Abstract
Objectives. We estimated the contribution of nonfatal work-related injuries on the injury burden among working-age adults (aged 18–64 years) in the United States.
Methods. We used the 1997–1999 National Health Interview Survey (NHIS) to estimate injury rates and proportions of work-related vs non–work-related injuries.
Results. An estimated 19.4 million medically treated injuries occurred annually to working-age adults (11.7 episodes per 100 persons; 95% confidence interval [CI]=11.3, 12.1); 29%, or 5.5 million (4.5 per 100 persons; 95% CI=4.2, 4.7), occurred at work and varied by gender, age, and race/ethnicity. Among employed persons, 38% of injuries occurred at work, and among employed men aged 55–64 years, 49% of injuries occurred at work.
Conclusions. Injuries at work comprise a substantial part of the injury burden, accounting for nearly half of all injuries in some age groups. The NHIS provides an important source of population-based data with which to determine the work relatedness of injuries. Study estimates of days away from work after injury were 1.8 times higher than the Bureau of Labor Statistics (BLS) workplace-based estimates and 1.4 times as high as BLS estimates for private industry. The prominence of occupational injuries among injuries to working-age adults reinforces the need to examine workplace conditions in efforts to reduce the societal impact of injuries.
In 1997, an estimated 34.4 million medically treated injuries and poisonings occurred in the United States—a rate of 12.9 episodes per 100 persons.1 Injuries to working-age adults, which represent an important part of this injury burden, are often overlooked despite having a larger economic impact than injuries to other age groups.2 Until recently, comparable national data that distinguished work-related from non–work-related injuries were not available on the incidence and types of injuries to working-age adults. Moreover, existing workplace-based reporting systems may substantially underestimate occupational injuries.3–23 When adjustment is made for underreporting, annual estimates of nonfatal work-related injuries in the United States range from 6 million to 13 million.3,5 No comprehensive national data exist on nonfatal work-related injuries or even work-related injury hospitalizations.12–14
The National Health Interview Survey (NHIS) is one of the most important tools for monitoring the health of the US population.24–27 It recently has been revised to improve the quality of data collected on injuries and includes work relatedness.1 This revision now provides an opportunity to examine all injuries to adults in the US population and to assess those occurring at work, independent of workplace reporting. We used data from the redesigned NHIS for 1997–1999 to examine the contribution of nonfatal injuries at work to the total injury burden of working-age adults (aged 18–64 years).
METHODS
The NHIS is a nationwide survey conducted by the National Center for Health Statistics with trained interviewers from the Census Bureau. The survey provides health information about a nationally representative sample of the noninstitutionalized US civilian population.1,28,29 For each sampled household, in-person interviews are conducted with a resident adult who provides information on all household members. Information collected includes demographic and personal characteristics, health status, and use of health resources. Most analyses in this article were derived from data reported by the resident adult on behalf of all members of the family. However, to obtain the most accurate information on employment, occupation, industry, and other items, 1 adult in each household is randomly selected as the “sample” adult from whom data are gathered directly (data available as a separate sample adult file).
Beginning in 1997, more detailed information on injuries was collected by the NHIS.1 Details concerning all medically treated injuries (including those injuries about which advice was received) during the past 3 months to any member of the household, including injuries related to any paid work, were obtained from the respondent through a computer-assisted personal interview. Data from 1997 to 1999, the first 3 years of the redesigned survey, were combined to develop national estimates of nonfatal work-related and non–work-related injuries. The unit of analysis for the study was the injury episode; an injured person may have multiple episodes.
Injuries were defined as work related or at work if the response “Working at a paid job” was selected in answer to the question, “What were you doing when the injury happened?” Employed persons were defined as those who reported employment in a job or business during the week before the interview (regardless of whether they worked that week). It is possible that employment status changed between the time of the injury, which could be up to 3 months prior to the interview, and the week before the interview. Such a status change could result in some misclassification of employment status, but we assumed such changes to be minimal. We excluded all poisonings from our analyses, because the NHIS asked separate questions for injuries and for poisonings and did not ascertain the work relatedness of poisonings during 1997–1999. Musculoskeletal disorders are also not included by definition.
Study Population
The working-age population was defined as persons aged 18 to 64 years. People younger than 18 years and people 65 years and older were excluded because of the small numbers of work-related injury episodes reported for these age groups (n = 19 and 25, respectively [unweighted]). A total of 113614 households were surveyed by the NHIS during the 3 year-period, with an adult representative providing information for 298388 household members; 99357 sample adults were interviewed directly. The overall survey response rate for all ages was 90.3% in 1997, 88.2% in 1998, and 86.1% in 1999.29,30
Data Analysis
The descriptive analysis was performed with SAS version 8.0 (SAS Institute Inc, Cary, NC). To derive national estimates, sample weights that accounted for the complex sample design of the survey were assigned by the National Center for Health Statistics for each respondent on the basis of the number and composition of households; these weights included adjustment for non-response.29 Weights also were provided for the sample adults. The denominator population used for calculating injury rates was obtained directly from the survey.
