Abstract
The term “rural” suggests many things to many people, such as agricultural landscapes, isolation, small towns, and low population density.
However, defining “rural” for health policy and research purposes requires researchers and policy analysts to specify which aspects of rurality are most relevant to the topic at hand and then select an appropriate definition. Rural and urban taxonomies often do not discuss important demographic, cultural, and economic differences across rural places—differences that have major implications for policy and research. Factors such as geographic scale and region also must be considered.
Several useful rural taxonomies are discussed and compared in this article. Careful attention to the definition of “rural” is required for effectively targeting policy and research aimed at improving the health of rural Americans.
THE UNITED STATES HAS evolved from a rural agricultural society to a society dominated by its urban population. Depending on which definition is used, roughly 20% of the US population resides within rural areas. Approximately three fourths of the nation’s counties are rural, as is 75% of its landmass. While the rural population is in the minority, it is the size of France’s total (rural and urban) population.
As important as the rural population and its resources are to the nation, there is considerable confusion as to exactly what rural means and where rural populations reside. We will discuss defining rural and why it is important to do so in the context of health care policy and research.
WHAT DOES RURAL LOOK LIKE?
Although many policymakers, researchers, and policy analysts would prefer one standardized, all-purpose definition, “rural” is a multifaceted concept about which there is no universal agreement. Defining rurality can be elusive and frequently relies on stereotypes and personal experiences. The term suggests pastoral landscapes, unique demographic structures and settlement patterns, isolation, low population density, extractive economic activities, and distinct sociocultural milieus. But these aspects of rurality fail to completely define “rural.” For example, rural cultures can exist in urban places.1 Only a small fraction of the rural population is involved in farming, and towns range from tens of thousands to a handful of residents. The proximity of rural areas to urban cores and services may range from a few miles to hundreds of miles. Generations of rural sociologists, demographers, and geographers have struggled with these concepts.2,3
Despite the theoretical limitations of the concept of rurality, it is very useful as a practical analytic and policy tool. Common definitions of rurality are the basis for many policy decisions, including criteria for the allocation of the nation’s limited resources. It is important to specify which aspects of rurality are relevant to the phenomenon being examined and then use a definition that captures those elements. Only by defining “rural” appropriately to the situation at hand can we discern differences in health care concerns and outcomes across rural areas and between rural and urban locales. The definition of rurality used for one purpose may be inappropriate or inadequate for another.1
WHEN IS RURAL NOT SO RURAL?
Rural and urban taxonomies, researchers, policy analysts, and legislation generally view all rural areas as uniform in character. However, there are, in fact, huge variations in the demography, economics, culture, and environmental characteristics of different rural places. Large rural towns that are not too distant from larger metropolitan areas often have more in common with metropolitan areas than they do with remote and isolated small towns. By treating these diverse types of rural cities and towns and the problems they confront similarly, policy analysts may fail to identify each site’s distinct health care concerns and effective methods for resolving those problems. Access to medical specialists and surgical services is a case in point. The absence of certain services in a small place is expected. The lack of such services in a larger rural place might be construed as a critical provider shortage. A small rural town’s population base may only support 1 or 2 generalist physicians and a nurse practitioner or physician assistant. A larger rural town, whose geographic service area may include the small town, may serve as a regional center for accessing specialists and surgeons. Health planning, recruitment and retention, and identifying and optimizing the supply and mix of providers are going to be different in each place.1,4
HOW IS RURAL DIFFERENT?
