Abstract
Objectives. Housing typically is not provided to homeless persons during drug abuse treatment. We examined how treatment outcomes were affected under 3 different housing provision conditions.
Methods. We studied 196 cocaine-dependent participants who received day treatment and no housing (NH), housing contingent on drug abstinence (ACH), or housing not contingent on abstinence (NACH). Drug use was monitored with urine testing.
Results. The ACH group had a higher prevalence of drug abstinence than the NACH group (after control for treatment attendance), which in turn had a higher prevalence than the NH group. All 3 groups showed significant improvement in maintaining employment and housing.
Conclusions. The results of this and previous trials indicate that providing abstinence-contingent housing to homeless substance abusers in treatment is an efficacious, effective, and practical intervention. Programs to provide such housing should be considered in policy initiatives.
Homelessness affects 3.5% to 6.0% of Americans at some point in their lives, and as many as 11.4% of urban women of childbearing age are homeless.1–4 The point prevalence of homelessness has been estimated at 1% of the general US population and 6.3% of people in poverty.5,6 Lack of child care and a history of physical and/or sexual abuse greatly increase risk for homelessness.7 Homelessness, in turn, increases risk for diseases including HIV, other sexually transmitted diseases, tuberculosis, asthma, and bronchitis.8 These diseases contribute to morbidity and premature death.9–11
Providing effective drug abuse intervention for homeless substance abusers is a daunting challenge because of this population’s high morbidity, poverty, and social instability.12–19 In particular, homelessness necessitates a continuous search for food and shelter, which seriously interferes with treatment participation. For example, O’Brien et al.20 found that day treatment reduced drug abuse among non-homeless participants but that no homeless participants were retained in treatment.
Previous trials have shown that provision of housing for homeless substance abusers while they are undergoing behavioral day treatment improved addiction outcomes and resulted in less homelessness.21,22 In those studies, housing was available only when participants were drug-free; that is, housing was “abstinence-contingent.”
Such a contingency differs greatly from the typical “housing first” approach to fighting homelessness, in which housing is provided with no abstinence requirements, on the premise that housing provision alone will lead to improvement. In theory, non–abstinence-contingent housing for homeless substance abusers in treatment could be less expensive and logistically simpler, because treatment staff would not be required to monitor drug use and implement ejection from housing because of a failed urine test. Some authorities in the field believe non–abstinence-contingent housing to be an easier, cheaper, and more effective way to provide treatment for homeless drug abusers, but until now no studies have examined whether this approach is effective and cost-efficient.
In the trial, we examined how providing housing with and without an abstinence contingency affected drug use, homelessness, and employment among cocaine-dependent homeless persons. We considered 2 hypotheses: (1) that the housed groups would have better treatment retention and outcomes than those without housing, and (2) that those who received housing contingent on abstinence would have better outcomes than those who receive housing not contingent on abstinence.
METHODS
Participants
Participants were homeless persons from the Birmingham, Alabama, area with coexisting cocaine dependence and nonpsychotic mental disorders who were clients at Birmingham Health Care between September 1994 and November 2001. All met McKinney Act23 criteria for homelessness (they lacked a fixed nighttime residence, including shelters or other temporary accommodations, or were at imminent risk of becoming homeless), met criteria for cocaine dependence as outlined in the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition,24 had used cocaine within the past 2 weeks, and scored above 70 (2 standard deviations [SDs] above the mean) on 1 or more Symptom Checklist–90—Revised scales at intake.25,26 Potential participants were excluded if cognitive impairment precluded informed consent or if they required immediate inpatient medical treatment.
The final study set consisted of 196 participants randomly divided into 3 groups: those receiving abstinence-contingent housing (ACH; n = 63), those receiving non–abstinence-contingent housing (NACH; n = 67), and those receiving no housing (NH; n = 66). All groups received the same treatment during 12 months. Participant demographics are summarized in Table 1 ▶.
