Abstract
Objectives. To estimate the contribution of stress-related and physical work factors to occupational class disparities in sickness absence from work.
Methods. Our sample consisted of 8847 men and 2886 women participating in the French GAZEL cohort study. Occupational class and medically certified sickness absence data (1995–2001) were obtained from the participants’ employer. Work characteristics (physical and stress-related) were self-reported. We calculated rate ratios with Poisson regression models; fractions of sickness absence attributable to work factors were estimated with the Miettinen formula.
Results. Sickness absence was distributed along an occupational gradient. Work characteristics accounted for 19% (women) and 21% (men) of all absences. Physical work conditions accounted for 42% and 13% of absences for musculoskeletal reasons, and work stress accounted for 48% and 40% of psychiatric absences. Overall, about 20% of the occupational class gradient in sickness absence could have been associated with deleterious work conditions.
Conclusion. Work conditions contribute to sickness absence, particularly among manual workers and clerks. Policies that decrease ergonomic constraints and work stress also could reduce the burden of ill health and sickness absence among the lowest strata of working populations.
Among working populations, occupational hazards and job stress may contribute to occupational class disparities in health.1 Specifically, adverse work conditions may influence the risk of musculoskeletal disorders, psychiatric symptoms, and injury that occur frequently among middle-aged populations and may constitute some of the leading reasons for taking sick leave.2,3 There is some evidence that job stress contributes to occupational class differences in both health and sickness-related absence from work (sickness absence)4,5; however, little research has examined the contribution of other work conditions. To date, only 2 studies have investigated the joint contribution of physical and psychosocial work characteristics to occupational class health disparities; however, both were cross-sectional and used self-reported health as an outcome.6,7
In a previous analysis of the GAZEL cohort study, we showed that job stress is most prevalent among manual workers and office clerks and predicts the occurrence of sickness absence.8 In this study, we examined the contribution of both stress-related and physical work exposures to the occupational class gradient in overall and cause-specific sick leave.
METHODS
Study Population
The GAZEL cohort study began in 1989, when 44 922 employees of France’s national gas and electricity company, Electricité de France-Gaz de France (EDF-GDF), were asked to participate in a long-term observational study. Forty-five percent of those eligible—14 752 men and 5317 women—accepted. At baseline, men were aged 40 to 50, and women were aged 35 to 50 years old. Women represented only 20% of company employees and therefore were oversampled.9
EDF-GDF employees hold a civil servant–like status that entails job stability and opportunities for occupational mobility. Typically, employees are hired when they are in their 20s and stay with the company until retirement (usually around 55 years of age). Retirees’ pensions are paid by the company. Because of these characteristics, study follow-up is very thorough: since baseline (1989), less than 1% of participants were lost to follow-up (39 left the company, and 19 withdrew from the study).
GAZEL participants are followed with an annual mailed survey, which is usually completed by 75% of the cohort.9 Additionally, participants’ records are linked to validated occupational and health data collected by the company, including medically certified sickness absence.
In this study, we analyzed data from GAZEL participants who responded to the 1995 survey (11183 men and 4095 women; 75% of the original cohort), which included measures of job stress. We excluded respondents who had retired (n=2304) or who had incomplete work exposure data, which left a sample of 8847 men and 2886 women. The study population was healthier than GAZEL participants who did not complete the 1995 questionnaire.8
Person-time of follow-up with regard to the outcome—sickness absence—was accrued from the date of completion of the 1995 GAZEL survey until the date of retirement, death, withdrawal from EDF-GDF or the GAZEL cohort, or December 31, 2001 (whichever occurred first).
Measures
Occupational class in 1995, which was obtained from company records, was coded in accordance with the French national job classification: manual workers, clerks, foremen/ technicians, administrative associate professionals, engineers, and managers. There were no female manual workers in our study population.
Other explanatory variables were collected from GAZEL surveys. Physical work characteristics, including postural constraints (7 items), occupational hazards (5 items), night work (yes or no), and outdoor work activities (never, sometimes, > 50% of the time) were measured in 1990 (Table 1 ▶). These were the only measures of physical work exposures available to us. For postural constraints and occupational hazards, we summed all the relevant items into summary scales, with ranges of 0 to 4 and 0 to 7, respectively. The questionnaire also included a question about customer contact (yes or no), which we considered to be potentially stressful.