On average, rural populations have relatively more elderly people and children, higher unemployment and underemployment rates, and lower population density with higher percentages of poor, uninsured, and underinsured residents. Rural populations are more vulnerable than their urban counterparts to economic downturns because of their concentrated economic specialization. Other unique circumstances include longer travel distances to—and higher costs associated with—needed health care services; diseconomies of scale; high rates of fixed overhead per-patient revenue; fewer health care providers and a greater emphasis on generalists; health care facilities with limited scopes of service; economically fragile hospitals with high closure rates; greater dependency on Medicare and Medicaid reimbursement; higher rates of chronic diseases; and different clinical practice behaviors, practice arrangements, and reimbursement levels.5–8 Hong and Kindig9 found that residents of counties with larger numbers of workers who commute out of the county and who travel more than 30 minutes each way to reach their care providers received substantially lower levels of health resources. Access to proximate services for care often makes the difference between life and death.10
The environment in which rural physicians and other providers practice also differs enormously both across rural areas and between rural and urban areas.11–13 Physicians who practice in smaller and more remote rural towns practice in a medical care delivery system characterized by financially vulnerable medical organizations, small populations, long distances to specialists and tertiary hospitals, longer practice hours, lack of collegial support, limited access to advanced technologies, and relatively high fixed costs per delivered service. This milieu creates especially difficult circumstances for rural providers and populations.14 Rural physician practice concerns—patient privacy, clinical adaptations in the absence of nearby specialists, generalist scarcities, quality assurance programs, compliance with the Health Insurance Portability and Accountability Act of 1996 regulations, and continuing medical education—are different from those of their large city contemporaries, differences that have a potential impact on health outcomes. For example, studies have shown substantial differences between rural and urban physicians in clinical prenatal and intrapartum practice styles for similar low-risk patients, without apparent differences in outcome,15 and that physician attitudes regarding physician-assisted suicide vary dramatically by rural or urban practice location and practitioner gender.16 While there are many common threads between urban clinical medicine and its rural cousin, there are many substantive differences.7,8,17,18
HOW DO ACCURATE DEFINITIONS HELP?
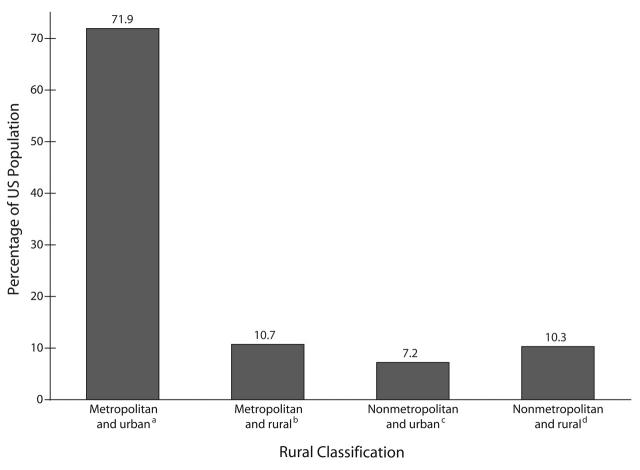
The federal government defines “rural” in a variety of ways. The Office of Management and Budget’s (OMB) definition of metropolitan and nonmetropolitan populations and the Census Bureau’s definition of rural and urban fail to identify the same populations as rural. When the 2 definitions were cross-tabulated for the 2000 census, 72% of the population was classified as both metropolitan (OMB definition) and urban (Census Bureau definition), while 10% was classified as nonmetropolitan and rural (Figure 1 ▶). However, nearly 18% of the nation’s population was divided between the 2 taxonomies: 11% were metropolitan but rural, and 7% were non-metropolitan but urban. Depending on how the categories are combined, the rural population can vary from 10% to 28% of the nation’s total (i.e., a population of 29–79 million). Research findings and policies may appear to conflict when those findings and policies are based on different rural definitions and populations. The use of noncongruent definitions of rural may result in markedly different conclusions and policy implications.
FIGURE 1—
Comparison of metropolitan and nonmetropolitan classifications with urban and rural classifications, by proportion of 2000 US population (N = 281 421 898): 2000 Census Bureau data.
Note. “Metropolitan” and “nonmetropolitan” are Office of Management and Budget terminology; “urban” and “rural” are Census Bureau terminology.
an = 202 000 000.
bn = 30 000 000.
cn = 20 000 000.
dn = 29 000 000.
