Abstract
Historical work on cancer has suggested that a range of political, social, and medical concerns stimulated the emergence of cancer as a public health problem in the early 20th century.
I argue that anxiety about cervical cancer mortality was instrumental in establishing cancer as a major focus of concern for the British public health service. This development was closely bound to assumptions about the association of gender with cancer, the redefinition of cancer as a surgical problem, the politics of empire, and the climate of public and medical disquiet about gynecological surgery engendered by feminist and antivivisectionist critiques of medical science.
CANCER IS AN OLD DISEASE, but its emergence as a social, medical, economic, and political concern is a new phenomenon. Efforts to understand and control the disease were stimulated in the early 20th century by concerns over rising cancer mortality, and sustained by the particular interests of key social groups: medical specialists (especially surgeons and radiation specialists), wealthy philanthropists, politicians, insurance companies, feminists, and health reform organizations.
Thanks to the work of historians, notably James Patterson, Barron Lerner, Barbara Clow, Pierre Darmon, Patrice Pinell, Robert Proctor, and David Cantor, we are now beginning to understand something about the dynamics of the process of social recognition of and response to cancer in different national contexts.1 For example, in France it was concern about older age groups recruited into the army during World War I that prompted the establishment of cancer treatment centers.2 In the United States, anxiety about breast and cervical cancer stimulated the establishment in 1913 of the American Society for the Control of Cancer, a powerful alliance of insurance interests, wealthy philanthropists, and leading doctors—especially surgeons and gynecologists.3
Surgeons and gynecologists were also prominent in the anti-cancer campaigns launched in Britain in the early 20th century. Their role in shaping prevention policies and treatment options for women cannot be underestimated, yet little is known about the social and professional dynamics that ensured their prominence in the organized fight against cancer.4 I explore the way in which medical concern about gynecological cancer helped establish the disease as a major focus for public health intervention in early 20th-century Britain. This history is closely intertwined with assumptions about the association of gender with cancer; the redefinition of cancer as a surgical problem; the politics of empire, which served to direct public and medical attention to the health of working-class mothers; and a climate of feminist and antivivisectionist opposition to gynecological surgery.
A FEMALE DISEASE
Noting that cancer mortality was on the rise among men, a late-19th-century writer argued that “want of proper exercise, and excess of food” were emasculating men and leaving them subject to “women’s diseases.”5 The perception that cancer was a “female” disease was based on the observation that women were especially liable to cancer of the breast and uterus. This view had a long history, but it was no doubt reinforced during the 19th century by the belief that disease of the reproductive organs defined “woman’s nature”: “La femme est une malade,” wrote the 19th-century French historian Jules Michelet (1798–1874).
In 1846, Walter H. Walshe, author of the standard textbook on cancer in the mid-19th century, drew attention to the connection between gender and cancer: “There is no fact in the history of cancer more absolutely demonstrated than the influence exercised by sex on its development,” he said. “The female population of this country is destroyed to about two and three quarter times as great an extent by cancer as the male—a difference the more remarkable from the fact, that the mean rate of mortality from all diseases is 20.8 per thousand among males, while it is 19.7 among females.”6
Walshe’s claims were supported by figures drawn from the mortuary registers for the Paris region, and by the national statistics of disease that the British government had been collating since 1837. The former were of particular interest to Walshe as they showed the comparative proneness of different organs to cancer. The data revealed that between 1830 and 1840, cancer had claimed 9118 lives in and around Paris. Of these deaths, 2996 had been attributed to uterine cancer (a term that applied both to cancer of the body of the uterus and to cancer of the cervix uteri), 1147 to cancer of the female breast, and 64 to ovarian cancer. By contrast, cancer of the testicles had claimed 21 lives, while deaths from cancer of the prostate and of the male breast only numbered 5 each. Although the gender ratio in the remaining 4880 cases (i.e., 53.5% of the total) was not stated, Walshe concluded “that sex exercises a powerful influence on the point under consideration is obvious.”7
By this, Walshe meant that women were at special risk from cancer because of their biological role in reproduction—a point that his contemporaries already took for granted, although they might have disagreed about the precise mechanisms. Walshe suggested that cancer was associated with menopause, but many of his colleagues believed that women’s liability to cancer was due instead to the intermittent and periodical activity of the reproductive system.8 Others blamed “nutritional” disturbances caused by repeated pregnancies. This applied in particular to cervical cancer, which was widely associated with multiparity.9
Figure 1.