The distribution of injuries was examined for all injury episodes by various characteristics and by work relatedness. Standard errors and 95% confidence intervals were calculated with SUDAAN software31 to account for the complex, multistage sample design used in the survey. Estimates with relative standard errors greater than 30% were considered unreliable. To identify contrasts between sub-populations that were both meaningful and significant, differences in injury rates and proportions were tested with a 2-sided z test at the 0.05 level of significance. Because multiple, simultaneous tests were performed, the Bonferroni method was used to provide a more conservative threshold for identifying significant differences. The trend in rates by age group was tested by fitting a linear regression model weighted inversely to the variance of each rate. Tests of differences between estimates discussed in the text were conducted with these methods (results not shown).
RESULTS
Survey respondents reported a total of 4925 injury episodes (unweighted) among adults aged 18 to 64 years from 1997 to 1999. When weighted, these responses formed the basis of our national estimates. There were 1386 persons in the survey who were injured at work, resulting in 1422 work-related injury episodes (2.4% sustained 2 episodes during the 3-month period, and 2 people sustained 3 or more episodes).
Injury Estimates and Rates
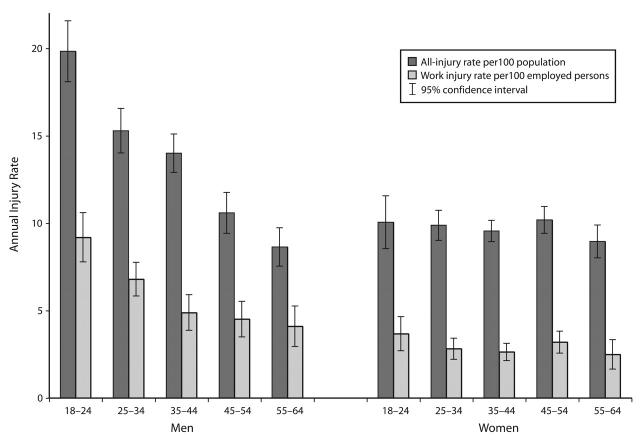
The civilian, noninstitutionalized adult US population aged 18 to 64 years (approximately 165 million) sustained an estimated 19.4 million injury episodes annually, a rate of 11.7 per 100 persons (Table 1 ▶). About 5.5 million at-work injury episodes occurred annually among the estimated 124 million people who were employed at the time of the interview, a rate of 4.5 per 100 employed persons. For men, the overall injury rate was 40% higher than the rate for women, but the work-related injury rate was double that of women. Overall injury rates decreased with age. The trend, however, was driven by the rate among men, because no trend by age was found among the rates for women (Figure 1 ▶). When stratified by gender, the rates for men were highest among those aged 18 to 24 years (Figure 1 ▶), both for all injuries (19.8 per 100) and for work-related injuries (9.2 per 100), and declined significantly by age. Non-Hispanic White adults had the highest injury rates, followed by non-Hispanic Black adults and Hispanic adults (Table 1 ▶). When the data were limited to work-related injuries, the order of the rates was the same, but the differences among racial/ethnic groups were smaller and nonsignificant. When rates were stratified by age and gender, differences in work-related injury rates by race/ethnicity persisted and were greatest among younger men (data not shown).
TABLE 1—
Number, Percentage, and Rate of All Injury Episodes and Work-Related Injury Episodes Among the Working-Age Population (Aged 18–64 years), by Age, Gender, and Race/Ethnicity: National Health Interview Survey, 1997–1999
| All Injuries Annually | Work-Related Injuries Annually | |||
| No. in 1000s (%) | Rate per 100 Populationa (95% CI) | No. in 1000s (%) | Rate per 100 Employed Populationb (95% CI) | |
| Age, y | ||||
| 18–24 | 3807 (19.6) | 14.9 (13.8, 16.1) | 1088 (19.6) | 6.6 (5.7, 7.5) |
| 25–34 | 4858 (25.1) | 12.5 (11.8, 13.3) | 1561 (28.2) | 5.0 (4.4, 5.5) |
| 35–44 | 5191 (26.8) | 11.7 (11.0, 12.5) | 1401 (25.3) | 3.8 (3.4, 4.2) |
| 45–54 | 3576 (18.4) | 10.4 (9.6, 11.1) | 1069 (19.3) | 3.9 (3.4, 4.4) |
| 55–64 | 1961 (10.1) | 8.8 (8.0, 9.6) | 426 (7.7) | 3.4 (2.7, 4.0) |
| Gender | ||||
| Male | 11 189 (57.7) | 13.8 (13.2, 14.4) | 3863 (69.7) | 5.8 (5.4, 6.2) |
| Female | 8204 (42.3) | 9.8 (9.3, 10.2) | 1683 (30.3) | 2.9 (2.6, 3.2) |
| Race/ethnicity | ||||
| White non-Hispanic | 15 320 (79.0) | 12.8 (12.3, 13.3) | 4392 (79.2) | 4.7 (4.4, 5.0) |
| Black non-Hispanic | 2030 (10.5) | 10.4 (9.5, 11.4) | 542 (9.8) | 4.0 (3.3, 4.7) |
| Hispanic | 1438 (7.4) | 7.9 (7.2, 8.7) | 486 (8.8) | 3.8 (3.3, 4.4) |
| Other | 605 (3.1) | 8.0 (6.5, 9.5) | 126 (2.3) | 2.3 (1.5, 3.2) |
| Total | 19 393 (100.0) | 11.7 (11.3, 12.1) | 5546 (100.0) | 4.5 (4.2, 4.7) |
Note. CI = confidence interval.
