Abstract
There is now a substantial literature on risk factors for suicide across the life course. Therefore, it is essential to extend this knowledge by considering more fully which age- and gender-specific groups bear the greatest public health burden owing to suicide and its antecedents. With this in mind, suicide mortality rates alone may not sufficiently inform U.S. policy makers who must distribute scarce suicide prevention resources.
We compared age- and gender-specific mortality rates, age- and gender-specific estimates of years of potential life lost, and age- and gender-specific present value of lost earnings that individuals would have contributed to society had they lived to their full life expectancies.
Men in the middle years of life contribute disproportionately to the public health burden because of completed suicide. The substantial burden evident in this group has not translated into a public health priority.
THERE IS NOW A SUBSTANTIAL literature on risk factors for suicide in the United States to suggest that suicide1–19 is a public health problem of considerable magnitude.3,5,20 There were 31655 deaths from suicide in 2002 (the 11th leading cause of death) and 17638 deaths from homicide (the 14th leading cause of death21). But the death toll from homicide draws much more attention, and many more resources are spent to reduce associated violent crime. Since the 1950s, the rate of youth suicide has tripled,3 and there has been an alarming gradual upswing in suicide among young African-American males in the United States between 1980 and 1995.22,23 Substantially higher rates of suicide in elders in the United States have been observed consistently for some time.24
These statistics are informative, but they relay only a partial picture of the true public health burden of suicide. The consideration of other groups that also may bear a significant public health burden because of suicide is necessary in order to assist policymakers who are tasked to establish appropriate target populations for effective intervention. Estimates of morbidity and mortality typically are good indicators for establishing national health priorities, such as the broad initiatives to prevent heart disease over the last 50 years. But suicide, like heart disease, occurs within a background of complex interacting clinical disorders and biological, social, and environmental risk factors. In contrast to preventive cardiology, we have few measures to fully assess the true public health burden attributable to suicide and the myriad of its antecedents, such as depression and attempted suicide. Furthermore, estimates of suicide mortality rates are likely underreported in the United States.25,26 The 2002 report released from the President’s New Freedom Commission on Mental Health5 established suicide prevention as a national priority. If this vision is to be fully realized, it will be imperative to clearly illuminate the full extent of the loss of life and related morbidity attributable to suicide and attempted suicide in this country.
Another crucial component of the current challenge to move from rhetoric to action relates to our imprecise estimates of the true magnitude of the overall public health burden because of suicide. Suicide, although not a disease, is a tragic end point or a “tip-of-the-iceberg”27 indicator of multiple competing risks. When a person is diagnosed with HIV infection, serious heart disease, or treatable but incurable cancer, a key measure of disease burden entails determining the time of survival after initial diagnosis.28 There is presently no comparable method for estimating the burden of antecedent conditions that lead to death from suicide, yet it is just such metrics that are required to estimate accurately the costs that are associated with this highly deleterious outcome. Developing the methods to comprehensively address these deficiencies is beyond the scope of this article, even as it remains an area for future investigation. We examined the absolute risk of suicide and the rates of suicide across the life cycle, comparing the rates of suicide to other measures that may extend our understanding of the public health burden attributable to suicide.
METHODS
Mortality Data
Final data on the deaths of US residents in 2002 were obtained from the National Center for Health Statistics (NCHS) Vital Statistics System from death certificates filed in all 50 states and the District of Columbia.21 This system supplied both the gender-specific numerator and denominator data for the number of suicides in 5-year increments which were used to calculate the age- and gender-specific rates of suicide for each group. Gender-specific years of potential life lost (YPLL) and present value of lifetime earnings (PVLE)
Premature mortality is measured by the YPLL statistic, which is simply the sum of the years of life lost annually by persons who suffered early deaths.29 For the purpose of calculating YPLL, premature death from suicide was defined as death occurring up through the age of 85. Thus, the population at risk of premature mortality is the US population between the ages of 0 and 85 in 2002.21 Because relatively few suicides have occurred before the age of 10 in the United States, age groups were defined in 5-year increments beginning with the age group of 10- to 14-year-olds. The calculations of YPLL were performed on males and females separately. We took the number of suicides in each of the 5-year increments (beginning with 10 to 14 years, and so forth) and multiplied this number by the life expectancy in the year 200030 for an individual at the midpoint of the range. All age group totals were summed to obtain an overall total for each gender. The totals for males and females were combined to get total YPLL attributable to suicide. Therefore, for gender-specific and total calculations, YPLL is the ∑ (number of deaths in each age group by gender× life expectancy for a person at the midpoint of the age range). Although 65 years of age has been the customary age of retirement from work in the United States, overall life expectancy in this country in 2000 was 76.9 years.30 Because of the importance of retaining information on rates of suicide in elders, we considered 85 years of age as an important cutoff point.