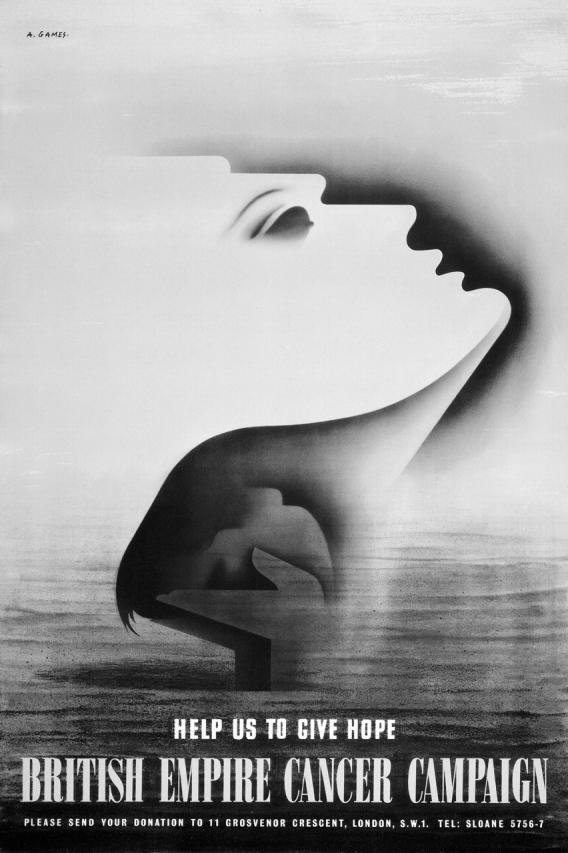
“A Matter of Imperial Concern.” The association of cancer with women continued well beyond the period under consideration. In this 1947 anticancer propaganda poster, a ghostly female profile is juxtaposed with the image of a hand releasing a bird, symbolizing Britain’s hopes of defeating cancer. (Courtesy of the Abram Games Estate, and of the Wellcome Library for the History and Understanding of Medicine, London)
Mid-19th-century medical practitioners believed cancer to be a constitutional disorder produced by some kind of morbid alteration of the body’s fluids. It was a systemic disease with local manifestations. By “constitutional,” doctors also meant that cancer was a hereditary and incurable disease: what people inherited was not the disease itself, but the potential for it. Heredity was deemed to be a risk factor, particularly in female cancer. Indeed, some mid-19th-century clinicians cited the tendency for breast and uterine cancer to run in families as evidence of the inheritability of the disease in general.10 Although little statistical evidence existed for the transmissibility of disease, physicians applied the notion of hereditary predisposition to other chronic diseases like gout, tuberculosis, and insanity, perhaps in an attempt to justify their inability to provide efficacious cures.11
Predisposing causes could be acquired as well as inherited. Acquired causes included not only biological sex, but also temperament, general state of health, diet, immoral habits, unhappy emotions, place of residence, and occupation. Both sets of causes prepared the individual for the action of direct or “exciting” causes, namely, local injury and “irritation.” Breast cancer, for instance, was widely attributed to trauma, while cervical cancer was sometimes blamed on the irritation caused by excessive sexual activity.
In both sexes, however, individual predisposition was regarded as more important than the influence of extrinsic causes. This was because practitioners realized that not all the people exposed to trauma or irritation developed cancer. As Walshe argued, influences external to the individual played but an “accidental and subsidiary role” in the etiology of cancer. Individual predisposition or “constitutional aptitude” was “a necessary condition” for the production of the disease.12 Physician James Copland (1791–1870), author of the Dictionary of Practical Medicine, stressed that “although irritating agents of any description may give occasion to its appearance, . . . there must have previously existed cancerous diathesis, or constitutional disposition, in which it almost always originates.”13 In many cases, cancer appeared to be an entirely spontaneous disease, precipitated by internal factors that medicine could not explain.
This framework had implications for prevention and treatment—what Walshe called prophylactic and curative “treatment,” respectively.14 Because cancer, in Copland’s words, essentially depended “upon a weakened and otherwise morbid state of the system generally” arising from “original or acquired diathesis,” means of prevention and cure referred primarily to the state of the constitution that favored its development and progress.15 A hereditary taint could not be eradicated, but its effects could be mitigated through changes in lifestyle and behavior. Preventive measures promoted a state of general healthfulness, with an emphasis on good food, clean air, proper clothing, sufficient rest, and exercise. “Tainted” individuals were also advised to avoid exhausting, stressful occupations. Work as a governess—the only “respectable” occupation for the unmarried upper-middle-class woman—was not an option for the female with a family history of cancer.16
As with most other hereditary conditions associated with a dismal prognosis, the aim of treatment for malignancies was palliation rather than cure. Therapies were used in a holistic way, to lower the activity of the system. Patients suffering from cervical cancer, for example, were advised to eat in moderation, avoid all exertion, keep the bowels open and avoid sexual activity. In advanced cases, cauterization was practiced.17 Opium and morphine were freely prescribed to alleviate the pain of terminal cancer.
The question of surgical treatment for gynecological cancer was regularly discussed during the first half of the 19th century. In the early part of the century, amputation of the cervix for malignant cancer enjoyed a brief vogue, but the practice was soon rejected as “cruel and unscientific.”18 As cancer was deemed to be a constitutional disorder, it made little sense to remove cancerous growths: sooner or later the underlying cancerous diathesis would reassert itself and the disease would return. Furthermore, operative treatment was risky and the probability that it might actually hasten the death of the patient was constantly in the mind of practitioners. Most medical authorities thus cautioned against surgical treatment in gynecological and other cancers, particularly where the operation involved cutting deep into the body.19
Attitudes toward surgery were transformed during the second half of the century as constitutional theories of disease gradually lost ground. From about 1860 onward, cancer was increasingly understood as a local disease contained in particular tissues and organs. This change has been characterized by historians as a move from physiological to ontological conceptions of disease and an emergence of a more reductivist approach to prevention and treatment.20
The rise of localist views of disease and of anatomical constructions of the body owed much to the growing influence of surgeons relative to physicians. It provided new possibilities for surgical intervention, not only in repairing and removing damaged parts but also in the treatment of internal diseases that until then had been the province of physicians.21 By the end of the 19th century, generalists were being urged not to “temporize” with medical treatments in cases of malignancy, but to refer patients early for tumor extirpation.