Another problem associated with defining “rural” is that conventional definitions use a single rural classification and thereby fail to differentiate categories of rurality. Rural areas are not homogeneous across the nation, and aggregating rural areas of differing sizes and levels of remoteness may obscure emerging problems at the local level. As a result, policies may fail to include appropriate intrarural targeting.
Rural and urban taxonomies have usually been developed based on population size, density, proximity, degree of urbanization, adjacency and relationship to a metropolitan area, principal economic activity, economic and trade relationships, and work commutes. An appropriate rural and urban taxonomy should (1) measure something explicit and meaningful; (2) be replicable; (3) be derived from available, high-quality data; (4) be quantifiable and not subjective, and (5) have on-the-ground validity.
To some extent, all definitions will either underbound or over-bound rurality. Some large counties, for example, have large cities and less densely settled areas that may be considered rural in terms of economic activities, landscape, and service level. However, because of the presence of a large urban core the entire county is often considered urban. In this case, “rural” is being underbounded—areas that might reasonably be called rural are actually being classified as urban. At the same time, “urban” is being overbounded. A certain amount of overbounding and underbounding is inherent to any definition of rurality; the researcher must simply be aware of this problem when evaluating data across the rural and urban dimension.1(p15)
Because numerous taxonomies have been used to categorize the rural/urban continuum, we examined the 4 that are most often applied (Table 1 ▶).
TABLE 1—
Comparison of Commonly Applied Rural Taxonomiesa
| Geographical Unit | Characteristics | Strengths | Weaknesses | |
| OMB Metropolitan/Nonmetropolitan | County | This OMB definition is used extensively in federal policy. Significant 2003 update with 2000 census data. Counties are assigned as metropolitan (n = 1090) or nonmetropolitan (n = 2052). Nonmetropolitan counties are now designated as micropolitan or noncore based on the presence of an urban cluster (areas with a population less than 50 000 but greater than 2500 people) with a population of 10 000 or more. In 2000, 17.4% of the US population resided in nonmetropolitan counties. |
Useful for a general definition of rural status. The methodology and county assignments were significantly changed in 2003. Underlying geographic unit (county) is very stable over time. | Substantial underbounding of rurality in many large metropolitan counties. The large size of counties often obscures intracounty differences. |
| ERS Urban Influence Codes | County | Metropolitan counties are grouped into 2 categories based on size of urban population. Nonmetropolitan counties are grouped into 7 categories based on size of largest city in county and adjacency/nonadjacency to a metropolitan county. Updated with significant changes associated with the OMB metropolitan/nonmetropolitan definition changes in 2003 on the basis of 2000 census data. |
Use of largest city criterion, which differentiates counties with several small towns from those with 1 or 2 large towns for grouping nonmetropolitan counties, may be better than RUCA method for suggesting level of locally available services. Adjacency criteria may be suggestive of degree of economic integration with metropolitan county. | Overbounding and underbounding occurs just as in OMB metropolitan and nonmetropolitan categories. Does not differentiate metropolitan counties as well as does RUCA. The large size of counties often obscures intracounty differences. |
| Census Bureau Rural and Urban | Census tract | Census Bureau definition of rurality based on census tracts. Rural census tracts are those outside of urbanized areas and clusters with populations of 2500 or greater that do not have substantial commuting In 2000, 21% of the US population lived in rural areas. |
Helps reduce problems of underbounding and overbounding associated with county-based terminology. | Data other than census data are infrequently collected by census tract. Difficult to apply to health data that are often collected at the county or zip code area levels. Lack of familiarity of most data users with census tract geography and terminology. Not stable across census years—there were substantial changes for the 2000 census. |
| RUCA | Census tract | Multitiered taxonomy developed by University of Washington and the Economic Research Service, with funding from the Federal Office of Rural Health Policy and the Economic Research Service. Uses census commuting data to classify census tracts on the basis of geography and work commuting flows between places. Updated in spring 2005 with 2000 census data. |
Use of work commuting data strongly differentiates rural areas according to their economic integration with urban areas and other rural areas. Very sensitive to demographic change. The structure of the codes allows for many levels of generalization—from 2 groups (rural and urban) to 33. | Difficult to apply to health data that are often collected at the county or zip code area levels. Will not be stable over time. Complex structure of codes not easy to master for casual users. |
| RUCA–zip code approximation | US Postal Service zip code areas | Multitiered system developed by University of Washington, with funding from the Office of Rural Health Policy. Census work commuting data are used to classify census tracts on the basis of geography and work commuting activity between places. Approximates the census tract RUCA codes for 2000 zip codes. Updated in spring 2005 with 2000 census data and 2004 zip codes. |
Use of commuting data strongly differentiates rural areas according to their economic integration with urban areas and other rural areas. Very sensitive to demographic change. The structure of the codes allows for many levels of generalization—from 2 groups (rural/urban) to 33. Use of the zip code unit makes them useful with a wide variety of data collected at that level, including health data. | Complex structure of codes is not easy to master for casual users. The underlying geographic unit is subject to some change by the US Postal Service across time. |
Source. aAdapted from Larson and Hart.1
Note. OMB = Office of Management and Budget; RUCA = Rural–Urban Commuting Area.