aAll people in the population aged 18 to 64 years regardless of employment (n = 165 million).
bPeople who were reported to be employed at a job or business in the week before the interview (n = 124 million).
FIGURE 1—
Annual rates of total injuries and work-related injuries by gender and age: National Health Interview Survey, 1997–1999.
Proportion of All Injuries That Were Work Related
Among all working-age persons, 28.6% of injuries occurred while people were working (Table 2 ▶). Annually, the employed population sustained 14.8 million injuries (data not shown), of which 37.5% occurred at work (Table 2 ▶). Among all working-age men, 34.5% of injury episodes occurred at work, compared with only 20.5% of such episodes among working-age women, with higher proportions among employed people, 42.3% and 29.7%, respectively. When data were stratified by the age of the injured person, the percentage of episodes that were work related ranged between 22% and 32%; when data were limited to employed persons, the figure was between 33% and 41%. When data were stratified by age and gender, the proportion of injuries that were work related was consistently higher for employed men than for employed women.
TABLE 2—
Percentage of Injuries That Are Work Related Among Working-Age Adults Aged 18–64 Years), by Age, Race/Ethnicity, and Gender: National Health Interview Survey, 1997–1999
| Work-Related Injuries, % | ||
| Whole Working-Age Populationa (95% CI) | Employed Working-Age Populationb (95% CI) | |
| Age, y | ||
| 18–24 | 28.6 (25.5, 31.7) | 41.2 (36.8, 45.6) |
| 25–34 | 32.1 (29.2, 35.0) | 38.9 (35.4, 42.4) |
| 35–44 | 27.0 (24.5, 29.5) | 33.4 (30.4, 36.4) |
| 45–54 | 29.9 (26.6, 33.2) | 37.9(33.8, 42.0) |
| 55–64 | 21.7 (17.8, 25.6) | 38.0 (31.7, 44.3) |
| Gender and age | ||
| Male | 34.5 (32.5, 36.5) | 42.3 (40.0, 44.6) |
| 18–24 | 31.7 (27.6, 35.8) | 44.6 (39.0, 50.1) |
| 25–34 | 39.9 (36.0, 43.8) | 43.8 (39.5, 48.1) |
| 35–44 | 31.4 (28.1, 34.7) | 37.1 (33.0, 41.1) |
| 45–54 | 37.0 (32.3, 41.7) | 43.4 (37.8, 49.0) |
| 55–64 | 30.9 (24.4, 37.4) | 49.2 (39.6, 58.7) |
| Female | 20.5 (18.5, 22.5) | 29.7 (27.1, 32.3) |
| 18–24 | 22.4 (17.3, 27.5) | 34.0 (26.5, 41.5) |
| 25–34 | 20.6 (16.9, 24.3) | 29.4 (24.1, 34.7) |
| 35–44 | 20.6 (17.3, 23.9) | 27.5 (23.2, 31.8) |
| 45–54 | 22.9 (18.6, 27.2) | 31.5 (25.6, 37.3) |
| 55–64 | 13.7 (9.4, 18.0) | 26.2 (18.3, 34.1) |
| Race/ethnicity | ||
| White non-Hispanic | 28.7 (27.1, 30.3) | 36.9 (35.0, 38.8) |
| Black non-Hispanic | 26.7(22.2, 31.2) | 39.8 (33.2, 46.4) |
| Hispanic | 33.8 (30.1, 37.5) | 45.1 (40.2, 50.0) |
| Other non-Hispanic | 20.8 (14.5, 27.1) | 27.9 (19.8, 36.0) |
| Total | 28.6 (27.2, 30.0) | 37.5 (35.7, 39.3) |
aEveryone in the population aged 18–64 years regardless of employment status (n = 165 million).
bPeople who were reported to be employed at a job or business in the week before the interview (n = 124 million).
Nature of Injury and Body Region
For both work-related and non–work-related nonfatal injuries, sprains and strains were most common, followed by open wounds and fractures (Table 3 ▶). Crushing injuries, the presence of foreign bodies in an organ or body cavity, amputations, and burns accounted for the highest percentages of work-related injuries. Only 17% of fractures and 18% of superficial injuries were work related. Overall, 11.3% of injury episodes (9.9% of work-related injuries and 11.8% of non–work-related injuries) were coded as nature unspecified (denoting that the respondent provided insufficient description of the injury to enable assignment of an International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]32 medical diagnosis code).
