Abstract
Objectives. Recently, New York City and New York State increased cigarette excise taxes and New York City implemented a smoke-free workplace law. To assess the impact of these policies on smoking cessation in New York City, we examined over-the-counter sales of nicotine replacement therapy (NRT) products.
Methods. Pharmacy sales data were collected in real time as part of nontraditional surveillance activities. We used Poisson generalized estimating equations to analyze the effect of smoking-related policies on pharmacy-specific weekly sales of nicotine patches and gum. We assessed effect modification by pharmacy location.
Results. We observed increases in NRT product sales during the weeks of the cigarette tax increases and the smoke-free workplace law. Pharmacies in low-income areas generally had larger and more persistent increases in response to tax increases than those in higher-income areas.
Conclusions. Real-time monitoring of existing nontraditional surveillance data, such as pharmacy sales of NRT products, can help assess the effects of public policies on cessation attempts. Cigarette tax increases and smoke-free workplace regulations were associated with increased smoking cessation attempts in New York City, particularly in low-income areas.
Legislators and public health officials in New York City and New York state recently implemented a multifaceted comprehensive tobacco control program, including a state cigarette tax increase of $0.39 per pack in April 2002, a city tax increase of $1.42 in July 2002, sweeping smoke-free workplace legislation in March 2003, and a large nicotine patch giveaway program in April and May 2003. Similar policies have been shown to be effective in other jurisdictions in decreasing the prevalence of smoking, reducing tobacco use among smokers, and reducing exposure to environmental tobacco smoke.1–5 Such changes are likely to result in a reduction in morbidity and mortality associated with cigarette smoking.3 Several years may pass, however, before the public health impact of these measures can be evaluated for policymakers and the public by traditional surveillance methods such as analyses of vital statistics data or resource-intensive repeated large behavioral risk factor surveys.
The emerging field of syndromic surveillance uses administrative and other routinely collected electronic data for real-time non-traditional public health surveillance.6,7 The New York City Department of Health and Mental Hygiene syndromic surveillance system monitors multiple health indicators daily, including emergency department visits,8 ambulance dispatches,9 and pharmacy sales.10 While this syndromic surveillance system was implemented to detect abnormal changes in these health indicators that may signal the beginning of a disease outbreak, the same data may also be used for the timely surveillance of other health outcomes, including the use of smoking cessation products. To assess the impact of smoking policies on smoking cessation in New York City, we examined temporal trends in over-the-counter pharmacy sales of nicotine replacement therapy (NRT) products, a proxy measure for cessation attempts,11 across the city and by geographic location.
METHODS
Data on over-the-counter pharmacy sales are collected daily for syndromic surveillance from more than 200 store locations in New York City, representing approximately 30% of all pharmacies in New York City.10 For these analyses, we examined information on the weekly sales and product promotions of 12 over-the-counter brand-name and generic nicotine patch and nicotine gum products from July 29, 2001, to January 17, 2004. Only data from the 166 pharmacies that began contributing data by January 1, 2002, and continued providing data through the end of the study period are included in the analysis.
We assessed changes in mean weekly sales of nicotine patches and nicotine gum during the weeks of the implementation of the state tax increase (implemented April 3, 2002), the city tax increase (implemented July 2, 2002), and the Smoke-Free Air Act (SFAA, the New York City smoke-free workplace law, enacted March 30, 2003).12 We also examined changes in sales during the week prior to and the 4 weeks after each of these events. We evaluated the impact of New York City’s free patch program (April 2, 2003, to May 14, 2003), during which almost 35 000 free courses of the nicotine patch were distributed to heavy smokers, defined as those who smoked more than 10 cigarettes per day, living in New York City.13 Additionally, we examined changes in sales during the weeks encompassing New Year’s Day in 2002, 2003, and 2004; we expected to see increases in sales during these weeks because quitting smoking is a common New Year’s resolution.14,15
Analyses were conducted with SAS version 8.2 (SAS Institute Inc, Cary, NC). We conducted a repeated-measures analysis with Poisson generalized estimating equations (PROC GENMOD), using weekly counts of NRT product sales for each store.16 An exchangeable correlation structure was used to account for the correlation of the response variable, weekly counts within each store. The model controlled for temporal and seasonal patterns by including terms for linear and quadratic time trends and sine and cosine functions with annual periodicity. Indicators for weeks that included major holidays, the World Trade Center attack (September 11, 2001), and the Northeast blackout (August 14, 2003) were included in the model to account for store closings and modified consumer behaviors. Using the same methodology, we also conducted an analysis of over-the-counter sales of analgesic products, which would not be expected to change concomitantly with these smoking-related policies.