TABLE 1—
Work Characteristics and Sickness Absence, by Gender and Participants’ Occupational Class: the GAZEL Cohort Study, 1995–2001
| Manager | Engineer | Associate Professional | Foreman/Technician | Clerk | Manual Worker | P | RR (95% CI)a | |
| Men (n = 8307) | ||||||||
| Percentage of study population | 17.7 | 23.1 | 12.7 | 36.7 | 2.7 | 7.1 | . . . | |
| Postural constraints, mean (SD) | 0.15 (0.43) | 0.22 (0.53) | 0.30 (0.65) | 0.78 (0.81) | 0.57 (0.81) | 1.68 (1.29) | <.0001 | 1.60 (1.47–1.73) |
| Hazardous work conditions, mean (SD) | 0.53 (1.04) | 1.33 (1.73) | 0.53 (1.05) | 2.29 (1.87) | 0.87 (1.29) | 3.04 (1.55) | <.0001 | 1.28 (1.18–1.38) |
| Night work, % | 22.3 | 42.2 | 18.5 | 53.2 | 21.5 | 68.5 | <.0001 | 1.10 (1.02–1.19) |
| Work outdoors, % | <.0001 | |||||||
| Sometimes | 34.2 | 47.9 | 30.4 | 52.9 | 28.3 | 16.1 | 1.05 (0.97–1.15) | |
| 50% of time | 1.7 | 3.6 | 13.5 | 29.6 | 19.3 | 80.4 | 1.59 (1.44–1.75) | |
| Customer contact, % | 24.5 | 21.7 | 50.8 | 38.0 | 69.0 | 77.0 | <.0001 | 1.19 (1.10–1.29) |
| Low decision latitude, % | 14.9 | 17.7 | 32.1 | 39.9 | 73.9 | 67.2 | <.0001 | 1.64 (1.54–1.75) |
| High psychological demands, % | 52.3 | 52.8 | 44.8 | 38.7 | 41.7 | 32.1 | <.0001 | 0.90 (0.83–0.96) |
| Low social support at work, % | 36.0 | 31.3 | 38.9 | 32.9 | 49.2 | 38.2 | <.0001 | 1.28 (1.20–1.36) |
| Sick leave taken 1 or more times, % | 56.8 | 52.7 | 71.4 | 72.7 | 87.4 | 80.5 | <.0001 | . . . |
| Women (n = 2886) | ||||||||
| Percentage of study population | 7.4 | 5.1 | 58.3 | 10.9 | 18.3 | . . . | ||
| Postural constraints, mean (SD) | 0.04 (0.20) | 0.12 (0.45) | 0.16 (0.44) | 0.28 (0.59) | 0.20 (0.44) | . . . | <.0001 | 1.39 (1.24–1.56) |
| Hazardous work conditions, mean (SD) | 0.07 (0.28) | 0.29 (0.87) | 0.15 (0.48) | 0.34 (0.82) | 0.14 (0.43) | . . . | <.0001 | 1.11 (0.97–1.27) |
| Night work, % | 5.6 | 12.2 | 2.4 | 4.4 | 0.8 | . . . | <.0001 | 0.83 (0.62–1.11) |
| Work outdoors, % | <.0001 | |||||||
| Sometimes | 7.5 | 9.8 | 8.3 | 14.3 | 3.0 | . . . | 0.97 (0.82–1.15) | |
| 50% of time | . . . | . . . | . . . | . . . | . . . | . . . | . . . | |
| Customer contact, % | 21.7 | 14.9 | 35.4 | 27.4 | 56.8 | . . . | <.0001 | 1.24 (1.13–1.36) |
| Low decision latitude, % | 18.9 | 20.9 | 51.5 | 53.1 | 74.4 | . . . | <.0001 | 1.34 (1.23–1.45) |
| High psychological demands, % | 56.1 | 61.5 | 40.7 | 29.6 | 40.3 | . . . | <.0001 | 1.17 (1.05–1.31) |
| Low social support at work, % | 53.3 | 52.7 | 52.7 | 48.7 | 61.7 | . . . | <.0001 | 1.06 (0.97–1.15) |
| Sick leave taken 1 or more times, % | 70.7 | 75.6 | 86.8 | 85.3 | 92.0 | . . . | <.0001 | . . . |
Note. CI = confidence interval.aAge-adjusted rate ratios of all-cause sickness-related absences from work. For postural constraints and hazardous work conditions, participants who reported any level of exposure were compared to the nonexposed.
Job stress measures, which were based on the work of Karasek and Johnson,10,11 were obtained in 1995: control over the content and the execution of work-related tasks (6 items); psychological demands, evaluated work load, and time pressures (5 items); and social support received from colleagues (5 items). Each summary scale showed satisfactory factorial validity and adequate internal consistency reliability, with Cronbach α coefficients of 0.65 for decision latitude, 0.69 for psychological demands, and 0.52 for work social support (our measure of work social support showed lower reliability than in other studies because it included fewer items).12 After verifying that the association between quartiles of psychosocial work factors and sickness absence was graded (data not shown), we dichotomized each scale at its median value.13 To examine the contribution of work factors to the occupational gradient, we modeled job stress factors as continuous variables.14
Demographic and behavioral characteristics measured in 1995 included age (45–49, 50–54, and 55–56 years for men, and 42–44, 45–49, 50–54, and 55–56 years for women), marital status (married/living with a partner, single, or divorced), current smoking (none vs at least 1 cigarette per day), alcohol consumption in drinks per week (none, light [1–13 for men, 1–6 for women], intermediate [14–27 for men, 7–20 for women], or heavy [≥ 28 for men, ≥ 21 for women), body mass index (underweight [< 20], normal [20–24.9], overweight [25–29.9], and obese [≥ 30 kg/m2]), and the occurrence of stressful life events (divorce or separation, partner’s death, death of another family member, partner’s hospitalization, or partner’s unemployment) during the preceding 12 months (0, 1, 2, or more). The number of dependents, as a covariate, did not predict the occurrence of sickness absence and was not included in our analysis.
