Abstract
In the Diabetes Initiative of The Robert Wood Johnson Foundation, an ecological perspective helped identify the following key resources and supports for self-management (RSSM): individualized assessment, collaborative goal setting, skills enhancement, follow-up and support, access to resources, and continuity of quality clinical care. These RSSM reflect the grounding of diabetes self-management in the context of social and environmental influences. Research supports the value of each of these key resources and supports. Differences among self-management interventions may be seen as complementary, rather than conflicting, ways of providing RSSM. This way of understanding differences among interventions may aid development of varied programs to reach diverse audiences. In contrast to the “5 A’s” model of key provider services (Assess, Advise, Agree, Assist, and Arrange), RSSM articulate self-management from the perspective of individuals’ needs. Both approaches emphasize identification of goals, teaching of skills, and facilitation and reinforcement of the use of those skills.
Developed from research on how people may manage their behavior,1 extensions of this research to problems like smoking and overweight,2,3 and research on promoting healthier lifestyles and behavior patterns in health education, the concept of “self-management” has received emphasis in diabetes care and care of other chronic diseases over the past 30 years.4–6 In its National Standards for Diabetes Self-Management Education, the American Diabetes Association recognized self-management education as “the cornerstone of care for all individuals with diabetes who want to achieve successful health-related outcomes.”7(p682) Similarly, the Web page of the American Association of Diabetes Educators describes that organization as dedicated to “self-management training and care as integral components of health care for persons with diabetes.”8
In reaction to the determinism theory of behaviorism, Mahoney and Thoresen, in their 1974 book Self-Control: Power to the Person,1 advanced the argument that people could control their own behavior. However, the question of whether the individual controls his or her own behavior or whether behavior is controlled by environmental forces remains controversial. Although he titled his book Self-Efficacy: The Exercise of Control, Albert Bandura acknowledged that “Most human behavior . . . is determined by many interacting factors, and so people are contributors to, rather than the sole determiners of, what happens to them.”9 Nevertheless, an emphasis on individual responsibility remains a strong theme in writings on self-management. For example, a 2003 review included a statement that “Whether one is engaging in a health promoting activity such as exercise or is living with a chronic disease such as asthma, he or she is responsible for day-to-day management. . . . The issue of self management is especially important for those with chronic disease, where only the patient can be responsible for his or her day-to-day care over the length of the illness.”10
Data do not support the view that self-management interventions enable individuals to control their own behavior. A meta-analysis of self-management programs in diabetes by Norris and colleagues found sharp declines in benefits only a few months after interventions ended.11 Interventions promoting self-management resulted in an improvement in glycosylated hemoglobin of 0.76 percentage points in case subjects relative to control subjects at immediate follow-up, but this figure declined to 0.26 percentage points when assessments occurred more than 1 month after treatment ended. (Glycosylated hemoglobin represents the percentage of hemoglobin cells that have been modified by glucose in the blood and is thus an index of average blood sugar values over a period of approximately 120 days.12 Normal levels of glycosylated hemoglobin are 4% to 6%, and 7% is a widely endorsed target for glycemic control.) This finding mirrors well-established patterns of relapse after interventions promoting weight loss13 and smoking cessation.14 Among the demographic and intervention characteristics examined in the meta-analysis of Norris and colleagues, only duration of the intervention was found to predict a program’s success. As the authors noted, “Interventions with regular reinforcement are more effective than one-time or short-term education.”15 The association of benefit with length and variety of treatment has also been observed in meta-analyses of smoking cessation interventions16,17 and meta-analysis of a variety of patient education programs addressing health risks or health-promoting behaviors (e.g., breast self-examination).18 Self-management is dependent on the environmental contexts that surround the individual.
Much evidence exists for the importance of what has come to be called self-management training or education. For the purpose of their review, Norris and colleagues defined self-management interventions as including instruction in such skills as weight loss/weight management, physical activity, and medication management and blood glucose monitoring as well as other tasks specific to diabetes management. Self-management interventions meeting this definition have been found to improve patterns of disease management15 and metabolic control among adults with type 2 diabetes.11
Additional support for self-management has come from 2 major multisite clinical trials. To demonstrate that improved metabolic control reduces complications from diabetes, the Diabetes Control and Complications Trial relied upon effective interventions to teach patients the disease-management behaviors necessary to achieve improved metabolic control and to support patients in maintaining those behaviors over the course of the trial.19,20 In the Diabetes Prevention Program, behavioral interventions designed to help high-risk individuals achieve modest weight loss (7% of body weight) and modest levels of physical exercise (150 minutes per week) reduced conversion to type 2 diabetes in patients by 58% relative to controls.21 Lifestyle interventions in China22 and Finland23 reported similar findings. Additionally, a number of smaller group and individual self-management interventions have documented improvements in self-efficacy, self-management behaviors, metabolic control, patient satisfaction, and quality of life among individuals with diabetes,24–32 including older type 2 patients and ethnic minorities.33–35
BEYOND THE SELF IN SELF-MANAGEMENT
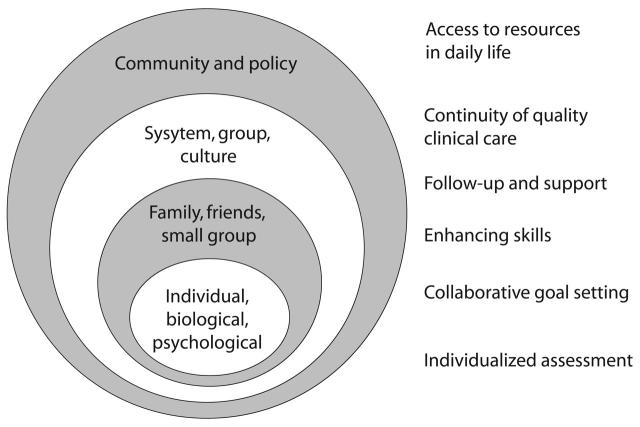
In contrast to views of self-management that emphasize a supposed ability of the individual to control his or her own behavior, an ecological approach to self-management integrates the skills and choices of individuals with the services and support they receive from (1) the social environment of family, friends, worksites, organizations, and cultures; and (2) the physical and policy environments of neighborhoods, communities, and governments.36 Self-management from an ecological perspective requires access to a variety of resources, including services provided by professionals and support for the initiation and maintenance of healthy behaviors. A range of influences cause behavior, including interventions and influences applied directly to the individual, as well as social, organizational, community, governmental policy, and economic factors.37–39 Figure 1 ▶ employs an ecological approach to portray levels of influence on self-management. (It also shows the resources and supports for self-management, which are described in the next section, that correspond with these levels of influence.)
FIGURE 1—
Correspondence of ecological levels of influence with resources and supports for self-management.
Ecological perspectives also point to the importance of access to key resources in self-management.40 Healthy eating patterns and physical activity levels are not likely to occur or persist without convenient sources of healthy foods and attractive and safe settings for exercise. The impact of “built environments” has been of increasing interest in recent years41,42; for example, studies have demonstrated the strong negative and positive effects, respectively, that access to resources for physical activity43,44 and consumption of food purchased away from home have on overweight.45
RESOURCES AND SUPPORTS FOR SELF-MANAGEMENT
The Diabetes Initiative of The Robert Wood Johnson Foundation includes 14 projects intended to both demonstrate and evaluate diabetes self-management promotion in primary care and community settings.46 To develop a shared template of self-management programs across the 14 projects, we used an ecological perspective to identify several key resources and supports for self-management (RSSM) needed by individuals: individualized assessment, collaborative goal setting, skills enhancement, follow-up and support, access to resources in daily life, and continuity of quality clinical care. These RSSM appear in Figure 1 ▶ as they correspond to the levels of behavioral influence posited by ecological perspectives. As the figure indicates, some of the RSSM, such as individualized assessment and collaborative goal setting, tend to be addressed at the individual level of influence, whereas others, such as access to resources and continuity of quality clinical care, are more often addressed at the system, group, and policy level. However, these correspondences are not rigid. Policies influence the choices and goals available to individuals; individuals may learn skills to access resources otherwise unavailable to them.