OMB Metropolitan and Nonmetropolitan Taxonomy
The federal government most frequently uses the county-based OMB metropolitan and non-metropolitan classifications as policy tools. These county-based definitions are the foundation for other, more detailed taxonomies and are used when determining eligibility and reimbursement levels for more than 30 federal programs, including Medicare reimbursement levels, the Medicare Incentive Payment program, and programs designed to ameliorate provider shortages in rural areas.4
Metropolitan areas were defined in 2003 as central counties with 1 or more urbanized areas (cities with a population greater than or equal to 50000) and outlying counties that are economically tied to the core, which was measured by commuting to work. The United States has 1090 metropolitan counties and 2052 nonmetropolitan counties (674 micropolitan and 1378 non-core) that have (according to 2002 census data) 239 million metropolitan and 49 million non-metropolitan residents, of whom 29 million lived in micropolitan counties and 20 million lived in noncore counties. Micropolitan counties are those nonmetropolitan counties with a rural cluster with a population of 10000 or more. Noncore counties are the residual. The most significant problem with this taxonomy is that county boundaries both overbound and underbound their urban cores. The metropolitan and nonmetropolitan taxonomy was most recently updated in 2003 in accordance with the 2000 census data.
US Department of Agriculture Economic Research Service Urban Influence Codes
The Urban Influence Codes (UIC) taxonomy is a county-based definition that builds on the OMB metropolitan and nonmetropolitan dichotomy. Counties are classified into 9 groups: 2 metropolitan and 7 nonmetropolitan. The nonmetropolitan counties are grouped according to their adjacency and nonadjacency to metropolitan counties and the size of the largest urban settlement within the county. To qualify as adjacent to a metropolitan county, a nonmetropolitan county must share a boundary with a metropolitan county and must meet a minimum work commuting threshold.1 The UICs’ use of the size of the largest town in a county is as a taxonomic criterion. The largest town, as used for health care purposes, is associated with the likelihood of local availability of hospitals, clinics, and specialty services. While the codes are often used for research, they are infrequently used in federal and state policies. In 2003, the UICs were updated in accordance with 2000 census data.
Census Bureau Rural and Urban Taxonomy
The Census Bureau partitions urban areas into urbanized areas and urban clusters. The same census tract–based criteria are used for both; however, the urbanized areas have cores with populations of 50 000 or more, and the urban clusters have cores with populations that range from 2500 to 49 999. All other areas are designated as rural. The nation has more than 65 000 census tracts that are made up of blocks and block groups. In 2000, 59 million residents—21% of the US population—were deemed rural by the Census Bureau taxonomy. The Census Bureau’s rural and urban taxonomy is the source of much of the available demographic and economic data. A weakness of this system with regard to health care policy is the paucity of health-related data at the census tract level. The Census Bureau and others often aggregate urban clusters with urbanized-area data. Depending on the purpose at hand, this may be misleading for rural health policymakers. For example, a town with a population of 3000 in a very remote area is considered urban under the Census Bureau definition, but that same town is often nonmetropolitan under the OMB definition.
