Abstract
Objectives. We explored the economic implications of conduct disorder (CD) among adolescents in 4 poor communities in the United States. We examined a range of expenditures related to this disorder across multiple public sectors, including mental health, general health, school, and juvenile justice.
Methods. We used self- and parental-report data to estimate expenditures during a 7-year period in late adolescence of a sample of youths. We contrasted expenditures for youths with CD and youths with oppositional defiant disorder, elevated symptoms (no CD diagnosis), and all others. Diagnosis was determined with a structured assessment.
Results. Additional public costs per child related to CD exceeded $70000 over a 7-year period.
Conclusions. Public expenditures on youths with CD are substantially larger than for youths with closely related conditions, reflecting the importance of prevention and early treatment for the disorder.
The high social costs of mental disorder and disease among adults are well documented. For example, in 1990, the costs of depression alone exceeded $43 billion in direct and indirect costs.1 These costs are realized in the health and specialty mental health sector and extend into the workplace and beyond.
By contrast, relatively little is known about costs of emotional and behavioral problems among children and youths. Much of the available research focuses on attention-related disorders and is limited to related health expenditures or education costs.2–6 The economic costs of other mental disorders, such as conduct disorder (CD) and oppositional defiant disorder, have received relatively little attention. This research gap is particularly striking in light of the link between these disorders and costly behaviors, such as delinquency. For example, CD, or “a repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated,”7 has been linked with criminal activities, illegal substance use and abuse, and problems associated with early sexual debut, such as unwanted pregnancies and sexually transmitted diseases.8,9 To be diagnosed with CD, a youth must display at least 3 criteria from a list of criteria (listed in The Diagnostic and Statistical Manual of Mental Disorders), which includes behaviors such as bullying, threatening, or intimidating others; being truant from school often; and frequently lying to get something or avoid obligations.
The resulting costs to society are potentially enormous and extend over many years. Particularly salient to policymakers are the costs taxpayers incur in the short term. Those costs stem from the youths’ involvement in a variety of child-serving sectors, such as juvenile justice, child welfare, special education, and mental health services. For example, in a sample of children served in community mental health centers across the country, conduct-related diagnoses were the most common. Expenditures on services for these children can be quite large, totaling $13000 or more per child during a 6-month period.10
We used data from the Fast Track study—a longitudinal study of youths residing in poor neighborhoods in 4 communities—to examine the public costs of early conduct problems. The Fast Track study provided the data on which our analyses were based. Those data provided information on system involvement only, and we supplemented that information with data on the costs of those services. We examined the effect of CD on public costs. Finally, we considered the implications of these expenditures and the implications for prevention research.
METHODS
The Fast Track Study
The data for our analyses were collected as part of the Fast Track project, a multicohort, multisite longitudinal study of 1191 children who were at risk for emotional/behavioral problems.11–13 The Fast Track project included an intervention targeted to children identified in kindergarten as “at risk” for such long-term problems; the individuals receiving such treatment are not included here. Rather, our focus was on 664 subjects: (1) children who were screened into the high-risk comparison group (n = 396) and (2) children not identified as being at risk but recruited as part of a “normative” sample (n = 268). When analyzed with probability weights, the combination of these 2 groups was representative of children from low–socioeconomic status neighborhoods in the 4 sites.
The Fast Track project was designed to answer 2 sets of questions. The first involved whether and for whom the intervention worked. The second set of questions involved normative development in these poor neighborhoods. Our analyses here fall into this second category.
The project relied on an array of sources for information on participating children and their families. Both the youths and their primary caregiver were present at in-person interviews. Information also was collected from school and court records and from the youths’ teachers. Recruitment for Fast Track began in 1990 and continued for 3 years. The annual interviews began in the summer after kindergarten and are ongoing.
