Abstract
Dental caries is a potentially preventable infectious disease that, untreated, can cause significant morbidity requiring costly treatment. The Access to Baby and Child Dentistry (ABCD) program increases access to prevention and early treatment for Medicaid-eligible children aged younger than 6 years in Washington State.
The program is a partnership of Washington Dental Service Foundation, the University of Washington School of Pediatric Dentistry, the state Medical Assistance Administration, and local stakeholders. Through training in pediatric dental techniques and enhanced reimbursement, ABCD equips and encourages dentists to serve young Medicaid patients. Family counseling increases oral care compliance and reduces no-show rates. Program evaluation demonstrates changing attitudes and behavior among participating families and dentists, with more young, low-income Washington children receiving oral health care.
DENTAL CARIES IS THE SINGLE most common chronic childhood disease—5 times more common than asthma and 7 times more common than hay fever.1 In Washington State, dental decay rates for 1- and 2-year-olds are substantially higher than national rates.2(p5) Children from low-income families are at higher risk for oral disease and often have difficulty accessing dental care.2(p6) More than 230000 Washington State children younger than 6 years old were enrolled in Medicaid during 1997, but fewer than 1 in 4 actually saw a dentist.3
The Access to Baby and Child Dentistry (ABCD) program was initiated to address the high incidence of oral disease and limited access to dental services among young, Medicaid-eligible children in Washington State. The goals are to increase access to prevention and early treatment for these children and thereby improve their lifelong oral health. ABCD, which began in Spokane County in 1995, is a statewide partnership of health districts, local dental societies, community health advocates, the University of Washington School of Pediatric Dentistry, the state Medicaid program, and the Washington Dental Service Foundation (WDSF).
Private dental practices provide services to Medicaid-enrolled children younger than age 6; local health jurisdictions identify and enroll families. Dentists are trained in early childhood dental techniques and paid enhanced reimbursement rates by the state Medicaid administration, respectively mitigating providers’ hesitance to treat young children and the financial disincentive to participation. Dental offices receive sensitivity training and often have multilingual staff and materials available to reduce cultural barriers. Services provided in a typical ABCD visit include a periodic oral examination and family oral health education, along with fluoride varnish application and restorative procedures if warranted. Client families are provided counseling aimed at reducing the number of no-shows, increasing home care compliance, and promoting prevention (e.g., by encouraging children’s first dental visit before their first birthday or with the eruption of their first tooth).
Highly conducive to replication, ABCD now operates in 20 Washington counties. Programs in each county differ as they are adapted to local communities, but key implementation elements and stakeholder roles are common to all and include the following:
A state Medicaid program willing to (1) support this cost-effective program, including establishment of an enhanced Medicaid fee schedule to attract participating dentists, and (2) contract with a local government agency to collect federal administrative matching funds for program operation.
Pediatric dentists (usually from a dental school) willing to develop and deliver training in nontraumatic, early pediatric techniques, as well as to offer certification and peer consultation.
A local health district or nonprofit organization for administering the program on a daily basis, including client outreach, case management, and program promotion (government agencies are eligible for federal matching funds).
A local dental society to encourage its members to become ABCD providers.
An oversight task force, composed of key stakeholders, for strategic planning and general guidance.
KEY FINDINGS.
Working together, public and private stakeholders can improve access to oral health care for low-income children.
Multiple interventions (pediatric training, enhanced reimbursement, client coaching) for health care providers encourage greater involvement in oral health promotion and decay prevention, and expand the number of providers willing to treat young children and low-income patients.
Multiple interventions for patients/clients (greater access, case management, oral health instruction) can diminish economic and cultural barriers to care while empowering parents to care for their children’s oral health.
Multifaceted program assessment has shown that more economically disadvantaged children are seeing oral health care providers at an earlier age, and parents understand that good oral health is essential to good overall health.
SUSTAINABILITY
WDSF helped to establish ABCD programs across Washington State by providing 3-year start-up grants and technical assistance. As programs have moved into their fourth year, program administrators have leveraged community ownership to find alternate revenue sources sufficient to sustain their operations when the WDSF funding cycle has been completed. Revenue sources have included the following: local government or health district funding; federal and state grants; Medicaid reimbursement for certain services (oral health education, fluoride varnish application); social events and fund-raising activities (golf tournaments, auctions, dinners). Area dentists donate their time, money, and services. Local governments, schools, and social service organizations (i.e., Head Start; Special Supplemental Nutrition Program for Women, Infants, and Children [WIC]; Healthy Mothers/Healthy Babies; United Way) assist with outreach and client referral. Local businesses and civic groups assist with fund-raising and provide financial support.
EVALUATION
WDSF has evaluated ABCD over the past several years by using a multifaceted approach. This process has entailed analyzing Medicaid data and individual site statistics, surveying client families and providers, and soliciting feedback from participants. Outcome measures have included (1) Medicaid dental service use (clients aged younger than 6 years), (2) the number of dentists serving young Medicaid clients, and (3) clients’ and dentists’ attitude changes. The results demonstrate improvement in access rates, especially for the youngest children, and attitude changes by families and dentists.
