Abstract
Objectives. We examined trends in obesity and arthritis prevalence among the “baby boom” (born 1946–1965) and “silent” (born 1926–1945) generations.
Methods. We conducted birth cohort analyses using successive waves of the National Health and Nutrition Examination Survey (1971–2002).
Results. Obesity rates increased markedly, beginning earlier in life with each successive birth cohort. When the members of the silent generation were aged 35–44 years, 14%–18% were obese. At comparable ages, 28%–32% of the youngest baby boomers were obese. Differences in arthritis prevalence were not evident across birth cohorts. However, the relative risk of arthritis because of obesity increased over time; consequently, the percentage of arthritis cases attributable to obesity increased from 3% to 18% between 1971 and 2002.
Conclusions. Our results showed that members of the baby boom generation were more obese, and became so at younger ages than their predecessors. Although differences in arthritis prevalence are not yet evident, findings suggest that obesity has contributed to more cases of arthritis in recent years than in previous decades.
The aging of the “baby boom” generation—that is, individuals born from 1946 through 1964—in the United States has profound societal implications because of the size of this generation relative to previous and subsequent ones.1–3 Understanding the effects on population disability of this progressing demographic shift is essential to anticipating health care needs and developing appropriate services for the new generation of elderly people. Although apparent declines in disability rates in the older population in recent decades have generated great optimism,4–6 it remains uncertain whether aging baby boomers will continue this trend. Several factors inspire hope for continued improvement while others raise concerns, especially regarding possible increases in disability from arthritis and chronic joint symptoms caused by widespread adoption of unhealthy lifestyle practices.
Trends in problems associated with sedentary behavior and obesity are worrisome, especially among baby boomers.7,8 Access to better nutrition has improved, but at the same time consumption of high-fat, high-carbohydrate foods has increased. In recent years, rates of obesity have risen dramatically, although physical activity rates have remained unchanged.8 Among children, rates of sedentary behavior are increasing.8 Moreover, substantial differences exist in prevalence of obesity, especially among women of differing racial/ethnic groups. More than half of non-Hispanic Black women aged 40 years and older were obese in 1999–2000, as compared with approximately one third of non-Hispanic White women in the same age group; 40%–50% of Mexican American women were obese.7
In the coming decades, such lifestyle factors are likely to contribute to large increases in rates of arthritis, as well as increases in diabetes and cardiovascular disease. Recent projections show that the aging of baby boomers will result in a doubling of the numbers of persons aged 65 years or older with arthritis or chronic joint symptoms by 2030, when the last of the baby boom generation will turn 65 years old.2 However, these calculations assume stability in arthritis prevalence and probably underestimate an impending surge in prevalence among more obese baby boomers. At the population level, disability and increased use of health services have accompanied higher rates of arthritis.9
We used US census data to examine changes in the racial/ethnic composition of the baby boom generation and its predecessor, commonly referred to as the “silent generation” (individuals born between 1926 and 1945). Also, to assess trends in prevalence of obesity, overweight, and arthritis among baby boomers and their predecessors, we analyzed data from successive waves of the National Health and Nutrition Examination Survey (NHANES) conducted between 1971 and 2002. In addition, we studied the relationship between obesity and arthritis among these birth cohorts.
METHODS
We analyzed publicly available data from the US Bureau of the Census and the National Center for Health Statistics. We explored changes in the racial/ethnic distribution of the baby boom and silent generations by examining data from the 1980 and 2000 decennial censuses. The Census Bureau first collected information on Hispanic ethnicity in 1980; thus, we used these data to examine trends over the past 20 years. We analyzed 4 waves of NHANES data: data from waves I through III and recently available data from the NHANES conducted between 1999 and 2002 (“NHANES 1999 through 2002”).
NHANES Data on Overweight and Arthritis
Under the auspices of the National Center of Health Statistics, periodic NHANES waves over several decades have collected detailed health information on nationally representative samples of US residents across age groups. NHANES involves a complex multistage probability cluster sampling design and sophisticated weighting approaches designed to yield national prevalence estimates. In NHANES I, conducted from 1971 to 1974, children and adults underwent extensive examinations, and medical histories were obtained from 18836 individuals aged 12–74 years. NHANES II was conducted from 1976 to 1980, and medical histories were obtained from 18447 individuals aged 12–74 years. In NHANES III, conducted in 2 phases of 3 years each between 1988 and 1994, 20050 individuals aged 17 years or older were interviewed.