TABLE 3—
Nature of Injury and Affected Body Region in Work-Related and Non–Work-Related Injuries Among the Working-Age Population (Aged 18–64 Years): National Health Interview Survey, 1997–1999
| Work-Related Injuries Annually, No. in 1000s (%) | Non–Work-Related Injuries Annually, No. in 1000s (%) | % of All Injuries That Were Work Related (95% CI) | |
| Nature of injury | |||
| Sprains and strains | 1892 (34.3) | 4536 (32.8) | 29.4 (26.9, 31.9) |
| Open wounds | 1170 (21.2) | 2354 (17.0) | 33.2 (29.9, 36.5) |
| Fractures | 498 (9.0) | 2393 (17.3) | 17.2 (14.3, 20.1) |
| Contusions | 360 (6.5) | 1197 (8.6) | 23.1 (18.6, 27.6) |
| Dislocations | 270 (4.9) | 485 (3.5) | 35.7 (28.4, 43.0) |
| Injury to internal organs | 120 (2.2) | 354 (2.6) | 25.3 (16.5, 34.1) |
| Burns | 183 (3.3) | 251 (1.8) | 42.1 (31.7, 52.5) |
| Superficial injuries | 62 (1.1) | 277 (2.0) | 18.3 (9.9, 26.7) |
| Foreign bodies | 164 (3.0) | 97 (0.7) | 62.9 (49.6, 76.2) |
| Crushing injuries | 138 (2.5) | 77 (0.6) | 64.2 (50.1, 78.3) |
| Nerves | 50 (0.9) | 91 (0.7) | 35.6 (20.5, 50.7) |
| Amputation of limbs | 57 (1.0) | 43 (0.3) | 56.9 (37.5, 76.3) |
| Other specifieda | . . .b (. . .b) | 61 (0.4) | 35.9 (15.9, 55.9) |
| Unspecified | 548 (9.9) | 1632 (11.8) | 25.1 (21.2, 29.0) |
| Body region | |||
| Lower extremity | 1401 (25.3) | 4716 (34.1) | 22.9 (20.7, 25.1) |
| Upper extremity | 2036 (36.7) | 3641 (26.3) | 35.9 (33.4, 38.4) |
| Spine and back | 949 (17.1) | 2140 (15.5) | 30.7 (27.4, 34.0) |
| Face and neck | 307 (5.5) | 955 (6.9) | 24.3 (19.4, 29.2) |
| Skull and brain | 154 (2.8) | 455 (3.3) | 25.3 (17.9, 32.7) |
| Thorax | 71 (1.3) | 499 (3.6) | 12.5 (7.0, 18.0) |
| Abdomen and pelvis | . . .b (. . .b) | 54 (0.4) | 38.3 (16.3, 60.3) |
| Other body regions | 430 (7.8) | 1291 (9.3) | 25.0 (20.5, 29.5) |
| Total | 5546 (100.0) | 13 847 (100.0) | 28.6 (27.2, 30.0) |
a“Other specified” includes injuries to blood vessels, toxic effects, external causes, late effects of injuries, early complications of trauma, and medical/surgical complications.
bEstimates are unreliable, with relative standard error of the estimate greater than 30%.
The upper- and lower-body extremities accounted for more than 60% of work-related and non–work-related injuries (Table 3 ▶). The upper extremities were involved in the largest percentage of work-related injuries, whereas for non–work-related injuries, the regions most affected were the lower extremities. Over a third of the upper-extremity injuries (36%) were work related, compared with less than a quarter of the lower-extremity injuries (23%). Fractures occurring at work were also more likely to affect an upper extremity, and non–work-related fractures were more likely to affect a lower extremity (data not shown).
Time Lost From Work
Among working-age adults, an estimated annual 8.9 million injury episodes and an estimated 3.6 million work-related injury episodes resulted in at least part of a day off work. Of all injury episodes among the working-age population, 46.1% resulted in loss of at least part of a day of work, and 38.1% involved loss of 1 or more days (1–5 days lost, 21.6%; 6 or more days lost, 16.5%). Of all work-related injury episodes, 65.6% resulted in at least part of a day of lost work, and 51.0% involved loss of 1 or more days (1–5 days lost, 27.5%; 6 or more days lost, 23.6%) (data not shown).
To compare NHIS data with data from Bureau of Labor Statistics (BLS) surveys,6,7,15–17 which cover only private industry, we conducted separate analyses of the NHIS sample adult file; industry data were gathered only from the sampled adults. On the basis of the data from the sample adult file, 50.4% of the work-related injury episodes resulted in 1 or more days off work. Of the estimated 3.01 million annual occupational injuries resulting in at least 1 day off work reported by sample adults, 2.36 million (78.4%) were reported by employees in private industry; the remainder were reported by government employees, farm workers, or the self-employed (not included in BLS surveys).
