Abstract
Cigarette smoking is the leading cause of preventable death in the United States. The health risks of smoking are well documented, as is the effectiveness of clinical and public health interventions to prevent and reduce smoking. However, many myths about smoking either encourage people to begin or continue smoking or deter them from quitting.
Some myths stem from a misapplied understanding of what might seem to be common sense; others are deliberately promulgated by the tobacco industry to induce people—especially children—to start smoking and to keep them smoking as adults. These myths undermine tobacco control. However, comprehensive tobacco control programs that include anti-smoking public education campaigns can effectively counter these myths and prevent illness and premature death.
CIGARETTE SMOKING IS THE leading cause of preventable death in the United States. It causes serious illness among an estimated 8.6 million persons, it costs $167 billion in annual health-related losses, and it kills approximately 438 000 people each year.1,2 Worldwide, smoking kills nearly 5 million people annually. If current trends continue, this number will double by 2030, and smoking will kill more than 1 billion people during this century.3,4
Although smoking prevalence is deceasing slowly in the United States and in some parts of the world,4,5 it is increasing sharply in other regions and among certain populations, especially in developing countries and among women.4 This is despite the fact that the health risks of smoking have been suspected and publicized since shortly after tobacco was first introduced to Europe 400 years ago,6 and these risks have been scientifically proven for at least the last half century.7
Many myths about smoking have arisen—myths that encourage people to begin or continue smoking or that deter them from quitting. These myths are believed true not only by many smokers but also by some physicians and policy makers, a fact that hinders development of effective tobacco control policy and treatment for individuals who are dependent on tobacco. This commentary reviews and rebuts 12 of the most common myths.
MYTH #1: PEOPLE HAVE FREE CHOICE WHETHER OR NOT TO SMOKE
We all like to think we are creatures of complete free will. However, free will in the case of tobacco is subverted by advertising and addiction. In 2002, the tobacco industry spent $12.5 billion in the United States on advertising, marketing, and promotion—more than double the amount spent in 1997, and 18 times the amount spent on tobacco control.8 Advertising and marketing encourage people to smoke, particularly when they are targeted at youth and other demographic subgroups.9–22
Cigarettes deliver an addictive drug—nicotine—to the body. The tobacco industry has shown its awareness of this fact by referring to cigarettes as a “nicotine delivery device” and by acknowledging that it is the nicotine in cigarettes that makes people want to smoke.23
Children are below the age of legal consent and are not legally competent to make most decisions, including the decision about whether or not to smoke. Starting to smoke during early adolescence is associated with higher daily cigarette consumption and a lower probability of quitting as an adult.24 More than 80% of all regular smokers began smoking by the time they were 18 years old.25
Most smokers want to quit.26 However, the tobacco industry ensures that there is enough nicotine in every cigarette to keep people addicted, and production methods and chemical additives may increase nicotine content.27,28
MYTH #2: EVERYONE KNOWS HOW BAD SMOKING IS
While most people are generally aware that smoking is not healthy, instances of poor knowledge about the health risks abound. Relatively few women are aware of gender-specific health risks, including cervical cancer, osteoporosis, early menopause, miscarriage, ectopic pregnancy, and infertility.29 Fewer than half of Canadian adults aged 55 to 74 years identified smoking as a major cause of heart disease.30
In China, where more than 90% of smokers are men, fewer than 1 in 4 smokers believes smoking causes serious health problems.31 This lack of knowledge may be why smoking prevalence among Chinese immigrant men in New York City is higher than among the population as a whole. Chinese-born men who have low levels of knowledge about the harmful effects of smoking are twice as likely to smoke than those who have higher levels of knowledge.32 Knowledge may even be decreasing among some groups: one survey showed that rural smokers who were surveyed in 1997 and 1998 ascribed more positive characteristics and fewer health risks to smoking than they did during the previous decade.33
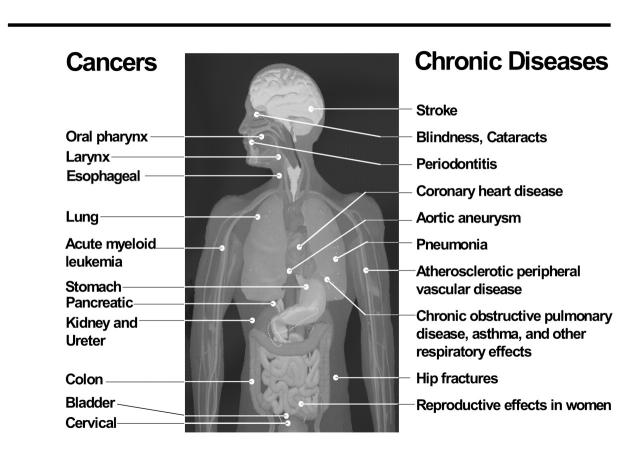
It is becoming clear that cigarettes cause disease in nearly every organ of the body (Figure 1 ▶). In addition to lung cancer, heart disease, stroke, and emphysema, smoking has been definitively linked to other cancers (colon, cervical, kidney, pancreatic, bladder, esophageal, larynx, oral cavity and pharynx, and stomach) and acute myeloid leukemia; cardiovascular disease (atherosclerosis and abdominal aortic aneurysm); respiratory disease (impaired lung function, chronic obstructive pulmonary disease, asthma, and pneumonia); other diseases (cataracts, periodontitis, hip fractures, and peptic ulcers); general diminished health status and increased morbidity (including increased work absenteeism, increased use of medical care services, and increased risk for adverse surgical outcomes); and, among women, low bone density and osteoporosis, pregnancy complications (including low-birthweight babies, preterm delivery, fetal death, stillbirths, reduced lung function in infants, and sudden infant death syndrome), and reduced fertility.34
FIGURE 1—
Diseases caused by smoking.