Most NHANES assessments were performed in mobile examination centers (large trailers equipped with various testing technologies); very few occurred in participants’ homes. The most recent wave of NHANES began in 1999 and will continue in 2-year cycles. At the time of our analyses, data were available from interviews conducted in 1999 through 2002 with 21004 individuals, including interviews of 10291 adults aged 20 years or older who provided medical histories.
During each wave of NHANES, study examiners measured weight and height. We calculated body mass index (BMI; weight in kilograms divided by height in meters squared) and used standard cut points to classify individuals as overweight (BMI≥ 25.0–29.9 kg/m2) and obese (BMI ≥ 30 kg/m2). During the interviews conducted in each NHANES wave, participants were asked whether a doctor had ever told them they had arthritis. Substantial across-wave differences in clinical evaluations of arthritis (e.g., X-rays and physical examinations) precluded our use of data other than self-reports to determine arthritis rates. For example, in NHANES III, hand and knee X-rays, physician joint examinations, and physical function tests were performed only with individuals aged 60 years or older. Despite the limitations of self-reported arthritis information, the interview question used to assess physician-diagnosed arthritis remained essentially the same over the 4 NHANES waves analyzed here.
Birth Cohort Analyses
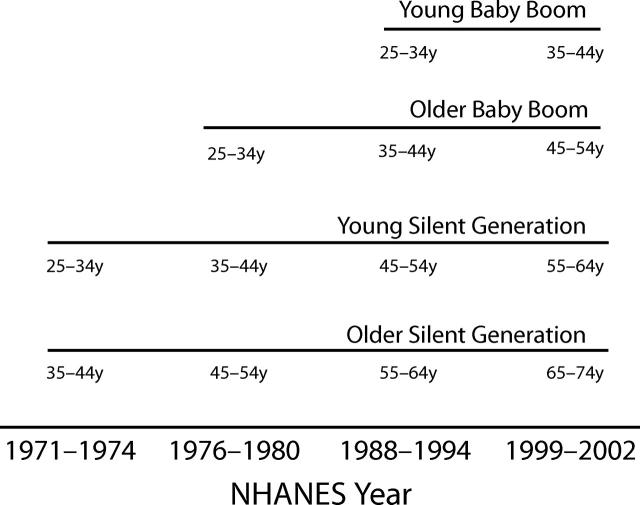
To illustrate trends in birth cohorts, we divided the baby boom and silent generations into 4 birth cohorts, each spanning 10 years (1926–1935, 1936–1945, 1946–1955, and 1956–1965). Figure 1 ▶ shows the schema we used to conduct analyses and portray trends in prevalence of obesity and arthritis within each birth cohort across the 1971–2002 NHANES waves. For example, we followed the oldest age group (i.e., those born between 1926 and 1935) through 4 waves of NHANES data. This birth cohort, the “older silent generation,” was 38–47 years of age at the time of the first NHANES and 65–74 years of age during NHANES 1999–2002. During these same time periods, members of the next birth cohort, the “young silent generation,” born between 1936 and 1945, were 28–37 and 55–64 years of age, respectively.
FIGURE 1—
Birth cohort analysis schema showing ages of the birth cohorts at the time of each wave of the National Health and Nutrition Examination Survey (NHANES).
In the case of the “older baby boom generation,” born during 1946–1955, only 3 waves of NHANES occurred during which all members of this cohort were older than 21 years. Thus, we did not use the data from NHANES I for this generation, because they were too young at the time of that survey. The youngest cohort, the “young baby boom generation,” born during 1956–1965, was older than 21 years only during the 2 most recent waves, NHANES III and NHANES 1999–2002.