Three of the Fast Track sites were urban: Durham, NC, Nashville, Tenn, and Seattle, Wash. The racial makeup across these 3 sites was 49% African American. The remaining 51% were nearly all White (48%) with a small number of Latinos and Asians (3%). The fourth site was in rural Pennsylvania, where 98% of the sample was White. At baseline, approximately 41% of the participating youths at the 4 sites lived in single-parent households, and the overall socioeconomic status was between lower and lower-middle class. In the initial screening process, children were identified as being at high risk for behavior problems (or not) on the basis of assessments by teachers and parents using the Teacher Observation of Classroom Adaptation (revised) and Child Behavior Checklist, respectively. High-risk children then were randomly assigned into treatment or comparison groups. The screening process was repeated across 3 cohorts. More detail on the overall screening process for this project can be found in other primary Fast Track research.11–13
Diagnostic Information
In years 7 (sixth grade) and 10 (ninth grade) of the project, the Fast Track group assessed the participants with the Diagnostic Interview Schedule for Children to determine the presence of mental disorders.14 Of the 664 participants, 638 (96%) provided diagnosis data in at least 1 of those years. Parents were asked whether their children demonstrated symptoms related to CD during the past year. Children exhibiting more than 2 symptoms were diagnosed as having CD. In the year 7 sample, 39 individuals (4.0% of the sample when weighted) were classified as having CD; in the year 10 interview, 31 (3.5%) were classified as having CD. Males in the sample were much more likely to be diagnosed with CD (10.5% males diagnosed vs 2.7% females diagnosed in either year). African Americans were also more likely to be diagnosed with CD than Whites (4.9% vs 2.3%, respectively).
The oversampling of high-risk children (i.e., children scoring positive for problem behaviors on the initial screening) boosted the number of children and youths with a diagnosis of CD. In particular, children scoring positive for such behaviors on the initial high-risk screening were more than twice as likely to have a subsequent diagnosis of CD in either year (10.9% vs 5.1%). Their presence in the weighted sample did not affect the representativeness of the data, but they greatly improved the precision of the cost estimates.
For our study, children with conduct problems were classified into 1 of 3 groups, with the remainder of the sample (488; 81.1%) classified as others. Participants were considered to have CD if they met diagnostic criteria in either year 7 or year 10 (59 cases; 6.2% of the sample). Of the remainder, a second group (78; 8.2%) comprised those meeting diagnostic criteria for oppositional-defiant disorder, “a pattern of negativistic, hostile and defiant behavior.”7 A final group (40; 4.4%) included those who never met diagnostic criteria but who exhibited elevated levels of problem behaviors (i.e., within 1 criterion of being diagnosed).
As noted, as many as 96% of the sample provided diagnostic information in at least 1 year. Our analyses relied on multiple imputations to correct for any systematic patterns in attrition or other nonresponse. Additional information on the imputation is available from the authors.
Data on Service Use
We derived information on service use from interviews with participating families and from administrative data. The latter involved a review of school records every summer, which provided information on whether youths repeated a grade or received special education. (These outcomes represent the marginal costs of additional services received. We did not include the costs of regular education because youths with and without conduct problems would experience those costs, canceling them out.)
Information on the use of health and mental health services as well as juvenile justice involvement was provided by parents in the Service Assessment for Children and Adolescents,15 including (for the purposes of our study) how many service visits and number of days a youth received service occurred in the past 12 months. Additionally, parents provided annual information on whether or not their child required medications for emotional/behavioral problems.
Data collection for this information began in year 7 of the project and is ongoing. The cohorts differed somewhat in the data they contributed to our analyses. For instance, because service assessments were staggered, cohort 1 did not receive the Service Assessment for Children and Adolescents in year 8. Additionally, cohort 3 had 2 fewer years of data than cohort 1 at the time of the analysis. In order to provide full (entire sample) estimates for the 7-year time period, we created multiple imputations to accommodate missing cases.
Calculation of Per-Unit Costs
Calculation of public costs of behaviors requires information on both the behaviors and the outcomes involved and also relevant per-unit costs. In general, these figures were calculated as the amount that a state or local government paid for the service or treatment. For costs that could not be derived from previous research, we relied on data from follow-up examination of service use within this sample. All figures taken from the literature were converted to 2000 dollars using the Consumer Price Index.