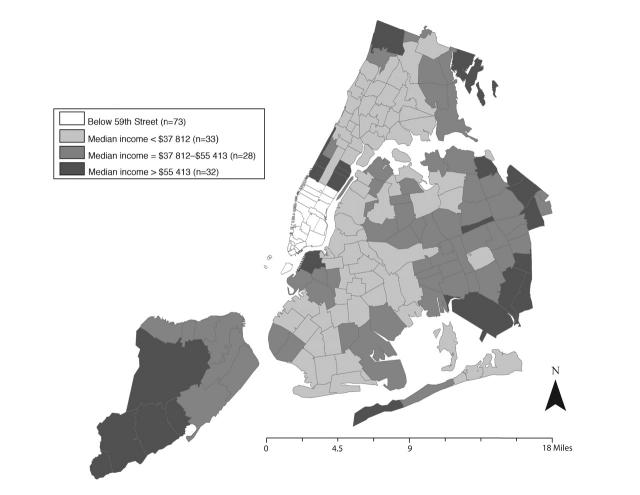
We also evaluated effect modification by pharmacy location. Zip codes for areas located south of 59th Street in Manhattan were considered to be areas populated during the day primarily by workers commuting from other parts of New York City and from surrounding states. Other New York City zip codes were categorized into tertiles on the basis of median income according to the 2000 US Census17 (Figure 1 ▶).
FIGURE 1—
Categorization of New York City zip codes used to evaluate effects of tobacco control measures on pharmacy sales of nicotine replacement therapy products by pharmacy location.
Note. Areas located south of 59th Street in Manhattan were considered to be occupied during the day by commuters; other areas were categorized by median income.
RESULTS
Citywide Trends
Data from 166 pharmacies were analyzed. The median number of weeks available from each pharmacy was 129 (range, 108–129); the median number of days available from each pharmacy was 897 (range, 586–903). The number of days per week provided by each pharmacy depended on store hours, weather, and other events. Few data transmission problems occurred; data were reported for 99.6% of nonholiday weekdays from all stores.
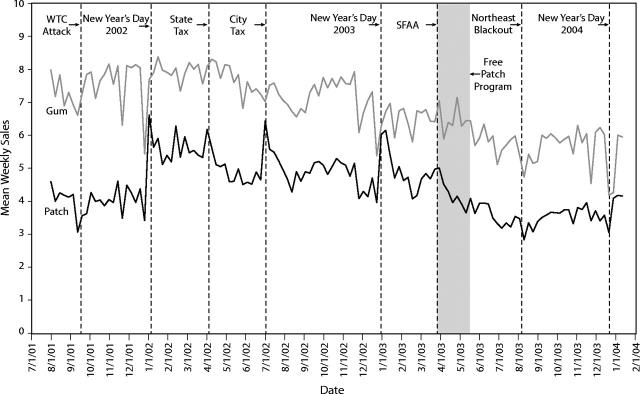
Figure 2 ▶ shows the mean weekly sales of nicotine patches and nicotine gum from July 29, 2001, to January 17, 2004. Unit sales were higher for the gum than for the patches for the entire period, with an average of 6.8 and 4.4 sales per store per week, respectively. Disruptions in commerce attributable to the World Trade Center attack and the Northeast blackout were associated with decreased sales of both products.
FIGURE 2—
Mean weekly over-the-counter pharmacy sales of nicotine replacement therapy products: New York City, July 29, 2001, to January 17, 2004.
After controlling for long-term temporal trends, we found significant increases in nicotine patch sales and significant decreases in nicotine gum sales during the weeks encompassing New Year’s Day in 2002, 2003, and 2004). We found a 27% increase in nicotine patch sales during the week of the state tax increase and a 50% increase during the week of the city tax increase (risk ratios × 100 indicate percentage increaes) (Table 1 ▶). These percentages gradually declined over the ensuing weeks. Sales of nicotine gum increased by 7% and 10% following the rise in state and city cigarette taxes, respectively, but these increases generally did not persist for a period as long as the increases in nicotine patch sales.
