIAN population and that 36% of AIAN TB patients were coinfected with HIV.45
A potential limitation of any study analyzing AIAN data is racial/ethnic group misclassification. This limitation can result in underestimation of disease incidence. One study that examined death certificate data revealed that 14.7% of American Indians/Alaska Natives were misclassified, with misclassification more common among people younger than 21 years, people aged 65 years and older, and people living in urban areas.46 Another study of sexually transmitted disease surveillance data found that racial/ethnic group misclassification resulted in underestimates of disease incidence and that the chance for misclassification increased as percentage of AIAN heritage decreased. For people claiming 50%–99% AIAN ancestry, misclassification for chlamydia was approximately 15%; for gonorrhea, the figure was approximately 35%.47 Although racial/ethnic data collected by the NTSS is based on patient self-identification and self-reporting, no quality assurance studies have been performed to assess the frequency of misclassification. Therefore, misclassification may occur, and the number of reported TB cases within the AIAN population may be underestimated.
Characteristics common to many AIAN communities, such as rural location, sovereign nation status, and elevated incidence of coexisting medical conditions (e.g., diabetes mellitus), pose unique challenges for TB control. The rural location of the majority of AIAN TB patients adds to the difficulty and cost of TB control owing to the distances health care workers and community members must travel, which in turn affects the detection of new TB cases, case management, directly observed therapy administration, TB treatment completion, and contact investigations.48 States with many TB patients resident in rural locales may be classified as low–TB incidence states (i.e., ≤ 3.5 TB cases per 100 000 population) and thus typically have very small TB control programs with few staff and resources. Some TB control programs have endeavored to overcome barriers inherent in rural locales with innovative options, such as videophones for TB patients to document directly observed therapy49 and community health aides to provide care to persons in rural locales.22 Because federally recognized AIAN tribes are self-governing and sovereign nations, they are not required to report TB disease to county and state health departments. The institution of special written agreements defining reporting policies would help ensure complete reporting. Several concerns facing tribal health agencies (e.g., funding, training, clinical consultation) also could be addressed through negotiated agreements (e.g., cooperative agreements, memoranda of understanding) with local and state TB control programs.13 A recent TB outbreak in Montana illustrated the need, especially in low–TB incidence areas, for adequate health care staff training and education, availability of clinical consultation, and thorough contact investigations that include both social networks and household contacts.20
Although many AIAN health units currently have a strong working relationship with their counterparts in local health departments to ensure that patients with TB are reported and their illness properly managed and that contact investigations are conducted,13 all these parties should continue to strengthen existing working relationships and to establish new ones when appropriate.50 Documentation of existing work and publication of annual reports (e.g., TB epidemiology) would allow TB control programs to disseminate data analyses and justify requests for additional resources. The annual Four Corners TB/HIV Conference is an excellent example: experts from various governmental and nongovernmental agencies gather to present and discuss timely TB and HIV issues concerning the AIAN population, particularly those populations from the Four Corners region (Arizona, Colorado, New Mexico, and Utah). A similar meeting of the Great Plains states (Colorado, Montana, Nebraska, North Dakota, South Dakota, and Wyoming) has been proposed and could provide northern tribe members an opportunity to review TB strategies in their regions.13
TB continues to be a major health problem for the AIAN population. TB elimination among American Indians/Alaska Natives will require continuous and effective communication between TB control programs and local, state, federal, and tribal governments and organizations. Collaboration between health care and public health partners, carried out with respect for traditional tribal culture, will promote TB case detection and management, help providers identify and treat contacts with latent TB infection and identify people for targeted testing, improve the capacity to respond to outbreaks, and optimize TB surveillance while decreasing the burden and cost of TB control. Continued vigilance and collaboration are essential to controlling TB among the AIAN population.
Acknowledgments
This work was funded by the Division of Tuberculosis Elimination, Centers for Disease Control and Prevention.
The author thanks the state and local tuberculosis control officials in health departments throughout the United States who collected and reported the national surveillance data presented in this article and the surveillance staff at the Division of Tuberculosis Elimination who maintain the national database. In addition, the author thanks Jeanne Bertolli, Ralph T. Bryan, Jennifer Giroux, Michael Iademarco, John Jereb, Ann H. Lanner, Marisa Moore, Thomas R. Navin, and John T. Redd for their critical review of the article.
Human Participant Protection The CDC National Tuberculosis Surveillance System is considered routine disease surveillance and does not constitute human or animal subjects research. Therefore, specific institutional review board approval was not needed for this study.
Peer Reviewed
References
- 1.Keppel KG, Pearcy JN, Wegener DK. Trends in Racial and Ethnic-Specific Rates for the Health Status Indicators: United States, 1990–98. Healthy People Statistics Notes No 23. Hyattsville, Md: National Center for Health Statistics; 2002. [PubMed]
- 2.American Public Health Association. Cover story, the nation’s health, April 2002. Health disparities improve in US, but still significant: gains found for all races, ethnicities. Available at: http://www.apha.org/journal/nation/disparitiescover402.htm. Accessed November 3, 2004.