The outcomes included cover several categories, each combining several service types. These categories include general health (emergency department, family doctor, general hospital); inpatient mental health costs (psychiatric hospital, residential treatment center, group home, foster care); outpatient mental health costs (drug and alcohol clinic, day treatment center, mental health center, in-home provider, individual counselor/therapist); juvenile justice (detention center, arrest costs); and school (school counseling, special education, grade retention).
RESULTS
Levels of Public Costs
Parental reports indicated high rates of service use and system involvement. For instance, by year 11 (the last year data were available for all cohorts), roughly 5% of youths had ever received services for emotional/behavioral problems at an inpatient facility, 15% had received outpatient services, and 18% had received special education services. An additional 21% had had contact with the police.
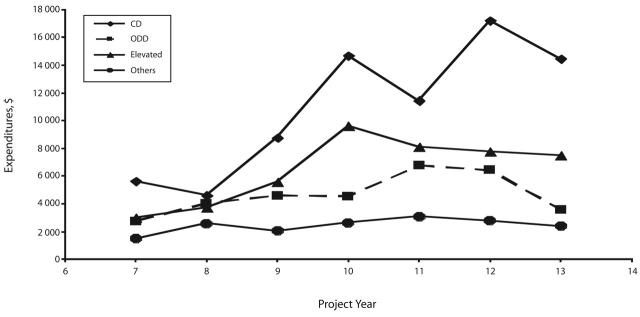
Figure 1 ▶ plots the average total costs across years for the conduct disorder symptom groups. The CD group stood out quite strikingly from the other 3 groups, which were clustered together. The differences grew as the children matured; annual costs in year 13 (end of high school) exceeded $14000 per child for the average youth with CD. This figure was over 6 times that for youths without conduct problems (roughly $2300). The trend over time was significant (P = .05) only for the CD group. (The time trend was assessed through a joint test of the group by year interaction.)
FIGURE 1—
Mean total costs per child across years, by group.
Note. CD = conduct disorder; ODD = oppositional defiant disorder.
Table 1 ▶ provides more detail on these overall levels. Statistical significance refers to the differences among the 4 groups, calculated by regressing the logarithm of the costs of the diagnosis groups. (Significance refers to the joint significance of the 3 dummy variables representing the between-group differences.) The between-group differences were significant at most ages and for most types of costs. The exceptions included physical and mental health services in some years. In the case of the former, especially inpatient mental health services, the lack of significance largely reflected the small number of individuals involved in those systems. When mental health costs were incurred, they were often quite substantial. For example, inpatient and outpatient mental health costs accounted for nearly 70% of the difference between the CD and Other groups.
TABLE 1—
Average Per-Child Expenditures (2000 $), by Conduct Disorder Symptom Group, Expenditure Type, and Project Year
| Symptom Group | |||||
| CD | CD-B | ODD | Other | Statistical Significancea | |
| Year 7 | |||||
| Medications | 65 | 24 | 33 | 10 | .01 |
| General health | 241 | 288 | 200 | 301 | .45 |
| Inpatient mental health | 1384 | 543 | 13 | 16 | .35 |
| Outpatient mental health | 958 | 169 | 406 | 123 | .02 |
| Juvenile justice | 17 | 21 | 40 | 4 | . . . |
| School | 2912 | 1921 | 2032 | 1005 | .01 |
| Combined | 5625 | 2991 | 2753 | 1493 | .00 |
| Year 8 | |||||
| Medications | 116 | 42 | 60 | 37 | .01 |
| General health | 566 | 338 | 310 | 254 | .63 |
| Inpatient mental health | 381 | 288 | 259 | 432 | .70 |
| Outpatient mental health | 726 | 448 | 392 | 464 | .84 |
| Juvenile justice | 352 | 249 | 258 | 130 | .54 |