MYTH #3: JUST A FEW CIGARETTES A DAY CAN’T HURT
Although lung cancer has, in general, a linear dose-response relationship with tobacco use,35 the risk for cardiovascular disease, which accounts for a significant proportion of tobacco-related illness and death, becomes evident with the consumption of 3 to 5 cigarettes a day.36 Risk for acute myocardial infarction and coronary heart disease associated with exposure to tobacco smoke appears to be nonlinear at low doses and increases rapidly with relatively small doses, such as those received from environmental tobacco smoke or from smoking just a few cigarettes a day. Even small exposures increase platelet aggregation and induce arterial and hemodynamic changes.37 Pregnant women who smoke as few as 5 cigarettes a day are more likely to have low-birthweight babies.38
Cancer is the leading cause of death among smokers in the United States, with lung cancer responsible for nearly 80% of tobacco-related deaths.1 However, cardiovascular disease (all forms combined) is the leading cause of all tobacco-related mortality, including both smokers and those exposed to environmental tobacco smoke.1 Cardiovascular disease is second only to respiratory disease (i.e., chronic bronchitis and emphysema) as the leading cause of tobacco-related morbidity.2 Cardiovascular disease may be caused by exposure to carbon monoxide and other combustion products,39,40 which suggests that any “reduced risk” tobacco product that is ignited and inhaled is unlikely to significantly decrease tobacco-related illness and death from cardiovascular causes.
MYTH #4: “LIGHT” CIGARETTES ARE LESS HARMFUL
So-called “light” cigarettes are just as harmful to health as “regular” brands, but most smokers remain sadly misinformed about this fact41: 60% percent of smokers believe the terms light and ultra-light refer to low-tar/low-nicotine cigarettes.42 However, there is no standard definition of what constitutes a light or ultra-light brand,43 and tobacco companies admit that these terms refer to the perceived taste and flavor of cigarettes, not their content.44 More than 160 countries have signed the World Health Organization’s Framework Convention on Tobacco Control, which prohibits the use of descriptors that may create the false impression that a particular tobacco product is less harmful than other tobacco products.45
Fewer than 10% of smokers are aware that 1 light or ultra-light cigarette provides the same amount of tar as 1 regular cigarette, and many of these smokers say that they would be likely to quit if they learned that 1 light or ultra-light cigarette is equivalent to 1 regular cigarette.46 However, while smokers of low-tar brands are more likely to attempt to quit, they are less likely to actually quit.47
Despite decades of the tobacco industry marketing light cigarettes that are purported to have lower tar and nicotine content,48 there is no meaningful difference in smoke exposure or health risks among cigarettes with different tar and nicotine yields.49 Light cigarettes deliver the same amounts of tar, nicotine, and carbon monoxide to smokers as standard brands, partly because testing machines do not burn cigarettes the same way cigarettes burn when actually smoked by a person.27
Many low-tar, light, or ultra-light cigarette smokers unconsciously compensate for these artificially reduced machine-measured tar and nicotine levels by smoking more cigarettes, by inhaling smoke harder and deeper into the lungs, and by blocking filter ventilation holes to increase the concentration of inhaled smoke.27,50 The tobacco industry has been aware of this compensation by smokers for at least the last 3 decades.51
MYTH #5: IT’S EASY TO STOP SMOKING; IF PEOPLE WANT TO QUIT, THEY WILL
While many smokers are able to stop on their own, many find it difficult or impossible to quit because nicotine is addictive.52 Even doctors find quitting hard; only half the doctors who smoked and who suffered a heart attack were able to quit.53 The tobacco industry has admitted privately that tobacco has an addictive potential similar to opium.54 Nicotine may be comparable to heroin, cocaine, and alcohol in addiction potential.55
The benefits of quitting smoking are well documented, and many people who are serious about quitting make several attempts before they quit for good.56 Most smokers want to quit and make at least 1 quit attempt each year.57 Of these, the majority attempt to stop smoking without counseling or medication,58 but only 7% of the people who try to quit without assistance succeed in stopping for 1 year or longer.59
MYTH #6: CESSATION MEDICATIONS DON’T WORK
Smoking cessation medications, including nicotine replacement therapies (NRT)—patch, gum, nasal spray, and lozenge—and bupropion, can double the likelihood that a person will successfully quit.59–62 For some smokers, combination therapies—e.g., multiple types of NRT, NRT with bupropion, NRT with counseling, and NRT with bupropion and counseling—may be even more effective than using a single cessation method.63,64 Retreatment after an initial failed course of cessation treatment also increases quit rates,65 and combination therapies are especially useful among relapsed smokers.59
MYTH #7: ONCE A SMOKER, ALWAYS A SMOKER
More than half the Americans who have ever smoked have already quit.5 Despite the difficulty many people have quitting smoking, the millions of former smokers are living proof that people can quit—and in many places, most smokers already have.