- 3.Centers for Disease Control and Prevention. Office of Minority Health. Eliminating racial and ethnic health disparities. Available at: http://www.cdc.gov/omh/aboutus/disparities.htm. Accessed November 3, 2004.
- 4.Grossman DC, Krieger JW, Sugarman JR, Forquera RA. Health status of urban American Indians and Alaska Natives. JAMA. 1994;271:845–850. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Health status of American Indians compared with other racial/ethnic minority populations—selected states, 2001–2002. MMWR Morb Mortal Wkly Rep. 2003;52(47);1148–1152. [PubMed] [Google Scholar]
- 6.Population Division, US Census Bureau. Annual resident population estimate of the United States by race and Hispanic or Latino origin: April 1, 2000 to July 1, 2002. Table NA-EST2002-ASRO-04-National Population Estimates—Characteristics. June 18, 2003. Available at: http://www.census.gov/popest/archives/2000s/vintage_2002/NA-EST2002-ASRO-04.html. Accessed February 1, 2005.
- 7.US Census Bureau. American Indian/Alaska Native Heritage Month: November 2002. Facts for Features. October 21, 2002. Available at: http://www.census.gov/Press-Release/www/2002/cb02ff17.html. Accessed November 3, 2004.
- 8.Indian Health Service. IHS Fact Sheet. Available at: http://www.ihs.gov/aboutihs/thisfacts.asp. Accessed November 3, 2004.
- 9.Centers for Disease Control and Prevention. Office of Minority Health. Guiding principles on tribal consultation. Available at: http://www.cdc.gov/omh/reports/guidingprinciples.htm. Accessed November 3, 2004.
- 10.US Department of Health and Human Services. Office of Minority Health. Available at: http://www.omhrc.gov. Accessed November 3, 2004.
- 11.Indian Health Service. Available at: http://www.ihs.gov. Accessed November 3, 2004.
- 12.Centers for Disease Control and Prevention. National Center for Health Statistics. Minority Health Statistics Grants Program. Promoting health traditions: reaching Native Americans with the Year 2000 National Health Objectives. Available at: http://www.cdc.gov/nchs/otheract/grants/projects/progdir/suagee.htm. Accessed November 3, 2004.
- 13.Centers for Disease Control and Prevention. Division of Tuberculosis Elimination (DTBE). Proceedings From a Meeting of Field Services Branch, DTBE: Advancing Tuberculosis Control for American Indians and Alaskan Natives: Developing a DTBE Plan. May 30, 2001. Located at: Centers for Disease Control and Prevention, Division of Tuberculosis Elimination (DTBE), Atlanta, Ga.
- 14.Centers for Disease Control and Prevention. National Center for Health Statistics. Healthy People 2010. Available at: http://www.cdc.gov/nchs/hphome.htm#Healthy%20People%202010. Accessed November 3, 2004.
- 15.Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion. Racial and Ethnic Approaches to Community Health (REACH 2010). Available at: http://www.cdc.gov/reach2010. Accessed November 3, 2004.
- 16.Centers for Disease Control and Prevention, National Center for Health Statistics. Health People 2000 Final Review. Hyattsville, Md: US Public Health Service; 2001. Available at: http://www.cdc.gov/nchs/products/pubs/pubd/hp2k/review/highlightshp2000.htm. Accessed November 3, 2004.
- 17.Indian Health Service. Office of Public Health, Division of Program Support. Regional Differences in Indian Health, 2000–2001. May 2003.
- 18.Chandler B. Update—Tuberculosis in Anchorage. State of Alaska Epidemiology Bulletin 9, May 15, 2000. Available at: http://www.epi.hss.state.ak.us/bulletins/docs/b2000_09.htm. Accessed November 3, 2004.
- 19.Centers for Disease Control and Prevention. Tuberculosis outbreak on Standing Rock Sioux Reservation—North Dakota and South Dakota, 1987–1990. MMWR Morb Mortal Wkly Rep. 1991;40(12):204–207. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Tuberculosis outbreak on an American Indian reservation—Montana, 2000–2001. MMWR Morb Mortal Wkly Rep. 2002;51(11):232–234. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Epidemiology Program Office. Epi-Aid Trip Report. Transmission of Mycobacterium tuberculosis in a low-incidence state (Epi-2002–59). November 26, 2002. Located at: Centers for Disease Control and Prevention, Division of Tuberculosis Elimination (DTBE), Atlanta, Ga.
- 22.Funk EA. Tuberculosis control among Alaska Native people. Int J Tuberc Lung Dis. 1998;2(9 suppl 1): S26–S31. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Tuberculosis control laws—United States, 1993. MMWR Recomm Rep. 1993;42(RR-15):1–28. [Google Scholar]
- 24.Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 2003. Atlanta, Ga: US Dept of Health and Human Services; 2004.