| School | 2806 | 2378 | 2776 | 1437 | .04 |
| Combined | 4604 | 3738 | 4034 | 2575 | .10 |
| Year 9 | |||||
| Medications | 421 | 274 | 260 | 45 | .02 |
| General health | 781 | 508 | 394 | 294 | .75 |
| Inpatient mental health | 1611 | 2350 | 696 | 137 | .08 |
| Outpatient mental health | 1506 | 535 | 369 | 127 | .00 |
| Juvenile justice | 1282 | 388 | 322 | 103 | .04 |
| School | 4448 | 2664 | 2932 | 1438 | .00 |
| Combined | 8769 | 5573 | 4604 | 2030 | .00 |
| Year 10 | |||||
| Medications | 308 | 46 | 51 | 26 | .15 |
| General health | 412 | 757 | 136 | 224 | .53 |
| Inpatient mental health | 9563 | 4695 | 1550 | 1007 | .13 |
| Outpatient mental health | 335 | 543 | 148 | 59 | .00 |
| Juvenile justice | 1389 | 1431 | 375 | 97 | .00 |
| School | 2943 | 2188 | 2321 | 1232 | .00 |
| Combined | 14 692 | 9639 | 4553 | 2633 | .00 |
| Year 11 | |||||
| Medications | 161 | 39 | 77 | 59 | .05 |
| General health | 1012 | 267 | 272 | 328 | .15 |
| Inpatient mental health | 2574 | 2691 | 1871 | 395 | .13 |
| Outpatient mental health | 1277 | 514 | 811 | 155 | .01 |
| Juvenile justice | 2495 | 509 | 538 | 277 | .00 |
| School | 4536 | 4230 | 3351 | 1917 | .01 |
| Combined | 11 440 | 8103 | 6780 | 3077 | .00 |
| Year 12 | |||||
| Medications | 365 | 242 | 332 | 144 | .08 |
| General health | 1677 | 681 | 560 | 389 | .84 |
| Inpatient mental health | 2743 | 3439 | 1374 | 572 | .11 |
| Outpatient mental health | 1783 | 412 | 622 | 412 | .04 |
| Juvenile justice | 7130 | 1055 | 1641 | 457 | .00 |
| School | 4814 | 2998 | 3599 | 1702 | .00 |
| Combined | 17 209 | 7760 | 6421 | 2759 | .00 |
| Year 13 | |||||
| Medications | 1664 | 610 | 643 | 251 | .20 |
| General health | 1738 | 976 | 548 | 519 | .30 |
| Inpatient mental health | 5833 | 4580 | 225 | 556 | .47 |
| Outpatient mental health | 3269 | 823 | 414 | 199 | .16 |
| Juvenile justice | 2446 | 366 | 481 | 323 | .01 |
| School | 3732 | 2220 | 2790 | 1381 | .01 |
| Combined | 14 456 | 7487 | 3573 | 2373 | .00 |
Note. CD = conduct disorder; CD-B = borderline conduct disorder; ODD = oppositional defiant disorder.
aStatistical significance refers to the differences among the 4 groups, calculated by regressing the logarithm of the costs of the diagnosis groups. Significance refers to the joint significance of the 3 dummy variables representing the between-group differences.
The other notable cost for which between-group differences were not significant involved juvenile justice at young ages. As we expected, youths were seldom involved in that system before year 9 of the study (eighth grade).
The variation across groups explained only 5% of the total variance (calculated using the log transformation of costs model). One explanation for the variation within groups is co-morbidity. Supplemental analyses revealed that comorbid attention problems did not raise expenditures substantially.
Hidden in these averages were substantial within-group differences. Table 2 ▶ reports the median and other key percentiles (25th, 75th, and 90th) for total costs. For all groups, mean expenditures were far greater than median expenditures, reflecting the presence of very high cost individuals. To provide a sense of how important a few cases were, the last column provides the percentage of total costs accounted for by the top 10% of each group (i.e., the individuals above the 90th percentile, which is also reported). These individuals accounted for roughly half of all expenditures in all 4 groups.