To examine the extent to which RSSM are addressed in current research and writing on diabetes management, we reviewed abstracts from Medline (available at: http://www.ncbi.nlm.nih.gov/entrez) published between January 2003 and June 2004 that included (a) cognates of “self-management,” “co-management,” “patient education,” or “empowerment” and (b) cognates of “diabetes.” Because this sampling covered only 18 months, it was not meant to form a basis for drawing broad conclusions but rather to provide an overview of recent research. Table 1 ▶ presents a digest of articles that we identified, organized in terms of each of the categories of RSSM. We have also included in Table 1 ▶ articles identified in a forthcoming book chapter describing self-management in primary care settings.93
TABLE 1—
Recent Research in Diabetes Management Regarding Resources and Supports for Self-Management
| Resource or Support Addressed | Reported Results of Research |
| Individualized assessment |
|
| Collaborative goal setting |
|
| Skills enhancement |
|
| Follow-up and support |
|
| Access to resources in daily life |
|
| Continuity of quality clinical care |
|
Note. GHb = glycosylated hemoglobin; PCP = primary care provider. Table was based on a Medline review of articles published between January 2003 and June 2004. It also includes articles identified in a forthcoming book chapter on self-management in primary care settings.93
Individualized Assessment
Substantial research has investigated psychological, cultural, and social factors in individuals’ “personal models of illness.”94 It is therefore considered a best practice for health education to begin with the perspective of the individual and that of the culture in which he or she was raised.95 This best practice often addresses issues such as concepts of illness, health, and death; the meaning of medication taking; views of the role of the individual; views of fate or control (including the natural history of diabetes); and views of the role of the individual vis-à-vis family and community. Professionals’ perspectives are presented not as the “right” way of viewing things but rather as the view of Western medicine, and one that the individual may consider in efforts to live a satisfying life with a chronic disease. This emphasis on the individual’s perspective contrasts with conventional practice, in which discussion and responses to the patient’s questions or reservations are organized around the professional’s view of the disease.
As indicated in Table 1 ▶, recent reports point to the importance of individualized assessment47 and have identified variation in perceived needs among people with diabetes.48 A key dimension for individualization may be individual perspectives associated with cultural differences. Self-management interventions have addressed superficial characteristics of culture, such as appropriate symbols or models, but not its deep structure, such as beliefs and norms.51 Also, it is interesting that the objective of individualizing assessment may be advanced by “high-tech” approaches such as computer-based applications for systematic tailoring of interventions to individual characteristics.53,54
Collaborative Goal Setting
Substantial research indicates both the importance of goal setting in behavior and the value of interventions that focus on goal setting.96,97 An influential demonstration of the benefits of enhancing the role of patients in planning their own care included a brief instruction and rehearsal session about how to ask questions of and negotiate with the primary care provider; the intervention resulted in significant improvements in multiple outcomes, including glycosylated hemoglobin levels, relative to controls.26 Table 1 ▶ presents data regarding the importance of active collaboration between patient and provider.55,56,58
Numerous approaches to collaborative goal setting exist. Motivational interviewing98 is one popular approach; it emerged from interventions for alcohol and drug dependence and gained considerable popularity in diverse patient education and health promotion interventions. Of growing interest is the application of high-tech approaches, such as computerized individual assessment to support efficient goal setting and attention to patient-selected goals throughout the course of care.53,54
Closely tied to an emphasis on collaborative goal setting is a recognition of the patient’s authority over his or her illness. Anderson and Funnell99 have suggested that the entire enterprise of patient education and self-management be referred to as “patient empowerment.” Building on previous research emphasizing individual choice and direction in self-management,100–102 they have documented the benefits of self-management interventions that stress the choices and responsibilities of the patient.99 This approach contrasts with a relationship in which professionals encourage goals and the patient’s role is primarily to accept them.
Skills Enhancement
A consensus document on self-management sponsored by The Robert Wood Johnson Foundation and the Center for the Advancement of Health noted that only an estimated 20% of skills in disease management are disease specific.103 This figure may be an underestimate for diabetes, given the complexity of management of this disease. Nevertheless, many of the skills to be taught in disease management are general problem-solving skills, skills for resisting temptation and preventing relapse, self-monitoring strategies applicable across behaviors, and skills for enhancing general healthy-lifestyle patterns, such as healthy eating and physical activity. Well-established principles of patient education and behavior change include the importance of (1) identifying and teaching concrete behaviors and skills (e.g., how to read food labels for frozen and processed foods; how to estimate percentages of protein, carbohydrates, and fats in daily diet); (2) modeling and demonstrating skills; (3) rehearsing skills; (4) self-monitoring and providing feedback to enhance performance; (5) monitoring the implementation of skills in real-life settings and reviewing results; (6) revising plans and testing revised plans in light of results of initial efforts; and, at each step, (7) reinforcing progress.13,104–106
Successful self-management interventions incorporate a sequence of contacts, often group meetings, in which skills are introduced, practiced, and reviewed, with opportunities for real-world tests between sessions followed by further review, practice, and skill enhancement. This approach is in marked contrast to interventions that provide a series of didactic lectures or presentations about disease management but do not focus at the level of individual skills and their successful application in daily life.15,106
As outlined in Table 1 ▶, research provides strong evidence for the importance of enhancement of skills for self-management and for the utility of the patient’s sense of competence or self-efficacy as an indication that interventions are effective.9,25,67,102
Because disease management must become established throughout the individual’s daily life, it affects diverse areas of his or her activities and faces a wide range of barriers. Consequently, disease management requires skills for solving problems in daily life. Most approaches to teaching problem-solving skills use a sequence of steps: (1) identifying and pinpointing the problem, (2) identifying alternative ways of coping with the problem, (3) choosing from among those alternatives, (4) rehearsing the chosen alternative, (5) attempting the alternative, and (6) reviewing, revising plans, further rehearsing or developing skills. These steps also occur in common approaches to problem solving.10,13,107,108 They have been extended to a wide range of challenges, such as coping with family or social factors that may interfere with disease management and gaining support for disease management from the family or workplace.
Substantial evidence exists linking poor health and disease management not only to depression109–111 but also to a variety of other negative emotions, such as hostility, anger, stress, and anxiety.112 As noted in Table 1 ▶, a recent review66 found that self-management interventions—as well as those that included psychological content, such as problem-solving therapy or cognitive-behavior therapy—led to greater improvements in negative mood or quality of life than did educational interventions in which “participants only received information.”
Evaluations of interventions to address negative emotions have included such emotions’ impact on clinical risk factors.113,114 For example, a recent study among men in Singapore found that a 6-session group workshop on managing negative emotions and enhancing social ties and relationships produced striking reductions in depression, anger, perceived stress, heart rate, and blood pressure along with increased satisfaction with social support and quality of life.115 The American Association of Diabetes Educators has recently added “Healthy Coping” to its 7 key self-care behaviors in diabetes management.116
Follow-Up and Support
Reviews of interventions for the self-management of diabetes,11,15 as well as interventions for smoking cessation14,15 and interventions in other areas of health promotion,17 all note the importance of ongoing follow-up and support for behavior change. The content of follow-up may include continued assistance in refining problem-solving plans and skills, encouragement when performance and success is less than perfect, and help in responding to new problems that may emerge. This assistance may entail linking patients to primary care providers or other elements of the disease management team.