Potential economic losses to society were estimated by calculating gender and age group-specific PVLE, which is the expected value of lost earnings an individual would have contributed to society if that person had lived out his or her full life expectancy.31 We took the number of suicides in each 5-year increment in the year 2002 and determined the median income for each group and for each gender using census data from 2000.30 The median income for each group also included a fringe benefit amount32 to allow for uncompensated wages (such as sick leave). Using the median income for each period, we estimated the present value of future earnings by first inflating earnings during the year by 1%. We then discounted all future expected earnings using a 3% discount rate32 to calculate the net present value. We assumed that all individuals would continue to be employed and that future earnings would be the income that someone in 2000 was receiving as the individual reached the next age group. We summed the discounted earnings and multiplied this figure by the number of suicides in each group. We did not, as others have done, calculate other economic costs, such as some proxy measure of lost household productivity; direct medical care expenses; or indirect societal costs, such as suffering by family and friends of suicide victims.33
Causes of Death Among Men in the Middle Years of Life
We ranked all of the major causes of death for the subpopulation of men aged 25 to 54 in order to determine whether suicide is a key determinant of mortality in this age group.
RESULTS
Table 1 ▶ gives the age- and gender-specific mortality attributable to suicide in the year 2002.
TABLE 1—
Number of Deaths, Rates of Suicide per 100 000 With 95% Confidence Intervals (CIs), by Gender and Age Group: United States, 2002
| Age Group, y | No. Deaths | Rate per 100 000 (95% CI) |
| Males | ||
| 0–4 | 0 | 0 (NA) |
| 5–9 | 3 | 0.03 (0.00, 0.06) |
| 10–14 | 196 | 1.81 (1.56, 2.06) |
| 15–19 | 1280 | 12.23 (11.56, 12.90) |
| 20–24 | 2152 | 20.63 (19.76, 21.5) |
| 25–29 | 2003 | 20.84 (19.93, 21.75) |
| 30–34 | 2132 | 20.31 (19.45, 21.17) |
| 35–39 | 2484 | 22.78 (21.88, 23.68) |
| 40–44 | 2821 | 24.76 (23.85, 25.67) |
| 45–49 | 2608 | 24.89 (23.93, 25.85) |
| 50–54 | 2188 | 23.84 (22.84, 24.84) |
| 55–59 | 1708 | 23.54 (22.42, 24.66) |
| 60–64 | 1129 | 20.46 (19.27, 21.65) |
| 65–69 | 975 | 21.95 (20.57, 23.33) |
| 70–74 | 1078 | 27.87 (26.21, 29.53) |