Sickness Absence Data
Sickness absence data (date, length, and medically certified diagnosis) were obtained from EDF-GDF company records. In principle, the medical cause of all occurrences of sickness absence is verified by company physicians and is recorded in accordance with a classification derived from the International Classification of Diseases (ICD; Ninth Edition for all nonpsychiatric diagnoses; for psychiatric disease, Ninth Edition until January 1, 1997, and 10th Edition thereafter).14,15 In our data, the underlying diagnosis was missing for 35% of the absences, 85% of which lasted less than 8 days. We studied sick leave due to all medical causes and the 4 most common medical causes: respiratory illness (ICD 9 460–519), disorders of the musculoskeletal system (ICD 9 710–739), psychiatric disease (ICD 9 299–305; ICD 10 F10–F99), and injury (work and nonwork related, EDF-GDF’s own classification). Absences due to less common or unknown medical reasons were classified as “other.” In secondary analyses, we examined the occurrence of short (≤ 7 days), intermediate (8–21 days), and long ( > 21 days) absences.
Statistical Analysis
Sickness absence occurrence was expressed in rates of absences over 100 person-years of observation. Rate ratios of sickness absence were computed with log-linear Poisson regression models. Sickness absence during any calendar year was correlated with future absences (by a factor of 0.5), which could have led us to overestimate the variance of the Poisson regression parameters. Therefore, all standard errors were adjusted with a scale parameter equivalent to the residual deviance divided by the number of degrees of freedom.16
The contribution of work factors to the occupational class gradient in sickness absence was evaluated in 4 steps. First, with managers as the reference category, we calculated rate ratios across occupational groups and adjusted for age, demographic characteristics, and health behaviors (Model 1). Next, we successively added physical work factors (Model 2) and job stress (Model 3) before including all work and adjustment variables in a single statistical model (Model 4). The contribution of work factors to the occupational gradient was measured by fitting a linear term for occupational class and comparing Models 4 and 1 (we show Models 1 and 4; more detailed data are available upon request). Additionally, we estimated the fraction of sickness absence attributable to work factors with the Miettinen formula (attributable fraction = [RR–1] / RR [no. exposed cases / no. cases]).17 For each work exposure statistically significant in Model 4, the attributable fraction was calculated controlling only for adjustment variables; the contribution of all work factors was calculated controlling for all work factors and adjustment variables.
We verified the consistency of the results in a subsample restricted to participants who worked in the same occupation in both 1990 and 1995 (n = 8830) by using different lengths of sickness absence (≤ 7 days, 8–21 days, > 21 days) as an outcome. We tested reverse causation by repeating the analyses in a “healthy” subsample composed of participants who did not experience sickness absence during the year preceding the beginning of follow-up (n = 7632).
All analyses were conducted separately for men and women with SAS, version 8.2 (SAS Institute Inc, Cary, NC); log-linear Poisson regression models were fitted with the PROC GENMOD procedure.18
RESULTS
The study population included 8847 men and 2886 women, on average, aged 50 years (range = 47–56) and 48 years (range = 42–56), respectively (Table 1 ▶). Men were most likely to work as technicians (37%), engineers (23%), or managers (18%); a majority of women worked in administrative jobs (58% in intermediate-grade positions, 18% as clerks). The proportion of manual workers was lower than among the French population of the same age. Eighty percent of participants worked in the same occupation in both 1995 and 1990, when physical work characteristics were measured.
Over the 6 years of follow-up (mean = 4.8, SD = 2.0 for men; mean = 5.8, SD = 1.72 for women), there were 18 818 absences among men and 15 803 female absences. On average, men experienced 47 absences per 100 person-years of observation, and women experienced 95; corresponding median numbers of sick leave days were 8 and 36, respectively. Most absences (58%) lasted 7 days or less, 26% lasted 8 to 21 days, and 17% lasted more than 21 days. Respiratory illness (14%) and musculoskeletal disorders (14%) were the leading causes of absence, followed by psychiatric reasons (7%) and injury (6%).
Manual workers and office clerks more frequently reported job stress and physical work exposures (Table 1 ▶). Male office clerks were more likely to be unmarried, to smoke cigarettes, and to abstain from alcohol; manual workers reported the highest alcohol consumption and were more likely to be obese. Among women, clerks were most likely to be divorced and obese, but smoking and alcohol consumption were more frequent among managers (data not shown).