Support may be provided through telephone calls73,117 or the internet.118 Automated telephone monitoring of patients, combined with nurse follow-up and tailored information, has been shown to reach low-income and minority patients, to elicit valid self-reported blood glucose levels, and to produce not only decreased blood glucose levels but also increased self-efficacy and reduced levels of depression.74–76,119 This finding is consistent with research in other areas, such as smoking cessation, in which telephone counseling has been shown to be effective.120,121
A popular and effective approach to providing follow-up and support is through use of community-based activities and nonprofessionals such as community health workers, lay health workers, promotoras (“health promoters”), or health coaches. In a number of settings, community health workers are involved in the care team and are effective in individualized assessment, goal setting, and teaching skills as well as in providing follow-up and support.122–124 The Diabetes Initiative projects exemplify the widespread use of promotoras in individualized, peer-based patient education, problem solving, and ongoing support and encouragement. Research has identified several characteristics of such providers that may be especially beneficial, including easy access, limited constraints on the extent or focus of service,125 and nondirective support (cooperating without taking control, accepting the individual’s perspective rather than prescribing correct courses of action)126,127 or support that enhances autonomy.128
Another way of both providing ongoing support and integrating such support with clinical care is the group medical visit,129 in which all patients in a particular category—for example, those with diabetes—are scheduled for a 2- to 3-hour group visit. Physicians and other staff perform basic assessments and individual medical visits; the group visit also includes educational and supportive discussions or other activities. Evaluations of group medical visits have indicated impressive effects on glycosylated hemoglobin and other measures relative to usual care.130,131
As indicated in Table 1 ▶, recent research on follow-up and support presents a mixed picture. The meta-analytic reviews of Norris et al.11,15 point to the importance of duration of treatment. Some individual studies, such as one demonstrating the benefits of nurse follow-up phone calls over 12 weeks,69 are striking examples of the value of extending support. Other studies also support the value of telephone follow-up.73,74–76,119 On the other hand, (1) some meta-analyses fail to find a relationship between duration of intervention and outcome,65 (2) stated interest in support may vary among individuals with diabetes,48 and (3) some efforts to provide support receive very little response from those they seek to help. For example, only 41% of participants attended even 1 meeting of monthly support groups over a 3- to 12-month period following a 4-hour education program.71 Although appreciable research in diabetes and other areas indicates the importance of follow-up and support, it is not well understood what types of support will actually benefit people, how much people want or will avail themselves of support, and what the relationship is between desire for support, desirable aspects of support, and effectiveness of support. As a result, follow-up and support are among the most difficult aspects of self-management to implement and the least frequently provided for a variety of health behaviors.132,133
Implicit in focusing on follow-up and support and on access to resources is the idea that because chronic disease management is for the rest of the patient’s life, interventions to support management need also to be extended over the lifetime. In addition, changes in circumstances, such as retirement, widowhood, marriage, children moving out of the household, or reduced physical ability with aging, may have substantial impacts on diabetes self-management, necessitating review and reestablishment of self-management plans. The services outlined in this article, including goal setting, individualization of care, education about disease and the role of individual behavior in its care, skill enhancement, follow-up and support, and attention to availability of resources, need to be repeated throughout the patient’s life. The principle that “chronic disease requires chronic care” applies as much to services and interventions to support self-management of chronic disease as it does to medical management of chronic disease. It should be noted, however, that, although follow-up and support need to be extended over time, they need not be extremely intensive or costly.
Access to Resources in Daily Life
Skills for disease management are of little utility without access to the resources needed to carry out those skills. For example, convenient access to healthy foods and to attractive and safe settings for physical activity is necessary if healthy diet and healthy levels of physical activity are to be maintained. Research on how the “built environment” influences behavior and health has increased markedly over the past decade. In a study of North Carolina communities, the availability of walking trails and places for physical activity was associated with engaging in recommended amounts of physical activity, after control for demographic and other environmental factors.43 More generally, “urban sprawl” and the corresponding absence of compact, walkable neighborhoods are associated with greater obesity and hypertension and less walking.44
Research has also examined the impacts of policy and environmental factors on the availability of healthy food.134 Brownell and Horgen’s 2004 book Food Fight: The Inside Story of the Food Industry, America’s Obesity Crisis, and What We Can Do About It135 describes an “obesigenic” environment and outlines policy initiatives to address this environment. Such attention to environmental and policy influences on healthy eating, obesity, and diseases such as diabetes and cardiovascular disease has begun to identify policy initiatives resembling those combating cigarette smoking.14,136,137
A variety of community- and peer-based approaches have addressed the problem of access to resources. These include use of promotoras or coaches to help individuals identify available resources. Community-based groups or advisory boards may develop resources such as walking paths138 or may pursue advocacy campaigns to further such development. Research has also begun to address how communities might be redesigned to improve health behaviors and thus population health.41,42 A systematic review of interventions to promote physical activity139 concluded that “creation of or enhanced access to places for physical activity combined with informational outreach activities” as well as social support interventions (e.g., “buddy” systems) were effective in promoting physical activity. Similarly, a recent review140 found that (1) improving access to places and opportunities for physical activity in communities and workplaces and (2) improving access to and reducing prices of healthy foods in vending machines, restaurants, and cafeterias were effective in increasing physical activity and healthy eating.
Although studies such as those cited here have reported interventions that address resources and supports for physical activity, healthy eating, and other healthy behaviors, the Medline search of articles related to diabetes self-management published between January 2003 and June 2004 identified no articles addressing access to resources. An additional search of Medline from January 1, 1996, through April 15, 2005, identified abstracts that included (1) cognates of “access” or “resources”; (2) cognates of “physical activity,” “exercise,” “diet,” “eat,” “food,” “support,” or “encourage”; and (3) cognates of “diabetes.” Restricting results to reports of studies involving humans and articles in English yielded 266 citations. Review of these articles identified the 5 projects described under “Access to Resources” in Table 1 ▶ that describe community and intervention studies to increase access to resources for diabetes self-management. These 5 projects include implementing community approaches to identify and develop resources for physical activity and healthy eating,80–82 using pharmacists to provide self-management resources in individuals’ daily circumstances,78,79 and developing an individualized, multilevel intervention to provide support for maintaining improvements brought about through a self-management program.83 Additional studies have found that Web-based discussion groups and other information resources are well accepted and used by individuals with type 2 diabetes.84,85 Although few in number, studies of access to resources in diabetes management suggest that the sorts of interventions used to promote physical activity and healthy eating in populations may be extended to management of diabetes and other chronic diseases.
Continuity of Quality Clinical Care
Self-management and quality clinical care are not only compatible with but also dependent on each other. Without sound clinical care, the individual’s efforts may be misdirected—for example, in frustration over failure of dietary changes to lower cholesterol when cholesterol-lowering medications are indicated. Without self-management, however, expert clinical care will fall far short of its potential, through patients’ failure to use prescribed medications or to implement management plans, or through their failure to carry out behavioral changes that can extend the benefits of medical management.
Wagner’s chronic care model89,90 provides an excellent framework for integrating RSSM with key components of clinical care. In a review of initial applications of the chronic care model, Glasgow and colleagues found that it had been successful “in over 300 diverse health care systems in the context of quality improvement efforts (Institute for Health Improvement Breakthrough Series) for asthma, congestive heart failure, depression, diabetes, and prevention of frailty in the elderly—where it has been found to provide an extremely helpful organizing framework for these diverse quality improvement efforts.”141,142
A report by Larsen et al.86 (Table 1 ▶) suggests the practicality and benefits of a comprehensive approach to improved clinical care (e.g., physician incentives for meeting testing guidelines) and a wide range of self-management services (e.g., outpatient and Web-based programs, telephone case management). The authors’ emphasis on the integration of comprehensive clinical and self-management services, however, is not widely shared in health care. Rather, a general lack of support prevails for “lifestyle” or behavioral aspects of chronic care management in health care systems. For example, a recent study of 19 health plans used by 2 Fortune 500 companies143 compared the number of plans offering various services relative to a base rate, 15 out of 19, of plans covering eye examinations. Nine offered smoking cessation services, and 8 offered diabetes self-management education. Only 3 offered services for obesity, 4 for exercise training, and 4 for case management.