TABLE 1—
Risk Ratios (95% Confidence Intervals) for Increased Sales of Nicotine Patches and Gum Before and After Implementation of Tobacco Control Measures and During the Weeks Encompassing New Year’s Day, With Temporal and Seasonal Trends Controlled: New York City, January 2002–January 2004
| Nicotine Patches | Nicotine Gum | |
| New Year 2002 | 1.27 (1.18, 1.37) | 0.94 (0.89, 1.00) |
| State cigarette tax increasea | ||
| Week −1 | 1.08 (0.99, 1.18) | 1.00 (0.95, 1.05) |
| Week 0 | 1.27 (1.19, 1.35) | 1.07 (1.02, 1.13) |
| Week +1 | 1.17 (1.09, 1.25) | 1.11 (1.05, 1.17) |
| Week +2 | 1.06 (0.99, 1.15) | 1.11 (1.05, 1.17) |
| Week +3 | 1.06 (1.00, 1.13) | 1.05 (0.99, 1.11) |
| Week +4 | 1.09 (1.01, 1.17) | 1.11 (1.05, 1.18) |
| City cigarette tax increaseb | ||
| Week −1 | 0.99 (0.92, 1.07) | 1.00 (0.95, 1.06) |
| Week 0 | 1.50 (1.40, 1.61) | 1.10 (1.02, 1.18) |
| Week +1 | 1.30 (1.21, 1.39) | 1.08 (1.02, 1.14) |
| Week +2 | 1.28 (1.19, 1.38) | 1.09 (1.03, 1.15) |
| Week +3 | 1.23 (1.14, 1.32) | 1.04 (0.98, 1.11) |
| Week +4 | 1.16 (1.07, 1.27) | 1.01 (0.96, 1.07) |
| New Year 2003 | 1.24 (1.16, 1.33) | 0.89f (0.83, 0.94) |
| Smoke-Free Air Actc | ||
| Week −1 | 1.02 (0.95, 1.10) | 0.95 (0.90, 1.00) |
| Week 0 | 1.31 (1.18, 1.45) | 1.08 (1.01, 1.16) |
| Week +1 | 1.20 (1.09, 1.31) | 0.91f (0.84, 0.99) |
| Week +2 | 1.17 (1.05, 1.27) | 1.00 (0.93, 1.08) |
| Week +3 | 1.08 (0.97, 1.20) | 0.99 (0.93, 1.07) |
| Week +4 | 1.07 (0.98, 1.17) | 1.11 (1.04, 1.18) |
| Free patch programd | 0.85f (0.80, 0.91) | 1.00 (0.95, 1.04) |
| New Year 2004 | 1.18 (1.07, 1.30) | 0.76 (0.69, 0.83) |
Note. A week is considered Sunday through Saturday. Thus, week 0 (the week of the event) for New Year 2002 was December 30, 2001, through January 5, 2002; week 0 for the state tax increase was March 31 through April 6, 2002; and so forth.
aImplemented April 3, 2002.
bImplemented July 2, 2002.
cImplemented March 30, 2003; enforcement began on April 27, 2003, in week +4.
dApril 2, 2003, through May 14, 2003.
The week of the implementation of the SFAA was associated with a 31% increase in nicotine patch sales and an 8% increase in nicotine gum sales, even though the free patch program began the same week (Table 1 ▶). Sales of the patch, but not the gum, declined during the subsequent weeks, corresponding with the duration of the 6 week free patch program. Gum sales increased by 11% during the fourth week after the SFAA was enacted, coinciding with the beginning of the act’s enforcement.
We did not find a similar pattern of excess sales of analgesics during the weeks of interest. The magnitudes of the estimated risk ratios for sales of analgesics were lower than those for the nicotine patch and gum, typically null or close to null (data not shown).
Geographic Analysis
Pharmacies located in Manhattan south of 59th Street accounted for 44% of all sales, and they had higher mean weekly sales of nicotine patches and nicotine gum than pharmacies in the rest of New York City. Pharmacies located in areas with the highest median incomes also had higher per-store sales of NRT products than those located in less affluent areas (data not shown).