The NHANES data sets contained information on respondents’ age in years but not their birth date. In the case of all waves, we used age at interview as age at the midpoint of the survey period. NHANES III was conducted over 6 years (1988–1994) in 2 phases of 3 years each, the longest survey period of the 4 waves; this data set included information about whether participants had completed an examination during the first or second phase. Thus, rather than assuming that all participants’ ages were at the midpoint of the 6-year interval, we added 1 year to the age of phase 1 participants in NHANES III, subtracted 1 year from the age of phase 2 participants, and assumed that participants’ age was at the midpoint of the 6-year survey period.
Statistical Analysis
We used SAS for Windows (version 8.01; SAS Institute, Cary, NC) for all analyses and SAS-callable SUDAAN (version 8; Research Triangle Institute, Research Triangle Park, NC) for analyses accounting for the cluster design and the survey’s complex multistage sampling. Appropriate interview and examination sampling weights were applied in all prevalence estimations. We derived adjusted odds ratios (ORs) and 95% confidence intervals from multivariate logistic regression models, using SUDAAN; these models accounted for weighting and the complex sampling design via the Taylor series method. Because of the high prevalence of arthritis in the population, we converted odds ratios for arthritis to relative risk approximations, using the method described by Zhang and Yu.10
To examine changes over time in the effects of obesity on arthritis risk among individuals aged 46–74 years, we calculated the population-attributable risk percents (PAR%), which is a measure of the percentage of a population with a condition that would be prevented if a risk factor were eliminated. We limited the analysis to this age group, because persons aged 46 years and older represented the segment of the population exhibiting the greatest increases in regard to arthritis incidence and prevalence. The upper age limit was set to 74, because individuals older than 74 years were not eligible to participate in NHANES I or II.
We used the following formula in estimating PAR%11: [P(OR − 1)]/[P(OR − 1) + 1] × 100, where P is the (age-adjusted, weighted) proportion of the population with exposure to the risk factor; odds ratios were derived from multivariate logistic regression models with self-reported arthritis as the dependent variable and the 3-category BMI variable as the independent variable, adjusted for age, gender, race/ethnicity, and education. We calculated PAR%, using both odds ratio and relative risk approximations; we present relative risks, which are more conservative estimates. Results were not materially different between the 2 approaches.
RESULTS
According to the US decennial census, the percentage of racial/ethnic minorities in the silent generation cohort increased in the 20 years between 1980 and 2000. In 1980, 18.3% of the cohort was composed of minority individuals, and this percentage grew to 20.1% in 2000. By contrast, 22.2% of the baby boom generation was composed of minority individuals in 1980, increasing to 27.7% by 2000.
Age-specific prevalence of obesity increased markedly among both men and women in each of the 10-year birth cohorts during the 3 decades beginning in 1971 (Figure 2 ▶). With each new birth cohort, proportions of members who were obese rose dramatically at younger ages. Specifically, members of the baby boom generation exhibited a substantially higher prevalence of obesity, and became obese at younger ages, than their predecessors in the silent generation; the difference was most evident in the 35- to 45-year age range. This was the only age group for which NHANES data were available for all 4 birth cohorts (Figure 2 ▶). In the 35- to 45-year age group, the prevalence of obesity was approximately twice as high among the youngest baby boomers (28%–32%) as among their counterparts in the silent generation (14%–18%). In the case of both women and men, obesity prevalence among young baby boomers in the 25- to 44-year age group was comparable to that among the silent generation cohorts when they were 10–20 years older.