DISCUSSION
Nonfatal injuries to working-age adults are common, annually resulting in 12 episodes of medically treated injuries per 100 adults aged 18 to 64 years. The redesigned NHIS enabled us to determine that work-related injuries are also common (4.5 episodes per 100 employed working-age persons) and are a significant part of the total injury burden; such injuries accounted for almost 30% of injuries to working-age adults, a figure that rose to almost 50% for 1 employed age group. Our ability to assess each injury recorded in the NHIS for work relatedness overcomes many of the shortcomings inherent in estimates of work-related injuries from other sources. Comparable data sources containing information on both work-related and non–work-related injuries have not been available; this lack of information has prevented an examination of the contribution of work-related injuries to the total injury burden.
Work-related injuries are often regarded as very different from non–work-related injuries in terms of etiology, surveillance, and prevention.12 For instance, separate workplace-based data sources, such as BLS surveys or worker’s compensation data, are used to study injuries at work.6,7,15–17 These sources are vulnerable to a variety of underreporting effects.5–7,9,10,18,19 For example, the BLS Survey of Occupational Injuries and Illnesses is the primary source of national nonfatal work-related injury data, but it covers only private industry. It excludes self-employed persons, government workers, and most workers on farms and in the informal workforce (e.g., domestic help, undocumented immigrants).15,16 In our study, 21.6% of all injuries occurred among workers not covered by the BLS survey. Direct comparisons of our study with data from the BLS are possible only for cases involving lost work days, because these 2 data sources use different definitions of injury. Our NHIS-based estimate of occupational injury episodes occurring in US private industry that result in 1 or more days off work (2.36 million) was 1.4 times higher than the BLS’s 1998 estimate of 1.649 million injuries that result in 1 or more days off work (i.e., excluding cases involving only restricted-duty days).16 This estimate confirms findings of previous studies that documented underreporting among the industry groups covered by the BLS.3–23 In addition, the total NHIS work-related injury count for the United States (3.01 million) was 1.8 times higher than the BLS. This ratio is a function of both incomplete coverage of the US work-force by the BLS and underreporting of work-related injuries in the BLS.
Other population-based sources of occupational-injury data rely heavily on the recording of work relatedness in the medical record and may examine only 1 level of medical care. Surveys of occupational injuries with emergency department records, for example,5,33–35 exclude medical care provided in private physician offices and occupational health clinics. One 1988 study found that only 34% of all occupational injuries were treated in emergency departments.13 The reporting of work relatedness in clinical record systems is also known to be inconsistent.5,36 Many data sources, such as hospital discharge databases, do not systematically record work relatedness. Health care providers can play an important role in improving these data sources for occupational injury surveillance by documenting work relatedness in medical charts.
It is important to determine the work relatedness of all injuries to adults, because the type of injury usually provides little indication of whether it occurred at work. The characteristics of work-related and non–work-related injuries are similar, with little variation in distribution (Table 3 ▶). Although crushing injuries, the presence of foreign bodies, and amputations are more likely to occur at work, many such episodes occur in non-work settings. Documenting and reporting work relatedness is just as important for injuries as it is for occupational diseases.37 Everyone involved in treating and preventing injuries should also evaluate work hazards, because many of the injuries occur at work, especially among working-age men.
Several earlier studies used NHIS data to examine injuries but did not compare all injuries with those occurring on the job. Warner and colleagues1 reported that during the first year of the revised NHIS, 53% of injuries to all age groups occurred among adults aged 22 to 64 years, but they provided limited data on occupational injuries. Two recent studies examined sports and recreation injuries but did not consider whether any of these may have been work related.30,38 Prior to revision of the NHIS, most analyses considered only broad classes of injury based on 4 combinations of place and activity (i.e., home, motor vehicle, work, and other place), but these classes were not mutually exclusive.
The revised NHIS now collects data on both cause and place of injury.1,39 One study that used NHIS data from 1983–1987 reported higher rates of occupational injuries than in our study, as did the BLS for that period (BLS rates declined in subsequent years).16 Comparisons with NHIS data from before 1997 are not valid because of the different survey instruments used.40,41 Other studies have used special annual supplements to the NHIS to examine the effects of disability and impairment in the workplace.27,42,43 The 1988 Occupational Health Supplement to the NHIS included questions on work-related injury, but lack of detail on the injuries, small sample size, and problems associated with using a 1-year recall period restricted the supplement’s utility in the study of workplace injuries.44,45
Study Limitations
Any study relying on data from respondents may suffer from recall bias, which can result in underestimation or overestimation of injury rates.44,46–49 A 3-month recall period was used to increase the number of episodes of injury reported in our study.1 Because recall improves as injury severity increases, we enhanced recall accuracy by defining injuries as those that were severe enough to require medical attention.47 It is possible that, in our study, home injuries were better recalled than work-related injuries because the interview took place in the home. However, we found no studies documenting such an “interview context” effect.