Although nicotine patch sales increased in all areas following the state and city tax increases, stronger and more persistent increases were seen in the lowest-income areas than in higher-income areas (Table 2 ▶). The week prior to the implementation of the state tax increase was also associated with increases in sales in low- and medium-income areas. After the state and city tax increases, more persistent increases in nicotine gum sales were seen at pharmacies located south of 59th Street and those located in less affluent areas (Table 2 ▶). At pharmacies located in the high- and medium-income areas, nicotine gum sales increased only during the week of the city tax increase.
TABLE 2—
Risk Ratios (95% Confidence Intervals) for Increased Sales of Nicotine Patches and Gum Before and After Implementation of State and City Cigarette Tax Increases, by Pharmacy Location, With Temporal and Seasonal Trends Controlled: New York City, January 2002–January 2004
| Pharmacy Locationa | ||||
| Commuter Area (n = 73) | Low-Income Areas (n = 33) | Medium-Income Areas (n = 28) | High-Income Areas (n = 32) | |
| Nicotine patch | ||||
| State cigarette tax increaseb | ||||
| Week −1 | 1.01 (0.90, 1.13) | 1.30c (1.10, 1.54) | 1.29c (1.09, 1.53) | 1.00 (0.77, 1.31) |
| Week 0 | 1.29c (1.19, 1.39) | 1.24c (1.04, 1.48) | 1.15 (0.96, 1.38) | 1.25c (1.02, 1.53) |
| Week +1 | 1.07 (0.97, 1.16) | 1.38c (1.16, 1.64) | 1.35c (1.16, 1.58) | 1.19 (1.00, 1.42) |
| Week +2 | 1.06 (0.97, 1.17) | 1.12 (0.96, 1.32) | 0.95 (0.77, 1.17) | 1.09 (0.92, 1.29) |
| Week +3 | 1.06 (0.96, 1.16) | 1.05 (0.90, 1.23) | 1.01 (0.87, 1.18) | 1.10 (0.97, 1.25) |
| Week +4 | 1.09c (1.01, 1.19) | 1.15 (0.95, 1.39) | 1.11 (0.82, 1.50) | 1.03 (0.88, 1.21) |
| City cigarette tax increased | ||||
| Week −1 | 0.99 (0.89, 1.10) | 0.90 (0.75, 1.08) | 1.16 (0.95, 1.41) | 1.01 (0.87, 1.19) |
| Week 0 | 1.43c (1.29, 1.58) | 1.61c (1.42, 1.83) | 1.78c (1.53, 2.08) | 1.57c (1.38, 1.79) |
| Week +1 | 1.31c (1.19, 1.44) | 1.69c (1.45, 1.97) | 1.22c (1.05, 1.43) | 1.16 (0.97, 1.38) |
| Week +2 | 1.29c (1.18, 1.41) | 1.45c (1.24, 1.71) | 1.10 (0.91, 1.33) | 1.34c (1.05, 1.69) |
| Week +3 | 1.20c (1.08, 1.33) | 1.39c (1.16, 1.66) | 1.13 (0.97, 1.31) | 1.35c (1.12, 1.63) |
| Week +4 | 1.15c (1.03, 1.29) | 1.20c (1.02, 1.42) | 1.24c (1.05, 1.46) | 1.19 (0.92, 1.54) |
| Nicotine gum | ||||
| State cigarette tax increaseb | ||||
| Week −1 | 1.01 (0.95, 1.07) | 1.37c (1.17, 1.62) | 0.95 (0.80, 1.14) | 0.92 (0.74, 1.14) |
| Week 0 | 1.10c (1.03, 1.16) | 1.14 (0.87, 1.51) | 1.10 (0.92, 1.31) | 0.99 (0.84, 1.17) |
| Week +1 | 1.12c (1.06, 1.20) | 1.17 (0.87, 1.56) | 1.07 (0.88, 1.31) | 1.10 (0.94, 1.27) |
| Week +2 | 1.11c (1.04, 1.19) | 1.25c (1.04, 1.50) | 1.06 (0.93, 1.20) | 1.12 (0.98, 1.28) |
| Week +3 | 1.09c (1.02, 1.15) | 0.86 (0.68, 1.09) | 1.08 (0.87, 1.34) | 0.95 (0.79, 1.14) |
| Week +4 | 1.14c (1.07, 1.22) | 1.25 (0.88, 1.78) | 0.95 (0.79, 1.14) | 1.06 (0.91, 1.24) |
| City cigarette tax increasec | ||||
| Week −1 | 1.00 (0.94, 1.08) | 1.06 (0.79, 1.43) | 1.08 (0.95, 1.22) | 0.91 (0.77, 1.07) |
| Week 0 | 0.97 (0.89, 1.06) | 1.59c (1.24, 2.05) | 1.39c (1.11, 1.73) | 1.25c (1.09, 1.43) |
| Week +1 | 1.07c (1.00, 1.14) | 1.44c (1.18, 1.75) | 1.11 (0.92, 1.33) | 0.97 (0.82, 1.15) |
| Week +2 | 1.13c (1.08, 1.20) | 1.00 (0.77, 1.30) | 0.97 (0.83, 1.13) | 0.96 (0.76, 1.20) |
| Week +3 | 1.06 (0.99, 1.13) | 1.34c (1.06, 1.71) | 1.02 (0.85, 1.22) | 0.89 (0.71, 1.11) |
| Week +4 | 1.00 (0.93, 1.08) | 1.51c (1.27, 1.79) | 1.04 (0.90, 1.20) | 0.90 (0.76, 1.07) |
Note. A week was Sunday through Saturday; thus, week 0 (the week of the event) for the state tax increase was March 31 through April 6, 2002, and so forth.