TABLE 1—
Demographic Characteristics and Treatment Group Comparisons
| Treatment Group | ||||
| NH (n = 66) | NACH (n = 66) | ACH (n = 63) | Pa | |
| Gender, n (%) | .98 | |||
| Male | 50 (76) | 50 (76) | 47 (75) | . . . |
| Female | 16 (24) | 16 (24) | 16 (25) | . . . |
| Age, yb (SD) | 38.2 (7.4) | 40.9 (7.2) | 38.4 (6.7) | .055 |
| Race/ethnicity, n (%) | .25 | |||
| African American | 59 (89) | 63 (95) | 55 (87) | . . . |
| European American | 7 (11) | 3 (5) | 8 (13) | . . . |
| Veteran, n (%)c | 11 (17) | 12 (19) | 11 (19) | .97 |
| Education, y (SD)d | 11.7 (1.6) | 12.2 (1.8) | 12.4 (1.8) | .22 |
| Longest full-time job, mo (SD)e | 51.6 (46.3) | 53.5 (40.9) | 65.9 (69.6) | .76 |
Note. NH = no housing; NACH = non-abstinence-contingent housing; ACH = abstinence-contingent housing.
aP values based on χ2 test (df=2) for categorical measures and on Kruskal–Wallis test for continuous measures. P tests were 2-tailed.
bOne NACH participant had missing data for age.
c Ten participants (3 NH, 3 NACH, 4 ACH) had missing data for veteran status.
dFour participants (2 NH, 2 NACH) had missing data for years of education.
eEighteen participants (5 NH, 9 NACH, 4 ACH) had missing data for longest employment period.
Intervention
The intervention was divided into phase 1 (months 1 through 2; day treatment), phase 2 (months 3 through 6; work therapy and after-care group meetings), and phase 3 (months 7 through 12; aftercare). Our manual-based cognitive–behavioral (CB) day treatment22 was provided to all participants. All participants were treated during the same types of group meetings, in the same offices, and by the same counselors. Day treatment was Mon-day through Friday, from 7:45 am to 2:00 pm, and included lunch, transportation to and from housing, individual counseling, and psychoeducational and therapy groups.
During the study period, urine testing was conducted for cocaine, marijuana, and alcohol use. Specimens were obtained from randomly selected participants twice weekly during phases 1 and 2 and once weekly during phase 3. During phase 1, ACH participants received rent-free housing after 2 consecutive drug-negative urine tests. NACH participants received rent-free housing in similar buildings in a different neighborhood after 2 consecutive urine tests, regardless of test results. In 1997 (midstudy) the ACH and NACH groups switched housing units with one another to balance any housing or neighborhood influences. NH participants received no program-provided housing.
For ACH participants, a drug-positive urine test resulted in immediate removal from housing to a shelter. Abstinence was considered reestablished with 2 consecutive drug-negative tests, after which ACH participants were immediately moved back to program housing. NACH participants remained in housing as long as they gave scheduled urine specimens, regardless of results. Exceptions occurred because of severe misbehavior at housing sites (e.g., damaging apartments, on-premise drug use, having overnight guests). Such behavior, which was observed in only 22 participants, was grounds for immediate housing restriction for both ACH and NACH participants for 1 week, during which the participant was placed in a shelter.
During phase 2, ACH and NACH participants were charged a monthly rent of $161.00; participants earned rent money through work therapy or other employment. Neither ACH nor NACH participants were removed from housing for not paying rent. All participants were offered work therapy at a minimum wage of $5.25 per hour. Continuation of work therapy was not contingent on abstinence, but the housing contingency remained in place for ACH participants.
During phase 3, ACH and NACH participants could remain in program housing if housing slots were available, but no abstinence contingency was imposed for any of the participants. All groups were offered aftercare group meetings once weekly for 6 months, with individual counseling provided as needed.
Outcome Measures
Participants were assessed by interviewers not aware of the participants’ treatment group at baseline and 2, 6, and 12 months after baseline. Participants were given backpacks containing personal hygiene items after baseline assessment and were paid $25 for each completed follow-up assessment. A nonparticipant “tracker” was tasked with locating participants and transporting them to the follow-up assessments. The tracker was paid $25 for each completed follow-up assessment.
Drug testing was conducted with the OnTrak TesTstik (Roche Diagnostic Systems, Somerville, NJ). To encourage compliance, clients were paid $3 per specimen during months 5 through 10 and $5 per specimen during months 11 and 12 for 4 randomly selected specimens out of the 8 scheduled urinalysis tests. If a urinalysis result was inconclusive, the original specimen was tested 1 or 2 more times, and the 2 most consistent results determined the data point. Urinalysis test results were used to implement the housing contingencies and to construct 2 drug use–dependent variables: (1) the proportion of participants, by group, whose urine tests all were drug-negative each week, and (2) the longest string of consecutive weeks of abstinence attained by each participant. Data from specimens obtained at follow-up are not reported here.