TABLE 2—
Total Expenditures (2000 $), by Diagnosis Group, All Project Years
| 25th Percentile | Median | Mean | 75th Percentile | 90th Percentile | Percentage of Total Accounted for by Top 10% | |
| Other | 83 | 508 | 3830 | 6251 | 8212 | 49% |
| Elevated | 217 | 3968 | 7258 | 7178 | 14 050 | 54% |
| ODD | 338 | 4033 | 6630 | 7254 | 12 848 | 48% |
| CD | 1368 | 6735 | 12 547 | 11 703 | 25 985 | 52% |
Note. ODD = oppositional defiant disorder; CD = conduct disorder.
Supplemental analyses illustrated how high levels of service use accounted for expenditures in these extreme cases. The year 10 data, for example, revealed that among those admitted to inpatient facilities, the median length of stay was 58 days. However, 10% of those admitted had a length of stay of 365 days—they were in a residential facility for the entire year.
Differential Composition of Expenditures
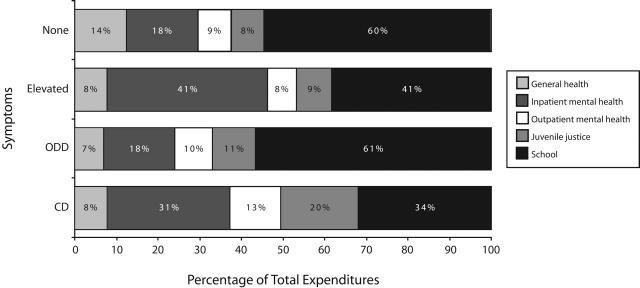
Figure 2 ▶ displays the average composition of public costs across sectors. School expenditures represented a substantial proportion of public expenditures and were influenced by the high costs of special education and retention. In proportional terms, these costs were smaller for the CD group. (In reading this figure, one should be careful not to translate the lower percentages into lower absolute amounts. The CD group still had the highest school costs averaged across years among these groups, as evidenced in Table 1 ▶.) To some extent, this difference reflects the fact that youths with CD were more likely to drop out of high school, reducing the use of school services. Figure 2 ▶ also shows that juvenile justice expenditures represented approximately 20% of total expenditures for the youths with CD. This far exceeds the highest percentage among the other groups (oppositional defiant disorder; 11%). Interestingly, children who had elevated levels of problem behaviors (but were not diagnosed with CD) required a higher percentage of spending on inpatient mental health assistance than the other groups.
FIGURE 2—
Percentage costs within service sectors by group (averaged across years).
Note. ODD = oppositional defiant disorder; CD = conduct disorder.
DISCUSSION
The public costs of behavior problems among children and youths are enormous. When summed across all 7 years (years 7 through 13), expenditures for the CD youths were nearly $70000 larger than those for the children in the No Disorder group. It is important to note, however, that the latter are hardly risk free. They live in poor neighborhoods and so are at much greater risk of poor outcomes than the average American youth. For that reason, one can think of these findings as capturing the effect of CD with control for a range of risk factors.
Our results are consistent with limited prior research. In a 1999 study of 10 youths referred for mental health services, Knapp et al.16 found that yearly social costs exceeded $15000. The greatest expense fell on the families themselves ( just over a third), while the education authority bore an additional third. Significant costs fell on the health, social services, and welfare systems. In a second study, Scott et al.17 examined the experiences of 142 youths living in central London. These youths were identified at 10 years of age as either having no conduct problems, conduct problems, or a diagnosis of CD. The authors then considered the costs incurred by various public agencies through 28 years of age. These costs primarily involved the costs of crime as well as educational, health, and social services expenditures. Costs for those with CD were 10 times those without problems and 3.5 times those for youths with conduct problems (but not meeting the criteria for CD). Crime-related costs were the largest for the conduct problems and CD groups (35% and 64%, respectively). Educational costs accounted for the second-highest proportion, representing 31% and 18% of the 2 groups, respectively. These findings suggested a somewhat greater gap for those with CD relative to those with only elevated levels of symptoms.