MYTH #8: SMOKERS MAY DIE EARLIER, BUT ALL THEY LOSE ARE A COUPLE OF BAD YEARS AT THE END OF LIFE
The average smoker who dies from tobacco-related causes loses about 14 years of life.66 Among nonsmokers, 95% of that additional time will be spent without disability.67 Not smoking extends life, including disability-free life, and compresses disability into a shorter period of time.68 Elderly smokers have the physical health expected of people 2 to 4 years older and the mental health expected of people 10 years older than their actual age.69 Smoking increases the risk that an older person will lose his or her independence, and it reduces the chance of regaining autonomy.67 It is never too late to quit—even people who quit after decades of smoking improve their health and their life expectancy.70
MYTH #9: ENVIRONMENTAL TOBACCO SMOKE MAY BE A NUISANCE, BUT IT ISN’T DEADLY
Exposure to environmental tobacco smoke causes illness and death.71–76 The circulatory system of a nonsmoker behaves similarly to that of a smoker after just 30 minutes of exposure to environmental tobacco smoke, which increases the risk of ischemic heart disease.74 Environmental tobacco smoke also is associated with a 25% higher risk for chronic respiratory disease, a 40% to 60% higher risk for developing asthma among adults, a 50% to 100% higher risk for acute respiratory illness among children,77–79 and a doubling of the risk for sudden infant death syndrome.80
MYTH #10: TOBACCO IS GOOD FOR THE ECONOMY
The tobacco industry, which has an incentive to portray itself as indispensable to the economy, argues that tobacco creates employment, raises tax revenues, and contributes to the national gross domestic product. However, the long-term societal costs of tobacco use far outweigh any economic benefits.
The World Bank analyzed the net economic effect of tobacco and concluded that money not spent on cigarettes would instead be spent on other goods and services that in turn would generate other jobs and economic activity to replace any that would be lost from the tobacco industry.81 In the United States, completely eliminating tobacco from the economy would result in an estimated net increase of more than 130 000 jobs nationwide.82
In the United States, smoking causes annual economic losses of $167 billion per year (about $3650 per smoker), including health care expenses and productivity losses caused by premature death.1,5 These costs are borne by individuals and by society as a whole, and they are more than twice the $81 billion (including taxes and manufacturing and marketing costs) that US smokers spend annually on tobacco.83
The science behind smoking cessation treatment is strong, and its cost-effectiveness compares favorably with many other medical interventions.84 Businesses and health insurers have financial incentives to support cessation programs for employees: nonsmokers are more productive and miss less work than smokers do,85 and tobacco cessation coverage is one of the most cost-effective health insurance benefits an employer can provide.86
MYTH #11: WE’VE ALREADY SOLVED THE TOBACCO PROBLEM
The public health problems caused by tobacco use are far from solved. Despite declining smoking prevalence in the United States, more than 1 in 5 US adults (nearly 50 million people) smoke, and the decline of smoking among both adults and youths has slowed or stalled in recent years.5,87 Globally, about 1.3 billion people are smokers—more than at any time in human history—and more than 1 billion will die from tobacco-related causes during this century unless urgent action is taken on the local, national, and international levels.4
Although there are many other important health issues that also demand attention, one of the most critical concepts of tobacco control is that we have proven interventions. Higher taxes, expansion of smoke-free environments, increased use of cessation treatments, and public education have all been proven to decrease tobacco use.88 We cannot afford to enter into a debate as to which health problems are more important than others—all are important, and all are worthy of attention and evidence-based interventions.