Homelessness and employment were measured with the Retrospective Interview for Housing, Employment, and Treatment History completed by each participant.27 Days employed was the number of days the participant was fully employed (i.e., worked at least 7 hours per day) the last 60 days. Homelessness was measured by number of days housed during the past 60 days.
Treatment Attendance and Study Retention
Treatment attendance was recorded in a counselor-verified daily service log in 15-minute increments. A complete treatment day was defined as participation in 10 or more increments per day during phase 1 and in 4 or more increments per day during phase 2. Study retention was measured by number of follow-up assessments completed.
Analysis
We employed an intention-to-treat analysis for the drug abstinence, housing, and employment outcomes, meaning that, in our analysis, we included all people for whom baseline data was available, regardless of each person’s participation in treatment. Some of the scheduled urine tests were missed by participants. To determine whether different coding schemes for the missed tests would produce different substantive conclusions, we conducted 3 types of analyses: (1) assuming missing data were drug-positive, (2) treating missing data as missing, and (3) carrying forward the previous observation. Although abstinence prevalence—the proportion of participants who were abstinent—differed across these approaches, the substantive conclusions were consistent. Thus, we report results obtained by the standard approach of treating missing data as drug-positive, with the exception that data missing for administrative reasons (test scheduled but not conducted owing to computer problems, daily test schedule received too late, tests scheduled on clinic holidays) were treated as randomly missing. Too few urine specimens were collected for analysis beyond month 6.
For our estimate of weekly abstinence prevalence, we used generalized estimating equation (GEE) extensions of generalized linear models to assess differences between housing groups and to determine whether group differences in abstinence were modified by treatment attendance.28 We used an initial model to estimate abstinence as a function of housing group and study phase. We used Wald tests based on Liang and Zeger’s procedure28 to test for group differences across each phase. We used a second model to estimate abstinence as a function of housing group, study phase, and treatment attendance. To estimate consecutive weeks of abstinence, we used an analysis-of-variance model to test for differences between housing groups, with and without control for treatment attendance.
We used Wilcoxon rank sum tests to assess group differences in days housed and days employed. Changes in days housed and days employed from baseline to 6 months and from baseline to 12 months were analyzed by treatment group and overall with paired t tests.
RESULTS
Abstinence Outcomes
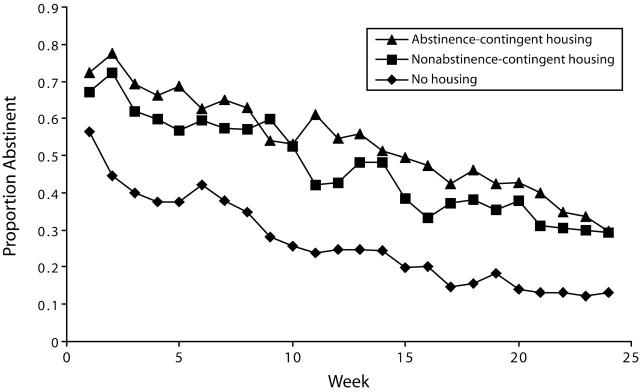
Figure 1 ▶ shows the abstinence prevalence for weeks 1 through 24; it also shows a clear separation between the ACH/NACH groups and the NH group, with the former showing consistently higher abstinence prevalence than the latter. Among the housed groups, ACH participants had higher abstinence prevalence than NACH participants during 22 of the 24 weeks, but this difference was small and not statistically significant. Table 2 ▶ shows the statistical results of the GEE model: during both phase 1 and phase 2, the ACH and NACH groups had significantly higher abstinence levels than the NH group, whereas the ACH and NACH groups did not differ from one another.
FIGURE 1—
Weekly prevalence of abstinence among participants during treatment and aftercare.
Note. ACH = abstinence-contingent housing; NACH = non-abstinence-contingent housing; NH = no housing.