| 75–79 | 1054 | 34.26 (32.19, 36.33) |
| 80–84 | 884 | 44.08 (41.17, 46.99) |
| ≥ 85 | 704 | 51.14 (47.36, 54.92) |
| Females | ||
| 0–4 | 0 | 0 (NA) |
| 5–9 | 1 | 0.01 (0.01, 0.03) |
| 10–14 | 64 | 0.62 (0.47, 0.77) |
| 15–19 | 233 | 2.36 (2.06, 2.66) |
| 20–24 | 345 | 3.49 (3.12, 3.86) |
| 25–29 | 420 | 4.52 (4.09, 4.95) |
| 30–34 | 491 | 4.76 (4.34, 5.18) |
| 35–39 | 657 | 6.03 (5.57, 6.49) |
| 40–44 | 889 | 7.7 (7.19, 8.21) |
| 45–49 | 865 | 8.02 (7.49, 8.55) |
| 50–54 | 647 | 6.75 (6.23, 7.27) |
| 55–59 | 478 | 6.19 (5.63, 6.75) |
| 60–64 | 303 | 4.99 (4.43, 5.55) |
| 65–69 | 222 | 4.32 (3.75, 4.89) |
| 70–74 | 188 | 3.88 (3.33, 4.43) |
| 75–79 | 177 | 4.06 (3.46, 4.66) |
| 80–84 | 144 | 4.36 (3.65, 5.07) |
| ≥ 85 | 122 | 3.82 (3.14, 4.5) |
YPLL and PVLE Across the Life Course
There were more than 1 million YPLL attributable to suicide across the life course for men and for women in the year 2002, of which 67% was attributable to men and women in the middle years of life, as shown in Figure 1 ▶. (Note that the total YPLL is similar to that reported by the Centers for Disease Control and Prevention for total YPLL in 2002 if calculated through age 8534). This potential loss of life was associated with an estimated PVLE of $13 billion for all of those who died from suicide in that year. Using both the estimates of YPLL and PVLE, we found that the highest public health burden attributable to suicide is for men in the middle years of life, although rates are higher in youth and elders. The YPLL and lost earnings we estimated here do not reflect the impact of suicide attempts. In a previous study of hospitalizations from suicide attempts, Palmer et al.33 estimated that hospital and physician costs in 1994 were $581 million for attempted suicide. However, because there has not been national surveillance of attempted suicide, the actual cost to society in terms of long-term disability is unknown.
FIGURE 1—
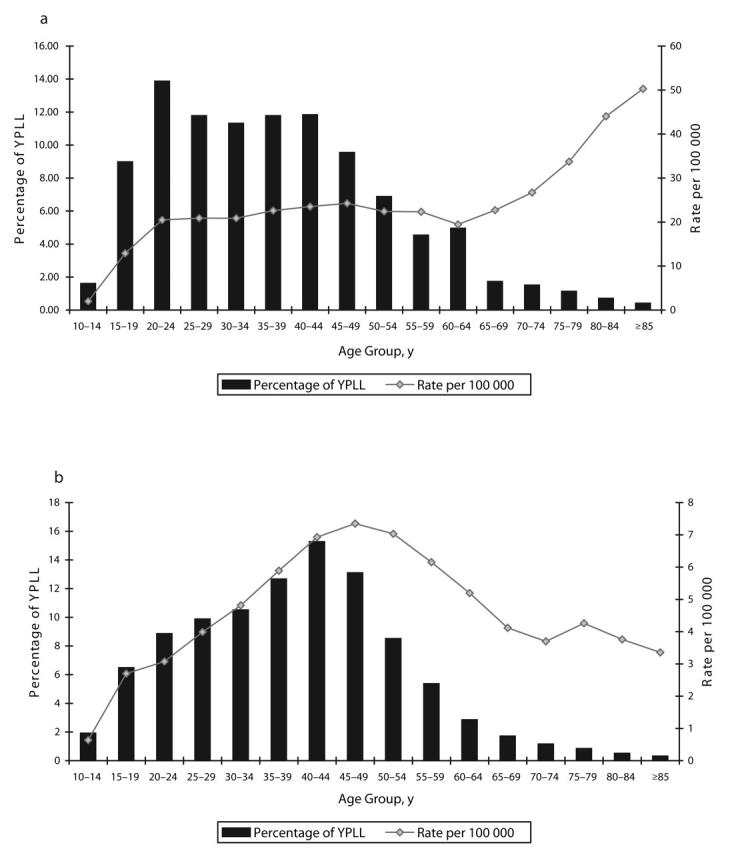
Percentage of total years of potential life lost and rates of suicide in the United States in 2002.
Note. YPLL = years of potential life lost.
Leading Causes of Death Among Men in the Middle Years of Life
In 2002, suicide ranked fourth as a leading cause of death among men in the middle years of life (after heart disease, malignant neoplasms, and unintentional injuries) and exceeded other leading causes of death in this age group, such as HIV, homicide, diabetes, and stroke.