MYTH #12: THE TOBACCO INDUSTRY NO LONGER MARKETS TO KIDS OR UNDERMINES PUBLIC HEALTH EFFORTS
This is perhaps the most dangerous myth about tobacco. Despite the tobacco industry’s pledge to curtail many of its activities as part of the 1998 Master Settlement Agreement (MSA),89 cigarette advertising and marketing continues to reach children and tobacco companies continue to fight public health efforts.90 For decades, the tobacco industry has employed lawyers, public relations experts, and scientists to divert attention from global public health issues, distort scientific studies, interfere with politics, and reduce budgets for scientific and policy activities.91–93 More recently, tobacco companies have filed lawsuits to stop public health advertising campaigns that they claim are “anti-industry.”94
Tobacco industry market leaders have recently been pressured to adopt corporate social-responsibility programs to account for and redress the tobacco industry’s adverse impact on society. However, the tobacco business—with its fiduciary responsibility to preserve and increase tobacco profits—is inherently socially irresponsible. For example, Philip Morris executives privately admit that the purposes of these programs are to protect the company’s reputation, enhance shareholder value, and defend the right of adults to smoke, and that the programs do not indicate any significant change in the way Philip Morris does business.95
Cigarette advertising continues to reach children.87,96 For example, magazine ads for each of the 3 most popular brands among youths reached more than 80% of young people in the United States an average of 17 times in 2000.97 Children who own tobacco company promotional items (T-shirts, caps, etc.) are up to 7 times more likely to smoke than those who do not own these items.98
Children aged 12 to 17 years—the most likely age of smoking initiation—are twice as likely as adults to be exposed to tobacco advertising,99 and teenagers are 3 times more sensitive to cigarette advertising than adults are.100 Depictions of smoking in movies also increases smoking among teens. Those who see movies that depict smoking are 3 times more likely to smoke than teens who do not see smoking in movies, and half of all smoking experimentation among teens has been attributed to this exposure.101 There is more smoking in movies now than at any time since 1950,102 and use of a specific cigarette brand imparts greater appeal to the brand.103 Endorsement of cigarette brands—the use of specific brands by stars in movies—has increased 11-fold since implementation of the MSA.103 Stars who smoke onscreen strongly influence smoking behaviors among teens, and the greater the level of smoking depicted, the higher the likelihood that teens will become smokers.104 Depictions of smoking in music videos, on television, and in other media also influence the smoking behaviors of teens.105,106
Tobacco industry promotion of smoking even undermines the ability of parenting to prevent adolescents from starting to smoke—which contradicts the tobacco industry’s contention that parenting practices, and not their marketing activities, are critical determinants of smoking among youths.107
CONCLUSIONS
Many of the myths that surround smoking are the result of a misapplied understanding of what might seem to be common sense. Others are deliberately promulgated by the tobacco industry to induce people—especially children—to start smoking and to keep them smoking as adults. These myths are believed to be true not only by many smokers but also by some physicians and policy makers. All of these myths are false, and each myth undermines effective tobacco control policy and smoking cessation efforts by individuals. Yet, the means to counter these myths are available, and more effective employment of these means will help prevent illness and premature death.
Antismoking public education campaigns work, especially when they are implemented across multiple media settings and in conjunction with comprehensive tobacco control programs that include increased taxation, smoke-free workplace legislation, and cessation programs.88,108–114 While government and public health agencies must take the lead, the health care system, businesses, insurers, communities, and individuals all have important roles to play in tobacco control. We must continue to find innovative ways to both communicate the facts and counter the various myths, half-truths, and lies that encourage people to start smoking and reduce their odds of quitting.
Acknowledgments
There was no funding for this paper other than that provided by the New York City Department of Health and Mental Hygiene.
The authors thank Dr Kelly Henning for valuable suggestions and insight.
Peer Reviewed
References
- 1.Annual smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 1997–2001. MMWR Morb Mortal Wkly Rep. 2005;54:625–628. [PubMed] [Google Scholar]
- 2.Cigarette smoking-attributable morbidity—United States, 2000. MMWR Morb Mortal Wkly Rep. 2003; 52:842–844. [PubMed] [Google Scholar]
- 3.Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362: 847–852. [DOI] [PubMed] [Google Scholar]
- 4.Mackay J, Eriksen M. The Tobacco Atlas. Geneva, Switzerland: World Health Organization; 2002.
- 5.Cigarette smoking among adults—United States, 2002. MMWR Morb Mortal Wkly Rep. 2004;53:427–431. [PubMed] [Google Scholar]
- 6.Charlton A. Tobacco or health 1602: an Elizabethan doctor speaks. Health Educ Res. 2005;20:101–111. [DOI] [PubMed] [Google Scholar]
- 7.Doll R, Hill AB. The mortality of doctors in relation to their smoking habits: a preliminary report. BMJ. 1954;ii: 1451–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Federal Trade Commission Cigarette Report for 2002. Washington, DC: Federal Trade Commission; 2004.