TABLE 2—
Proportion (SE) of Participants Who Were Abstinent During Phases 1 and 2 of Treatment: Results of Generalized Estimating Equation Model
| Prevalence Within Attendance Group (SE) | ||||||
| Abstinence Prevalence (SE)a | Low Attendersb | High Attendersc | ||||
| Phase 1 | Phase 2 | Phase 1 | Phase 2 | Phase 1 | Phase 2 | |
| NH | 0.41 (0.044) | 0.18 (0.036) | 0.25 (0.038) | 0.08 (0.016) | 0.56 (0.053) | 0.25 (0.038) |
| NACH | 0.60 (0.038) | 0.40 (0.043) | 0.42 (0.066) | 0.21 (0.038) | 0.64 (0.035) | 0.51 (0.048) |
| ACH | 0.69 (0.045) | 0.46 (0.046) | 0.45 (0.063) | 0.29 (0.048) | 0.82 (0.029) | 0.60 (0.047) |
Note. NH = no housing; NACH = non-abstinence-contingent housing; ACH = abstinence-contingent housing.
aPhase 1 Wald tests showed an overall treatment effect (P < .0001), with pairwise differences between the NH and ACH groups (P < .0001) and the NH and NACH groups (P = .0015) but no evidence of a difference between the NACH group and the ACH group (P = .17). The results for phase 2 also showed an overall treatment effect (P = .0001), with pairwise differences between the NH and ACH groups (P < .0001) and the NH and NACH groups (P = .0003) but no evidence of a difference between the NACH group and the ACH group (P = .29).
bAmong low attenders, phase 1 Wald tests showed an overall treatment effect (P = .010), with pairwise differences between the NH and ACH groups (P = .0080) and the NH and NACH groups (P = .032) but no evidence of a difference between the NACH group and the ACH group (P = .69). The results for phase 2 also showed an overall treatment effect (P = .0009), with pairwise differences between the NH and ACH groups (P = .0007) and the NH and NACH groups (P = .010) but no evidence of a difference between the NACH group and the ACH group (P = .21).
cAmong high attenders, phase 1 Wald tests showed an overall treatment effect (P = .0005), with pairwise differences between the NH and ACH groups (P = .0004) and the ACH and NACH groups (P = .0011) but no evidence of a difference between the NACH group and the NH group (P = .26). The results for phase 2 also showed an overall treatment effect (P = .010), with pairwise differences between the NH and ACH groups (P = .0024) and the NH and NACH groups (P = .0011) but no evidence of a difference between the NACH group and the ACH group (P = .19).
Because a string of consecutive weeks of abstinence could include the treatment phase transition, phase was not included as a factor in the analyses. Mean (SD) consecutive weeks of abstinence (out of a possible 24 weeks) for the NH, NACH, and ACH groups were 4.48 (4.98), 6.60 (6.32), and 8.32 (6.79), respectively. Analysis of variance showed an overall group effect (P = .0020), with strong evidence of a difference between the NH and ACH groups (P = .0004), but no evidence of a difference between the NH and NACH groups (P = .058) or between the NACH and ACH groups (P = .091).
On the basis of previous experience,29,30 we defined participants who completed 20 or more treatment days during a single phase as high attenders for that phase. Participants who had fewer than 20 treatment days during a phase were defined as low attenders for that phase. During phase 1, mean (SD) days attended for the NH, NACH, and ACH groups were 18.3 (12.2), 26.7 (9.3), and 24.9 (11.5), respectively, with strong evidence of differences between the NH group and the NACH group (P < .0001) and the NH group and the ACH group (P = .0010) but no evidence of difference between the NACH group and the ACH group (P = .35). After summation across both phases, mean (SD) days attended for the NH, NACH, and ACH groups were 32.0 (28.4), 56.6 (29.9), and 50.1 (29.1), respectively, with strong evidence of a difference between the NH group and the NACH group (P < .0001) and the NH group and the ACH group (P = .0005), but no evidence of a difference between the NACH group and the ACH group (P = .21).
We used a second GEE model to examine the abstinence prevalence as a function of housing group, phase, and attendance. As shown in Table 2 ▶, attendance modified the housing group effect. In both phase 1 and phase 2, low attenders in the ACH and NACH groups had greater abstinence than low attenders in the NH group, with no evidence of a difference between NACH and ACH low attenders. Among high attenders, the phase 1 data showed a clear trend for higher abstinence prevalence in the ACH group, followed by the NACH group, with the lowest abstinence again in the NH group. The phase 2 results for high attenders were comparable to the results for low attenders, but the point estimates suggested greater difference between ACH and NACH high attenders than was observed between ACH and NACH low attenders.