- 25.Centers for Disease Control and Prevention. Case definitions for infectious conditions under public health surveillance. MMWR Recomm Rep. 1997;46(RR-10): 40–41. [PubMed] [Google Scholar]
- 26.Curtis AB, McCray E, McKenna M, Onorato IM. Completeness and timeliness of tuberculosis case reporting: a multistate study. Am J Prev Med. 2001;20(2): 108–112. [DOI] [PubMed] [Google Scholar]
- 27.Yokoe DS, Subramanyan GS, Nardell E, Sharnprapai S, McCray E, Platt R. Supplementing tuberculosis surveillance with automated data for health maintenance organizations. Emerg Infect Dis. 1999;5: 779–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yokoe DS, Coon SW, Dokholyan R, et al. Pharmacy data for tuberculosis surveillance and assessment of patient management. Emerg Infect Dis. 2004;10: 1426–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trepka MJ, Beyer TO, Proctor ME, Davis JP. An evaluation of the completeness of tuberculosis case reporting using hospital billing and laboratory data; Wisconsin, 1995. Ann Epidemiol. 1999;9:419–423. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention, Division of Tuberculosis Elimination. Tuberculosis Information Management System (TIMS) User’s Guide. Atlanta, Ga: Centers for Disease Control and Prevention; 1998. Surveillance Appendix 1.
- 31.Ogunwole S. The American Indian and Alaska Native population: 2000. Census Bureau 2000 Brief. February 2002;1–12. Available at: http://www.census.gov/prod/2002pubs/c2kbr01-15.pdf. Accessed November 3, 2004.
- 32.US Census Bureau. Available at: http://www.census.gov. Accessed November 3, 2004.
- 33.Centers for Disease Control and Prevention. Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep. 2000;49(RR-6): 1–54. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Tuberculosis among American Indians and Alaskan Natives—United States, 1985. MMWR Morb Mortal Wkly Rep. 1987;36(30):493–495. [PubMed] [Google Scholar]
- 35.Sugarman J. Tuberculosis among American Indians and Alaska Natives, 1985–1990. IHS Primary Care Provider. 1991;16:186–190. [Google Scholar]
- 36.Cantwell M, McKenna M, McCray E, Onorato I. Tuberculosis and race/ethnicity in the United states: impact of socioeconomic status. Am J Respir Crit Care Med. 1997;157:1016–1020. [DOI] [PubMed] [Google Scholar]
- 37.Nelson LJ, Schneider E, Wells CD, Moore M. Epidemiology of childhood tuberculosis in the United States, 1993–2001: the need for continued vigilance. Pediatrics. 2004;114:333–341. [DOI] [PubMed] [Google Scholar]
- 38.Pablos-Mendez A, Blustein J, Knirsch CA. The role of diabetes mellitus in the higher prevalence of tuberculosis among Hispanics. Am J Public Health. 1997;87: 574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Diabetes prevalence among American Indians and Alaska Natives and the overall population—US, 1994–2002. MMWR Morb Mortal Wkly Rep. 2003;52(30): 702–704. [PubMed] [Google Scholar]
- 40.Mori MA, Leonardson G, Welty TK. The benefits of isoniazid chemoprophylaxis and risk factors for tuberculosis among Oglala Sioux Indians. Arch Intern Med. 1992;152:547–550. [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. Essential components of a tuberculosis prevention and control program. MMWR Recomm Rep. 1995;44(RR-11): 1–17. [Google Scholar]
- 42.American Thoracic Society, Centers for Disease Control and Prevention, and Infectious Diseases Society of America. Statement on the treatment of tuberculosis. Am J Respir Crit Care Med. 2003;167:603–662. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Prevention and treatment of tuberculosis among patients infected with human immunodeficiency virus: principles of therapy and revised recommendations. MMWR Recomm Rep. 1998;47(RR-20):1–58. [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report. 2001;13(No. 2):1–44. Available at: http://www.cdc.gov/hiv/stats/hasr1302.pdf. Accessed November 3, 2004. [Google Scholar]
- 45.Lofy K, Narita M, Goldberg S, Lake L. An outbreak of TB among homeless persons in Seattle & King County—Washington State, 2002–2003. Centers for Disease Control and Prevention TB Notes Newsletter. 2003;3:8–10. [Google Scholar]
- 46.Stehr-Green P, Bettles J, Robertson LD. Effect of racial/ethnic misclassification of American Indians and Alaskan Natives on Washington State death certificates, 1989–1997. Am J Public Health. 2002;92:443–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thoroughman DA, Frederickson D, Cameron HD, Shelby LK, Cheek JE. Racial misclassification of American Indians in Oklahoma state surveillance data for sexually transmitted diseases. Am J Epidemiol. 2002; 155(12):1137–1141. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. Progressing toward tuberculosis elimination in low-incidence areas of the United States. MMWR Recomm Rep. 2002;51(RR-05):1–16. [PubMed] [Google Scholar]
- 49.Pate SM. Videophone pilot project in Washington State for TB patients. Centers for Disease Control and Prevention TB Notes Newsletter. 2003;1:13–15. [Google Scholar]
- 50.Giroux J. Advancing TB control among American Indians and Alaska Natives. Centers for Disease Control and Prevention TB Notes Newsletter. 2003;3:10–11. [Google Scholar]