aData for the analysis came from 166 pharmacies. Zip code areas located south of 59th Street in Manhattan were considered an area populated during the day by commuters; other zip codes were categorized by median annual income (low = less than $37 812, medium = $37 812–$55 413, High = more than $55 413).
bImplemented April 3, 2002.
cImplemented July 2, 2002.
DISCUSSION
Over-the-counter pharmacy sales data can be used to provide rapid validation of the efficacy of tobacco control policies. We found increases in nicotine patch and gum sales following implementation of 3 important smoking-related policies in New York City and New York State. The increases in sales of NRT products after the city and state tax increases were larger and more persistent in pharmacies in lower-income areas compared to those in higher-income areas.
These results are consistent with research indicating that increased taxation and smoke-free legislation are associated with increases in smoking cessation behaviors. Increased smoking cessation has also been observed in other areas with local public health ordinances that restrict worksite smoking.3,18,19 Furthermore, econometric analyses have shown that as the real price of cigarettes increases, the demand for cigarettes decreases and the demand for NRT products increases.3,20 Smokers with lower incomes are also more likely to reduce or quit smoking in response to a cigarette price increase.21 A large community health survey among New York City adults indicated that 15.8% of smokers quit or tried to quit in response to the city tax increase, while 4.2% quit or tried to quit in response to the SFAA.22
NRT product sales may be a reasonable proxy measure for smoking cessation attempts. Aggregate national retail sales of over-the-counter NRT products were previously found to have increased by 11% during the 4 weeks of the Great American Smokeout in 1996.11 Additionally, we observed increases in nicotine patch sales coincident with 3 consecutive New Year’s holidays, an observation compatible with previous evidence for increased smoking cessation associated with New Year’s resolutions.14,15 Because an estimated 60% of NRT purchases represent new smoking cessation attempts,23 our finding of increased NRT product sales coincident with the tax increases and the SFAA suggest that cessation attempts also increased in response to these measures.
The patterns of the increases in nicotine patch sales differed from those for nicotine gum; increases in patch sales were 4 times as high and more persistent during the weeks of the tax increases and the week of the SFAA. Some research suggests that the nicotine patch is preferred to nicotine gum as an aid to smoking cessation, particularly among smokers who have previously tried to quit using nicotine gum.24 Sales of nicotine gum actually decreased during New Year’s holidays, while patch sales increased significantly, suggesting that, in New York City, the nicotine patch may be the preferred product for quitting smoking. Interestingly, nicotine gum sales increased more in the commuter and low-income areas of the city following tax increases than in medium- and high-income areas, suggesting that nicotine gum may be used as a price-sensitive alternative to cigarettes for some individuals.
The data used in this analysis came from approximately 30% of the pharmacies in New York City.10 Most of these pharmacies were in Manhattan, with fewer stores in the other 4 boroughs. We have no evidence that these pharmacies differ systematically from other pharmacies in the city in terms of purchasing patterns or consumer behaviors, particularly in relation to the temporal trends we observed. Thus, the assumption that these results are generalizable to all pharmacies citywide is not unreasonable.