A SURGICAL DISEASE
The localist view was championed in Britain in the 1860s by surgeons Charles Moore and William De Morgan of the Middlesex Hospital in London, where a cancer ward had been in existence since the late 18th century. Following Rudolf Virchow (1821–1902), the German founder of cellular pathology, Moore and De Morgan argued that all cancers originated from degenerative changes in the cells. They claimed that cancer was curable if treated by an “early and adequately extensive operation,” before it had had a chance to spread to distant body sites.22
Moore’s and De Morgan’s support for the localist theory was inspired in part by concerns about the stigma associated with the notion of cancerous diathesis. Culturally, a family history of chronic disease evoked a picture of weakness and undesirable qualities. A poor family record of health could blight people’s lives socially, economically, and emotionally: life insurance companies penalized those with a “bad heredity,” and the fear of marrying into hereditarily tainted families was well entrenched in British society.23 Moore’s argument was that the fear of stigmatization prompted people to conceal their symptoms and delay seeking medical advice until the disease was too advanced for treatment. People needed to understand, first, that cancer affected the healthiest and strongest individuals and, second, that it was curable if detected and removed early. Any inherited peculiarity was not systemic, but local.
Surgeons, of course, had a direct interest in combating the stigma of cancer. They needed to boost public confidence in the efficacy of orthodox treatment, so as to reduce the competition they faced from the vast army of irregular healers who catered to people suffering from the disease.24 Cancer curers claimed success in cases that orthodox medicine had abandoned as hopeless, cashing in on doctors’ inability to cure the disease. They challenged doctors’ authority and hit them where it hurt most: their wallets.
Perhaps not surprisingly, by the mid-1880s constitutional explanations of cancer were in eclipse as a new generation of surgeons, obstetricians, and pathologists eagerly embraced the local theory of cancer. Localists were especially concerned to debunk the idea that cancer was a hereditary disease, because the notion of inheritability precluded the possibility of surgical treatment.25 As cancer specialist Herbert Snow, an antihereditarian, argued in 1883, belief in the inheritability of cancer was a fallacy that served only “to hide our ignorance of cancerous causation . . . [and] to proclaim the uselessness and hopelessness of surgical treatment.”26 Snow was echoed by surgeon Hugh Percy Dunn, who declared in 1883:
I believe that the pregnancy, so to speak, of the non-identity of cancer with heredity has begun, . . . and that in the future we shall be able to show unequivocally that there is no such thing as the hereditary transmission of cancer. . . . What, if we cannot show directly that cancer is not hereditary, can the surgeon hope for from operative treatment? What more than despair can the suffering patient exhibit whose disease has been pronounced as hereditary by the attending surgeon?27
Some localists did concede that some sort of constitutional vulnerability to the disease may be important. They insisted, however, that any susceptibility of the person to cancer was more likely to be caused by environmental than by hereditary factors. As Ernest Bashford, the first director of the Imperial Cancer Research Fund, argued in 1908, “there are . . . constitutional conditions which are favorable, and others which are unfavorable, to the growth of cancer, and they can be induced experimentally at will.”28 For example, according to Bashford, the susceptibility of English mice to transplantable carcinomata could be modified by prolonged sojourn in Norway. Others emphasized the importance of direct exciting causes: “[T]he strongest argument against heredity to my mind,” wrote Herbert Snow in 1898, “is afforded by the fact that no case ever arises without a direct and definite exciting cause whether there be cancerous relatives or not.”29 According to Snow, cases in which several members of a family had succumbed to cancer could be readily explained in terms of the depressing influence of unhappy emotions.30
The redefinition of cancer as a local disease proceeded pari passu in gynecology. In Allbutt’s and Playfair’s System of Gynaecology (1896), for example, leading obstetrician William Japp Sinclair claimed that “in cancer of the uterus . . . [heredity] appears to be a factor of little etiological importance.”31 Some medical writers did acknowledge the importance of predisposing factors such as poor diet and overwork. Nonetheless, they insisted that exposure to exogenous exciting causes, such as trauma and “chronic irritation,” was a necessary condition for the production of the disease.
Sinclair, for instance, believed that poor social conditions favored the development of cancerous afflictions. He observed, however, that
when we follow such suggestions as possible causal relations between cancer of the uterus and constitution, temperament, occupation, and previous illnesses not connected with infection or traumatism of the sexual organs, anomalies of menstruation, sexual excess, and such like, we can find no trace of a constant factor.32
Injury and the irritation from tight dresses and corsets were widely blamed for breast cancer, while accounts of cervical cancer usually cited lack of personal hygiene, venereal disease, and the recurrent lacerations, abrasions, and infections associated with multiparity and poor obstetric care.
Belief in the exogenous origin of cancer was reinforced in the 1880s by reports that germs and parasites had been detected in cancerous cells. The “infectious theory” of cancer was controversial, but for some it provided a plausible explanation for women’s proclivity to cancer of the reproductive system. As a general practitioner remarked in 1902, “the loose and open arrangement of the nether garments of the majority of women would naturally favour access to the generative organs of the infective microorganism.”33 It was not unreasonable to suppose that, once the cancer germ had gained access to women’s reproductive organs, it would go on to penetrate the interior of the body via the fissures and lesions so common in women who had borne children.