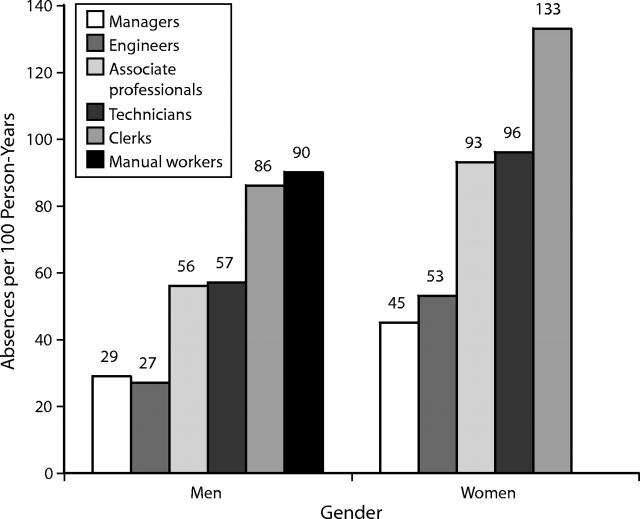
As expected, sickness absence occurred along an occupational gradient (Figure 1 ▶) and was associated with work factors (Table 2 ▶). After we adjusted for age, demographic characteristics, and health behaviors, manual workers and clerks had rates of absence that were 3 times higher than the rates of managers (Table3 ▶, Model 1), regardless of the length of absence (data not shown). Occupational class disparities were greatest for absences owing to musculoskeletal causes (men and women) and injury (men only). Work factors contributed to these occupational class differences (Table3 ▶, Model 4): physical exposures among men who had musculoskeletal- and injury-related sickness absences (particularly if the injury occurred at work), and work stress among men and women who had musculoskeletal- and psychiatric-related sickness absence.
FIGURE 1—
Occupational class and sickness absence, by gender, in the GAZEL cohort study, 1995–2001.
TABLE 2—
Occupational Class Gradients in Sickness Absence (1995–2001) and the Contribution of Work Factors: the GAZEL Cohort Study, 1995–2001
| Total Sickness Absence RR (95% CI) | Respiratory Illness RR (95% CI) | Musculoskeletal Cause RR (95% CI) | Psychiatric Diagnosis RR (95% CI) | Injury RR (95% CI) | Other Diagnosis RR (95% CI) | |
| Men | ||||||
| No. absences | 18 818 absences | 2721 absences | 2945 absences | 1015 absences | 1339 absences | 10 798 absences |
| Model 1: adjusted for age, demographics, health behaviors | ||||||
| Manager | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Engineer | 0.95 (0.85, 1.08) | 1.14 (0.90, 1.44) | 1.05 (0.79, 1.39) | 0.67 (0.41, 1.10) | 1.22 (0.89, 1.68) | 0.91 (0.80, 1.04) |
| Administrative associate professional | 1.89 (1.68, 2.13) | 2.74 (2.19, 3.42) | 2.20 (1.67, 2.90) | 2.82 (1.88, 4.22) | 2.20 (1.60, 3.02) | 1.59 (1.39, 1.82) |
| Foreman/Technician | 1.97 (1.78, 2.18) | 2.92 (2.40, 3.56) | 2.84 (2.24, 3.59) | 1.63 (1.11, 2.38) | 3.07 (2.35, 4.01) | 1.62 (1.44, 1.81) |
| Clerk | 2.88 (2.46, 3.38) | 3.61 (2.67, 4.88) | 3.91 (2.76, 5.53) | 3.17 (1.80, 5.58) | 3.02 (1.93, 4.70) | 2.55 (2.12, 3.06) |
| Manual worker | 3.06 (2.70, 3.45) | 4.21 (3.33, 0.31) | 5.83 (4.49, 7.57) | 2.60 (1.63, 4.16) | 4.58 (3.35, 6.27) | 2.31 (2.00, 2.67) |
| Model 4: Model 1+ work factors | ||||||
| Manager | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Engineer | 0.96 (0.85, 1.08) | 1.14 (0.89, 1.43) | 1.04 (0.79, 1.38) | 0.68 (0.42, 1.10) | 1.21 (0.88, 1.67) | 0.91 (0.81, 1.04) |
| Administrative associate professional | 1.79 (1.59, 2.01) | 2.58 (2.06, 3.23) | 1.99 (1.51, 2.61) | 2.54 (1.70, 3.79) | 2.08 (1.51, 2.87) | 1.51 (1.32, 1.73) |
| Foreman/Technician | 1.82 (1.63, 2.03) | 2.70 (2.18, 3.35) | 2.26 (1.75, 2.91) | 1.57 (1.03, 2.37) | 2.73 (2.03, 3.68) | 1.52 (1.34, 1.72) |
| Clerk | 2.42 (2.05, 2.85) | 2.93 (2.13, 4.03) | 2.84 (1.97, 4.09) | 2.03 (1.11, 3.70) | 2.52 (1.58, 4.03) | 2.09 (1.73, 2.54) |
| Manual worker | 2.59 (2.23, 3.01) | 3.66 (2.75, 4.87) | 3.53 (2.56, 4.85) | 2.28 (1.28, 4.05) | 3.51 (2.38, 5.16) | 2.03 (1.73, 2.54) |
| Women | ||||||
| No. absences | 15 803 absences | 2242 absences | 1970 absences | 1564 absences | 754 absences | 9273 absences |
| Model 1: adjusted for age, demographics, health behaviors | ||||||
| Manager | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Engineer | 1.20 (0.88, 1.63) | 1.16 (0.65, 2.10) | 1.99 (1.02, 3.89) | 0.72 (0.29, 1.77) | 1.25 (0.63, 2.47) | 1.16 (0.83-, .61) |
| Administrative associate professional | 1.99 (1.61, 2.46) | 2.56 (1.71, 3.84) | 2.64 (1.57, 4.45) | 2.01 (1.18, 3.41) | 1.63 (1.01, 2.63) | 1.83 (1.46, 2.31) |
| Foreman/Technician | 2.07 (1.63, 2.62) | 2.44 (1.56, 3.80) | 2.97 (1.69, 5.22) | 1.73 (0.95, 3.17) | 1.78 (1.03, 3.05) | 1.96 (1.52, 2.53) |
| Clerk | 2.76 (2.21, 3.44) | 3.71 (2.45, 5.61) | 4.15 (2.44, 7.07) | 3.14 (1.82, 5.40) | 2.33 (1.41, 3.82) | 2.39 (1.88, 3.03) |
| Model 4: Model 1+ work factors | ||||||