Results for consecutive weeks of abstinence differed somewhat from results for abstinence prevalence. To assess the effect of attendance on the relationship between housing group and sustained abstinence, we fit a series of linear models with an ordinal measure of attendance that included treatment days in both phases. Participants were classified as low attenders if their attendance was low during both phase 1 and phase 2, as intermediate attenders if their attendance was low during one phase and high during the other, and as high attenders if their attendance was high during both phases. A model including housing group, attendance, and an interaction term showed no evidence of effect modification (P = .34 for the interaction). A model without the interaction term showed that attendance acted as an intervening variable for the housing group effect. This analysis provided strong evidence of an overall housing group effect after adjustment for attendance (P = .0080) and an effect of attendance on abstinence (P < .0001). The mean adjusted consecutive weeks of abstinence for the NH, NACH, and ACH groups were 5.28, 4.68, and 7.32, respectively, with evidence of a difference between the ACH group and the NH group (P = .024) and between the ACH group and the NACH groups (P = .0031), but no evidence of a difference between the NACH group and the NH group (P = .51).
As previous studies of homelessness have observed,21,22 our participants missed scheduled urine tests for administrative and other reasons. Data missing for administrative reasons were comparable across groups, ranging from 17% to 21% in phase 1 and from 8% to 11% in phase 2. Data missing for other reasons differed across groups and increased throughout the study, with phase 1 missing rates of 43%, 21%, and 14% and phase 2 missing rates of 67%, 43%, and 35% for the NH, ACH, and NACH groups, respectively. Although these rates are less than ideal for study purposes, sensitivity analyses indicated that our results are robust across all approaches to handling the missing data (data not shown).
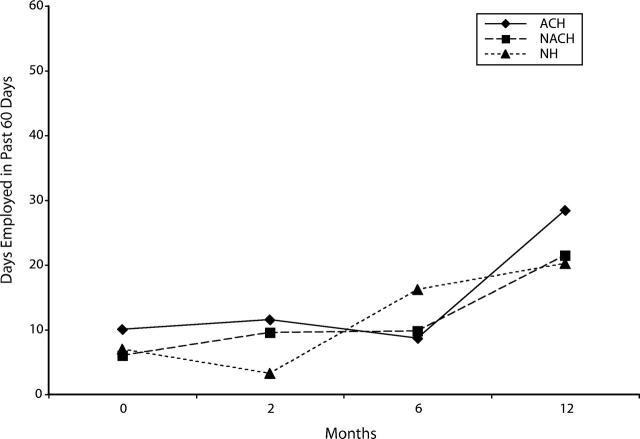
Homelessness Outcomes
Results for days housed are shown in Figure 2 ▶ and provide strong evidence of within-group housing changes from baseline to 12 months for all groups (P < .0001) and for each group (ACH, P < .0014; NACH, P < .0006; NH, P < .021). No significant within-group differences from baseline to 6 months were found for any group, and the groups did not differ significantly from each other at any time point.
FIGURE 2—
Mean days housed at baseline and at 3 follow-up assessments.
Note. ACH = abstinence-contingent housing; NACH = non-abstinence-contingent housing; NH = no housing.
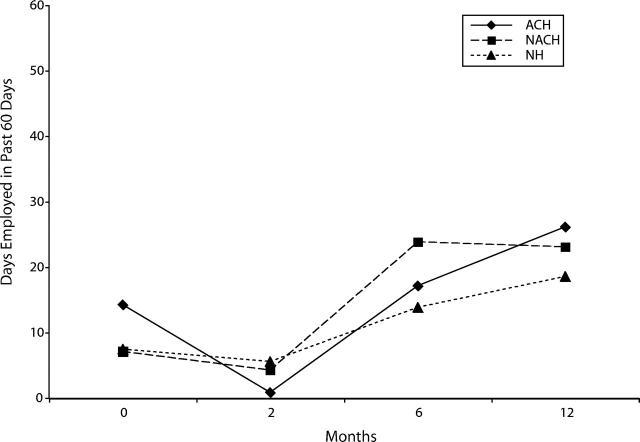
Employment Outcomes
Results for days employed are shown in Figure 3 ▶ and provide strong evidence of within-group employment changes from baseline to 6 months and from baseline to 12 months for all groups combined (both P < .0001). No evidence of significant differences between the groups was found at any time point. Separate analyses within each group from baseline to 6 months showed significant differences for 2 of the 3 groups (ACH, P = .28; NACH, P < .0001; NH, P = .052). Separate group analyses from baseline to 12 months showed significant employment changes for all groups (ACH, P = .0014; NACH, P = .0006; NH, P = .021).