- 9.Basil MD, Basil DZ, Schooler C. Cigarette advertising to counter New Year’s resolutions. J Health Commun. 2000;5:161–174. [DOI] [PubMed] [Google Scholar]
- 10.Shafey O, Fernandez E, Thun M, et al. Cigarette advertising and female smoking prevalence in Spain, 1982–1997: case studies in International Tobacco Surveillance. Cancer. 2004;100: 1744–1749. [DOI] [PubMed] [Google Scholar]
- 11.O’Keefe AM, Pollay RW. Deadly targeting of women in promoting cigarettes. J Am Med Womens Assoc. 1996; 51:67–69. [PubMed] [Google Scholar]
- 12.Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. Am J Public Health. 2002; 92:908–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz SK, Lavack AM. Tobacco-related bar promotions: insights from tobacco industry documents. Tob Control. 2002;11(suppl 1) 1:I92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardiner PS. The African Americanization of menthol cigarette use in the United States. Nicotine Tob Res. 2004;6(suppl 1):S55–S65. [DOI] [PubMed] [Google Scholar]
- 15.Stevens P, Carlson LM, Hinman JM. An analysis of tobacco industry marketing to lesbian, gay, bisexual, and transgender (LGBT) populations: strategies for mainstream tobacco control and prevention. Health Promot Pract. 2004; 5(suppl 1):129–134. [DOI] [PubMed] [Google Scholar]
- 16.Pierce JP, Gilpin EA. A historical analysis of tobacco marketing and the uptake of smoking by youth in the United States: 1890–1977. Health Psychol. 1995;14:500–508. [DOI] [PubMed] [Google Scholar]
- 17.Pierce JP, Gilpin E, Burns DM, et al. Does tobacco advertising target young people to start smoking? Evidence from California. JAMA. 1991; 266:3154–3158. [PubMed] [Google Scholar]
- 18.Evans N, Farkas A, Gilpin E, et al. Influence of tobacco marketing and exposure to smokers on adolescent susceptibility to smoking. J Natl Cancer Inst. 1995;87:1538–1545. [DOI] [PubMed] [Google Scholar]
- 19.While D, Kelly S, Huang W, et al. Cigarette advertising and onset of smoking in children: questionnaire survey. BMJ. 1996;313:398–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pierce JP, Choi WS, Gilpin EA, et al. Tobacco industry promotion of cigarettes and adolescent smoking. [Erratum published in JAMA.1998;280:422]. JAMA. 1998;279:511–515. [DOI] [PubMed] [Google Scholar]
- 21.MacFadyen L, Hastings G, MacKintosh AM. Cross-sectional study of young people’s awareness of and involvement with tobacco marketing. BMJ. 2001;322:513–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donovan RJ, Jancey J, Jones S. Tobacco point-of-sale advertising increases positive brand user imagery. Tob Control. 2002;11:191–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reuter B. Table: competitive analysis 1st draft, organization 1st draft, production to follow. 1992 (est.). Bates: 2021118664–2021118680. Available at: http://tobaccodocuments.org/pm/2021118664-8680.html. Accessed April 5, 2005.
- 24.Chen J, Millar WJ. Age of smoking initiation: implications for quitting. Health Rep. 1998;9:39–46. [PubMed] [Google Scholar]
- 25.Preventing tobacco use among young people: a report of the Surgeon General. Atlanta, Ga: US Dept of Health and Human Services; 1994.
- 26.Cigarette smoking among adults—United States, 2000. MMWR Morb Mortal Wkly Rep. 2002;51:642–645. [PubMed] [Google Scholar]
- 27.Risks associated with smoking cigarettes with low machine-measured yields of tar and nicotine. Bethesda, Md: National Cancer Institute; 2001.
- 28.Armitage AK, Dixon M, Frost BE, et al. The effect of tobacco blend additives on the retention of nicotine and solanesol in the human respiratory tract and on subsequent plasma nicotine concentrations during cigarette smoking. Chem Res Toxicol. 2004;17:537–544. [DOI] [PubMed] [Google Scholar]
- 29.Roth LK, Taylor HS. Risks of smoking to reproductive health: assessment of women’s knowledge. Am J Obstet Gynecol. 2001;184:934–939. [DOI] [PubMed] [Google Scholar]
- 30.Kirkland SA, MacLean DR, Langille DB, et al. Knowledge and awareness of risk factors for cardiovascular disease among Canadians 55 to 74 years of age: results from the Canadian Heart Health Surveys, 1986–1992. CMAJ. 1999;161(suppl 8):S10–S16. [PMC free article] [PubMed] [Google Scholar]
- 31.Yang G, Ma J, Chen A, et al. Smoking cessation in China: findings from the 1996 national prevalence survey. Tob Control. 2001;10:170–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shelley D, Fahs M, Scheinmann R, Swain S, Qu J, Burton D. Acculturation and tobacco use among Chinese Americans. Am J Public Health. 2004;94: 300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frank E, Denniston M, Pederson L. Declines in smokers’ understanding of tobacco’s hazards between 1986 and 1998: a report from north Georgia. South Med J. 2002;95:675–680. [PubMed] [Google Scholar]
- 34.The health consequences of smoking: a report of the Surgeon General. Washington, DC: US Dept of Health and Human Services; 2004.