Happily, women were relatively immune to cancers of the lip and oral cavity, which were commonly associated with “male” habits such as smoking and drinking. Long-continued irritation from unglazed pipe stems and alcohol, it was claimed, was a risk factor in buccal cancer, as was poor oral hygiene—another department where men fared badly compared with women.34
The new emphasis on the action of exogenous “irritants” established the association of cancer with conditions that sanitarians had long recognized as causes of mortality in the population: bad water, bad air, dirty and immoral habits. The sanitarian framework was reflected in the emergence of notions of prevention tightly focused on the theme of hygiene. Recommended preventive measures at the turn of the century stressed the need for improved sanitation, including the disinfection of houses and the cremation of bodies, the use of pure drinking water, scrupulous personal cleanliness, and the use of the Turkish bath; appropriate clothing, diet, and exercise; moderate alcohol consumption; and general observance of the laws of health.35
With regard to cancer, prophylactic hygiene importantly involved attending to what British anticancer propagandist Charles Childe called the “toilette” of those parts of the body where the disease commonly occurred: the skin, the mouth, and the genitals.36 This was a term that evoked the cosmetic dimensions of hygiene: the association of cleanliness with grooming and the beautification of the body.37 Closely related to the concept of grooming was the surgical correction and removal of potentially cancerous blemishes and lesions. This practice was particularly important for women, given their liability to injuries and lacerations during their childbearing years. Because cervical lesions and erosions were also a source of unpleasant discharges, such surgery was another way in which hygiene and cosmetic treatment came together in anticancer prophylaxis. By the early 1900s, prophylactic surgical treatments included not only the removal of warts, but also the treatment of cervical erosions and “plastic” reconstructive operations for cervical tears (Emmet’s operation, or trachelorraphy). In the more severe cases of laceration, amputation was practiced.38
The list of irritants liable to cause gynecological cancer in the last quarter of the 19th century included a new threat: unclean male genitalia. The view that male sexuality was a source of physical and moral pollution was largely because of the propaganda activities of the social purity movement, a coalition of feminists, medics, evangelicals, and nonconformist Protestants who were seeking to reshape the nation’s morals.39 Purists campaigned against sinful activities like masturbation, denounced the “double standard” of sexual morality, and stressed the importance of chastity and moral restraint for both men and women. In this context, men’s foreskins emerged as a major public health hazard. Doctors claimed that the prepuce harbored dirt and germs that caused chronic irritation and led not only to masturbatory activity, but also to venereal disease and penile and cervical cancer.40 As stated in a monograph published in 1893,
The prepuce tends to keep the surface of the glans penis moist and . . . little cracks . . . are liable to occur on and around it. These may be easily inoculated by any noxious or contagious matter. . . . . Hence they are often the starting point of chancres or syphilis in young persons, and of cancer in the aged.41
The remedy was at hand, however: hygienic circumcision of all male infants. In arguing the case for circumcision, doctors drew attention to the supposedly low incidence of syphilis, gonorrhea, and cervical cancer among the Jews, hailing Moses as the author of hygienic regulations that would have done credit to the public health reformers of the 19th century.
If late-19th-century surgery was staking a claim to cancer prophylaxis, it was in the sphere of therapeutics that surgery came into its own. In the early part of the century, many practitioners had vigorously opposed operative treatment for gynecological cancer; by the late 19th century, surgery had become the treatment of choice. Indeed, some of the most spectacular developments in cancer surgery occurred in gynecology.42 The establishment of ovariotomy, the surgical removal of ovarian cysts pioneered by the American Ephraim McDowell in 1806, opened up the whole field of abdominal surgery, laying the foundation for radical operations such as Wertheim’s hysterectomy for cancer of the cervix (1898) and Schlatter’s total gastrectomy (1897).
Radical cancer surgery was justified on the grounds that total removal of the affected parts and of the surrounding healthy tissues would prevent the likelihood of recurrence, but the high operative mortality did not inspire the confidence of the British public. The development of extensive gynecological operations was a particular cause for concern in Britain, where feminist and antivivisectionist sentiment was strong. Feminists, many of whom were also antivivisectionists, claimed that gynecologists were mutilating and “unsexing” women in needless experimental operations. This belief was responsible for the myth that “Jack the Ripper,” author of a gruesome series of murders of women in 1888, was a vivisecting surgeon from London University.43
Gynecologists themselves were uneasy about the ethics of radical surgery. Survival figures showing little improvement in cure rates led many to argue that the risks of extensive surgery were unjustifiable. Practitioners in Britain (and some in America, too) were especially concerned about the dismal results achieved with total abdominal hysterectomy for cervical cancer. Some surgeons confessed that they had never had a single case of cure; others spoke gloomily of “prolonged survivals.”44 More sanguine operators adopted Halsted’s redefinition of the term cure as “freedom from recurrence for three years.”45
Most worrying for British practitioners was that the failure of gynecological cancer surgery was becoming apparent just at the time when maternal health was emerging as a major cause for public concern. In the last decades of the 19th century and first decades of the 20th century, motherhood, prompted by anxieties about high levels of infant mortality and class and race differentials in birth rates, was coming into prominence as the key to a healthy population. The belief that the production of a strong workforce and armed force depended on “maternal efficiency” gave a boost to the efforts of the emerging Mother-craft movement to improve the welfare of mothers and children. It was against this background that cancer of the cervix, a disease widely associated with multiparity and low social class, began to emerge as a major focus of medical and public health concern.