However, the NHIS definition of injury requires that medical attention be sought, and people injured at work may be more likely to seek medical attention than people injured at home for such reasons as improved access, compensation, and legal liability. This definition could result in the reporting of more work-related injuries than home injuries, but we were not able to address this issue in our study. Similarly, differences among recent immigrants in access to care or immigrants’ reluctance to identify an injury as work related may also explain some of the observed variation by race/ethnicity. Other studies have in fact found higher rates of occupational injuries among Hispanics and Blacks, but studies across a broad range of industries have been restricted to evaluation of fatalities.50,51 A detailed examination of racial/ethnic differences would require careful adjustment for factors such as differences in occupational exposures and employment patterns.
Poisonings were excluded from our analyses because the activity question (asking what the person was doing when the injury occurred), which we used to define work relatedness, was not asked of those who had been poisoned until 2000. Poisonings account for less than 0.6% of all occupational injuries (from national emergency department visit data52), and their exclusion is thus unlikely to have significantly altered our study findings. Owing to other questionnaire wording and survey design modifications, we did not combine the 1997–1999 estimates with more recent estimates because of concerns about comparability.41 The activity question used to define work relatedness allowed up to 2 responses. For instance, a respondent could choose “working for a paid job” and “driving or riding in a motor vehicle” as the activity being engaged in when the injury occurred. However, very few injury episodes had more than 1 activity listed, which may have resulted in underrepresentation of work relatedness, especially for motor vehicle injuries. Information on employment, including occupation and industry, was asked only of the sample adult, limiting our ability to conduct detailed comparisons by occupation and industry. Asking direct questions about work relatedness (e.g., whether the injury occurred during the course of paid work, or in what industry and at what occupation the injured person was working) would help to reduce the limitations of many health data systems.
Conclusions
Injuries to adults are an important public health problem that affects not only the person sustaining the injury but also other household members dependent on the injured adult for support. Injuries on the job are a significant part of this injury burden, comprising almost 30% of all medically treated injuries to adults aged 18 to 64 years. For employed men, 42% of all injuries were work related (49% among men aged 54–64 years). The NHIS is an important new source of data with which to determine the work relatedness of injuries and confirms previous studies in documenting serious underreporting by traditional workplace-based reporting systems.3–11 Population-based data, such as those obtained from the NHIS, provide a model for improving occupational injury surveillance and support proposals for community-oriented approaches that look at work-related and non–work-related injuries together.20–22 The fact that such a large proportion of injuries to working-age adults are occupational in nature also reinforces the need to examine workplace conditions in efforts to reduce the impact of injuries on society.
Acknowledgments
This study was supported in part by the Liberty Mutual Research Institute for Safety’s Visiting Scholars program.
We acknowledge the helpful comments on earlier drafts of the article provided by Dr David A. Lombardi and Barbara S. Webster, as well as Patti Boelsen for editorial assistance.
Human Participant Protection The Liberty Mutual Research Institute for Safety institutional review committee for the protection of human subjects approved the study.
Peer Reviewed
Contributors G. S. Smith conceived the study, supervised all aspects of its implementation, and led the writing of the article. H. M. Wellman conducted the analyses, and M. Warner assisted in calculating sample variances. All authors helped to conceptualize ideas, interpret findings, and review and revise drafts of the article.
References
- 1.Warner M, Barnes P, Fingerhut L. Injury and poisoning episodes and conditions; National Health Interview Survey, 1997. Vital Health Stat 10. 2000; No. 202. [PubMed]
- 2.Boden LI, Galizzi M. Economic consequences of workplace injuries and illnesses: lost earnings and benefit adequacy. Am J Ind Med.1999;36:487–503. [DOI] [PubMed] [Google Scholar]
- 3.Leigh JP, Markowitz SB, Fahs M, et al. Occupational injury and illness in the United States: estimates of costs, morbidity, and mortality. Arch Intern Med.1997;157:1557–1568. [PubMed] [Google Scholar]
- 4.Cormack RM, Chang YF, Smith GS. Estimating deaths from industrial injury by capture-recapture: a cautionary tale. Int J Epidemiol.2000;29:1053–1059. [DOI] [PubMed] [Google Scholar]
- 5.McCaig LF, Burt CW, Stussman BJ. A comparison of work-related injury visits and other injury visits to emergency departments in the United States, 1995–1996. J Occup Environ Med.1998;40:870–875. [DOI] [PubMed] [Google Scholar]
- 6.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health.2002;92: 1421–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy PL, Sorock GS, Courtney TK, Webster BS, Leamon TB. Injury and illness in the American work-place: a comparison of data sources. Am J Ind Med.1996:30:130–141. [DOI] [PubMed] [Google Scholar]
- 8.Webb GR, Redman S, Wilkinson C, Sanson-Fisher RW. Filtering effects in reporting work injuries. Accid Anal Prev.1989;21:115–123. [DOI] [PubMed] [Google Scholar]
- 9.Glazner JE, Borgerding J, Lowery JT, et al. Construction injury rates may exceed national estimates: evidence from the construction of Denver International Airport. Am J Ind Med.1998;34:105–112. [DOI] [PubMed] [Google Scholar]
- 10.Leigh JP, Marcin JP, Miller TR. An estimate of the US Government’s undercount of non-fatal occupational injuries. J Occup Environ Med.2004;46:10–18. [DOI] [PubMed] [Google Scholar]
- 11.Pollack ES, Keimig DG. Counting Injuries and Illnesses in the Workplace: Proposals for a Better System. Washington, DC: National Academy Press; 1987.