FIGURE 2—
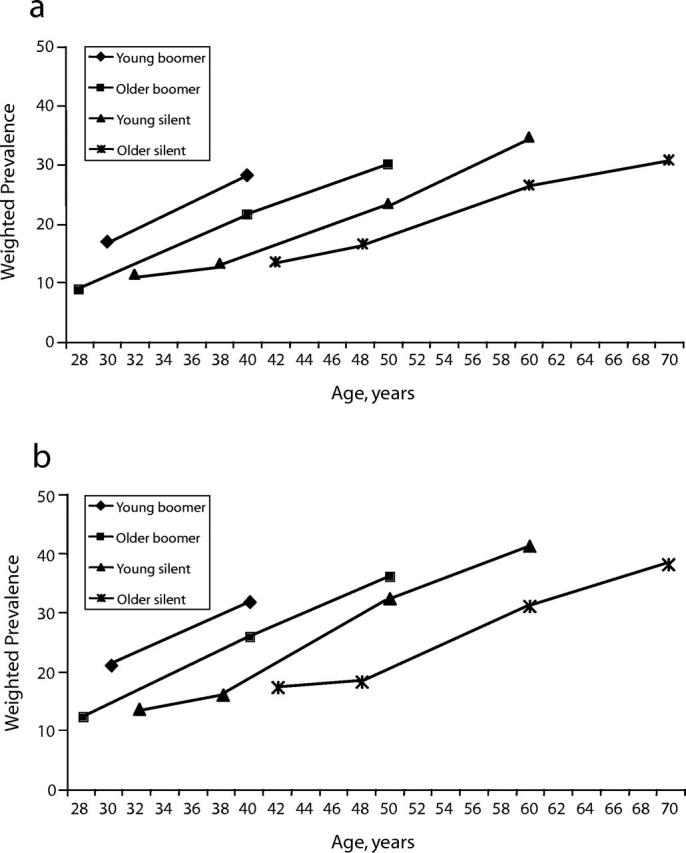
Prevalence of obesity (body mass index of ≥ 30) among men (a) and women (b), according to age, within 10-year birth cohorts: National Health and Nutrition Examination Survey, 1971–2002.
In more recent years (indicated by the uppermost 2 points on each birth cohort line in panels A and B of Figure 2 ▶), men and women in both the baby boom generation and the silent generation exhibited obesity prevalences ranging from 22% to 42%. In earlier waves of NHANES, when members of the oldest birth cohort were younger than 55 years, obesity prevalence did not exceed 20% among men or women in any of the cohorts.
The prevalence of arthritis rose with age in all 4 birth cohorts, with few differences observed across groups (Figure 3 ▶). Because obesity is a known risk factor for arthritis, this somewhat unexpected finding prompted us to more closely examine the BMI distribution among participants with and without self-reported arthritis in the group aged 55–64 years (arthritis prevalence increases substantially during this decade). We found that although the prevalence of obesity increased over time, a greater proportion of individuals with than without arthritis were obese, most notably in recent years (data not shown). These differences were more evident among men than among women.
FIGURE 3—
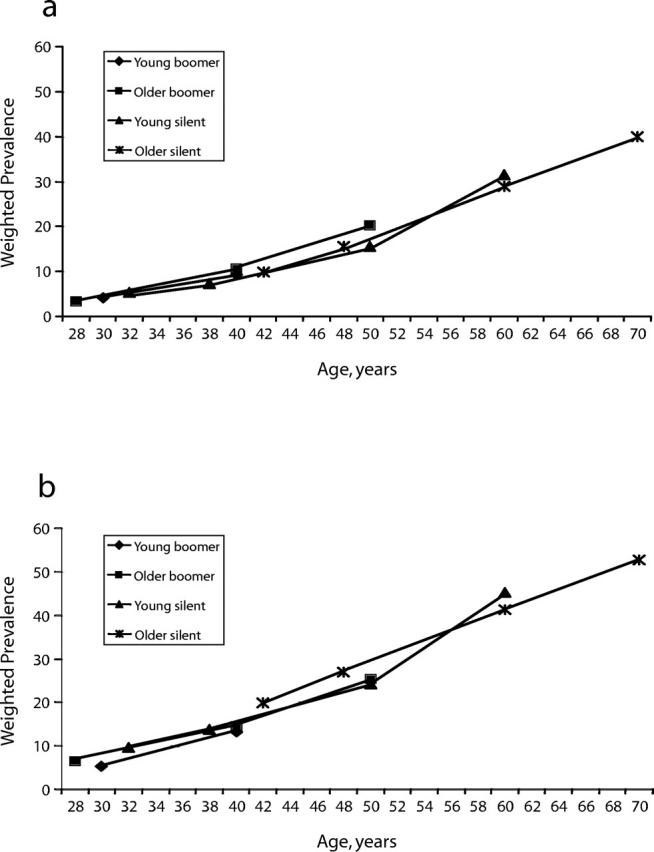
Prevalence of self-reported arthritis among men (a) and women (b), according to age, within 10-year birth cohorts: National Health and Nutrition Examination Survey, 1971–2002.