Rural/Urban Commuting-Area Taxonomy
A recently developed taxonomy uses census tract–level demographic and work-commuting data to define 33 categories of rural and urban census tracts.19 The Rural–Urban Commuting Areas (RUCAs) were developed and are maintained by the University of Washington Rural Health Research Center and the USDA Economic Research Service (ERS), with the support of the federal Health Resource and Service Administration’s Office of Rural Health Policy and the ERS. (For more information about RUCAs, see http://www.fammed.washington.edu/wwamirhrc and http://www.ers.usda.gov.) The RUCA categories are based on the size of settlements and towns as delineated by the Census Bureau and the functional relationships between places as measured by tract-level work-commuting data. For example, a small town where the majority of commuting is to a large city is distinguished from a similarly sized town where there is commuting connectivity primarily to other small towns. Because 33 categories can be unwieldy, the codes were designed to be aggregated in various ways that highlight different aspects of connectivity, rural and urban settlement, and isolation, aspects that facilitate better program intervention targeting. The census tract version of the RUCAs has been supplemented by a zip code–based version. There are more than 30000 zip code areas.
RUCAs range from the core areas of urbanized areas to isolated small rural places, where the population is less than 2500 and where there is no meaningful work commuting to urbanized areas. While the zip code version of the RUCAs is slightly less precise than the census tract version, the RUCA zip codes have an advantage in the health field because they can be used with zip code health-related data. The RUCAs are widely used for policy and research purposes (e.g., by the Centers for Medicare and Medicaid Services and many researchers). RUCAs can identify the rural portions of metropolitan counties and the urban portions of nonmetropolitan counties.
RUCAs are flexible and can be grouped in many ways to suit particular analytic or policy purposes. For example, there is a tool that provides the road mileage and the travel time along the fastest route between each zip code area and the nearest edge of a core in an urbanized area and the closest large rural city. When this tool is used with the RUCA codes, users can identify highly isolated “frontier” areas—counties with 6 or fewer persons per square mile—in a more precise manner than with previous definitions. The RUCA taxonomy was updated in the spring of 2005.
Other Taxonomies
Common taxonomies that have been designed for related purposes include (1) ERS’s Rural–Urban Continuum Codes, (2) ERS’s Economic Typology of Nonmetropolitan Counties, and (3) frontier areas, which is a crude measure at best. The term “frontier” is a problematic term for research purposes, because it has a very different meaning for demographers and geographers.20 There also are many rural and urban definitions developed by the states for various geographic scales. For an introduction to older rural and urban taxonomies, see Hewitt.21 Other taxonomies that lend themselves to use with the rural and urban taxonomies include the new county-based amenity index.22
Other schemes regionalize the nation or individual states for diverse uses, for example, ambulatory care utilization via the national Primary Care Service Areas.23 The federal government has used taxonomies and measures to allocate resources to rural and urban areas. In these schemes, factors such as physician-to-population ratios, infant mortality rate, poverty, and resident age are used to rate geographic units (combinations of counties, census tracts, facilities, populations, etc.) and to delineate those places and populations most in need of federal health care resources. These methods (e.g., Health Professional Shortage Areas) have significant flaws, and efforts are being made to substantially revise them.
How Have OMB and Census Bureau Methodologies Changed After the 2000 Census?
Despite the common assumption that Census Bureau and OMB methodologies change little between decennial censuses, about a quarter of the census tract boundaries changed between the 1990 and 2000 censuses, and the number of counties designated as metropolitan by OMB in 2003 based on 2000 census data increased by 27%. Many of these changes have important policy consequences. For example, researchers and analysts who examine data across years, when different definitions were in place, need to be aware of these changes and adjust result analyses and interpretations accordingly. (For more detailed information about methodological changes in the Census, see the US Census Bureau and ERS Web sites at http://www.census.gov and http://www.ers.usda.gov, and see Slifkin, Randolph, and Ricketts.24–26) While it is beyond the scope of this article to describe all of the concerns associated with new methodologies, 2 are most noteworthy.