That health systems generally fail to support lifestyle or behavioral aspects of chronic care management is apparent from surveys of individuals with diabetes. Among adults with type 2 diabetes surveyed in 1989 through the National Health Interview Survey, 91% reported having 1 physician whom they saw for regular care of diabetes. Fifty-two percent of the adults taking insulin and 40% of those not taking insulin reported at least 4 visits per year to a physician for diabetes, but only 21% reported seeing a dietitian or nutritionist. Among the adults taking insulin, 49% reported having had a “diabetes education class or course,” but among those not taking insulin, only 24% reported such education.144 Apparently, health care systems and policy-makers have failed to grasp the value of what should be central components of state-of-the-art care, even though (1) expert panels have advocated the importance of patient education in chronic care,103 (2) research has clearly identified the value of patient education and self-management interventions in the prevention and management of diabetes,19,21 and (3) the research summarized in Table 1 ▶ supports the value of RSSM.
“EQUIFINALITY” AND THE VARIETY OF SELF-MANAGEMENT INTERVENTIONS
RSSM are particularly useful in that they provide a way of making sense of what is frequently a dizzying maze of competing treatment approaches. For example, both motivational interviewing98 and interventions that are based on the transtheoretical model145 designed for patients in the pre-contemplation or contemplation phases of change may be viewed as approaches to goal setting. Rather than viewing these approaches as competing or incompatible, it may be more helpful to see them as alternative ways of addressing the similar objectives of goal setting.146
The concept of “equifinality” may help to clarify how varied intervention approaches may have similar roles or purposes. Drawn from research on organizational behavior,147 equifinality refers to different procedures’ or programs’ following different paths to achieve similar ends—that is, differing procedures and paths share common final effects. Consider smoking cessation. Evidence from the 2000 Agency for Healthcare Research and Quality guidelines for smoking cessation17 indicates that the number of different formats combined in a treatment is more important than the nature of the formats themselves.14 In other words, a number of effective approaches to smoking cessation exist, with no particular intervention being remarkably more effective than others. Additionally, different interventions may be effective in fulfilling similar functions. Thus, counseling in primary care, mass media, or messages tailored to smokers not yet ready to quit may each be effective approaches for reaching smokers and helping motivate them to quit. Continuing with the example of smoking cessation, individual counseling, group programs, and self-help materials may each be effective ways to help people plan cessation and master behavioral self-management skills for avoiding relapse. Follow-up from professionals, from trained volunteers, or through print or other media may also help smokers who have quit not to start again.
The concept of equifinality also applies to self-management of diabetes and to other areas of health promotion. Table 2 ▶ provides a template in which individual RSSM are listed with diverse approaches to accomplishing each. Depending on the setting, the individuals to be served, other local factors, and the preferences of those to be served, different approaches may be appropriate for addressing each of the key areas of RSSM. Thus, collaborative goal setting may be pursued by a primary care provider, a medical assistant, a community health worker, or a Web resource. Enhancement of skills can occur through group classes, manuals and self-help materials, television shows, or many other channels. Follow-up and support may include training family members, using community health workers for ongoing support, and providing telephone support lines, in addition to ongoing follow-up by professionals. Thus, equifinality means that a variety of tactics and intervention approaches may be used to address key functions or objectives of self management. RSSM or some similar model is necessary to identify what those key functions or objectives are.
TABLE 2—
Resources and Supports for Self-Management and Tactics and Channels for Addressing Them
| Resources and Supports for Self-Management | Tactics and Channels |
| Individualized assessment | Web-based interventions Individual counseling Delivered by PCP, nurse, community health worker |
| Collaborative goal setting | Web-based interventions Individual counseling Group programs Delivered by PCP, nurse, community health worker |
| Skills enhancement | Web-based interventions Individual counseling Group programs Group medical visits Community-based classes (e.g., for physical activity, healthy cooking) Delivered by PCP, nurse, community health worker, community-based teachers |
| Follow-up and support | Group medical visits Telephone follow-up Support groups Community-based activities (e.g., walking groups) Delivered by PCP, nurse, medical assistant, community health worker, community volunteers, voluntary health organizations |
| Access to resources in daily life | Patient education regarding locating and accessing resources Community coalitions Governmental groups (e.g., park and recreation commissions) Commercial fitness clubs and weight-loss programs Advocacy campaigns of voluntary health organizations Delivered/organized by nurses, community health workers, voluntary health organizations |
| Continuity of quality clinical care | Application of Chronic Care Model89,90 within clinical settings Patient activation and empowerment campaigns of voluntary health organizations Health provider and health financing organizations |
Note. PCP = primary care provider.
INTEGRATION OF RSSM WITH OTHER MODELS OF SELF-MANAGEMENT
The approach to self-management emphasizing RSSM shares much with other approaches in the field. Extending the “5 A’s” mnemonic for encouraging smoking cessation in primary care,148 Whitlock and colleagues149 suggest Assess, Advise, Agree, Assist, and Arrange as an approach to self-management implemented through clinical settings. The Quality Alliance program of The Robert Wood Johnson Foundation has extended the framework of the 5 A’s as a structure for planning and implementing ongoing services to support patients’ self-management at multiple levels (see Glasgow et al.150).
As shown in Table 3 ▶, the 2 versions of self-management posited by the 5 A’s and RSSM may be viewed as 2 sides of the same coin, reflecting their origins. The 5 A’s emerge from initiatives to promote self-management through clinical interventions; accordingly, they tend to direct attention to things providers can do and services providers can arrange that will promote patient self-management. Rooted in ecological perspectives, RSSM reflect individuals’ needs not only for clinical services but also for resources and supports for self-management in the context of daily life.
TABLE 3—
Correspondence of Core Concepts of Self-Management with the “5 A’s” and Resources and Supports for Self-Management
| Core Concepts of Self-Management | “5 A’s” | Resources and Supports for Self-Management |
| Identification of objectives | Assess | Individualized assessment |
| Advise | ||
| Agree | Collaborative goal setting | |
| Skills | Assist | Skills for—
|
| Facilitation, incentives, support for maintaining behavior | Arrange | Ongoing follow-up and support Access to resources in daily life |
| Link to clinical care | Implicit in assumption that in most cases, 5 A’s are implemented within clinical settings | Continuity of quality clinical care |
Note. For “5 A’s,” see Whitlock et al.149
The difference is clearly one of emphasis rather than an essential one. For example, the “Arrange” of the 5 A’s can easily be expanded to include attention to resources for self-management in people’s daily lives. However, this difference in emphasis may have practical utility, depending on setting and objectives—for example, whether to plan and evaluate services to be offered by a provider or provider group or whether to plan and evaluate services intended to address the full range of needs and resources available to a population. The 5 A’s may have pertinence if the focus is on implementing services in clinical or other focused settings, whereas RSSM may be helpful if the focus is on community or other broad approaches to assessing and addressing the needs of a population.
Underlying both the 5 A’s and RSSM is a simple framework of behavior change and self-management that encompasses 3 essential features: (1) identification of objectives or goals, (2) learning of skills to achieve the objectives, and (3) facilitation and reinforcement of skills and their execution. Thus, for behavior change to occur, a goal or objective must have been chosen (preferably by the person whose behavior is to change), necessary skills must be present or acquired, and incentives and opportunities must exist for the behavior to be performed. From the perspective of the individual, this framework leads to a simple characterization of self-management as requiring 3 types of assistance:
Help me figure out where I am and where I want to go.
Help me acquire the skills and resources to get there.
Help me stay motivated and adjust my plan.