- 12.Smith GS. Public health approaches to occupational injury prevention: do they work? Inj Prev.2001; 7(suppl 1):i3–i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Control Centers for Disease and Prevention. Surveillance for nonfatal occupational injuries treated in hospital emergency departments—United States, 1996. MMWR Morb Mortal Wkly Rep.1998:47;302–306. [PubMed] [Google Scholar]
- 14.Welch LS, Hunting K. Injury surveillance in construction: what is an “injury,” anyway? Am J Ind Med.2003:44:191–196. [DOI] [PubMed] [Google Scholar]
- 15.BLS Handbook of Methods. Chapter 9, Occupational Safety and Health Statistics. US Dept of Labor, Bureau of Labor Statistics, Washington, DC. Bulletin 2490, April 1997. Available at: www.bls.gov/opub/hom. Accessed April 20, 2005.
- 16.Occupational Injuries and Illnesses: Counts, Rates, and Characteristics, 1998. Washington, DC: US Dept of Labor, Bureau of Labor Statistics; July 2001. Bulletin 2538.
- 17.Courtney TK, Webster BS. Disabling occupational morbidity in the United States. An alternative way of seeing the Bureau of Labor Statistics’ data. J Occup Environ Med.1999;41:60–69. [DOI] [PubMed] [Google Scholar]
- 18.Shannon HS, Lowe GS. How many injured workers do not file claims for workers’ compensation benefits? Am J Ind Med.2002;42:467–473. [DOI] [PubMed] [Google Scholar]
- 19.Oleinick A, Guire KE, Hawthorne VM, et al. Current methods of estimating severity for occupational injuries and illnesses: data from the 1986 Michigan Comprehensive Compensable Injury and Illness Database. Am J Ind Med.1993;23:231–252. [DOI] [PubMed] [Google Scholar]
- 20.Smith GS, Veazie MA. Principles of prevention: the public health approach to preventing injuries in the workplace. In: ILO Encyclopedia of Occupational Health and Safety. Geneva, Switzerland: International Labor Office; 1998:56.26–56.30. Available at http://www.ilo.org/encyclopedia. Accessed April 20, 2005.
- 21.Tracking Occupational Injuries, Illnesses, and Hazards: The NIOSH Surveillance Strategic Plan. Cincinnati, Ohio: US Dept of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; January 2001. NIOSH publication 2001-118. Available at: http://www.cdc.gov/niosh/2001-118.html. Accessed June 13, 2003.
- 22.National Institute for Occupational Safety and Health. Traumatic Occupational Injury Research Needs and Priorities: A Report by the NORA Traumatic Injury Team. Cincinnati, Ohio: US Dept of Health and Human Services, Centers for Disease Control and Prevention; 1998. DHHS publication (NIOSH) 98–134.
- 23.Smith GS. Injury prevention: blurring the distinctions between home and work. Inj Prev.2003;9:3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA.2003;290:1884–1890. [DOI] [PubMed] [Google Scholar]
- 25.Weller WE, Minkovitz CS, Anderson GF. Utilization of medical and health-related services among school-age children and adolescents with special health care needs (1994 National Health Interview Survey on Disability [NHIS-D] Baseline Data). Pediatrics.2003; 112(3 Pt 1):593–603. [DOI] [PubMed] [Google Scholar]
- 26.Weil E, Wachterman M, McCarthy EP, et al. Obesity among adults with disabling conditions. JAMA.2002;288:1265–1268. [DOI] [PubMed] [Google Scholar]
- 27.Zwerling C, Whitten PS, Davis CS, Sprince NL. Occupational injuries among workers with disabilities: the National Health Interview Survey, 1985–1994 [published erratum appears in JAMA.1998;279: 1350]. JAMA. 1997;278:2163–2166. [PubMed] [Google Scholar]
- 28.Botman SL, Moore TF, Moriarity CL, et al. Design and estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat 2.2000;130: 14–19. [Google Scholar]
- 29.National Center for Health Statistics. National Health Interview Survey (NHIS), 1997, 1998, 1999: NHIS survey description and dataset documentation. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed September 9, 2003.