- 35.Law MR, Morris JK, Watt HC, Wald NJ. The dose-response relationship between cigarette consumption, biochemical markers and risk of lung cancer. Br J Cancer. 1997;75: 1690–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prescott E, Scharling H, Osler M, et al. Importance of light smoking and inhalation habits on risk of myocardial infarction and all-cause mortality. A 22-year follow-up of 12 149 men and women in The Copenhagen City Heart Study. J Epidemiol Community Health. 2002;56:702–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pechacek TF, Babb S. How acute and reversible are the cardiovascular risks of secondhand smoke? BMJ. 2004;328:980–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ventura SJ, Hamilton BE, Mathews TJ, et al. Trends and variations in smoking during pregnancy and low birthweight: evidence from the birth certificate, 1990–2000. Pediatrics. 2003;111: 1176–1180. [PubMed] [Google Scholar]
- 39.Yang W, Jennison BL, Omaye ST. Cardiovascular disease hospitalization and ambient levels of carbon monoxide. J Toxicol Environ Health A. 1998;55: 185–196. [DOI] [PubMed] [Google Scholar]
- 40.Benowitz NL. The role of nicotine in smoking-related cardiovascular disease. Prev Med. 1997;26:412–417. [DOI] [PubMed] [Google Scholar]
- 41.Cohen JB. Smokers’ knowledge and understanding of advertised tar numbers: health policy implications. Am J Public Health. 1996;86:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilpin EA, Emery S, White MM, et al. Does tobacco industry marketing of “light” cigarettes give smokers a rationale for postponing quitting? Nicotine Tob Res. 2002;4(suppl 2):S147–S155. [DOI] [PubMed] [Google Scholar]
- 43.Federal Cigarette Labeling and Advertising Act of 1965. Pub. L. No. 89–92, 15 U.S.C. 1331 et seq. (July 27, 1965, as amended by Pub. L. No. 91–222, 84 Stat. 87, Apr. 1, 1970 and Pub. L. No. 98–474, 98 Stat. 2204, Oct. 12, 1984).
- 44.Information for smokers. Richmond, Va.: Philip Morris USA; 2004. Available at: http://www.philipmorris-usa.com/downloads/health_issues/low_tar_cigarettes/onsert.pdf. Accessed April 5, 2005.
- 45.WHO framework convention on tobacco control. Geneva: World Health Organization. May 1, 2003. Available at: http://www.who.int/tobacco/fctc/text/en/fctc_en.pdf. Accessed April 5, 2005.
- 46.Kozlowski LT, Goldberg ME, Yost BA, et al. Smokers’ misperceptions of light and ultra-light cigarettes may keep them smoking. Am J Prev Med. 1998; 15:9–16. [DOI] [PubMed] [Google Scholar]
- 47.Ling PM, Glantz SA. Tobacco industry research on smoking cessation. Recapturing young adults and other recent quitters. J Gen Intern Med. 2004; 19(5 Pt 1):419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pollay RW, Dewhirst T. The dark side of marketing seemingly “light” cigarettes: successful images and failed fact. Tob Control. 2002;11(suppl 1):I18–I31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.FTC Consumer Alert. Up in Smoke: The Truth About Tar and Nicotine Ratings. Washington, DC: Federal Trade Commission; 2000.
- 50.Hoffmann D, Hoffmann I. The changing cigarette, 1950–1995. J Toxicol Environ Health. 1997;50:307–364. [DOI] [PubMed] [Google Scholar]
- 51.Darnell A. Memorandum re: Philip Morris documents. Sept. 1, 1987. Available at: http://tobaccodocuments.org/landman/28340.html. Accessed April 5, 2005.
- 52.The Health Consequences of Smoking: Nicotine Addiction. A Report of the Surgeon General. Rockville. Md: US Dept of Health and Human Services; 1988.
- 53.Doll R, Peto R, Wheatley K, et al. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ. 1994;309:901–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tobacco. 19830000;19870205. Bates: 504231648–504231658. Available at: http://tobaccodocuments.org/rjr/504231648-1658_D1.html. Accessed April 5, 2005.
- 55.Stolerman IP, Jarvis MJ. The scientific case that nicotine is addictive. Psychopharmacology (Berl). 1995;117:2–10. [DOI] [PubMed] [Google Scholar]
- 56.The Health Benefits of Smoking Cessation: A Report of the Surgeon General. Rockville, Md: US Dept of Health and Human Services; 1990. [PubMed]
- 57.Cigarette smoking among adults—United States, 1995. MMWR Morb Mortal Wkly Rep. 1997;46:1217–1220. [PubMed] [Google Scholar]
- 58.Zhu S, Melcer T, Sun J, et al. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000;18:305–311. [DOI] [PubMed] [Google Scholar]
- 59.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence. Clinical Practice Guideline. Rockville Md: US Dept of Health and Human Services, Public Health Service; 2000.