THE PROBLEM OF CERVICAL CANCER
Fears of national decline, first expressed in the late 19th century, were exacerbated by the dismal performance of the British Army during the Boer War in South Africa (1899–1902), where the Imperial Army faced near-defeat at the hands of a force that was barely trained.46 The debacle provoked intense debate about the nation’s health and the need for social reform. It also served to stimulate medical and public concern about a number of chronic diseases, from rheumatism to cancer. Although controversial at the time, the belief that cancer mortality was on the rise served to engender a climate of growing medical and public anxiety about what was rapidly becoming the “cancer problem.”47
In the early 1900s, the fight against cancer became closely identified with Britain’s imperial interests.48 Its rhetoric stressed both the domestic and international aspects of British imperial domination. Cancer was redefined as a disease of “anarchic” or “Bolshevik” cells that threatened the internal stability of the British state.49 In a reference to the tradition of state-sponsored exploration and exploitation of distant lands, the disease was also described as the “darkest Africa” on the map of medicine.50
A related theme highlighted the way in which Britain’s colonial power might further the war on cancer. In the early 20th century, philanthropic support for cancer research and treatment in Britain came from the new plutocracy of mining financiers, many of them of German-Jewish descent, who were playing a key role in the colonial exploitation of mineral resources in South Africa. Julius Wernher, of Wernher, Beit & Co, was instrumental in establishing the Imperial Cancer Research Fund in 1902, and in the late 1920s the Beit estate gave the King’s Fund for London £50 000 for the purchase of radium—an enormous sum by contemporary standards. Sir Ernest Cassel, another entrepreneur who had invested heavily in the South African mines developed by Wernher and Beit, helped establish the London Radium Institute in 1911.51
Mirroring developments in other Western countries, the British debate over the quality of the national stock and the future of the “imperial breed” stimulated new social concerns about the survival of infants and the health of mothers and schoolchildren. The belief that motherhood was the key to a healthy population gave the topic of gynecological cancer a special centrality, for cancer tended to kill older married women, most of whom had domestic and family responsibilities. Medical commentators were particularly alarmed by the prevalence of uterine cancer: “More women die of cancer of the uterus than of cancer of any other part of the body,” observed leading obstetrician Herbert Spencer in 1907. “We have . . . in cancer of the uterus a disease which carries off annually in England and Wales nearly 4,000 adult women, the great majority of them mothers—usually mothers of large families.”52
By “mothers of large families,” Spencer meant lower-class women, because it was in the poorer ranks of society that the highest rates of fertility were found. The view that uterine, and especially cervical, cancer was a “disease of poverty” was well established in gynecology by the early 1900s. In the late 1800s, Herbert Snow had argued that “a life of hard work, of occasional privation, of too frequent child-bearing and prolonged lactation, greatly predisposes [to cervical cancer].”53 William Sinclair stressed that cervical cancer occurred almost exclusively among “the chronically overworked and underfed, among women, poor, prolific, harassed, worried, drained by lactation, reposeless.”54 According to Sinclair, the predisposing causes were poor sanitation, money worries, bereavement, and physical and mental exhaustion from pregnancy and lactation, not to mention the suffering caused by childbirth trauma and the irritation from “chronically filthy genitals.” The long list included gonorrheal infections, which Sinclair blamed on the promiscuous behavior of irresponsible husbands.55
If cervical cancer was truly a disease of poverty, it was difficult to escape the conclusion that any reduction in its incidence depended on programs of social amelioration. This was indeed what Sinclair argued. In 1896, he wrote,
The hypothesis of morbus miseriae places cancer of the cervix in the same category as leprosy . . . and by analogy we may assume that cancer may be banished by social amelioration which will raise the presently existing cancer-producing class to the higher level of the presently existing immune, just as the disappearance of the horrors in the individual lives and environment of past generations has made leprosy in England an historic disease.56
In the meantime, however, the profession could not afford to remain “supine and inactive.”54(p327) Doctors needed to focus on the most easily performed public actions that could make a significant difference in the mortality from cancer. As far as Sinclair was concerned, there was only one option here: “Our Hopes of Immediate Amelioration Rest Therefore on Surgery [italics and capitalization in original].”57 Yet Sinclair was far from recommending the radical operations advocated by some of his colleagues, especially those in Germany. In Sinclair’s view, less radical operations having a smaller mortality needed to replace the “homicidal vivisections” popularized by German gynecologists. According to the localist model of cancer, the possibility for less extensive surgery rested on early diagnosis of cancer. It was in this context that Sinclair proposed that women be educated in recognizing the early symptoms of cancer.58
The movement for cancer education was boosted by fears that pessimism about the curability of cervical cancer might have a negative impact on both lay and medical opinion. As leading gynecologist Herbert Spencer argued in 1907, “Pessimistic views on the subject . . . do much harm by inducing in the mind of the public and of the profession an entirely erroneous view that cancer is incurable, and lead to delay in seeking medical advice, which would be of little consequence were it true that cancer is incurable.”59
Medical pessimism was dangerous partly because it might encourage women to resort to the services of domestic and alternative healers. In calling for “a crusade against the neglect of the well-known early symptoms of cancer of the womb,” practitioners aimed to stave off the threat by reiterating the message of hope that surgery had been offering since the 1860s: cancer is curable if detected and removed early.60
The idea of educating women in the early recognition of cervical cancer was discussed at a meeting of the British Medical Association in 1907. Gynecologists who attended this meeting were encouraged by the results obtained by gynecologist Georg Winter. It was claimed that the campaign that Winter had launched in East Prussia in the late 1800s had significantly increased public awareness of cervical cancer.61 However, in spreading their message, activists faced formidable problems of strategy and information management. The chief question for doctors to solve was the means by which the uneducated masses could be reached. Winter had taken the unusual step of using the lay press as the medium for his “Exhortation to Womankind.”61 In Britain, there was less enthusiasm for newspaper advertisements, partly because of anxieties about “cancerphobia,” partly because of concerns about the “taboo” nature of the subject. References to the “morbid and lurid aspects” of cervical cancer, such as abnormal bleeding and discharges from the vagina, doctors argued, were bound to shock the sensibilities of the public.62
Thus, rather than waging a propaganda war against the disease, British gynecologists initially opted for a low-key approach. They relied on midwives, health visitors, and sanitary associations to instruct women regarding the early symptoms of the disease and to impress on women the importance of seeking medical advice from professionals rather than from less-reputable healers. The idea was to enlist the educated upper middle classes in the medical campaign to instruct the “unreading and unthinking” members of the public, the definition used by a public health official in the 1920s.63
The British Medical Association in 1909 took the first step toward raising public awareness by creating an advice leaflet for midwives and general practitioners to use that urged practitioners to look out for the signs of the disease when they attended women in childbirth.64 By the early 1910s, local initiatives were beginning to spring up in London and the provinces. Most of these early campaigns were instigated by abdominal surgeons and gynecologists involved in municipal affairs, who used their position of influence on local public health committees to their advantage.