There is some confusion about a new OMB metropolitan and nonmetropolitan taxonomy category: micropolitan—an urban cluster with a population that ranges from 10 000 to 49 999. While some of the designation criteria have undergone subtle changes, the micropolitan counties have historically been designated as nonmetropolitan. Unfortunately, the term micropolitan has led some to think of these counties as being urban or metropolitan in nature. However, changing the terminology does not make these counties any more or any less rural and urban than they were before—historically rural, albeit larger rural towns/cities. Micropolitan counties could just as well have been titled macrorural or large rural counties. A general problem with the creation of so many taxonomies is that they take on a life of their own and are often used without considering the suitability or meaning of the category.27
The 2003 update of the metropolitan and nonmetropolitan taxonomy resulted in a net gain of 253 counties in the metropolitan ranks (now 1090 counties). This also resulted in a net loss of 7.3 million residents who would have been counted, in accordance with the older definition, as nonmetropolitan. Whether or not the rural population is shrinking depends on how the question is asked. As rural counties and cities grow, they are designated as being metropolitan and urban. Thus, because these rural populations are no longer counted as non-metropolitan or rural, it appears that the nation’s rural population is shrinking or stagnant. However, according to Dr Calvin Beale (senior demographer, ERS), if the 1993 nonmetropolitan definition is held constant, the overall population change between 1990 and 2000 shows an 11% increase compared with a 13% increase for the nation (written communication, March 2004). Nevertheless, some rural areas are experiencing population loss.28
GEOGRAPHIC SCALE AND DATA AVAILABILITY
Another problem associated with rural health research involves the geographical level of available data. Typical units used for the collection of health and demographic data include states, counties, municipalities, census tracts, and zip codes. The county is a convenient and frequently used unit of analysis, and many health-related data are collected at this level. However, the large geographic size of counties, and the failure to distinguish between the demographic and economic heterogeneity that often exists within counties, can weaken the meaningfulness of policy analyses. Both the strengths and weaknesses of any given definition are strongly rooted in the underlying geographic unit used in the definition.1 As already noted, some degree of overbounding and underbounding is inherent in any definition of rurality. It is important to consider which way the “error” goes when evaluating data and policy.1 The more mixing of diverse groups within units of analysis, the more difficult it is to show real differences between groups.
Rural data from federal surveillance systems and surveys are extremely limited,18 and funds for rural surveys are scarce, both of which impede rural health research and policy analysis. Better rural health research methods and tools are needed to produce meaningful findings. Substantial progress has been made recently in data procurement and methods because of focused funding from the Health Resource and Service Administration’s Office of Rural Health Policy, the Bureau of Health Professions, and the Bureau of Primary Health Care. To maximize the utility of these new methods, they must be widely disseminated to state offices of rural health, primary care officers, and researchers and analysts.29–31
WHY ARE DIFFERENTIATED LEVELS OF RURALITY NOT GENERALLY USED?
Federal and state policies tend to treat rural areas as a single entity for several reasons. First, the political process often requires that a significant coalition be formed to pass rural-related legislation, and it is more expedient to lump than to divide. Second, policymakers and legislators often do not understand rural variability and diversity or the methods for making these distinctions. Third, self-interest often prevails, wherein people advocate greater selectivity and more effective targeting as long as they do not lose anything in the process—regardless of what they may also gain. Finally, in some cases the availability of data at different geographic scales dictates the geographic unit that is used in policies.
WHY SHOULD WE CARE?
Definitions of rural are the basis for targeting resources to underserved rural populations. If the only outcome of clarifying the definition were an improved mechanism for funneling health care to where it is needed most, the clarification would be well worth the effort. Because there are 50 to 60 million rural residents in the nation, decisions about resource use have significant ramifications in terms of the dollars spent and the well-being of rural populations. Inappropriate definitions may bias research findings and policy analyses and may result in different conclusions than those that are based on another unit of analysis (often called the modifiable unit problem).32 The more we aggregate different types of rural areas, the less we can pinpoint localized health care and delivery problems at the state, region, county, town, or zip code levels.