Unlike Scott et al., we have not extended our analyses beyond the public costs to include social costs. Nonetheless, the expenditures captured here are especially important from a public policy perspective. They highlight the fact that these children and youths are already costing taxpayers a great deal of money. The key policy question is not whether to spend money on these children but rather how to spend it.
Still, this perspective does have limitations. For example, the school costs began to fall in later years as the youths left school. Dropping out may reduce public expenditure but only when gauged from a very narrow, short-term perspective. Clearly, dropping out of school raises the likelihood of future welfare and crime-related expenditures. For that reason, these expenditures represent a lower bound for the potential societal benefits of prevention.
As briefly noted, a surprising finding is that comorbid attention problems did not raise public costs. However, this finding rests on the validity and reliability of the instrumentation used, and the role of other comorbid conditions or profiles deserves additional attention.
Strengths and Limitations
The data on which this study was based are unique and have several strengths. They were longitudinal and included an oversample of young children who were at greater risk of developing CD. Because expenditures were so skewed, these children were particularly important in statistical analyses. This study also has other strengths, such as data collection from 4 diverse communities and high follow-up rates. Furthermore, the data included true diagnostic measures of CD rather than simple measures of aggressive symptoms (such as the Child Behavior Checklist).
Nonetheless, this study has several limitations. One limitation of these analyses is that we applied the same per-unit costs to facilities (within a given category) regardless of the diagnosis of the children involved. As a result, our findings may understate the difference between youths with CD and other youths if the former were treated in more expensive or intensive settings. For that reason, our findings are best judged as conservative.
Another limitation is that measures of service use reflected parental self-reports and may have underreported actual service activity. As a result, the costs presented may be underestimates. However, comparisons of system involvement for which we have both parental report and administrative data are somewhat reassuring. For example, a comparison of court records and parental reports of juvenile justice involvement showed 85% agreement. If parents or youths under-reported services, we have no reason to believe that one group underreported to a greater degree than another. In that case, the between-group gaps would be smaller in absolute terms but not in percentage terms. (Measures of statistical significance involving between-group differences would not be affected either.)
Conclusions
The high costs of bad behavior are discouraging. These figures, however, offer some reason for hope. In particular, the expenditure gap between children with CD and those with lower, but elevated, levels of behavior problems was still substantial. This gap suggests that the problem behaviors of the high-cost children with CD need not be eliminated entirely to achieve substantial savings; rather, substantial savings could be realized simply by reducing those problems.
Our analysis suggests that public expenditures may be reduced if resources are moved from coping with problem behaviors to preventing them. A necessary condition is that effective programs be developed, and results in this area are encouraging. Furthermore, even among these youths with CD in high-risk neighborhoods, the public costs are still relatively concentrated among a small group. As a result, the cost-effectiveness of an effective intervention could be enhanced by effective targeting, and research suggests that these children can be identified accurately.18
The implementation of such programs, however, represents a public health challenge. Resources will need to be shifted from established uses, such as juvenile detention, into other areas, such as the public mental health system. Such a change in focus and resources likely will require strong leadership from a public health leader with a broad public health perspective.
Acknowledgments
This work was supported by the National Institute of Mental Health (NIMH) (grants R18 MH48043, R18 MH50951, R18 MH50952, and R18 MH50953). The Center for Substance Abuse Prevention and the National Institute on Drug Abuse also have provided support for Fast Track through a memorandum of agreement with NIMH. This work was also supported in part by Department of Education (grant S184U30002 and NIMH grants K05MH00797 and K05MH01027). The economic analysis of the Fast Track project was supported by the National Institute of Public Health (grant R01MH62988).
Members of the Conduct Problems Prevention Research Group are, in alphabetical order, Karen L. Bierman, Pennsylvania State University; John D. Coie, Duke University; Kenneth A. Dodge, Duke University; E. Michael Foster, Pennsylvania State University; Mark T. Greenberg, Pennsylvania State University; John E. Lochman, University of Alabama; Robert J. McMahon, University of Washington; and Ellen E. Pinderhughes, Tufts University.