Even after controlling for seasonal and other temporal factors (including holidays), we found that the weekly variability in NRT sales was high, possibly owing to other patterns in consumer behaviors that we were not able to account for in the model. Despite this variability, we were able to see strong associations between NRT sales and times when smoking cessation would be expected to increase.
We extrapolated the results of this study to quantify, approximately, the number of citywide smoking cessation attempts associated with the tobacco control policies, a method previously used to estimate citywide burden of illness on the basis of emergency department visits.25 Although these estimates rely on a number of assumptions—particularly, that there is no bias in our results, that the results are generalizable to pharmacies citywide, that NRT purchases are representative of NRT-assisted cessation attempts, and that NRT-assisted cessation attempts are representative of all quit attempts—they provide us with some approximation of the effect of these policies on smoking cessation attempts in New York City.
For the city tax increase, we first calculated the number of excess sales of nicotine patches and nicotine gum by applying the percentage increase obtained from modeling for the week of and 4 weeks after the increase (Table 1 ▶) to the average weekly sales of each product. An average of 730 nicotine patch products (166 stores × 4.4 patch sales per week per store) and 1129 nicotine gum products (166 × 6.8 gum sales per week per store) were sold each week. For these 5 weeks, we estimated an excess of 1073 sales of the nicotine patch [730 × (0.50 + 0.30 + 0.28 + 0.23 + 0.16)] and an excess of 361 sales of nicotine gum [1129 × (0.10 + 0.08 + 0.09 + 0.04 + 0.01]. Because the pharmacies from which we obtained data constitute approximately 30% of pharmacies in New York City,10 we calculated that there were 4780 excess sales of the nicotine patch and nicotine gum citywide [(1073 + 361)/0.30]. Assuming that 60% of purchases were the initial purchase of a cessation aid,23 we estimated that 2868 nicotine patch and gum products were purchased for new cessation attempts (4780 × 0.60). Finally, because a 2002 survey of New York City adults found that 19% of smokers who attempted to quit used NRT products,26 we estimated that 15094 smoking cessation attempts (2868/0.19) were associated with the city tax increase in the short term. Using similar calculations, we estimated that 10337 smoking cessation attempts were associated with the state tax increase and 8621 attempts were associated with the SFAA. Finally, sales of nicotine patches only declined by an estimated 3067 units during the 6-week free patch program, suggesting that the majority of the 35000 free courses of therapy distributed during the program represented additional quit attempts by individuals who would not have otherwise tried to quit smoking.
Increases in cigarette excise taxes and implementation of smoke-free workplace legislation can be expected to encourage cessation, decrease smoking prevalence, and, in the longer term, reduce smoking-related morbidity and mortality. Electronic retail data can be used to help understand smoking cessation behaviors, target cessation activities, and provide a rapid assessment of tobacco control initiatives. Routinely collected electronic data that are gathered for syndromic surveillance may also prove useful in other public health priority areas.
Acknowledgments
This research was supported by Centers for Disease Control and Prevention Cooperative Agreement U90/CCU 2241298—Public Health Preparedness and Response for Bioterrorism.
The authors thank Rick Heffernan and Debjani Das in the Syndromic Surveillance Unit of the Bureau of Communicable Disease for their assistance with the data.
Human Participant Protection No human participants were involved in this study.
Peer Reviewed
Contributors K.B. Metzger designed the study, conducted the analysis, and led the interpretation of the findings and the writing of the article. F. Mostashari conceived and designed the study and participated in the interpretation of the findings and the writing of the article. B.D. Kerker participated in the interpretation of the findings and the writing of the article.
References
- 1.Chaloupka FJ, Warner KE. The economics of smoking. In: Culver AJ, Newhouse JP, eds. Handbook of Health Economics. Vol 1B. Amsterdam, Netherlands: Elsevier; 2000:1539–1627.
- 2.Fichtenberg CM, Glantz SA. Association of the California tobacco control program with declines in cigarette consumption and mortality from heart disease. N Engl J Med. 2000;343:1772–1777. [DOI] [PubMed] [Google Scholar]
- 3.Reducing Tobacco Use: A Report of the Surgeon General. Atlanta, Ga: National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000.