| Manager | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Engineer | 1.18 (0.88, 1.60) | 1.16 (0.64, 2.08) | 1.92 (1.00, 3.68) | 0.73 (0.30, 1.74) | 1.28 (0.65, 2.50) | 1.15 (0.83, 1.60) |
| Administrative associate professional | 1.80 (1.46, 2.23) | 2.42 (1.61, 3.62) | 2.26 (1.35, 3.76) | 1.70 (1.00, 2.86) | 1.53 (0.95, 2.47) | 1.69 (1.34, 2.13) |
| Foreman/Technician | 1.88 (1.48, 0.39) | 2.36 (1.51, 3.69) | 2.40 (1.37, 4.17) | 1.54 (0.85, 2.79) | 1.69 (0.98, 2.92) | 1.82 (1.41, 2.36) |
| Clerk | 2.30 (1.84, 2.89) | 3.22 (2.10, 4.93) | 3.20 (1.87, 5.46) | 2.17 (1.24, 3.78) | 2.04 (1.21, 3.42) | 2.03 (1.58, 2.60) |
Note. RR = relative ratio; CI = confidence interval.
aBased on 39 647 person-years of observation.
bBased on 20 509 person-years of observation.
TABLE 3—
Population Fraction of Sickness Absence Attributable to Work Factors, by Cause: the GAZEL Cohort Study, 1995–2001
| All Causes, % | Musculoskeletal Reasons, % | Psychiatric Reasons, % | Injury, % | |||||
| Men | Women | Men | Women | Men | Women | Men | Women | |
| Postural constraints | 10 | 4 | 24 | 9 | a | 6 | 15 | 4 |
| Occupational hazards | 6 | 1 | 12 | 3 | . . . | . . . | 6 | . . . |
| Night work | . . . | . . . | . . . | < 1 | . . . | . . . | . . . | . . . |
| Outdoor work activities | . . . | 6 | 1 | . . . | < 1 | . . . | 2 | |
| Customer contact | . . . | 4 | . . . | 2 | . . . | 9 | . . . | 9 |
| Low decision latitude | 9 | 9 | 15 | 15 | 13 | 19 | 7 | . . . |
| High psychological demands | < 1 | 4 | . . . | . . . | 11 | 7 | . . . | 4 |
| Low social support at work | 8 | 2 | 10 | . . . | 24 | 5 | . . . | 10 |
| All work factorsb | 21 | 19 | 46 | 27 | 42 | 43 | 26 | 26 |
a The exposure was not significantly associated with the outcome in a model that adjusted for age, marital status, occupational class, cigarette smoking, alcohol consumption, body mass index, and life events.
b The fraction of sickness absence attributable to all work factors was estimated in models that included all work exposures and that were adjusted for age, marital status, occupational class, cigarette smoking, alcohol consumption, body mass index, and life events.
Adjustment for all work factors reduced the occupational class gradient in all-cause sickness absence by 16% for men and 25% for women; musculoskeletal absences were reduced by 27% and 25%, and psychiatric absences were reduced by 10% and 40%. Work factors’ contribution was greatest with regard to men and women’s gradient in absences of 8 to 21 days (21% and 27%, respectively) and was less for short and long absences (13 days and 26 days; 9% and 20%, respectively). Associations between occupational class and work factors and sickness absence(s) were weaker among healthier participants than among the full sample. All-cause absenteeism rates among manual workers and clerks were 2 times higher than among managers, which is 30% lower than among the entire study population, and work factors’ contribution to men and women’s occupational gradients were 35% and 70% lower.
Across occupational groups, 21% of men’s and 19% of women’s all-cause sickness absences were attributable to work factors (Table 3 ▶). Postural constraints accounted for 24% of men’s musculoskeletal-related absences and for 15% of their injury-related absences. Work stress contributed to musculoskeletal-related absences (15% for low decision latitude) and psychiatric-related absences (a lack of social support among men; low decision latitude among women).
DISCUSSION
Main Results
Overall, 19% to 21% of all-cause sickness absences and 16% to 25% of the occupational class gradient in absenteeism were related to adverse work conditions. Adding to previous research,19 we found that occupational gradients in cause-specific sickness absences were associated with physical and psychosocial work exposures. Occupational class differences in sickness absences due to injury were associated with physical work exposures, and work stress contributed to psychiatric sickness absence gradients. Sickness absence due to musculoskeletal reasons reflected both physical and stress-related work exposures.