CONCLUSIONS
Self-management, with its many dimensions and influences, emerges as an ecologically framed set of processes and behaviors.36–39 Understanding self-management of diabetes leads to an appreciation of the complementary nature of processes rooted at the individual level (e.g., assessment, goal setting, learning skills) and processes that are intrinsically social and based in families, organizations, neighborhoods, and communities (e.g., access to resources or ongoing support and encouragement of effective management).
RSSM provide a framework for key functions in self-management and varied approaches to addressing them. This framework may be especially helpful in understanding and organizing different tactical approaches for achieving similar ends—for example, collaborative goal setting through interaction with a primary care physician, a community health worker, or an interactive Web utility. Recognition of the concept of “equifinality”—that diverse approaches may achieve similar ends—may lead to programs offering a broader range of intervention approaches with greater appeal to adults with diabetes or other chronic diseases. Recognizing equifinality also sheds light on how different intervention tactics or approaches may contribute to intervention packages tailored to specific audiences’ contexts and environments.
Recent literature on diabetes management addresses and generally confirms the importance of each of the components of RSSM. The single exception is access to resources in daily life, such as attractive and safe locations for physical activity and sources of affordable and attractive healthy food. Substantial research in general populations indicates the utility of addressing access to and opportunities for physical activity and purchase of healthy food,41–44,138–140 and several studies have suggested the promise of applying these approaches to diabetes self-management.78–85 However, further research is needed in this important area. In fact, the relative scarcity of research in diabetes self-management that examines resources in daily life shows the importance of the ecological perspective in pointing out how self-management is grounded in the community, society, and health policy. Extending ecological perspectives, Stokols and colleagues151 have combined an emphasis on “cultivation of human resources” (e.g., social capital152) with attention to material resources (e.g., built environment and economic and employment factors) to provide a broader approach to understanding the effects of human environments on behavior and health.
In addition to exploring ways to address RSSM, future research should address (1) how to integrate individualized assessment, collaborative goal setting, and instruction in self-management skills into primary care settings; (2) how to redesign primary care delivery to better accommodate self-management interventions, such as through group medical visits; (3) how to develop comprehensive approaches to depression and other negative emotions as they emerge during the course of diabetes and compromise its management as well as quality of life; (4) how to provide consistent and ongoing support, monitoring, and assistance for diabetes management; and (5) how to enhance access to resources for diabetes self-management in daily life.
Acknowledgments
This work was supported by The Robert Wood Johnson Foundation Diabetes Initiative and the Washington University Diabetes Research and Training Center (grant NIDDK DK 20579).
Peer Reviewed
Contributors E.B. Fisher and R.E. Glasgow wrote the initial version of the article. C.A. Brownson, M.L. O’Toole, G. Shetty, and V.V. Anwuri collaborated in developing the model of Resources and Supports for Self-Management and applying the ecological model to diabetes self-management. All authors revised and edited the article.
References
- 1.Mahoney MJ, Thoresen CE. Self-Control: Power to the Person. Monterey, Calif: Brooks/Cole; 1974.
- 2.Stuart RB. Behavioral control of overeating. Behav Res Ther. 1967;5:357–365. [Google Scholar]
- 3.Lando H. Successful treatment of smokers with a broad-spectrum behavioral approach. J Consult Clin Psychol. 1977;45:361–366. [DOI] [PubMed] [Google Scholar]
- 4.Etzwiler DD. Teaching allied health professionals about self-management. Diabetes Care. 1980;3:121–123. [DOI] [PubMed] [Google Scholar]
- 5.Etzwiler DD. Diabetes management. The importance of patient education and participation. Postgrad Med. 1986;80:67–72. [DOI] [PubMed] [Google Scholar]
- 6.Hiss RG. The activated patient: a force for change in diabetes health care and education. Diabetes Educ. 1986;12:600–602. [PubMed] [Google Scholar]
- 7.Mensing C, Boucher J, Cypress M, et al. National standards for diabetes self-management education. Diabetes Care. 2000;23(5):682–689. [DOI] [PubMed] [Google Scholar]
- 8.American Association of Diabetes Educators. About AADE. Available at: http://www.aadenet.org/AboutAADE. Accessed June 10, 2005.
- 9.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: W. H. Freeman; 1997.
- 10.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. [DOI] [PubMed] [Google Scholar]
- 11.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein DE, Little RR, Lorenz RA, et al. Tests of glycemia in diabetes. Diabetes Care. 2004;27:1761–1773. [DOI] [PubMed] [Google Scholar]
- 13.Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegen BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. J Consul Clin Psychol. 2001;69:722–726. [PubMed] [Google Scholar]
- 14.Fisher EB, Brownson RC, Heath AC, Luke DA, Sumner W II. Cigarette smoking. In: Boll TJ, Raczynski J, Leviton L, eds. Handbook of Clinical Health Psychology, Vol. 2. Washington, DC: American Psychological Association; 2004; 75–120.
- 15.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. [DOI] [PubMed] [Google Scholar]
- 16.Kottke TE, Battista RN, DeFriese GH. Attributes of successful smoking cessation interventions in medical practice: a meta-analysis of 39 controlled trials. JAMA. 1988;259:2882–2889. [DOI] [PubMed] [Google Scholar]
- 17.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline. Rockville, Md: US Dept of Health and Human Services, Public Health Service; 2000.
- 18.Mullen PD, Green LW, Persinger GS. Clinical trials of patient education for chronic conditions: a comparative meta-analysis of intervention types. Prev Med. 1985;14:753–781. [DOI] [PubMed] [Google Scholar]
- 19.Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. [DOI] [PubMed] [Google Scholar]
- 20.Diabetes Control and Complications Trial Research Group. Implementation of treatment protocols in the Diabetes Control and Complications Trial. Diabetes Care. 1995;18(3):361–376. [DOI] [PubMed] [Google Scholar]
- 21.Diabetes Prevention Program Research Group. Reduction of the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–544. [DOI] [PubMed] [Google Scholar]
- 23.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. [DOI] [PubMed] [Google Scholar]
- 24.Anderson RM, Funnell MM, Barr PA, Dedrick RF, Davis WK. Learning to empower patients: results of professional education program for diabetes educators. Diabetes Care. 1991;14:584–590. [DOI] [PubMed] [Google Scholar]
- 25.Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment: results of a randomized controlled trial. Diabetes Care. 1995; 18:943–949. [DOI] [PubMed] [Google Scholar]
- 26.Greenfield S, Kaplan SH, Ware JE, Yano EM, Frank H. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–457. [DOI] [PubMed] [Google Scholar]
- 27.Rubin RR, Peyrot M, Saudek CD. Effect of diabetes education on self-care, metabolic control, and emotional well-being. Diabetes Care. 1989;12:673–679. [DOI] [PubMed] [Google Scholar]
- 28.Rubin RR, Peyrot M, Saudek CD. The effect of a comprehensive diabetes education program incorporating coping skills training on emotional well-being and diabetes self-efficacy. Diabetes Educ. 1993;19:210–214. [Google Scholar]
- 29.Muhlhauser I, Berger M. Diabetes education and insulin therapy: when will they ever learn? J Intern Med. 1993;233:321–326. [DOI] [PubMed] [Google Scholar]
- 30.Pieber TR, Brunner GA, Schnedl WJ, Schattenberg S, Kaufmann P, Krejs GJ. Evaluation of a structured outpatient group education program for intensive insulin therapy. Diabetes Care. 1995;18:625–630. [DOI] [PubMed] [Google Scholar]
- 31.Clement S. Diabetes self-management education. Diabetes Care. 1995;18:1204–1214. [DOI] [PubMed] [Google Scholar]
- 32.Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization: a randomized, controlled trial. Ann Intern Med. 1998; 129(8):605–612. [DOI] [PubMed] [Google Scholar]
- 33.Glasgow R, Toobert DJ, Hampson S. Participation in outpatient diabetes education programs: how many patients take part and how representative are they? Diabetes Educ. 1991;5:376–380. [DOI] [PubMed] [Google Scholar]
- 34.Glasgow RE, Toobert DJ, Hampson SE, et al. Improving self-care among older patients with type II diabetes: the “Sixty Something...” Study. Patient Educ Couns. 1992;19:61–74. [DOI] [PubMed] [Google Scholar]
- 35.Anderson RM, Herman WH, Davis JM, Friedman RP, Funnell MM, Neighbors HW. Barriers to improving diabetes care for black persons. Diabetes Care. 1991;14:605–609. [DOI] [PubMed] [Google Scholar]
- 36.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10(4):282–298. [DOI] [PubMed] [Google Scholar]
- 37.Sallis JF, Owen N. Ecological models of health behavior. In: Glanz K, Lewis FM, Rimer BK, eds. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, Calif: Jossey-Bass; 2002:462–484.