We examined the 2000 American Medical Association Master-file data on the nation’s physician distribution and found that the most remote UIC subgroup of counties had a generalist physician–to-population ratio of 46.4 per 100 000 population. When we examined these same data with the census tract version of the RUCA taxonomy, we found a much lower ratio of 38.5 per 100 000 population—17% lower. For resource allocation purposes, where money is spent is clearly influenced by how that locale is defined. A recent study of acute myocardial infarction that used zip code–based RUCAs10 found substantial rural and urban and intrarural differences in the use of needed initial hospital services, where a previous county-based study found little difference.33 (For a comprehensive explanation of the policy consequences of rural definitions, see Hewitt.21) Health care researchers focus great attention and time on statistical methodologies; however, geographical methodologies are often neglected.34 Expert geographic consultation should be sought when determining the most appropriate geographical unit and rural definition to use in a given analysis.
CONCLUSIONS
Deciding which rural definition to apply to an area depends on the purpose at hand, the availability of data, and the appropriate and available taxonomy. There is no perfect rural definition that meets all purposes. Researchers must be deliberate and insightful when defining rural and when applying the appropriate definition and its associated taxonomy to program targeting, intervention, and research. It is recommended that researchers familiarize themselves with various rural definitions and geographic methodologies and then carefully weigh the pros and cons of available definitions. Defining rural and urban must be a methodological priority at the start of any project that examines health-related concerns associated with the rural and urban dimension. Grappling early and systematically with the problems of defining rurality will significantly enhance the validity and the utility of health research work, which is essential in rural-focused health research.
Peer Reviewed
Contributors L. G. Hart originated the study and was the principal writer. E. H. Larson helped develop the study and wrote and edited portions of the article. D. M. Lishner edited the article.
Human Participant Protection No protocol approval was needed for this study.
References
- 1.Larson EH, Hart LG. Rural health workforce methods and analysis. In: Larson EH, Johnson KE, Norris TE, et al., eds. State of the Health Workforce in Rural America: State Profiles and Comparisons. Seattle, Wash: WWAMI Rural Health Research Center, University of Washington; 2003:15–22.
- 2.Miller MK, Luloff AE. Who is rural? A typological approach to the examination of rurality. Rural Sociol.1981;46:608–625. [Google Scholar]
- 3.Miller KM, Farmer FL, Clarke LL. Rural populations and their health. In: Beaulieu JE, Berry DE, eds. Rural Health Services: A Management Perspective. Ann Arbor, Mich: AUPHA Press/ Health Administration Press; 1994: 3–26.
- 4.Council on Graduate Medical Education. Tenth Report: Physician Distribution and Health Care Challenges in Rural and Inner-City Areas. Washington, DC: Government Printing Office; 1998.
- 5.Hassenger EW, Hobbs DJ. Rural society—the environment of rural health care. In: Straub LA, Walzer N, eds. Rural Health Care: Innovation in a Changing Environment. Westport, Conn: Praeger; 1992:178–190.
- 6.Ricketts TC III. The rural patient. In: Geyman JP, Norris TE, Hart LG, eds. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001:15–26.
- 7.Geyman JP, Norris TE, Hart LG. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001.
- 8.Loue S, Quill BE. Handbook of Rural Health. New York, NY: Kluwer Academic/Plenum Publishers; 2001.
- 9.Hong W, Kindig DA. The relationship between commuting patterns and health resources in nonmetropolitan counties of the United States. Med Care.1992;30:1154–1158. [DOI] [PubMed] [Google Scholar]
- 10.Baldwin L-M, MacLehose RF, Hart LG, Beaver SK, Every N, Chan L. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health.2004;20:99–108. [DOI] [PubMed] [Google Scholar]
- 11.Ricketts TC III, Johnson-Webb KD, Randolph RK. Populations and places in rural America. In: Ricketts TC III, ed. Rural Health in the United States. New York, NY: Oxford University Press; 1999.