Conversely, the percentage of individuals with arthritis who were not overweight decreased substantially across time in the 55- to 64-year age group, again more among men than among women. In an additional analysis (data not shown), we found that average within-category BMIs increased over time; for example, among obese individuals aged 46 to 74 years, average BMIs were 33.8 kg/m2 in NHANES I and 35.5 kg/m2 in NHANES 1999–2002, indicating a general shift in the BMI distribution over the 3 decades covered.
The association between obesity and arthritis was of a greater magnitude across waves of the NHANES among adults aged 46–74 years (Table 1 ▶). In the first NHANES, after adjustment for age, gender, race/ ethnicity, and education, individuals who were obese were approximately 20% more likely than their peers who were not overweight to report physician-diagnosed arthritis. In NHANES 1999–2002, obese individuals were more than 60% as likely to report having arthritis as people who were not overweight. We estimated the influence of obesity on arthritis prevalence in terms of opportunities for prevention; our estimates showed that in 1971 through 1974, 3.2% of arthritis cases could have been prevented had none of the members of the population been obese. In 1999–2002, 18.1% of arthritis cases could have been prevented in the absence of obesity (Table 1 ▶).
TABLE 1—
Relationships Between Overweight and Self-Reported Arthritis Among Individuals Aged 46–75 Years and Effects of Overweight on Prevalence of Arthritis: National Health and Nutrition Examination Survey (NHANES), 1971–2002
| NHANES I (1971–1974) | NHANES II (1976–1980) | NHANES III (1988–1994) | NHANES 1999–2002 | |||||
| RR (95% CI) | PAR% | RR (95% CI) | PAR% | RR (95% CI) | PAR% | RR (95% CI) | PAR% | |
| Nonoverweight (BMI ≤ 25) | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Overweight (BMI 25–29) | 1.13 (1.00, 1.26) | 4.6 | 0.97 (0.88, 1.06) | . . . | 1.09 (0.98, 1.20) | . . . | 1.24 (1.07, 1.45) | 7.8 |
| Obese (BMI ≥ 30) | 1.19 (1.06, 1.34) | 3.2 | 1.33 (1.16, 1.49) | 5.6 | 1.55 (1.40, 1.69) | 13.3 | 1.61 (1.41, 1.82) | 18.1 |
Note. Odds ratios were derived from logistic regression models adjusted for age, gender, race/ethnicity, and education and accounting for complex sampling design effects. See text for the equation used in calculating population-attributable risk percentage (PAR%). BMI = body mass index; CI = confidence interval.
DISCUSSION
Our findings reveal 2 major obesity trends that raise serious concerns about the future physical functioning of the aging baby boom generation in the United States. First, baby boomers are more obese, and became so at younger ages than their predecessors, the members of the silent generation. Baby boomers are spending more of their adult years in an obese state than their predecessors, many of whom became obese later in life. Obesity prevalence was approximately twice as high among baby boomers in their 30s and 40s as among older members of the silent generation when they were in their 30s and 40s. Second, such results reflect a broad trend affecting all 4 birth cohorts: substantial increases in obesity prevalence in recent decades with no evidence of a leveling off, even among individuals of older ages.
Previous research has reported on the dramatic increases in prevalence of overweight and obesity and its consequences over the past few decades.7,12,13 Recently, concern has shifted to even younger individuals, with worrisome findings showing dramatic increases in obesity among children.8 However, few studies have examined the wide-ranging implications of these changes for the aging baby boom generation, which will swell the proportion of older adults in the United States population over the next 3 decades. The impact of obesity on life expectancy is one major concern. A recent analysis of the 40-year follow-up of the Framingham Study showed that obese 40-year-old nonsmokers lost 6–7 years of life expectancy relative to their normal-weight peers.14 Others have reported similar results with national data and shorter follow-up periods.15
Perhaps as important as the mortality risk is the impact of obesity on the prevalence of chronic conditions and disability among baby boomers. Obesity is strongly associated with many chronic conditions and health risks.16 In elderly people, high BMIs predict loss of mobility and disability.17,18 Given the rise in obesity prevalence and the risk of arthritis because of obesity,19 we expected the population prevalence of arthritis to mirror obesity trends and were surprised that the prevalence of arthritis did not appear to differ between the baby boom and silent generation cohorts.