- 4.Wilson N, Thomson G. Still dying from secondhand smoke at work: a brief review of the evidence for smoke-free workplaces in New Zealand. N Z Med J. 2002;115:240–249. [PubMed] [Google Scholar]
- 5.Fiore MC, Croyle RT, Curry SJ, et al. Preventing 3 million premature deaths and helping 5 million smokers quit: a national action plan for tobacco cessation. Am J Public Health. 2004;94:205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henning KJ. What is syndromic surveillance? MMWR Morb Mortal Wkly Rep. 2004;53(suppl):7–11. [Google Scholar]
- 7.Mostashari F, Hartman J. Syndromic surveillance: a local perspective. J Urban Health. 2003;80(suppl 1): i1–i7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heffernan R, Mostashari F, Das D, Karpati A, Kulldorff M, Weiss D. Syndromic surveillance in public health practice, New York City. Emerg Infect Dis. 2004; 10:585–864. [DOI] [PubMed] [Google Scholar]
- 9.Mostashari F, Fine A, Das D, Adams J, Layton M. Use of ambulance dispatch data as an early warning system for community wide influenza like illness, New York City. J Urban Health. 2003;80(suppl 1):i43–i49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Das D, Mostashari F, Weiss D, Balter S, Heffernan R. Monitoring over-the-counter pharmacy sales for early outbreak detection in New York City [abstract]. MMWR Morb Mortal Wkly. 2004;53(suppl):235. [Google Scholar]
- 11.Burton SL, Kemper KE, Baxter TA, Shiffman S, Gitchell J, Currence C. Impact of promotion of the Great American Smokeout and availability of over-the-counter nicotine medications, 1996. MMWR Mortal Wkly Rep. 1997;46:867–871. [PubMed] [Google Scholar]
- 12.New York City Smoke-Free Air Act, Chapter 5, Title 17 of the New York City Administration Code as amended by Local Law no. 47, 2003.
- 13.Miller N, Frieden TR, Liu SY, et al. Effectiveness of a large-scale free nicotine patch distribution program. Lancet. In press. [DOI] [PubMed]
- 14.Norcross JC, Vangarelli DJ. The resolution solution: longitudinal examination of New Year’s change attempts. J Subst Abuse. 1989;1:127–134. [DOI] [PubMed] [Google Scholar]
- 15.Walsh RA, Paul CL. New Year quit smoking resolutions. Aust N Z J Public Health. 2002;26:181. [DOI] [PubMed] [Google Scholar]
- 16.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 17.Census 2000 Summary File 3. New York: US Census Bureau; 2001. Available at: http://www.census.gov/prod/cen2000/doc/sf3.pdf. Accessed May 3, 2005.
- 18.Tauras JA. The Transition to Smoking Cessation: Evidence From Multiple Failure Duration Analysis. Cambridge, Mass: National Bureau of Economic Research; 1999. NBER Working Paper 7412. Available at: http://www.nber.org/papers/w7412. Accessed February 2, 2004.
- 19.Moskowitz JM, Lin Z, Hudes ES. The impact of workplace smoking ordinances in California on smoking cessation. Am J Public Health. 2000;90:757–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tauras JA, Chaloupka FJ. The demand for nicotine replacement therapies. Nicotine Tob Res. 2003;5:237–243. [DOI] [PubMed] [Google Scholar]
- 21.Farralley MC, Bray JW. Response to increases in cigarette prices by race/ethnicity, income and age groups—United States, 1976–1993. MMWR Morb Mortal Wkly Rep. 1998;47:605–609. [PubMed] [Google Scholar]
- 22.Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health. 2005;95:1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaw JP, Ferry DG, Pethica D, Brenner D, Tucker IG. Usage patterns of transdermal nicotine when purchased as a non-prescription medicine from pharmacies. Tob Control. 1998;7:161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.West R, Hajek P, Nilsson F, Foulds J, May S, Meadows A. Individual differences in preference for and responses to four nicotine replacement products. Psychopharmacology. 2001;153:225–230. [DOI] [PubMed] [Google Scholar]
- 25.Metzger KB, Hajat A, Crawford M, Mostashari F. How many illnesses does one emergency department visit represent? Use of a population-based telephone survey to estimate the syndromic multiplier. MMWR Morb Mortal Wkly Rep. 2004;53(suppl):106–111. [PubMed] [Google Scholar]
- 26.Mostashari F, Kerker BD, Hajat A, Miller N, Frieden TR. Smoking practices in New York City: the use of a population-based survey to guide policy-making and programming. J Urban Health. 2005;82:58–70. [DOI] [PMC free article] [PubMed] [Google Scholar]