The authors thank E. J. Kang for expert research assistance.
Human Participant Protection No protocol approval was needed for this study.
Peer Reviewed
Contributors E. M. Foster conceptualized and executed the analyses and participated in preparing the article. D. E. Jones assisted with analyses and writing the article. The Conduct Problems Prevention Research Group provided editorial suggestions.
References
- 1.Pincus HA, Pettit A. The societal costs of chronic major depression. J Clin Psychiatry. 2001;62(suppl 6):5–9. [PubMed] [Google Scholar]
- 2.Forness SR, Kavale KA. Impact of ADHD on school systems. In: Jensen PS, Cooper JR, eds. Attention Deficit Hyperactivity Disorder: State of the Science—Best Practices. Kingston, NJ: Civic Research Institute; 2002: 24–1—24–20.
- 3.Guevara J, Lozano P, Wickizer T, Mell L, Gephart H. Utilization and cost of health care services for children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:71–79. [DOI] [PubMed] [Google Scholar]
- 4.Guevara JP, Mandell DS, Rostain AL, Zhao H, Hadley TR. National estimates of health services expenditures for children with behavioral disorders: an analysis of the medical expenditure panel survey. Pediatrics. 2003;112:e440–e446. [DOI] [PubMed] [Google Scholar]
- 5.Kelleher KJ. Use of services and costs for youth with ADHD and related conditions. In: Cooper JR, ed. Attention Deficit Hyperactivity Disorder. Kingston, NJ: Civic Research Institute; 2002:27–1–27–12.
- 6.Leibson CL, Katusic SK, Barbaresi WJ, Ransom J, O’Brien PC. Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder. JAMA. 2001;285(1):60–66. [DOI] [PubMed] [Google Scholar]
- 7.Task Force on DSM-IV. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Washington, DC: American Psychological Association; 2000.
- 8.Brook JS, Whiteman M, Finch SJ, Cohen P. Young adult drug use and delinquency: childhood antecedents and adolescent mediators. J Am Acad Child Adolesc Psychiatry. 1996;35:1584–1592. [DOI] [PubMed] [Google Scholar]
- 9.Capaldi DM, Crosby L, Stoolmiller M. Predicting the timing of first sexual intercourse for at-risk adolescent males. Child Dev. 1996;67:344–359. [PubMed] [Google Scholar]
- 10.Foster EM, Kelsch CC, Kamradt B, Sosna T, Yang Z. Expenditures and sustainability in systems of care. J Emotional Behav Disord. 2001;9(1):53–62. [Google Scholar]
- 11.Conduct Problems Prevention Research Group. A developmental and clinical model for the prevention of conduct disorders: the Fast Track program. Dev Psychopathol. 1992;4:509–527. [Google Scholar]
- 12.Conduct Problems Prevention Research Group. Initial impact of the Fast Track prevention trial for conduct problems, I: the high-risk sample. J Consult Clin Psychol. 1999;67:631–647. [PMC free article] [PubMed] [Google Scholar]
- 13.Conduct Problems Prevention Research Group. Initial impact of the Fast Track prevention trial for conduct problems, II: classroom effects. J Consult Clin Psychol. 1999;67:648–657. [PMC free article] [PubMed] [Google Scholar]
- 14.Shaffer D, Fisher P, Christopher PL, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV: description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. [DOI] [PubMed] [Google Scholar]
- 15.Stiffman AR, Horwitz SM, Hoagwood K, et al. The Service Assessment for Children and Adolescents (SACA): adult and child reports. J Am Acad Child Adolesc Psychiatry. 2000;39:1032–1039. [DOI] [PubMed] [Google Scholar]
- 16.Knapp M, Scott S, Davies J. The cost of antisocial behaviour in younger children. Clin Child Psychol Psychiatry. 1999;4:457–473. [Google Scholar]
- 17.Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001;323:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones D, Dodge KA, Foster E, Nix R, Conduct Problems Prevention Research Group. Early identification of children at risk for costly mental health service use. Prev Sci. 2002;3:247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]