In Portsmouth (southwest England), for example, leading surgeon and anticancer propagandist Charles Childe was instrumental in persuading the town council to start a system of cancer education for nurses and upper-class ladies involved in philanthropic work. Portsmouth also pioneered the direct methods of propaganda (leaflets and newspaper notices) that were to become more common during the period between the world wars. The dominant message of these campaigns was that early intervention saved lives; however, preventive advice was also given with regard to chronic irritation. The leaflet issued in Portsmouth, for example, recommended the removal of warts and moles exposed to constant irritation, as well as the avoidance of irritation. It also highlighted the potential of broken teeth and clay pipes to produce cancerous lesions.65
Women’s cancers remained a prominent target of anticancer propaganda in Britain during the interwar period, despite statistics indicating that stomach cancer was the cancer type most common in both genders, and the leading cause of cancer death in men. Between 1916 and 1920, for example, there were 21195 deaths from breast cancer and 20 596 from cancer of the uterus. During the same period, 36 802 people died from stomach cancer (men and women combined), of which 19 308 were men.66 Yet very little was done to alert the public, especially men, to the danger signs of stomach cancer. In fact, it was not until the 1950s that men were drawn into the educational arena because of concern over smoking and that a gendered division of cancer began to emerge in anticancer education programs.67
Studying the history of cancer detection and treatment can help uncover and explain the reasons why a gendered understanding of cancer has played such an important role in popular cancer discourse. Understanding this history can also provide a perspective from which current beliefs and practices may be analyzed, such as the association of cervical cancer with women’s promiscuity, and the use of cancer screening as treatment strategy despite recurrent evidence that early detection does little to change overall health outcomes.68 What I have argued in this article is that in late 19th-and early 20th-century Britain, struggles for professional dominance and the politics of gender were the main factors that helped propel gynecological cancer to the top of the anticancer agenda.
Acknowledgments
The Wellcome Trust provided funds for the research that led to this article.
I am grateful to Virginia Berridge, Aileen Clarke, John Pickstone, and the 2 anonymous reviewers for their comments.
Peer Reviewed
Endnotes
- 1.Patterson James T., The Dread Disease: Cancer and Modern American Culture (Cambridge, Mass: Harvard University Press, 1987); Barron H. Lerner, The Breast Cancer Wars: Fear, Hope and the Pursuit of a Cure in Twentieth-Century America (New York: Oxford University Press, 2003); Barbara Clow, Negotiating Disease: Power and Cancer Care, 1900–1950 (Montreal: McGill-Queen’s University Press, 2001); Pierre Darmon, Les cellules folles: l’homme face au cancer de l’Antiquité à nos jours (Paris: Librairie, Plon, 1993); Patrice Pinell, The Fight Against Cancer: France 1890–1940 (New York: Routledge, 2002); Robert N. Proctor, The Nazi War on Cancer (Princeton, NJ: Princeton University Press, 1999); David Cantor, “Cancer,” in Companion Encyclopedia of the History of Medicine, ed. William F. Bynum and Roy Porter (New York: Routledge, 1993), 537–561.
- 2.Pinell, Fight Against Cancer.
- 3.Patterson, Dread Disease.
- 4.On Britain, see Caroline Murphy, A History of Radiotherapy to 1950. Cancer and Radiotherapy in Britain 1850–1950 [PhD thesis] (Manchester, England: University of Manchester, 1986); Caroline Murphy, “From Friedenheim to Hospice: A Century of Cancer Hospitals,” in The Hospital in History, ed. Lindsay Granshaw and Roy Porter (New York: Routledge, 1989), 221–241; Paolo Palladino, “Speculations on Cancer-Free Babies: Surgery and Genetics at St Mark’s Hospital, 1924–1995,” in Heredity and Infection: The History of Disease Transmission, ed. Jean-Paul Gaudillière and Ilana Löwy (New York: Routledge, 2001), 285–310; David Cantor, “Cancer”; David Cantor, “The MRC’s Support for Experimental Radiology During the Inter-War Years,” in Historical Perspectives on the Role of the MRC: Essays in the History of the Medical Research Council of the United Kingdom and Its Predecessor, the Medical Research Committee, 1913–1953, ed. Joan Austoker and Linda Bryder (Oxford: Oxford University Press, 1989); Joan Austoker, A History of the Imperial Cancer Research Fund 1902–1896 (New York: Oxford University Press, 1988).