Medicaid Data
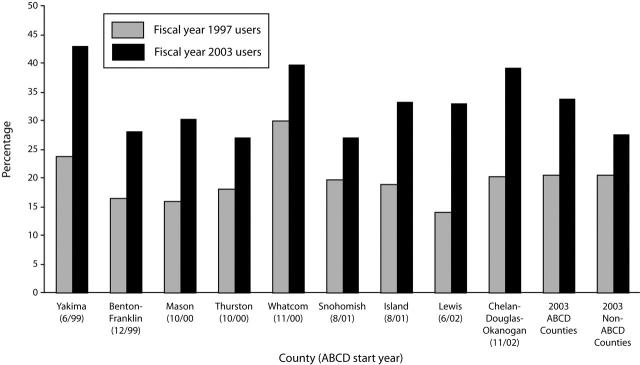
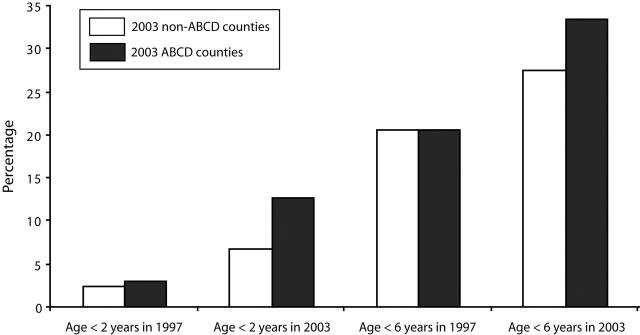
State Medicaid data suggest a correlation between program initiation and increased use of Medicaid-reimbursed dental services. In counties where ABCD began between 1999 and 2002, use of Medicaid-reimbursed dental services by children aged younger than 6 years was the same as that of non-ABCD counties in 1997 (20.6%); by 2003, however, Medicaid use in ABCD counties was 33.6%, compared with 27.6% in non-ABCD counties. In these same ABCD counties, use of Medicaid dental services has risen an average of 39% since the program’s inception for children aged younger than 6 years (97% for children aged younger than 2 years) (Figures 1 ▶ and 2 ▶).
FIGURE 1—
Percentage of Medicaid enrollees in ABCD and non-ABCD counties aged younger than 6 years who received dental services: Washington State, fiscal years 1997 and 2003.
Note. ABCD = Access to Baby and Child Dentistry. Month in which each county began the ABCD program is given in parentheses.
FIGURE 2—
Use of Medicaid dental services in ABCD and non-ABCD counties among children aged younger than 2 years and younger than 6 years: Washington State, fiscal years 1997 and 2003.
Note. ABCD = Access to Baby and Child Dentistry. All ABCD programs represented in the figure were begun between 1999 and 2002.
Individual Site Statistics
Statewide ABCD enrollment has grown to over 32000 children. Current ABCD participants represent roughly 15% of all Washington State Medicaid-enrolled children aged younger than 6 years. Approximately 55% of enrolled children have had at least 1 dental visit (weighted average across programs; range= 43%–92%); the percentage generally depends on how aggressively each program pursues out-reach. Provider participation has been steady, with more than 330 participating dentists statewide.
Surveys
Pre- and postimplementation surveys were conducted on a sample of enrolled clients and providers (baseline in 2000, follow-up in 2003). Client respondents represent a convenience sample of parents of Medicaid-enrolled children who opted for their children to enroll in ABCD. The percentage of surveyed ABCD parents who indicated that their children had seen a dentist at least once a year increased from 36% to 94% between the baseline survey and follow-up. The percentage of parents who rated their children’s oral health as “excellent” in 2003 was nearly twice as high as in 2000 (49% vs 25%). Parents sought care for their children at an earlier age; in the 2003 survey, 48% reported that their child’s first dental visit occurred before age 2, compared with 23% in 2000. Nearly 80% of ABCD dentists rated their experiences with the program as “excellent” or “good,” and they were more likely than non-ABCD dentists to emphasize their willingness to treat young Medicaid-insured patients.
Access to Baby and Child Dentistry program logo.
Anecdotal Feedback
Client families provide feedback to program staff. Each program’s oversight task force also monitors quality through client feedback. Coordinators from individual programs across the state meet quarterly to identify and address problems.
DISCUSSION AND NEXT STEPS
Public and private stakeholders, collaborating on behalf of children’s oral health, can make a measurable improvement in both access to oral health services and quantifiable oral health indicators. Foundations can provide start-up funding, bring partners together, provide technical assistance to improve success, measure results, and assist in disseminating promising practices. From the beginning, ABCD has emphasized partnership, multiple interventions, and outcomes assessment. Demonstrating measurable achievement is one method used to stimulate interest in other counties considering an ABCD program.
With these promising results, ABCD will continue to build on the successful foundation it has established over the past decade. Continuing goals for the program include (1) achieving statewide coverage by establishing new (and strengthening existing) partnerships in counties and health agencies where ABCD does not exist, (2) preserving and augmenting realized gains through ongoing assessment of dental care use by young Medicaid enrollees, and (3) expanding opportunities to engage physicians and other nondental health care providers in improving children’s oral health.
Figure 3.
Acknowledgments
We thank the following for their support of ABCD programs in Washington State: ABCD program staff throughout the state; Washington Department of Social and Health Services staff; the University of Washington School of Dentistry; and Dianne Riter Hill and Kathy O’Meara-Wyman, program officers for the Washington Dental Service Foundation.
Peer Reviewed
Contributors G. J. Donahue performed data analysis and cowrote the first and final drafts of the article with N. Waddell. A. L. Plough, M. A. del Aguila, and T. E. Garland conceptualized the article and edited various versions.
References
- 1.Oral Health in America: A Report of the Surgeon General. Rockville, Md: US Dept of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research; 2000:2.
- 2.Smile Survey 2000. Olympia: Washington State Dept of Health; 2001.
- 3.Washington State Medical Assistance Administration. Dental Clients by Client Age, Ages 18 and Under Only, Fiscal Years 1996–2003. Olympia: Washington State Dept of Social and Health Services; January 30, 2004.