- 38.McLeroy K, Bibeau D, Steckler A. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. [DOI] [PubMed] [Google Scholar]
- 39.Glasgow RE. A practical model of diabetes management and education. Diabetes Care. 1995;18(1): 117–126. [DOI] [PubMed] [Google Scholar]
- 40.Glasgow RE, Toobert DJ, Barrera MJ, Strycker LA. The Chronic Illness Resources Survey: cross-validation and sensitivity to intervention. Health Educ Res. 2005:402–409. [DOI] [PubMed]
- 41.Frank LD, Engelke PO, Schmid TL. Health and Community Design: The Impact of the Built Environment on Physical Activity. Washington, DC: Island Press; 2003.
- 42.Frumkin H, Frank L, Jackson R. Urban Sprawl and Public Health: Designing, Planning, and Building for Healthy Communities. Washington, DC: Island Press; 2004.
- 43.Huston SL, Evenson KR, Bors P, Gizlice Z. Neighborhood environment, access to places for activity, and leisure-time physical activity in a diverse North Carolina population. Am J Health Promot. 2003;18:58–69. [DOI] [PubMed] [Google Scholar]
- 44.Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18:47–57. [DOI] [PubMed] [Google Scholar]
- 45.Thompson OM, Ballew C, Resnicow K, et al. Food purchased away from home as a predictor of change in BMI z-score among girls. Int J Obes Relat Metab Disord. 2004;28(2):282–289. [DOI] [PubMed] [Google Scholar]
- 46.Diabetes Initiative: a national program of The Robert Wood Johnson Foundation. Available at: http://diabetesnpo.im.wustl.edu. Accessed June 10, 2005.
- 47.Funnell MM, Kruger DF, Spencer M. Self-management support for insulin therapy in type 2 diabetes. Diabetes Educ. 2004;30:274–280. [DOI] [PubMed] [Google Scholar]
- 48.Solberg LI, Desai JR, O’Connor PJ, Bishop DB, Devlin HM. Diabetic patients who smoke: are they different? Ann Fam Med. 2004;2:26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof. 1996;19(2): 208–230. [DOI] [PubMed] [Google Scholar]
- 50.Cox RH, Carpenter JP, Bruce FA, Poole KP, Gaylord CK. Characteristics of low-income African-American and Caucasian adults that are important in self-management of type 2 diabetes. J Community Health. 2004;29:155–170. [DOI] [PubMed] [Google Scholar]
- 51.Jack L, Liburd L, Spencer T, Airhihenbuwa CO. Understanding the environmental issues in diabetes self-management education research: a reexamination of 8 studies in community-based settings. Ann Intern Med. 2004;140:964–971. [DOI] [PubMed] [Google Scholar]
- 52.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 53.Glasgow RE, Toobert DJ, Hampson SE. Effects of a brief office-based intervention to facilitate diabetes dietary self-management. Diabetes Care. 1996;19:835–842. [DOI] [PubMed] [Google Scholar]
- 54.Glasgow RE, La Chance PA, Toobert DJ, Brown J, Hampson SE, Riddle MC. Long-term effects and costs of brief behavioural dietary intervention for patients with diabetes delivered from the medical office. Patient Educ Couns. 1997;32:175–184. [DOI] [PubMed] [Google Scholar]
- 55.Williams GC, McGregor HA, Zeldman A, Freedman ZR, Deci EL. Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychol. 2004;23(1): 58–66. [DOI] [PubMed] [Google Scholar]
- 56.Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18:893–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cooper H, Booth K, Gill G. Using combined research methods for exploring diabetes patient education. Patient Educ Couns. 2003;51:45–52. [DOI] [PubMed] [Google Scholar]
- 58.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004; 164:1641–1649. [DOI] [PubMed] [Google Scholar]
- 59.Litzelman DK, Slemenda CW, Langefeld CD, et al. Reduction of lower extremity clinical abnormalities in patients with non-insulin-dependent diabetes mellitus: a randomized, controlled trial. Ann Intern Med. 1993;119:36–41. [DOI] [PubMed] [Google Scholar]
- 60.Glasgow RE, Nutting PA, King DK, et al. A practical randomized trial to improve diabetes care. J Gen Intern Med. 2004;19(12):1167–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Simmons D, Gamble GD, Foote S, Cole DR, Coster G. The New Zealand Diabetes Passport Study: a randomized controlled trial of the impact of a diabetes passport on risk factors for diabetes-related complications. Diabet Med. 2004;21:214–217. [DOI] [PubMed] [Google Scholar]
- 62.Hill-Briggs F, Cooper DC, Loman K, Brancati FL, Cooper LA. A qualitative study of problem solving and diabetes control in type 2 diabetes self-management. Diabetes Educ. 2003;29:1018–1028. [DOI] [PubMed] [Google Scholar]
- 63.Parchman ML, Arambula-Solomon TG, Noel PH, Larme AC, Pugh JA. Stage of change advancement for diabetes self-management behaviors and glucose control. Diabetes Educ. 2003;29:128–134. [DOI] [PubMed] [Google Scholar]
- 64.Oh JA, Kim HS, Yoon KH, Choi ES. A telephone-delivered intervention to improve glycemic control in type 2 diabetic patients. Yonsei Med J. 2003;44:1–8. [DOI] [PubMed] [Google Scholar]
- 65.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns. 2004;52:97–105. [DOI] [PubMed] [Google Scholar]
- 66.Steed L, Cooke D, Newman S. A systematic review of psychosocial outcomes following education, self-management and psychological interventions in diabetes mellitus. Patient Educ Couns. 2003;51:5–15. [DOI] [PubMed] [Google Scholar]
- 67.Krichbaum K, Aarestad V, Buethe M. Exploring the connection between self-efficacy and effective diabetes self-management. Diabetes Educ. 2003;29:653–662. [DOI] [PubMed] [Google Scholar]
- 68.Anderson BJ, Wolf FM, Burkhart MT, Cornell RG, Bacon GE. Effects of peer-group intervention on metabolic control of adolescents with IDDM: randomized outpatient study. Diabetes Care. 1989;12:179–183. [DOI] [PubMed] [Google Scholar]
- 69.Kim HS, Oh JA. Adherence to diabetes control recommendations: impact of nurse telephone calls. J Adv Nurs. 2003;44:256–261. [DOI] [PubMed] [Google Scholar]
- 70.Cooper HC, Booth K, Gill G. Patients’ perspectives on diabetes health care education. Health Educ Res. 2003;18:191–206. [DOI] [PubMed] [Google Scholar]
- 71.Banister NA, Jastrow ST, Hodges V, Loop R, Gillham MB. Diabetes self-management training program in a community clinic improves patient outcomes at modest cost. J Am Diet Assoc. 2004;104:807–810. [DOI] [PubMed] [Google Scholar]
- 72.Riley KM, Glasgow RE, Eakin EG. Resources for health: a social-ecological intervention for supporting self-management of chronic conditions. J Health Psychol. 2001;6(6):693–705. [DOI] [PubMed] [Google Scholar]