FIGURE 3—
Mean days employed at baseline and at 3 follow-up assessments.
Note. ACH = abstinence-contingent housing; NACH = non-abstinence-contingent housing; NH = no housing.
Retention During Follow-Up Assessments
The percentage of follow-up assessments completed did not differ between the 2 housed groups, but more participants were retained in the housed groups than in the NH group: 66.7% for ACH, 62.7% for NACH, and 42.4% for NH (χ2=8.19; df=2; P=.017).
Gender-Specific Effects
In exploratory analyses, we examined the relationship of gender to the outcomes of housing, employment, and abstinence. We found no evidence that gender acted as an effect modifier or a confounder in the relationship of treatment with any of the 3 outcomes.
DISCUSSION
Greater abstinence and attendance in the housed groups compared with the nonhoused group, for both abstinence variables (prevalence and continuous weeks of abstinence), supports our first hypothesis regarding the important role of housing in treatment of homeless substance abusers. The positive effects of housing were maintained after control for the contribution of attendance to abstinence.
The results related to our second hypothesis, that abstinence-contingent housing would improve outcomes more than non–abstinence-contingent housing, were more ambiguous. The ACH group had a consistently higher abstinence prevalence than the NACH group during the 24-week study period; this difference was not statistically significant but may be clinically important. However, by the more rigorous measure of consecutive weeks of abstinence, the ACH group was significantly more successful in maintaining abstinence than the NH group, whereas the NACH group was not more successful than the NH group. Moreover, for both abstinence variables, the ACH group’s abstinence levels were clearly superior to those of the NACH group after control for attendance, especially among high attenders early in treatment. Employment and housing outcomes were similar to those seen in our previous study, which also showed gains from baseline to 12 months with no differences between groups.32
The consistent trend of higher weekly abstinence prevalence in the ACH group compared with the NACH group and the significantly higher weekly abstinence prevalence among high attenders in the ACH group compared with the NH group (but not in the NACH group vs the NH group) all are consistent with our second hypothesis and support the clinical and administrative value of providing abstinence-contingent housing during drug treatment. In a previous study we conducted,31 ACH and NACH participants shared an apartment complex, a situation that resulted in clinical and management difficulties. In that study, several homeless clients assigned to ACH refused the free housing (a response previously unobserved in more than a decade of work with homeless substance abusers), stating that they were not yet “strong enough” to resist using drugs while fellow NACH clients used them regularly. Additionally, Birmingham Health Care incurred property losses owing to actions of NACH participants, and some NACH clients experienced incidents of being robbed and other crimes.
In our previous studies,21,22 abstinence among the housed group was clearly superior, but the provision of housing and the abstinence contingency were confounded for the housed group. Those studies and the current study suggest that provision of abstinence-contingent housing may both support higher abstinence and be easier to manage. Thus, available evidence supports serious consideration by public agencies serving homeless substance abusers of a policy to require abstinence-contingent housing during drug treatment.
Unlike previous studies,21,22 participants in the ACH and NACH groups in the current study could work and earn a stipend when they were not abstinent, and ACH participants could use their earnings to purchase other housing while barred from program-provided housing because of nonabstinence. This ability to access and use funds for secondary when a person was between abstinence and access to treatment program activities may have weakened abstinence support by weakening the effect of the abstinence contingency on housing allowance, especially during months 3 through 6, relative to the earlier studies.
This trial’s demonstration of the positive effect of housing, with or without an abstinence requirement, could be interpreted as favoring arguments for minimal or no barriers to housing entry during the rehabilitation of homeless persons. However, observed benefits accrued among persons who consented to participate in an addiction treatment trial, so it is unknown whether housing would confer similar benefits on addicted persons uninterested in treatment.