- 60.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation (Cochrane Review). In: The Cochrane Library. Issue 2. Chichester, UK: John Wiley & Sons, Ltd; 2004. [DOI] [PubMed]
- 61.Hurt RD, Sachs DP, Glover ED, et al. A comparison of sustained-release bupropion and placebo for smoking cessation. N Engl J Med. 1997;337: 1195–1202. [DOI] [PubMed] [Google Scholar]
- 62.Swan GE, McAfee T, Curry SJ, et al. Effectiveness of bupropion sustained release for smoking cessation in a health care setting: a randomized trial. Arch Intern Med. 2003;163: 2337–2344. [DOI] [PubMed] [Google Scholar]
- 63.Croghan GA, Sloan JA, Croghan IT, et al. Comparison of nicotine patch alone versus nicotine nasal spray alone versus a combination for treating smokers: a minimal intervention, randomized multicenter trial in a nonspecialized setting. Nicotine Tob Res. 2003;5:181–187. [DOI] [PubMed] [Google Scholar]
- 64.Bohadana A, Nilsson F, Rasmussen T, Martinet Y. Nicotine inhaler and nicotine patch as a combination therapy for smoking cessation: a randomized, double-blind, placebo-controlled trial. Arch Intern Med. 2000;160:3128–3134. [DOI] [PubMed] [Google Scholar]
- 65.Jamerson BD, Nides M, Jorenby DE, et al. Late-term smoking cessation despite initial failure: an evaluation of bupropion sustained release, nicotine patch, combination therapy, and placebo. Clin Ther. 2001;23:744–752. [DOI] [PubMed] [Google Scholar]
- 66.Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States, 1995–1999. MMWR Morb Mortal Wkly Rep. 2002; 51:300–303. [PubMed] [Google Scholar]
- 67.Martel L, Bélanger A, Berthelot JM. Smoking and disability-free life in Canada. In: Report on the Demographic Situation in Canada 2000: Current Demographic Analysis. Ottawa, Ont: Statistics Canada; 2001.
- 68.Nusselder WJ, Looman CW, Marangvan de Mheen PJ, et al. Smoking and the compression of morbidity. J Epidemiol Community Health. 2000; 54:566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arday DR, Milton MH, Husten CG, et al. Smoking and functional status among Medicare managed care enrollees. Am J Prev Med. 2003;24: 234–241. [DOI] [PubMed] [Google Scholar]
- 70.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328:1519–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Janson C. The effect of passive smoking on respiratory health in children and adults. Int J Tuberc Lung Dis. 2004;8:510–516. [PubMed] [Google Scholar]
- 72.Iribarren C, Darbinian J, Klatsky AL, Friedman GD. Cohort study of exposure to environmental tobacco smoke and risk of first ischemic stroke and transient ischemic attack. Neuroepidemiology. 2004;23:38–44. [DOI] [PubMed] [Google Scholar]
- 73.Pitsavos C, Panagiotakos DB, Chrysohoou C, et al. Association between exposure to environmental tobacco smoke and the development of acute coronary syndromes: the CARDIO2000 case-control study. Tob Control. 2002;11:220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Otsuka R, Watanabe H, Hirata K, et al. Acute effects of passive smoking on the coronary circulation in healthy young adults. JAMA. 2001;286: 436–441. [DOI] [PubMed] [Google Scholar]
- 75.Woodward A, Laugesen M. How many deaths are caused by secondhand cigarette smoke? Tob Control. 2001;10:383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hill S, Blakely T, Kawachi I, Woodward A. Mortality among “never smokers” living with smokers: two cohort studies, 1981–4 and 1996–9. BMJ. 2004;328:988–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Law MR, Hackshaw AK. Environmental tobacco smoke. Br Med Bull. 1996;52:22–34. [DOI] [PubMed] [Google Scholar]
- 78.Law MR, Morris JK, Wald NJ. Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence. BMJ. 1997;315: 973–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Coultas DB. Passive smoking and risk of adult asthma and COPD: an update. Thorax. 1998;53:381–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Anderson HR, Cook DG. Passive smoking and sudden infant death syndrome: review of the epidemiological evidence. Thorax. 1997;52: 1003–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jha P, Chaloupka FJ. Curbing the Epidemic: Governments and the Economics of Tobacco Control. Washington, DC: The World Bank; 1999.
- 82.Warner KE, Fulton GA, Nicolas P, Grimes DR. Employment implications of declining tobacco product sales for the regional economies of the United States. JAMA. 1996;275:1241–1246. [PubMed] [Google Scholar]
- 83.Capehart T. The changing tobacco user’s dollar. Washington, DC: US Dept of Agriculture, Economic Research Service; 2004. Outlook Report No. TBS257-01.
- 84.Harris JR, Schauffler HH, Milstein A, Powers P, Hopkins DP. Expanding health insurance coverage for smoking cessation treatments: experience of the Pacific Business Group on Health. Am J Health Promot. 2001;15:350–356. [DOI] [PubMed] [Google Scholar]
- 85.Halpern MT, Shikiar R, Rentz AM, Khan ZM. Impact of smoking status on workplace absenteeism and productivity. Tob Control. 2001;10:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Warner KE. Cost-effectiveness of smoking-cessation therapies. Interpretation of the evidence and implications for coverage. Pharmacoeconomics. 1997; 11:538–549. [DOI] [PubMed] [Google Scholar]
- 87.Tobacco use, access, and exposure to tobacco in media among middle and high school students—United States, 2004. MMWR Morb Mortal Wkly Rep. 2005;54:297–301. [PubMed] [Google Scholar]
- 88.Jamrozik K. Population strategies to prevent smoking. BMJ. 2004;328: 759–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Master settlement agreement (as amended). Available at: http://www.naag.org/issues/tobacco/index.php?sdpid=919. Accessed April 5, 2005.