- 73.Weinberger M, Kirkman MS, Samsa GP, et al. A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: impact on glycemic control and health-related quality of life. J Gen Intern Med. 1995;10:59–66. [DOI] [PubMed] [Google Scholar]
- 74.Piette JD, McPhee SJ, Weinberger M, Mah CA, Kraemer FB. Use of automated telephone disease management calls in an ethnically diverse sample of low-income patients with diabetes. Diabetes Care. 1999;22:1302–1309. [DOI] [PubMed] [Google Scholar]
- 75.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: a randomized, controlled trial. Medical Care. 2000;38:218–230. [DOI] [PubMed] [Google Scholar]
- 76.Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am J Med. 2000;108:20–27. [DOI] [PubMed] [Google Scholar]
- 77.Anderson RM, Fitzgerald JT, Funnell MM, et al. Evaluation of an activated patient diabetes education newsletter. Diabetes Educ. 1994;20:29–34. [DOI] [PubMed] [Google Scholar]
- 78.Cranor CW, Bunting BA, Christensen DB. The Asheville Project: long-term clinical and economic outcomes in a community pharmacy diabetes care program. J Am Pharm Assoc. 2003;43:173–184. [DOI] [PubMed] [Google Scholar]
- 79.Cranor CW, Christensen DB. The Asheville Project: short-term outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc. 2003;43:149–159. [DOI] [PubMed] [Google Scholar]
- 80.Reid L, Hatch J, Parrish T. Commentary: the role of a historically black university and the black church in community-based health initiatives: the Project DIRECT experience. J Public Health Manage Pract. 2003;November (suppl):S70–S73. [DOI] [PubMed]
- 81.Nasmith L, Cote B, Cox J, et al. The challenge of promoting integration: conceptualization, implementation, and assessment of a pilot care delivery model for patients with type 2 diabetes. Fam Med. 2004;36:40–50. [PubMed] [Google Scholar]
- 82.Dillinger TL, Jett SC, Macri MJ, Grivetti LE. Feast or famine? Supplemental food programs and their impacts on two American Indian communities in California. Int J Food Sci Nutr. 1999;50:173–187. [DOI] [PubMed] [Google Scholar]
- 83.Toobert DJ, Strycker LA, Glasgow RE, Barrera M, Bagdade JD. Enhancing support for health behavior change among women at risk for heart disease: the Mediterranean Lifestyle Trial. Health Educ Res. 2002; 17:574–585. [DOI] [PubMed] [Google Scholar]
- 84.Goldberg HI, Ralston JD, Hirsch IB, Hoath JI, Ahmed KI. Using an Internet comanagement module to improve the quality of chronic disease care. Jt Comm J Qual Saf. 2003;29:443–451. [DOI] [PubMed] [Google Scholar]
- 85.Zrebiec JF, Jacobson AM. What attracts patients with diabetes to an Internet support group? A 21-month longitudinal website study. Diabet Med. 2001; 18:154–158. [DOI] [PubMed] [Google Scholar]
- 86.Larsen DL, Cannon W, Towner S. Longitudinal assessment of a diabetes care management system in an integrated health network. J Managed Care Pharm. 2003;9:552–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Renders CM, Valk GD, de Sonnaville JJJ, et al. Quality of care for patients with type 2 diabetes mellitus—a long-term comparison of two quality improvement programmes in the Netherlands. Diabet Med. 2003;20:846–852. [DOI] [PubMed] [Google Scholar]
- 88.Laffell LM, Brackett J, Ho J, Anderson BJ. Changing the process of diabetes care improves metabolic outcomes and reduces hospitalizations. Qual Manag Health Care. 1998;6:53–62. [DOI] [PubMed] [Google Scholar]
- 89.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996; 74:511–544. [PubMed] [Google Scholar]
- 90.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness. Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 91.Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams. Ann Behav Med. 2002;24:80–87. [DOI] [PubMed] [Google Scholar]
- 92.Chin MH, Cook S, Drum ML, et al. Improving diabetes care in Midwest community health centers with the health disparities collaborative. Diabetes Care. 2004;27(1):2–8. [DOI] [PubMed] [Google Scholar]
- 93.Glasgow RE. Medical office-based interventions. In: Snoek F, Skinner C, eds. Psychology in Diabetes Care. 2nd ed. New York, NY: Wiley & Co. In press.
- 94.Hampson SE, Glasgow RE, Strycker L. Beliefs versus feelings: a comparison of personal models and depression for predicting multiple outcomes in diabetes. Br J Health Psychol. 2000;5:27–40. [Google Scholar]
- 95.Haire-Joshu D. Management of Diabetes Mellitus: Perspectives of Care Across the Lifespan. 2nd ed. St Louis, Mo: C. V. Mosby Co; 1996.
- 96.Locke EA, Saari LM, Shaw KN, Latham GP. Goal setting and task performance: 1969–1980. Psychol Bull. 1981;90:125–152. [Google Scholar]
- 97.Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: a 35-year odyssey. Am Psychol. 2002;57(9):705–717. [DOI] [PubMed] [Google Scholar]
- 98.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
- 99.Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26:597–604. [DOI] [PubMed] [Google Scholar]
- 100.Loro AD Jr, Fisher EB Jr, Levenkron J. Comparison of established and innovative procedures for weight loss. J Appl Behav Anal. 1979;12:141–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37:5–14. [DOI] [PubMed] [Google Scholar]
- 102.Williams GC, McGregor HA, Zeldman A, Freedman ZR, Elder D, Deci EL. Promoting glycemic control through diabetes self-management: evaluating a patient activation intervention. Patient Educ Couns. 2005;56:28–34. [DOI] [PubMed] [Google Scholar]
- 103.The Robert Wood Johnson Foundation and Center for the Advancement of Health. Essential elements of self-management interventions. December 2001. Available at: http://www.cfah.org/pdfs/Essential_Elements_Report.pdf. Accessed July 15, 2005.
- 104.Anderson RM. Educational principles and strategies. In: Funnell MM, Hunt C, Kulkarni K, Rubin RR, Yarborough P, eds. A Core Curriculum for Diabetes Educators. Chicago, Ill: American Association of Diabetes Educators; 1998:5–26.
- 105.Hill-Briggs F. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. Ann Behav Med. 2003;25(3):182–193. [DOI] [PubMed] [Google Scholar]
- 106.Houston CA, Haire-Joshu D. Application of health behavior models to promote behavior change. In: Haire-Joshu D, ed. Management of Diabetes Mellitus: Perspectives of Care Across the Lifespan. St Louis, Mo: C. V. Mosby Co; 1996:527–552.
- 107.D’Zurilla TJ, Nezu AM. Problem-Solving Therapy. 2nd ed. New York, NY: Springer; 1999.