- 5.Williams William Roger, The Natural History of Cancer With Special Reference to Its Causation and Prevention (London: W. Heinemann, 1908), 58.
- 6.Walshe Walter Hayle, The Nature and Treatment of Cancer (London: Taylor and Walton, 1846), 152–153.
- 7.Ibid., 95.
- 8.Ibid., 94–95.
- 9.West Charles, Lectures on the Diseases of Women (London: John Churchill, 1858).
- 10.Moore Charles H., The Antecedents of Cancer (London: T. Richards, 1865); West, Lectures on the Diseases of Women.
- 11.Waller John C., “The Illusion of an Explanation: The Concept of Hereditary Disease, 1770–1870,” Journal of the History of Medicine and Allied Sciences 57 (2002): 410–448; Robert C. Olby, “Constitutional and Hereditary Disorders,” in Companion Encyclopedia of the History of Medicine, ed. William F. Bynum and Roy Porter (New York: Routledge, 1993), 412–437. [DOI] [PubMed] [Google Scholar]
- 12.Walshe, Nature and Treatment of Cancer, 168.
- 13.Copland James, Dictionary of Practical Medicine, vol. 1 (London: Longman, Brown, Green and Longmans, 1858), 285.
- 14.Walshe, Nature and Treatment of Cancer, 191–192.
- 15.Copland, Dictionary, 285.
- 16.Walshe, Nature and Treatment of Cancer, 192.
- 17.See, for example, West, Lectures on the Diseases of Women.
- 18.Quoted in Fleetwood Churchill, On the Diseases of Women; Including Those of Pregnancy and Childbed (Dublin: Fannin and Co, 1852), 327.
- 19.Walshe, Nature and Treatment of Cancer, 228; West, Lectures on the Diseases of Women, 395; Churchill, On the Diseases of Women, 329.
- 20.Jewson N. D., “The Disappearance of the Sick-Man From Medical Cosmology,” Sociology 10 (1976): 225–244. [Google Scholar]
- 21.Lawrence Christopher, “The History and Historiography of Surgery,” in Medical Theory, Surgical Practice, ed. Christopher Lawrence (New York: Routledge, 1992), 1–47.
- 22.De Morgan Campbell, “On the Origin of Cancer,” Lancet 2 (1871): 6–7, 41–42, 80–81, 118–119, 154–156, 165–166; Moore, Antecedents of Cancer; “Discussions in Scientific Medicine,” British Medical Journal 2 (1865): 165–166. [Google Scholar]
- 23.Waller, “Illusion of an Explanation.”
- 24.David Cantor makes this important point in “Cancer,” in Dictionnaire de la pensée médicale, ed. Dominique Lecourt, François Delaporte, Patrice Pinell, and Christine Sinding (Paris: Presses Universitaires de France, 2004).
- 25.The question of heredity was also a prominent issue in debates about the etiology of tuberculosis. See Olby, “Constitutional and Hereditary Disorders”; Michael Worboys, Spreading Germs: Disease Theories and Medical Practice in Britain, 1865–1900 (Cambridge: Cambridge University Press, 2000), 193–233.
- 26.Snow Herbert, Clinical Notes on Cancer: Its Etiology and Treatment With Special Reference to the Heredity-Fallacy, and to the Neurotic Origin of Most Cases of Alveolar Carcinoma (London: J. & A. Churchill, 1883), 22.
- 27.Dunn Percy H., “Theory of Cancerous Inheritance,” Lancet 1 (1886): 148–150, quotation from p. 148. [Google Scholar]
- 28.Bashford E. F., “Heredity in Cancer,” Lancet 2 (1908): 1508–1512, quotation from p. 1512. [Google Scholar]
- 29.Snow Herbert, “Heredity in Cancer [letter],” Lancet 1 (1898): 538.
- 30.Snow, Clinical Notes, 21; see also Dunn, “Theory of Cancerous Inheritance.”
- 31.Sinclair William Japp, “Malignant Diseases of the Uterus,” in A System of Gynaecology, ed. Thomas Clifford Allbutt and W. S. Playfair (London: Macmillan and Co, 1896), 643–743.
- 32.Ibid., 658.
- 33.Brand Alexander Theodore, “The Etiology of Cancer,” British Medical Journal 2 (1902): 238–42, quotation from p. 240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Snow Herbert, The Proclivity of Women to Cancerous Diseases (London: J. & A. Churchill, 1891).
- 35.Brand, “Etiology of Cancer,” 242; Charles Plumley Childe, The Control of a Scourge, Or How Cancer Is Curable (London: Methuen, 1906), 206.
- 36.Childe, Control of a Scourge, 225.
- 37.Smith Virginia Sarah, Cleanliness: The Development of Idea and Practice in Britain, 1770–1850 [PhD thesis] (London: London School of Economics, 1985).
- 38.Beverley M., “Twenty Cases of Emmet’s Operation for Laceration of Cervix Uteri,” British Medical Journal 1 (1887): 109–110; Frederick John Mc-Cann, The Treatment of Common Female Ailments (London: Edward Arnold, 1922), 42–43. By the end of the 20th century, the notion of prophylactic surgery had been extended to healthy, though potentially cancerous, organs such as the ovary, breast, and colon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.See, for example, Mort Frank, Dangerous Sexualities: Medico-Moral Politics in England Since 1830 (New York: Routledge and Kegan Paul, 1987).