Limitations
Our study has several limitations. First, work exposures were self-reported and may have reflected personality factors for which we could not control, such as negative affectivity. However, our measures of psychosocial work characteristics have previously been validated,8,20,21 and postural constraints and occupational hazards predicted the occurrence of sickness absence owing to musculoskeletal causes and injury, which is plausible. Furthermore, sickness absence data were obtained from company records, which limited the influence of reporting bias. Nonetheless, it is possible that individuals who complain about their work conditions are also likely to take sick leave for reasons other than health. Future research should test the role of more objective measures of work characteristics.
A second limitation is that physical work exposures were obtained 5 years before the beginning of follow-up, which may have resulted in measurement error. About 80% of participants held the same job in both 1990 and 1995, and results among this subgroup were comparable to the full sample, which is reassuring. However, it is possible that levels of exposure change over time, even within occupational groups, which may have reduced the precision of our estimates.
Third, to calculate attributable fractions, we dichotomized work-stress variables at their median value. Although this is the standard method used in the field, we recognize that it makes comparisons with other studies difficult. To our knowledge, work stress in GAZEL was as frequent as in other studies,22 and our results are valid among other populations. However, identifying meaningful work-stress exposure thresholds, which would make comparisons across study populations more straightforward, is an important goal for future research.
Finally, we studied employees of a large public sector company who were healthier than the general population of France,23 and we probably underestimated both occupational class differences in sickness absence and the role of work factors. At the same time, GAZEL participants’ jobs are not at stake if they take sick leave, and they may be less reluctant to be absent from work when ill than men and women who are in more unstable job situations.24 Other large cohorts, such as the Whitehall II study, faced similar issues.4 In our study, sickness absence rates were somewhat lower than among the White-hall II cohort, but not by very much (47 and 95 absences per 100 person-years for GAZEL men and women, respectively, compared with 70 and 120 absences, respectively, in the Whitehall II study). Therefore, our findings can be compared with previous reports from that cohort.4 Yet, more broadly, it is important to recognize that sickness absence patterns vary across work sectors, workplaces, time periods, countries, and study populations, and their association with occupational factors needs to be studied among other working populations.
Gender Differences
Patterns and causes of sickness absence and distributions of jobs and work factors vary by gender. In our study, men were more likely to work as manual workers, report numerous postural constraints, and seek sickness absence due to musculoskeletal problems; women were more likely to work in white collar jobs, suffer from work stress, and show susceptibility to psychiatric sickness absence. Even within broad occupational groups, job titles differed between men and women. For instance, female managers held jobs with lower responsibility levels than men, and although female clerks often worked as receptionists, male clerks were in positions with less frequent customer contact (e.g., administrative staff). It is important to keep these gender specificities in mind when studying occupational gradients in both sickness absence and health.
Work Factors and Sickness Absence
The global contribution of work factors to the occupational gradient in sickness absence reflects several mechanisms, some of which are occupation- and gender-specific. Postural constraints encompass a wide array of exposures that increase the risk for disorders of or injury to the back, neck, shoulder, and upper limbs.2,25 Some of these are characteristic of manual occupations (e.g., carrying heavy loads, experiencing vibrations), while others also occur in office jobs (e.g., standing or sitting in uncomfortable positions over extended periods of time). To gain a better understanding of occupational gradients in specific diseases of the musculoskeletal system, studies that use more precise postural exposures are necessary.
The health effects of work stress may be due to direct and indirect mechanisms. The specific pathways of musculoskeletal problems are not yet well understood, but increased muscle tension and the inability to take necessary breaks from work are the most likely explanations.25 Low job control and insufficient support from colleagues and supervisors may directly undermine psychological well-being and thus increase the risk for depression5 while simultaneously affecting health behaviors (e.g., cigarette smoking, alcohol consumption, and behaviors that result in being overweight).26,27
Manual workers and clerks are simultaneously exposed to a variety of deleterious work factors, some of which can be interrelated. For example, occupational hazards may cause stress. In our study, work variables showed at most modest collinearity, and we chose to include them jointly in our statistical models. We assumed that the effects of physical and stress-related factors were additive; however, we acknowledge that other approaches are possible (e.g., multiplicative models).
An important question when interpreting our results is whether the association between work factors and sickness absence can be considered causal. Indeed, it may be that individuals whose work conditions are the worst and who are employed in subordinate jobs are also exposed to nonwork situations associated with sickness absence (e.g., comorbidity or a lack of personal social support). More broadly, thought needs to be given to the complex associations between work exposures, nonwork characteristics, and sickness absence, including their patterning along occupational class lines.
Sickness Absence as a Measure of Health
Sickness absence reflects not only health but also attitudes toward health and work, as well as job authority. We were concerned that managers may miss work for health reasons without requesting sick leave, particularly for short periods of time. Reassuringly, in our study occupational gradients were similar across different durations of sickness absence, which suggests that our measure was adequate across occupational groups.