One possible explanation for these surprising results is that physicians may have changed the way they diagnose arthritis during the 3 decades under study. In the decade before the first NHANES, diagnostic criteria for osteoarthritis and other rheumatological diseases were less well defined than in recent years,20 which may have resulted in more frequent diagnoses of arthritis in middle-aged and elderly patients who presented with joint problems in years past. In the 1960s, national arthritis prevalence estimates, which were based on radiographic tests of patients’ hands and feet, were substantially higher than current estimates.20 This possible diagnostic bias may have masked a rising trend in arthritis over time.
Other factors may explain the arthritis findings as well. For example, the relative importance of specific arthritis risk factors may have changed over time. Our population-attributable risk analyses indicated that obesity was not as important a risk factor for arthritis in the 1970s and 1980s as it has been in the most recent decade, yet the prevalence of arthritis was as high in these earlier decades of relatively low obesity rates. These findings suggest that non–weight-related factors may have had a stronger influence. With labor market shifts away from the manufacturing and farm sectors, occupational risks for arthritis, particularly among men,21 may have become less of a factor in the baby boom generation. Findings from the first NHANES suggested that occupational factors might have been more important than obesity as a contributor to arthritis prevalence in the early 1970s.22 Similar research is needed to provide a more complete understanding of the role of occupational factors in arthritis in more recent decades.
Our analyses examining the BMI distribution among individuals with and without self-reported physician-diagnosed arthritis illustrated the birth cohort differences in regard to the relationship between obesity and arthritis. A greater proportion of men and women with arthritis were obese in the 2 most recent NHANES waves than in the earlier waves. In addition, we found an increase in the magnitude of relative risk of obesity being a cause of arthritis in the most recent waves. It is implausible that the physiological association between obesity and arthritis has changed in recent decades. Instead, the findings may be a reflection of the overall shift in the weight distribution such that, even within BMI categories, average BMIs were higher in more recent years than in the early NHANES waves.
Whether the increases observed in obesity prevalence will ultimately lead to increases in arthritis prevalence among the baby boom generation relative to the silent generation remains unclear. However, our findings suggest that obesity will continue to be an important risk factor for arthritis among aging baby boomers.
Previous research has shown age trends over the past several decades in terms of rising population prevalence of obesity.7 However, our findings reflect profound cultural changes leading to high rates of obesity that progressed rapidly across generations. Obesity has increasingly become a problem of the young, and this shift will probably influence baby boomers’ elderly years. Arthritis is only one of many obesity-related chronic conditions that could consume considerable health care resources, generate wide-ranging societal costs, and reduce quality of life. Both obesity and arthritis contribute to disability and are especially limiting as comorbid conditions.23,24 With the aging of the heavier baby boom generation, will we see a halt in or reversal of the trend toward decreasing disability that has been observed in the older population in the past decade?4–6 The looming problem of disability among baby boomers is yet another reason for designing and implementing aggressive public health strategies to reduce obesity.
Although questions may arise about our use of a self-reported measure of physician-diagnosed arthritis, misconceptions exist about the relevance of more “objective” measures of disease ascertainment, such as radiographic evidence of arthritis, in studies of disability risk. Substantial discordance exists between such radiographic evidence and complaints of musculoskeletal pain.25,26 In NHANES I, only 47% of individuals whose knee radiographs showed arthritic changes ranging from minimal to severe reported having knee pain, and, alternatively, only 15% of those reporting knee pain had radiographic evidence of knee osteoarthritis.25 In a population-based cohort of elderly North Carolina residents, knee pain, rather than radiographic evidence of disease, was found to be the strongest independent predictor of disability.27
Self-report measures may capture arthritis symptoms better than they capture radiographic evidence of disease, but these symptoms, specifically musculoskeletal pain, are key risk factors for disability among older individuals.27 Many elderly people endure chronic pain under insufficient treatment28 and suffer disabling consequences. In the absence of a cure for arthritis, we must develop a knowledge base for better symptom management with the goal of preventing disability.