- 30.Ni H, Barnes P, Hardy AM. Recreational injury and its relation to socioeconomic status among school aged children in the US. Inj Prev.2002;8:60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah H, Barnwell B, Bieler G. SUDAAN User’s Manual, Release 7.0. Research Triangle Park, NC: Research Triangle Institute, 1996.
- 32.Official ICD-9-CM Guidelines for Coding and Reporting. Hyattsville, Md: National Center for Health Statistics; 1997.
- 33.Jackson LL. Non-fatal occupational injuries and illnesses treated in hospital emergency departments in the United States. Inj Prev.2001;7(suppl 1):i21–i26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Worker Health Chartbook, 2000 Nonfatal Injury. Cincinnati, Ohio: National Institute for Occupational Safety and Health; May 2002. DHHS (NIOSH) publication 2002-119. Available at: www.cdc.gov/NIOSH. Accessed January 3, 2003.
- 35.Control Centers for Disease and Prevention. National estimates of nonfatal injuries treated in hospital emergency departments—United States, 2000. MMWR Morb Mortal Wkly Rep.2001;50:340–346. [PubMed] [Google Scholar]
- 36.Fingar AR, Hopkins RS, Nelson, M. Work-related injuries in Athens County 1982–1986: a comparison of emergency department and workers’ compensation data. J Occup Med.1992;34:779–787. [DOI] [PubMed] [Google Scholar]
- 37.Freund E, Seligman PJ, Chorba TL, Safford SK, Drachman JG, Hull HF. Mandatory reporting of occupational diseases by clinicians. JAMA.1989;262: 3041–3044. [PubMed] [Google Scholar]
- 38.Conn JM, Annest JL, Gilchrist J. Sports and recreation related injury episodes in the US population, 1997–99. Inj Prev.2003;9:117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith GS, Sorock GS, Wellman HM, Courtney TK, Pransky GS. Blurring the distinctions between home and work: similarities and differences in injury circumstances. Inj Prev. In press. [DOI] [PMC free article] [PubMed]
- 40.Wagener D, Winn D. Injuries in working populations: black-white differences. Am J Public Health.1991; 81:1408–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Warner M, Heinen MA, Barnes P, Fingerhut L. Collection of injury and poisoning data in the National Health Interview Survey, 1997–2000. Paper presented at: 130th Annual Meeting of the American Public Health Association; November 12, 2002; Philadelphia, Pa. Available at: http://apha.confex.com/apha/130am/techprogram/paper_46858.htm. Accessed February 11, 2004.
- 42.Zwerling C, Whitten PS, Sprince NL, et al. Work-force participation by persons with disabilities: the National Health Interview Survey Disability Supplement, 1994 to 1995. J Occup Environ Med.2002;44: 358–364. [DOI] [PubMed] [Google Scholar]
- 43.Zwerling C, Whitten PS, Sprince NL, et al. Work-place accommodations for people with disabilities: National Health Interview Survey Disability Supplement, 1994–1995. J Occup Environ Med.2003;45:517–525. [DOI] [PubMed] [Google Scholar]
- 44.Landen DD, Hendricks S. Effect of recall on reporting of at-work injuries. Public Health Rep.1995; 110:350–354. [PMC free article] [PubMed] [Google Scholar]
- 45.Landen DD, Hendricks SA. Estimates from the National Health Interview Survey on occupational injury among older workers in the United States. Scand J Work Environ Health.1992;18(suppl 2):18–20. [PubMed] [Google Scholar]
- 46.Zwerling C, Sprince NL, Wallace RB, Davis CS, Whitten PS, Heeringa SG. Effect of recall period on the reporting of occupational injuries among older workers in the Health and Retirement Study. Am J Ind Med.1995;28:583–590. [DOI] [PubMed] [Google Scholar]
- 47.Harel Y, Overpeck MD, Jones DH, et al. The effects of recall on estimating annual nonfatal injury rates for children and adolescents. Am J Public Health.1994;84:599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jenkins P, Earle-Richardson G, Slingerland DT, May J. Time dependent memory decay. Am J Ind Med.2002;41:98–101. [DOI] [PubMed] [Google Scholar]
- 49.Mock C, Acheampong F, Adjei S, Koepsell T. The effect of recall on estimation of incidence rates for injury in Ghana. Int J Epidemiol.1999;28:750–755. [DOI] [PubMed] [Google Scholar]
- 50.Richardson D, Loomis D, Bena J, Bailer AJ. Unintentional fatal occupational injury rates in the US by race and Hispanic ethnicity: a comparison of the South to the rest of the country. Am J Public Health.2004; 94:1756–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Loomis D, Richardson D. Race and the risk of fatal injury at work. Am J Public Health.1998;88: 40–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Institute for Occupational Safety and Health. Work-Related Injury Statistics Query System (Work-RISQS). Available at: http://www2a.cdc.gov/risqs/default.asp. Accessed June 13, 2003.