Despite potential biases that may have affected reports of sickness absence, this indicator bears public health relevance because it reflects individuals’ general physical, psychological, and social well-being8,28–30 and collective workplace factors (e.g., it is lower in workplaces that have equitable policies).31 Organizations and employees are embedded within a broader social, political, and economic context, and sickness absence also reflects the generosity of sick leave provisions and macroeconomic trends (e.g., downsizing of firms and contingent job insecurity).32,33 The population effects of these macrolevel factors, which we did not take into account because we restricted our study to middle-aged employees of a single company with high levels of job security, deserve further research attention.
Health Selection into Occupational Groups
We hypothesized that higher sickness absence rates among manual workers and clerks would partly reflect detrimental work conditions. Yet, individuals are not randomly selected into occupations, and health influences occupational attainment. In France, salaried workers undergo a medical examination before starting a new job, and the GAZEL cohort did not include individuals who were severely ill when recruited by EDF-GDF. However, less healthy individuals were probably less likely to be promoted34: in our study, 39% of male office clerks previously held a manual occupation and may have switched to an office-based job for health reasons. Furthermore, occupational class and work characteristics were less strongly associated with sickness absence among participants who had not experienced sickness absence during the preceding year, which, along with findings from other populations, suggests that both health-related selection and social causation contribute to occupational class health disparities.34–36 Additional longitudinal studies are needed to disentangle the role of these 2 processes.
Conclusions
In the GAZEL study, work conditions account for approximately 20% of occupational class differences in sickness absence. Our study did not include extremely disadvantaged workers, and our results probably underestimate the effect of work on health-related absenteeism among the general population. Policies that decrease postural constraints and job stress have the potential to improve the health of men and women who work in manual and clerical jobs and to reduce the burden of sickness absence, particularly when associated with musculoskeletal problems and psychiatric reasons.
Acknowledgments
The authors wish to thank EDF-GDF and the men and women who participate in the GAZEL study. We particularly thank the Service des Etudes Médicales, Service Général de Médecine de Contrôle, who collected the sickness absence data. We are grateful to the GAZEL cohort study team, particularly Sébastien Bonenfant, who is responsible for data management. Additionally, we thank Alice Guégen for statistical advice, and David Ellwood, Annette Leclerc, Doris V. Báez-Feliciano, and an anonymous reviewer for their comments on previous versions of the article.
Human Participant Protection The GAZEL cohort received the approval of France’s national ethics committee (Commission Nationale Informatique et Liberte); our study was conducted with the approval of the human subjects committee of the Harvard School of Public Health.
Peer Reviewed
Contributors M. Melchior designed the study, performed the analyses, and wrote the article. N. Krieger, I. Kawachi, L. F. Berkman, and M. Goldberg helped design the study and interpret the findings. I. Niedhammer originated the study and assisted with study design.
References
- 1.Goldberg M, Melchior M, Leclerc A, Lert F. Epidémiologie et déterminants sociaux des inégalités de santé. Rev Epidemiol Sante Publique. 2003;51: 381–401. [PubMed] [Google Scholar]
- 2.Hoogendoorn WE, Bongers PM, de Vet HC, Ariens GA, van Mechelen W, Bouter LM. High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med. 2002; 59:323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paterniti S, Niedhammer I, Lang T, Consoli SM. Psychosocial factors at work, personality traits and depressive symptoms. Longitudinal results from the GAZEL Study. Br J Psychiatry. 2002;181:111–117. [PubMed] [Google Scholar]
- 4.North F, Syme SL, Feeney A, Shipley M, Marmot MG. Psychosocial work environment and sickness absence among British civil servants: the Whitehall II study. Am J Public Health. 1996;86: 332–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stansfeld SA, Head J, Marmot MG. Explaining social class differences in depression and well-being. Soc Psychiatry Psychiatr Epidemiol. 1998;33:1–9. [DOI] [PubMed] [Google Scholar]
- 6.Schrijvers CT, van der Mheen HD, Stronks K, Mackenbach JP. Socioeconomic inequalities in health in the working population: the contribution of working conditions. Int J Epidemiol. 1998;27:1011–1018. [DOI] [PubMed] [Google Scholar]
- 7.Borrell C, Muntaner C, Benach J, Artazcoz L. Social class and self-reported health status among men and women: what is the role of work organisation, household material standards, and household labour? Soc Sci Med. 2004;58:1869–1887. [DOI] [PubMed] [Google Scholar]
- 8.Melchior M, Niedhammer I, Berkman LF, Gold-berg M. Psychosocial work factors, social relations, and sickness absence: a 6-year prospective study of the GAZEL cohort. J Epidemiol Community Health. 2003; 57:285–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldberg M, Leclerc A, Chastang J, Morcet J, Marne M, Luce D. Mise en place d’une cohorte épidémiologique à Electricité de France—Gaz de France: principales caractéristiques de l’échantillon. Rev Epidemiol Sante Publique. 1990;38:378–380. [Google Scholar]
- 10.Karasek R, Theorell T. Healthy Work: Stress, Productivity and the Reconstruction of Working Life. New York, NY: Basic Books; 1990.