The current study is part of a series intended to examine the impact of applying contingency management (CM) interventions to substance use disorders. In a comparison of CM and CB treatment in polydrug abusers, Rawson and colleagues33 found that whereas CM interventions produced better short-term outcomes, CB treatment produced better long-term outcomes. However, when Higgins and colleagues34 conducted a trial that compared voucher reinforcements that were contingent or not contingent on abstinence, in a population with less severe addiction and rehabilitation problems than the current study, they observed greater abstinence at 15 months’ follow-up in the abstinence-contingent voucher group than in the non–contingent abstinence voucher group. Maude-Griffin and colleagues35 also observed treatment differences for cocaine-dependent outpatients at long-term follow-up after day treatment. These treatment successes using CM suggest that long-term abstinence may be obtainable in cocaine dependence treatment with behaviorally based procedures. However, no study with a cocaine-dependent homeless population has yet shown persistent abstinence gains beyond 6 months.
The most important limitation of this study concerns the missing data. We were unable to obtain sufficient assessments of abstinence beyond 6 months, and many scheduled urine tests during months 1 through 6 were missed by participants. High rates of missing data are a significant concern. However, 3 conventional analytic approaches for dealing with missing data yielded consistent results in group comparisons. Furthermore, we reported the results with the most conservative of the procedures (coding missed tests as drug-positive), an approach that underestimates actual abstinence for all groups. Finally, missing data and less-than-ideal analytic procedures for missing data were not unique to this study but are chronic problems in the substance abuse treatment field. Better methods for addressing these concerns would have improved this study, just as they would improve all such studies.
Provision of housing during day treatment of homeless substance abusers was associated with greater drug abstinence. This study has clear implications for treatment and housing of homeless substance abusers.
Acknowledgments
Data collection and manuscript preparation were supported by the National Institutes of Health (grants DA08475 and DA11789, respectively).
The following individuals contributed substantial assistance: Jonathan Dunning, MA, Sonja Frison, PhD, Stefan Kertesz, MD, Cecelia McNamara, PhD, Max Michael, MD, Mary A. Plant, PhD, Stewart Usdan, PhD, and Catherine Ward, PhD.
Human Participant Protection All procedures and research reported here were reviewed, approved, and monitored by the University of Alabama at Birmingham institutional review board for Human Research.
Peer Reviewed
Contributors J. B. Milby and J. E. Schumacher originated the study and supervised implementation. D. Wallace completed all data analyses and assisted in data interpretation and writing. M. J. Freedman supervised day-to-day implementation of the 3 experimental groups, data collection, and data review and participated in manuscript preparation. R. E. Vuchinich coordinated urine database preparation and, with D. Wallace, participated in data review, data interpretation, and manuscript preparation.
References
- 1.Link BG, Susser E, Stueve A, Phelan J, Moore RE, Struening E. Lifetime and five-year prevalence of homelessness in the United States. Am J Public Health. 1994;84:1907–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reardon ML, Burns AB, Preist R, Sachs-Ericsson N, Lang AR. Alcohol use and other psychiatric disorders in the formerly homeless and never homeless: prevalence, age of onset, comorbidity, temporal sequencing, and service utilization. Subst Use Misuse. 2003;38: 601–644. [DOI] [PubMed] [Google Scholar]
- 3.Link B, Phelan J, Bresnahan M, Stueve A, Moore R, Susser E. Lifetime and five-year prevalence of homelessness in the United States: new evidence on an old debate. Am J Orthopsychiatry. 1995;65:347–354. [DOI] [PubMed] [Google Scholar]
- 4.Webb DA, Culhane J, Metraux S, Robbins JM, Culhane D. Prevalence of episodic homelessness among adult childbearing women in Philadelphia, PA. Am J Public Health. 2003;93:1895–1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burt MR, Aron LY, Douglas T, Valente J, Lee E, Iwen B. Homelessness: Programs and the People They Serve. Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, DC: Urban Institute; 1999. Available at: http://www.huduser.org/publications/homeless/homeless_tech.html. Accessed March 23, 2005.
- 6.Burt MR, Aron LY. Helping America’s Homeless. Washington, DC: Urban Institute; 2001.