- 90.Lombardi F, Saltonstall D. Firms stoked to fight smoke ban. New York Daily News. September 19, 2002:14.
- 91.Tobacco Industry Strategies to Undermine Tobacco Control Activities at the World Health Organization. Geneva, Switzerland: World Health Organization; July 2000.
- 92.Glantz SA. The truth about big tobacco in its own words. BMJ. 2000; 321:313–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Francey N, Chapman S. “Operation Berkshire”: the international tobacco companies’ conspiracy. BMJ. 2000;321: 371–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kasindorf M. Tobacco execs launch attack on anti-smoking ads. USA Today. June 8, 2003:A4.
- 95.Hirschhorn N. Corporate social responsibility and the tobacco industry: hope or hype? Tob Control. 2004;13: 447–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chung PJ, Garfield CF, Rathouz PJ, et al. Youth targeting by tobacco manufacturers since the Master Settlement Agreement. The first study to document violations of the youth-targeting ban in magazine ads by the three top US tobacco companies. Health Aff (Millwood). 2002;21:254–263. [DOI] [PubMed] [Google Scholar]
- 97.King C III, Siegel M. The Master Settlement Agreement with the tobacco industry and cigarette advertising in magazines. N Engl J Med. 2001;345: 504–511. [DOI] [PubMed] [Google Scholar]
- 98.Sargent JD, Dalton M, Beach M. Exposure to cigarette promotions and smoking uptake in adolescents: evidence of a dose-response relation. Tob Control. 2000;9:163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Campaign for Tobacco-Free Kids. New poll shows kids still bombarded with tobacco advertising [press release]. Apr. 3, 2002. Available at: http://tobaccofreekids.org/Script/DisplayPressRelease.php3?Display=472. Accessed April 5, 2005.
- 100.Pollay RW, Siddarth S, Siegel M, et al. The last straw? Cigarette advertising and realized market shares among youths and adults, 1979–1993. J Marketing. 1996;60:1–16. [Google Scholar]
- 101.Dalton MA, Sargent JD, Beach ML, et al. Effect of viewing smoking in movies on adolescent smoking initiation: a cohort study. Lancet. 2003;362: 281–285. [DOI] [PubMed] [Google Scholar]
- 102.Glantz SA, Kacirk KW, McCulloch C. Back to the future: smoking in movies in 2002 compared with 1950 levels. Am J Public Health. 2004;94: 261–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sargent JD, Tickle JJ, Beach ML, Dalton MA, Ahrens MB, Heatherton TF. Brand appearances in contemporary cinema films and contribution to global marketing of cigarettes. Lancet. 2001; 357:29–32. [DOI] [PubMed] [Google Scholar]
- 104.Tickle JJ, Sargent JD, Dalton MA, Beach ML, Heatherton TF. Favourite movie stars, their tobacco use in contemporary movies, and its association with adolescent smoking. Tob Control. 2001;10:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.DuRant RH, Rome ES, Rich M, et al. Tobacco and alcohol use behaviors portrayed in music videos: a content analysis. [Published erratum in Am J Public Health.1997;87:1514.] Am J Public Health. 1997;87:1131–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wakefield M, Flay B, Nichter M, et al. Role of the media in influencing trajectories of youth smoking. Addiction. 2003;98(suppl 1):79–103. [DOI] [PubMed] [Google Scholar]
- 107.Pierce JP, Distefan JM, Jackson C, et al. Does tobacco marketing undermine the influence of recommended parenting in discouraging adolescents from smoking? Am J Prev Med. 2002; 23:73–81. [DOI] [PubMed] [Google Scholar]
- 108.Farrelly MC, Healton CG, Davis KC, Messeri P, Hersey JC, Haviland ML. Getting to the truth: evaluating national tobacco countermarketing campaigns [Published erratum in Am J Public Health.2003;93:703]. Am J Public Health. 2002;92:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hu T, Sung HY, Keeler TE. Reducing cigarette consumption in California: tobacco taxes vs an anti-smoking media campaign. Am J Public Health. 1995;85: 1218–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pierce JP, Macaskill P, Hill D. Long-term effectiveness of mass media–led anti-smoking campaigns in Australia. Am J Public Health. 1990;80:565–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Macaskill P, Pierce JP, Simpson JM, Lyle DM. Mass media–led anti-smoking campaign can remove the education gap in quitting behavior. Am J Public Health. 1992;82:96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Flynn BS, Worden JK, Secker-Walker RH, Badger GJ, Geller BM, Costanza MC. Prevention of cigarette smoking through mass media intervention and school programs. Am J Public Health. 1992;82:827–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Perry CL, Kelder SH, Murray DM, Klepp KI. Communitywide smoking prevention: long-term outcomes of the Minnesota Heart Health Program and the Class of 1989 Study. Am J Public Health. 1992;82:1210–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health. 2005; 95:1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]