- 11.Johnson J, Hall E, Theorell T. Combined effects of job strain and social isolation on cardiovascular disease morbidity and mortality in a random sample of the Swedish male working population. Scand J Work Environ Health. 1989;15:271–279. [DOI] [PubMed] [Google Scholar]
- 12.Stansfeld SA, Bosma H, Hemingway H, Marmot MG. Psychosocial work characteristics and social support as predictors of SF-36 health functioning: the Whitehall II study. Psychosom Med. 1998;60: 247–255. [DOI] [PubMed] [Google Scholar]
- 13.Landsbergis P, Theorell T. Measurement of psychosocial workplace exposure variables. Occup Med. 2000;15:163–188. [PubMed] [Google Scholar]
- 14.International Classification of Diseases. Manual of the International Statistical Classification of Diseases, Injuries and Causes of Death. Geneva, Switzerland: World Health Organization; 1977.
- 15.International Classification of Diseases: 10th Revision. Geneva, Switzerland: World Health Organization; 1992.
- 16.Niedhammer I, Bugel I, Goldberg M, Leclerc A, Guegen A. Psychosocial factors at work and sickness absence in the Gazel cohort: a prospective study. Occup Environ Med. 1998;55:735–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanley J. A heuristic approach to the formulas for population attributable fraction. J Epidemiol Community Health. 2001;55:508–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SAS Institute. SAS/STAT Software: Changes and Enhancements Through Release 6.12. Cary, NC: SAS Institute; 1997.
- 19.North F, Syme SL, Feeney A, Head J, Shipley MJ, Marmot MG. Explaining socioeconomic differences in sickness absence: the Whitehall II study. Br Med J. 1993;306:361–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niedhammer I. Psychometric properties of the French version of the Karasek Job Content Questionnaire: a study of the scales of decision latitude, psychological demands, social support and physical demands. Int Arch Occup Environ Health. 2002;75:129–144. [DOI] [PubMed] [Google Scholar]
- 21.Césard M, Dussert F. Le travail ouvrier sous contrainte. In: INSEE, ed. Données Sociales. Paris, France: INSEE; 1993:202–211.
- 22.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–355. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg M, Chastang J-F, Leclerc A, Zins M, Bonenfant S, Bugel I. Socioeconomic, demographic, occupational and health factors associated with participation in a long-term epidemiological survey. A prospective study of the French Gazel cohort and its target population. Am J Epidemiol. 2001;154:373–384. [DOI] [PubMed] [Google Scholar]
- 24.Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Community Health. 2000;54:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leclerc A, Chastang J-F, Niedhammer I, Landre M-F, Roquelaure Y. Study Group on Repetitive Work. Incidence of shoulder pain in repetitive work. Occup Environ Med. 2004;61:39–44. [PMC free article] [PubMed] [Google Scholar]
- 26.Sorensen G, Stoddard A, Hammond SK, Hebert JR, Avrunin JS, Ockene JK. Double jeopardy: workplace hazards and behavioral risks for craftspersons and laborers. Am J Health Promotion. 1996;10:355–363. [DOI] [PubMed] [Google Scholar]
- 27.Brisson C, Larocque B, Moisan J, Vezina M, Dagenais G. Psychosocial factors at work, smoking, sedentary behavior, and body mass index: a prevalence study among 6995 white collar workers. J Occup Environ Med. 2000;42:40–46. [DOI] [PubMed] [Google Scholar]
- 28.Kivimäki M, Head J, Ferrie JE, Shipley MJ, Vahtera J, Marmot MG. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. Br Med J. 2003; 327:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kristensen TS. Sickness absence and work strain among Danish slaughterhouse workers: an analysis of absence from work regarded as coping behaviour. Soc Sci Med. 1991;32:15–27. [DOI] [PubMed] [Google Scholar]
- 30.Rael E, Stansfeld S, Shipley M, Head J, Feeney A, Marmot M. Sickness absence in the Whitehall II study, London: the role of social support and material problems. J Epidemiol Community Health. 1995;49:474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kivimäki M, Elovainio M, Vahtera J, Ferrie JE. Organisational justice and health of employees: prospective cohort study. Occup Environ Med. 2003;60:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kivimäki M, Vahtera J, Ferrie J, Hemingway H, Pentti J. Organisational downsizing and musculoskeletal problems in employees: a prospective study. Occup Environ Med. 2001;58:811–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knutsson A, Goine H. Occupation and unemployment rates as predictors of long-term sickness absence in two Swedish counties. Soc Sci Med. 1998;47:25–31. [DOI] [PubMed] [Google Scholar]
- 34.Ribet C, Zins M, Guéguen A, et al. Occupational mobility and cardiovascular risk factors in working men: selection, causality, or both? Results from the GAZEL study. J Epidemiol Community Health. 2003; 57:901–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Power C, Matthews S, Manor O. Inequalities in self-rated health in the 1958 birth cohort: lifetime social circumstances or social mobility? Br Med J. 1996; 313:449–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hallqvist J, Lynch JW, Bartley M, Lang T, Blane D. Can we disentangle life course processes of accumulation, critical period and social mobility? An analysis of disadvantaged socio-economic positions and myocardial infarction in the Stockholm Heart Epidemiology Program (SHEEP). Soc Sci Med. 2004; 8:1555–1562. [DOI] [PubMed] [Google Scholar]