- 108.Nezu AM, Nezu CM, Felgoise SH, et al. Project Genesis: assessing the efficacy of problem-solving therapy for distressed adult cancer patients. J Consult Clin Psychol. 2003;71:1036–1048. [DOI] [PubMed] [Google Scholar]
- 109.Lustman PJ, Griffith LS, Freedland KE, Kissel SS, Clouse RE. Cognitive behavior therapy for depression in type 2 diabetes mellitus: a randomized, controlled trial. Ann Intern Med. 1998;129(8):613–621. [DOI] [PubMed] [Google Scholar]
- 110.deGroot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001; 63:619–630. [DOI] [PubMed] [Google Scholar]
- 111.Lustman PJ, Freedland KE, Griffith LS, Clouse RE. Fluoxetine for depression in diabetes: a randomized double-blind placebo-controlled trial. Diabetes Care. 2000;23(5):618–623. [DOI] [PubMed] [Google Scholar]
- 112.Williams RB, Barefoot JC, Schneiderman N. Psychosocial risk factors for cardiovascular disease: more than one culprit at work. JAMA. 2003;290:2190–2192. [DOI] [PubMed] [Google Scholar]
- 113.Levenkron JC, Cohen JD, Mueller HS, Fisher EB Jr. Modifying the type A coronary-prone behavior pattern. J Consult Clin Psychol. 1983;51:192–204. [DOI] [PubMed] [Google Scholar]
- 114.Penedo FJ, Dahn JR, Molton I, et al. Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer. 2004;100:192–200. [DOI] [PubMed] [Google Scholar]
- 115.Bishop GD, Kaur D, Tan VLM, Chua YL, Liew SM, Mak KH. Effects of a psychosocial skills training workshop on psychophysiological and psychosocial risk in patients undergoing coronary artery bypass grafting. Am Heart J. In press. [DOI] [PubMed]
- 116.American Association of Diabetes Educators. Products: AADE7 self-care behaviors goal sheet. Available at: http://www.diabeteseducator.org/AADE7/goalsheet.html. Accessed June 10, 2005.
- 117.Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch HG. Telephone care as a substitute for routine clinic follow-up. JAMA. 1992;267(13): 1788–1793. [PubMed] [Google Scholar]
- 118.McKay HG, Feil E.G., Glasgow RE, Brown JE. Feasibility and use of an Internet support service for diabetes self-management. Diabetes Educ. 1998;24:174–179. [DOI] [PubMed] [Google Scholar]
- 119.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24:202–208. [DOI] [PubMed] [Google Scholar]
- 120.Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM. Telephone counseling for smoking cessation: rationales and meta-analytic review of evidence. Health Educ Res. 1996;11(2):243–257. [DOI] [PubMed] [Google Scholar]
- 121.Zhu SH, Stretch V, Balabanis M, Rosbrook B, Sadler G, Pierce JP. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol. 1996;64(1): 202–211. [DOI] [PubMed] [Google Scholar]
- 122.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19:11–20. [DOI] [PubMed] [Google Scholar]
- 123.Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care. 1997;20:254–257. [DOI] [PubMed] [Google Scholar]
- 124.Zuvekas A, Nolan L, Tumaylle C, Griffin L. Impact of community health workers on access, use of services, and patient knowledge and behavior. J Ambul Care Manage. 1999;22:33–44. [DOI] [PubMed] [Google Scholar]
- 125.Fisher EB. A behavioral-economic perspective on the influence of social support on cigarette smoking. In: Green L, Kagel JH, eds. Advances in Behavioral Economics. Norwood, NJ: Ablex; 1996:207–236.
- 126.Fisher EB Jr, La Greca AM, Greco P, Arfken C, Schneiderman N. Directive and nondirective support in diabetes management. Int J Behav Med. 1997;4:131–144. [DOI] [PubMed] [Google Scholar]
- 127.Fisher EB, Todora H, Heins J. Social support in nutrition counseling. On the Cutting Edge. 2003;24(4): 18–20. [Google Scholar]
- 128.Williams GC, Rodin GC, Ryan RM, Grolnick WS, Deci EL. Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychol. 1998;17:269–276. [DOI] [PubMed] [Google Scholar]
- 129.Beck A, Scott J, Willliams P, et al. A randomized trial of group outpatient visits for chronically ill older HMO members: the Cooperative Health Care Clinic. J Am Geriatr Soc. 1997;45(5):543–549. [DOI] [PubMed] [Google Scholar]
- 130.Trento M, Passera P, Borgo E, et al. A 5-year randomized controlled study of learning, problem solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care. 2004;27:670–675. [DOI] [PubMed] [Google Scholar]
- 131.Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24:995–1000. [DOI] [PubMed] [Google Scholar]
- 132.Glasgow RE, Eakin E.G., Fisher EB, Bacak SJ, Brownson RC. Physician advice and support for physical activity: results from a national survey. Am J Prev Med. 2001;21:189–196. [DOI] [PubMed] [Google Scholar]
- 133.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care. 2005;43(5):436–444. [DOI] [PubMed] [Google Scholar]
- 134.Haire-Joshu D, Nanney MS. Prevention of overweight and obesity in children: influences on the food environment. Diabetes Educ. 2002;28(3):415–423. [DOI] [PubMed] [Google Scholar]
- 135.Brownell KD, Horgen KB. Food Fight: The Inside Story of the Food Industry, America’s Obesity Crisis, and What We Can Do About It. New York, NY: McGraw-Hill; 2004.
- 136.Fichtenberg CM, Glantz SA. Association of the California Tobacco Control Program with declines in cigarette consumption and mortality from heart disease. N Engl J Med. 2000;343(24):1772–1777. [DOI] [PubMed] [Google Scholar]
- 137.Siegel M. The effectiveness of state-level tobacco control interventions: a review of program implementation and behavioral outcomes. Annu Rev Public Health. 2002;23:45–71. [DOI] [PubMed] [Google Scholar]
- 138.Brownson RC, Housemann RA, Brown DR, et al. Promoting physical activity in rural communities: walking trail access, use, and effects. Am J Prev Med. 2000; 18:235–241. [DOI] [PubMed] [Google Scholar]
- 139.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity: a systematic review. Am J Prev Med. 2002;22:73–107. [DOI] [PubMed] [Google Scholar]
- 140.Matson-Koffman DM, Brownstein JN, Neiner JA, Greaney ML. A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: what works? Am J Health Promot. 2005;19:167–193. [DOI] [PubMed] [Google Scholar]
- 141.Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27:63–80. [DOI] [PubMed] [Google Scholar]
- 142.Glasgow RE, Orleans CT, Wagner EH, Curry SJ, Solberg LI. Does the Chronic Care Model serve also as a template for improving prevention? Milbank Q. 2001; 79(4):579–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cooksey C, Lanza AP. Examining diabetes health benefits in health plans of large employers. J Public Health Manage Pract. 2003;November (suppl): S30–S35. [DOI] [PubMed]
- 144.Janes GR. Ambulatory medical care for diabetes. In: Diabetes in America. 2nd ed. Bethesda, Md: National Diabetes Data Group, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 1995:541–552. NIH publication 95–1468.
- 145.Prochaska JO, Redding CA, Evers KE. The Trans-theoretical Model and stages of change. In: Glanz K, Lewis FM, Rimer B, eds. Health Behavior and Health Education: Theory, Research, and Practice. 3rd ed. San Francisco, Calif: Jossey-Bass/Pfeiffer; 2002:99–120.
- 146.DiClemente CC, Velasquez MM. Motivational interviewing and the stages of change. In: Miller WR, Rollnick S, eds. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002:201–216.
- 147.Nord WR, Tucker S. Implementing Routine and Radical Innovations. Lexington, Mass: D. C. Heath & Co; 1987.
- 148.Glynn T, Manley M. How to Help Your Patients Stop Smoking: A National Cancer Institute Manual for Physicians. Bethesda, Md: National Cancer Institute; 1989. NIH publication 89–3064.
- 149.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–284. [DOI] [PubMed] [Google Scholar]
- 150.Glasgow RE, Goldstein M, Ockene J, Pronk JP. Translating what we have learned into practice: principles and hypotheses for addressing multiple behaviors in primary care. Am J Prev Med. 2004;27:88–101. [DOI] [PubMed] [Google Scholar]
- 151.Stokols D, Grzywacz JG, McMahan S, Phillips K. Increasing the health promotive capacity of human environments. Am J Health Promot. 2003;18:4–13. [DOI] [PubMed] [Google Scholar]
- 152.Pearce N, Davey-Smith G. Is social capital the key to inequalities in health? Am J Public Health. 2003;93:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]