This study involved a series of cross-sectional surveys; thus, we were unable to conduct statistical tests comparing prevalence or risk estimates across the birth cohorts. Also, the population was dynamic across the NHANES waves, as evidenced by the increasing proportions of minority respondents, particularly among baby boomers. Some of the increases in rates of overweight and obesity could be caused by the changing composition of the population rather than just weight increases among the stable sectors of the population. In addition, the trend toward a stronger association between obesity and arthritis over time may relate to an ascertainment bias resulting from the fact that obese patients visit physicians more frequently than do nonobese patients and subsequently are more likely to be diagnosed with arthritis.
We used the formula developed by Kleinbaum et al.11 PAR%. This formula assumes that disease does not affect risk exposure and that exposure does not affect duration of disease. However, because we used cross-sectional data, we cannot assume that arthritis had no effect on degree of obesity. Also, obesity may influence duration of arthritis. Hence, we may have overestimated population-attributable risk percentages, although we attempted to minimize this potential bias through our use of more conservative estimates based on relative risks rather than odds ratios. Nonetheless, the 2 methods lead to essentially the same conclusions.
In our multivariate analysis, we could not adjust for certain risk factors for arthritis because of differences in the information collected across NHANES waves. For example, physical activity items changed substantially with each wave of the survey. Other known risk factors, such as occupational hazards, are challenging to study because of variations in risk exposures within the same occupational class. A recent study showed that occupational risks are related to specific activities such as squatting and heavy lifting rather than to occupational categories.29 In other words, the results of this study revealed that in some cases, different individuals who report the same occupation also report different sets of job-related hazardous activities.29
In NHANES I, when we examined arthritis prevalence according to occupational group (e.g., blue collar vs other), we found that the prevalence was slightly higher in the non–blue-collar category in both women and men (data not shown). Although in-depth analyses of occupational risks were beyond the scope of this study, repetitive activities—whether occupation, sport, or leisure related—warrant further study in regard to their influence on arthritis prevalence across birth cohorts.
The first members of the baby boom generation will reach the age of 65 years in 2011. Arthritis stands out as the most common chronic condition affecting the older population and the condition contributing the greatest burden of disability in this group.30,31 If obesity prevalence continues to climb as the baby boom generation ages, the expected increases in musculoskeletal conditions and disability will place an unprecedented burden on both baby boomers and society as a whole. Further research is needed to determine the ongoing effects of obesity on the prevalence of chronic disease among aging baby boomers. Public health initiatives will continue to play an important role in the prevention and management of obesity and arthritis among the baby boom generation.
Acknowledgments
Funding for this research was provided by the Arthritis Foundation and the National Bureau of Economics Research, along with the National Institute on Aging and the Lasker Foundation.
We thank Mary Beth Hamel, MD, for her valuable contribution.
Human Participant Protection No protocol approval was needed for this study.
Peer Reviewed
Contributors S. G. Leveille and L. I. Iezzoni conceptualized the study and the analytic plan, S. G. Leveille conducted the data analysis and wrote the article, C. C. Wee and L. Iezzoni contributed to interpretation of the results and to the writing of the article.
References
- 1.Day J. Population Projections of the United States, by Age, Sex, Race, and Hispanic Origin: 1993 to 2050. Washington, DC: US Bureau of the Census; 1993.
- 2.Centers for Disease Control and Prevention. Public health and aging: projected prevalence of self-reported arthritis or chronic joint symptoms among persons aged > 65 years—United States, 2005–2030. MMWR Morb Mortal Wkly Rep. 2003;52:489–491. [PubMed] [Google Scholar]
- 3.Kinsella K, Velkoff V. An Aging World: 2001. Washington, DC: US Bureau of the Census; 2001.
- 4.Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002; 288:3137–3146. [DOI] [PubMed] [Google Scholar]
- 5.Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Proc Natl Acad Sci USA. 1997;94: 2593–2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manton KG, Gu X. Changes in the prevalence of chronic disability in the United States black and non-black population above age 65 from 1982 to 1999. Proc Natl Acad Sci USA. 2001;98:6354–6359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. [DOI] [PubMed] [Google Scholar]
- 8.Manson JE, Skerrett PJ, Greenland P, VanItallie TB. The escalating pandemics of obesity and sedentary lifestyle: a call to action for clinicians. Arch Intern Med. 2004;164:249–258. [DOI] [PubMed] [Google Scholar]
- 9.Dunlop DD, Manheim LM, Song J, Chang RW. Health care utilization among older adults with arthritis. Arthritis Rheum. 2003;49:164–171. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. [DOI] [PubMed] [Google Scholar]
- 11.Kleinbaum D, Kupper L, Morgenstern H. Epidemiologic Research: Principles and Quantitative Methods. New York, NY: Van Nostrand Reinhold; 1982.