- 12.Fuguitt GV, Brown DL, Beale CL. Rural and Small Town America. New York, NY: Russell Sage Foundation; 1989.
- 13.Hart JF. The Rural Landscape. Baltimore, MD: John Hopkins University Press; 1998.
- 14.Rosenblatt RA. The health of rural people and the communities and environments in which they live. In: Geyman JP, Norris TE, Hart LG, eds. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001:3–14.
- 15.Hart LG, Dobi.e., SA, Baldwin LM, Pirani MJ, Fordyce M, Rosenblatt RA. Rural and urban differences in physician resource use for low-risk obstetrics. Health Serv Res.1996;31:429–452. [PMC free article] [PubMed] [Google Scholar]
- 16.Hart LG, Norris TE, Lishner DM. Attitudes of family physicians in Washington State toward physician-assisted suicide. J Rural Health.2003;19: 461–469. [DOI] [PubMed] [Google Scholar]
- 17.Yawn BP, Bushy A, Yawn RA. Exploring Rural Medicine: Current Issues and Concepts. Thousand Oaks, Calif: Sage Publications; 1994.
- 18.Ricketts TC III, ed. Rural Health in the United States. New York, NY: Oxford University Press; 1999.
- 19.Morrill R, Cronmartie J, Hart LG. Metropolitan, urban, and rural commuting areas: toward a better depiction of the US settlement system. Urban Geography.1999;20:727–748. [Google Scholar]
- 20.Popper DE, Lang RE, Popper FJ. From maps to myth: the census, Turner, and the idea of the frontier. J Am Comp Cult. 2000;Spring:91–102.
- 21.Hewitt M. Defining “Rural” Areas: Impact on Health Care Policy and Research. Washington, DC: US Government Printing Office; 1989. US Office of Technology Assessment Staff Paper.
- 22.McGranahan DA. Natural Amenities Drive Rural Population Change. Washington, DC: Economic Research Service, US Department of Agriculture; 1999. Agricultural Economic Report No. 781.
- 23.Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res.2003;38(1 Pt 1): 287–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slifkin RT, Randolph R, Ricketts TC. The changing metropolitan designation process and rural America. J Rural Health.2004;20:1–6. [DOI] [PubMed] [Google Scholar]
- 25.US Census Bureau. Census Bureau Home Page. Available at: http://www.census.gov. Accessed June 25, 2004.
- 26.Economic Research Service. Economic Research Service—USDA. Available at: http://www.ers.usda.gov. Accessed June 25, 2004.
- 27.Ratcliffe MR. Creating metropolitan and micropolitan statistical areas. Paper presented at: American Sociological Association Annual Meeting; August 19, 2002; Chicago, Ill.
- 28.McGranahan DA, Beale CL. Understanding rural population loss. Rural Am.2002;17:2–11. [Google Scholar]
- 29.Ricketts TC III, Savitz LA, Gesler WM, Osborne DN. Geographic Methods for Health Service Research. New York, NY: University Press of America; 1994.
- 30.Hart LG, Taylor P. The emergence of federal rural policy in the United States. In: Geyman JP, Norris TE, Hart LG, eds. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001:73–90.
- 31.Hart LG, Salsberg E, Phillips DM, Lishner DM. Rural health care providers in the United States. J Rural Health.2002;18(suppl):211–232. [DOI] [PubMed] [Google Scholar]
- 32.Openshaw S, Taylor PJ. The modifiable areal unit problem. In: Wrigley N, Bennet RJ, eds. Quantitative Geography: a British View. London, UK: Routledge & Kegan Paul; 1981:60–69.
- 33.Medicare Payment Advisory Commission. Report to the Congress: Medicare in Rural America. Washington, DC: Medicare Payment Advisory Commission; 2001.
- 34.Thomas R. Geomedical Systems: Intervention and Control. London, UK: Routledge; 1992.