- 40.Darby Robert, “ ‘Where Doctors Differ’: The Debate on Circumcision as a Protection Against Syphilis,” Social History of Medicine 16 (2003): 57–78; David L. Gollaher, “From Ritual to Science: The Medical Transformation of Circumcision in America,” Journal of Social History 28 (1994): 5–36. [DOI] [PubMed]
- 41.Quoted in Darby, “Where Doctors Differ,” 64.
- 42.On the development of gynecological surgery, see Moscucci Ornella, The Science of Woman: Gynaecology and Gender in England, 1800–1929 (Cambridge: Cambridge University Press, 1990). The question of radical surgery is examined by Gert H. Brieger, “From Conservative to Radical Surgery in Late Nineteenth-Century America,” in Medical Theory, Surgical Practice: Studies in the History of Surgery, ed. Christopher Lawrence (New York: Routledge, 1995), 216–231.
- 43.French R. D., Antivivisection and Medical Science in Victorian Society (Princeton, NJ: Princeton University Press, 1975). On the feminist opposition to gynecological surgery, see Moscucci, Science of Woman, 158–160.
- 44.See, for example, Spencer Herbert, “A Discussion of the Measures to Be Recommended to Secure the Earlier Recognition of Uterine Cancer,” British Medical Journal 2 (1907): 431–440. [Google Scholar]
- 45.Childe, Control of a Scourge, 67.
- 46.See, for example, Soloway Richard A., Demography and Degeneration: Eugenics and the Declining Birthrate in Twentieth-Century Britain (Chapel Hill: University of North Carolina Press, 1990); Jane Lewis, The Politics of Motherhood: Child and Maternal Welfare in England (London: Croom Helm, 1980); Dorothy Porter, Health, Civilization and the State: A History of Public Health From Ancient to Modern Times (New York: Routledge, 1999), 173–190.
- 47.Some health officials claimed that the rise was because of better diagnosis. See Newsholme Arthur, “The Statistics of Cancer,” The PractitionerNS 9 (1899): 371–384. [Google Scholar]
- 48.For an illuminating discussion of the relationship between empire and chronic disease, see David Cantor, “Cortisone and the Politics of Empire: Imperialism and British Medicine, 1918–1955,” Bulletin of the History of Medicine 67 (1993): 463–493. [PubMed] [Google Scholar]
- 49.See, for example, “A Biological View of the Cancer Cell [leading article],” British Medical Journal 2 (1911): 1494–1495. [Google Scholar]
- 50.“Cancer Curers,” The PractitionerNS 9 (1899): 518–523. [Google Scholar]
- 51.See Austoker, History of the Imperial Cancer Research Fund; Frank K. Prochaska, Philanthropy and the Hospitals of London: The King’s Fund 1897–1990 (Oxford: Clarendon Press, 1992), 116–117; and the biographies of Julius Wernher, Alfred Beit, and Ernest Cassel in the Oxford Dictionary of National Biography (Oxford: Oxford University Press, 2004).
- 52.Spencer, “Discussion of the Measures,” 431.
- 53.Snow, Clinical Notes, 50.
- 54.Sinclair William Japp, “Carcinoma in Women, Chiefly in Its Clinical Aspects,” British Medical Journal 2 (1902): 321–327, quotation from p. 327. [Google Scholar]
- 55.Sinclair, “Malignant Diseases,” 559–560. On the sexual politics of gonorrhoea, see Michael Worboys, “Unsexing Gonorrhoea: Bacteriologists, Gynaecologists, and Suffragists in Britain, 1860–1920,” Social History of Medicine 17 (2004): 41–59. [Google Scholar]
- 56.Sinclair, “Malignant Diseases,” 661.
- 57.Sinclair, “Carcinoma in Women,” 326.
- 58.Ibid.
- 59.Spencer, “Discussion of the Measures,” 432.
- 60.Not all doctors agreed with this message, however. Some feared that it might induce unrealistic expectations of cure. See “The Public Appreciation of the Dangers and Treatment of Cancer [leading article],” Lancet 1 (1905): 39–40. For a critique of the “delay” message, see Robert A. Aronowitz, “Do not Delay: Breast Cancer and Time, 1900–1970,” Milbank Quarterly 79 (2001): 355–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.“War Against Cancer [leading article],” British Medical Journal 1 (1904): 1448. [Google Scholar]
- 62.See, for example, Childe Charles Plumley, “Cancer, Public Authorities, and the Public,” British Medical Journal 1 (1914): 643–645; “The Need for Public Education in the Control of Cancer [leading article],” British Medical Journal 1 (1923): 509–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Holden Oscar M., “The Present Position With Respect to Cancer,” Public Health 36 (1922): 248–253, quotation from p. 253. [Google Scholar]
- 64.“The Early Recognition of Uterine Cancer,” British Medical Journal 1 (1909): 1408–1410. [Google Scholar]
- 65.Childe, “Cancer, Public Authorities, and the Public,” 645. [DOI] [PMC free article] [PubMed]
- 66.Figures drawn from data published in Holden, “Present Position,” 251.
- 67.Reagan Leslie J., “Engendering the Dread Disease: Women, Men, and Cancer,” American Journal of Public Health 87 (1997): 1779–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.See, for example, Lerner, Breast Cancer Wars, 241–250.