- 12.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998;22:39–47. [DOI] [PubMed] [Google Scholar]
- 13.Flegal KM, Williamson DF, Pamuk ER, Rosenberg HM. Estimating deaths attributable to obesity in the United States. Am J Public Health. 2004;94: 1486–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. [DOI] [PubMed] [Google Scholar]
- 15.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost because of obesity. JAMA. 2003;289:187–193. [DOI] [PubMed] [Google Scholar]
- 16.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. [DOI] [PubMed] [Google Scholar]
- 17.Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469. [DOI] [PubMed] [Google Scholar]
- 18.LaCroix AZ, Guralnik JM, Berkman LF, Wallace RB, Satterfield S. Maintaining mobility in late life: II. Smoking, alcohol consumption, physical activity, and body mass index. Am J Epidemiol. 1993;137: 858–869. [DOI] [PubMed] [Google Scholar]
- 19.Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635–646. [DOI] [PubMed] [Google Scholar]
- 20.Roberts J, Burch TA. Osteoarthritis prevalence in adults by age, sex, race, and geographic area. Vital Health Stat 1. 1966;15:1–27. [PubMed] [Google Scholar]
- 21.Kutscher RE. Historical trends, 1950–92, and current uncertainties. Monthly Labor Rev. November 1993:3–10.
- 22.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first National Health and Nutrition Examination Survey (NHANES I): evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988;128: 179–189. [DOI] [PubMed] [Google Scholar]
- 23.Jordan JM, Luta G, Renner JB, et al. Self-reported functional status in osteoarthritis of the knee in a rural southern community: the role of sociodemographic factors, obesity, and knee pain. Arthritis Care Res. 1996;9: 273–278. [DOI] [PubMed] [Google Scholar]
- 24.Ettinger WH, Davis MA, Neuhaus JM, Mallon KP. Long-term physical functioning in persons with knee osteoarthritis from NHANES, I: effects of comorbid medical conditions. J Clin Epidemiol. 1994;47: 809–815. [DOI] [PubMed] [Google Scholar]
- 25.Hochberg MC, Lawrence RC, Everett DF, Cornoni-Huntley J. Epidemiologic associations of pain in osteoarthritis of the knee: data from the National Health and Nutrition Examination Survey and the National Health and Nutrition Examination–I Epidemiologic Follow-up Survey. Semin Arthritis Rheum. 1989; 18(suppl 2):4–9. [DOI] [PubMed] [Google Scholar]
- 26.Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000; 27:1513–1517. [PubMed] [Google Scholar]
- 27.Jordan J, Luta G, Renner J, Dragomir A, Hochberg M, Fryer J. Knee pain and knee osteoarthritis severity in self-reported task specific disability: the Johnston County Osteoarthritis Project. J Rheumatol. 1997;24: 1344–1349. [PubMed] [Google Scholar]
- 28.Pahor M, Guralnik JM, Wan JY, et al. Lower body osteoarticular pain and dose of analgesic medications in older disabled women: the Women’s Health and Aging Study. Am J Public Health. 1999;89:930–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coggon D, Croft P, Kellingray S, Barrett D, McLaren M, Cooper C. Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum. 2000; 43:1443–1449. [DOI] [PubMed] [Google Scholar]
- 30.Kramarow E, Lentzer H, Rooks R, Weeks J, Saydah S. Health and Aging Chartbook. Hyattsville, Md: National Center for Health Statistics; 1999.
- 31.Boult C, Altmann M, Gilbertson D, Yu C, Kane RL. Decreasing disability in the 21st century: the future effects of controlling six fatal and nonfatal conditions. Am J Public Health. 1996;86:1388–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]