- 7.Herman D, Susser ES, Struening EL, Link BL. Adverse childhood experiences: are they risk factors for adult homelessness? Am J Public Health. 1997;87: 249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smereck G, Hockman EM. Prevalence of HIV infection and HIV risk behaviors associated with living place: on-the-street homeless drug users as a special target population for public health intervention. Am J Drug Alcohol Abuse. 1998;24:299–319. [DOI] [PubMed] [Google Scholar]
- 9.Martens W. A review of physical and mental health in homeless persons. Public Health Rev. 2001; 29:13–33. [PubMed] [Google Scholar]
- 10.Plumb JD. Homelessness: care, prevention, and public policy. Ann Intern Med. 1997;126:973–975. [DOI] [PubMed] [Google Scholar]
- 11.Hwang SW. Is homelessness hazardous to your health? Obstacles to the demonstration of a causal relationship. Can J Public Health. 2002;93:407–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corrigan EM, Anderson SC. Homeless alcoholic women on skid row. Am J Drug Alcohol Abuse. 1984; 10:535–549. [DOI] [PubMed] [Google Scholar]
- 13.Galanter M, Egelko S, De Leon G, Rohrs C, Franco H. Crack/cocaine abusers in the general hospital: assessment and initiation of care. Am J Psychiatry. 1992;149:810–815. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994; 51:8–19. [DOI] [PubMed] [Google Scholar]
- 15.Koegel P, Burnam MA, Farr RK. The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45:1085–1092. [DOI] [PubMed] [Google Scholar]
- 16.Rahav M, Link BG. When social problems converge: homeless, mentally ill, chemical misusing men in New York City. Int J Addict. 1995;30:1019–1042. [DOI] [PubMed] [Google Scholar]
- 17.Rahav M, Rivera JJ, Nuttbrock L, et al. Characteristics and treatment of homeless, mentally ill, chemical-abusing men. J Psychoactive Drugs. 1995;27:93–103. [DOI] [PubMed] [Google Scholar]
- 18.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 19.Rosenheck R, Leda C, Gallup P, et al. Initial assessment data from a 43-site program for homeless chronic mentally ill veterans. Hosp Community Psychiatry. 1989;40:937–942. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien CP, Alterman A, Walter D, Childress AR, McLellan AT. Evaluation of treatment for cocaine dependence. NIDA Res Monogr. 1989;95:78–84. [PubMed] [Google Scholar]
- 21.Milby JB, Schumacher JE, Raczynski JM, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend. 1996; 43:39–47. [DOI] [PubMed] [Google Scholar]
- 22.Milby JB, Schumacher JE, McNamara C, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug Alcohol Depend. 2000;60: 55–67. [DOI] [PubMed] [Google Scholar]
- 23.Stewart B. McKinney Homelessness Assistance Act (1987), Public Law 100-177.
- 24.Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised. Washington, DC: American Psychiatric Association; 1987.
- 25.Derogatis LR. SC-R-90: Administration, Scoring and Procedures Manual. Baltimore, Md: Clinical Psychometric Research; 1977.
- 26.Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90-R: a study in construct validation. J Clin Psychol. 1977;33:981–989. [Google Scholar]
- 27.Drake RE, McHugo GJ, Biesanz JC. The test-retest reliability of standardized instruments among homeless persons with substance use disorders. J Stud Alcohol. 1995;56:161–167. [DOI] [PubMed] [Google Scholar]
- 28.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73: 13–22. [Google Scholar]
- 29.Schumacher JE, Milby JB, Caldwell E, et al. Treatment outcome as a function of treatment attendance with homeless persons abusing cocaine. J Addict Dis. 1995;14:73–85. [DOI] [PubMed] [Google Scholar]
- 30.Schumacher JE, Usdan S, Milby JB, Wallace D, McNamara C. Abstinent-contingent housing and treatment retention among crack-cocaine-dependent homeless persons. J Subst Abuse Treat. 2000;19:81–88. [DOI] [PubMed] [Google Scholar]
- 31.Milby JB, Schumacher JE, McNamara CL, Usdan SL, Wallace D, Frison S, et al. Abstinent vs non-abstinent contingent housing for cocaine dependent homeless: effects of housing together or apart. Paper presented at: College on Problems of Drug Dependence 62nd Annual Scientific Meeting; June 17–22, 2000; San Juan, Puerto Rico.
- 32.Milby JB, Schumacher JE, Wallace D, et al. Day treatment with contingency management for cocaine abuse in homeless persons: 12-month follow-up. J Consult Clin Psychol. 2003;71:619–621. [DOI] [PubMed] [Google Scholar]
- 33.Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Ling W. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Arch Gen Psychiatry. 2002;59:817–824. [DOI] [PubMed] [Google Scholar]
- 34.Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol. 2000;68:64–72. [DOI] [PubMed] [Google Scholar]
- 35.Maude-Griffin PM, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, Hall SM. Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol. 1998;66:832–837. [DOI] [PubMed] [Google Scholar]