DISCUSSION
The purpose of this study was to initiate a more in-depth discussion of how we can better understand the public health burden attributable to suicide in the United States. Men in the middle years of life have the highest absolute risk for suicide. This group accounts for the greatest YPLL and the greatest expected value of lost earnings that they would have contributed to society. The YPLL has been widely used to elucidate the burden of disease for other public health problems.35–38 The YPLL is recognized by the US General Accounting Office as the best single indicator for reflecting differences in the health status of the states of the nation.39 We use it as an indicator to begin a discussion about the potential impact that the distribution of resources for suicide prevention to nontraditional prevention sites, such as the workplace, would likely have on a largely unrecognized at risk population. (Worth noting is that 1 limitation of our use of the PVLE is that unemployed men have a higher suicide rate than employed men. In addition, suicide rates are higher in lower socioeconomic classes, where incomes are lower, thus, multiplying the number of suicides by the average income for men in the middle years of life may lead to bias.40). Although there are no published reports of effective workplace interventions for suicide prevention, we have shown that a multilayered suicide prevention program in the US Air Force was associated with a 33% relative risk reduction for suicide. As well, after “exposure” to the US Air Force Suicide Prevention Program, there were relative risk reductions because of homicide, accidental death, and domestic violence.27 As such, men in the middle years of life may offer a potential target population to reduce the public health burden attributable to suicide and other, related deleterious outcomes.
Economists, lawyers, and philosophers have struggled to determine the “value of life.”41 It was not our intention to contribute to this debate; nor are we implying that preventing suicide in youth or elders should be relegated as a secondary priority to any other group. However, the crucial need for prevention efforts in these subpopulations has been recognized for some time, and there are some significant initiatives that target reducing suicide in these groups.42–51 Yet, men in the middle years of life, who contribute largely to the YPLL because of suicide, are rarely recognized as an important group for suicide prevention.
Overall, suicide prevention has struggled to gain a foothold in the public health realm, largely because of the perception that it is an outcome with a low base rate. The establishment of the leading causes of death in the United States is dependent to a great extent on the manner in which the disease categories are constructed. For example, heart disease is, by far, the leading cause of death in the United States. However, the NCHS tabulates mortality of “diseases of the heart” by grouping all diseases containing words that refer to the heart, which encompasses a number of ICD-10 codes.21 The same is true for malignant neoplasms, which include all cancers. Moreover, the American Heart Association52 uses a different definition than the NCHS to define “cardiovascular disease,” using one that includes mortality from stroke and high blood pressure, and increases the apparent burden of disease. Suicide is presently limited to 2 ICD-10 codes that categorize suicide as either attributable to a firearm or to other unspecified means and their sequelae. In spite of being defined as a narrow category, suicide is the 11th leading cause of death in the United States overall21,25 and is the 4th leading cause of death among men in the middle years. Were depression and alcohol addiction considered the stroke and high blood pressure of suicide, the true need for prevention would become more evident.
Depression is a well-known risk factor for suicide in many Western countries.53–56 The Global Burden of Disease Project 200057 reports that unipolar depressive disorders rank as the fourth-leading cause of burden of all outcomes (following all respiratory infections, perinatal, and HIV), accounting for 4.4% of the total disability adjusted life years (DALYs) lost. In the age group of 15 to 44 years, it is the second highest burden, accounting for 8.6% of DALYs lost. These estimates clearly reflect a demonstratively high burden of disease, albeit one that is likely underestimated. Projections based on present demographic and epidemiological transitions during the coming decade suggest that, by the year 2020, the burden of depression will increase to 5.7% of the total burden of disease, becoming the second leading cause of DALYs lost.57 The implications of this are considerable. For example, 1 study has found that clinical depression was significantly associated with suicidal ideation, with a population-attributable risk of 46.9%.58 Moreover, a recent study in US workers estimated that workers with depression cost employers $44 billion per year in lost productive time, which was in excess of $32 billion per year compared with peers without depression.59
Several reports suggest the men in the workplace as a group may be at especially high risk for undiagnosed depression.60–62 A number of studies have found that men are less likely to seek help for depression than are women.63–66 As cited by Moller-Leimkuhler,67 a recent German study of suicide concluded, “women seek help—men die.” However, there is relatively little evidence that can explain the discrepancy between the perception of need and help-seeking behaviors for a mental health or psychosocial problem. Interestingly, gender-specific studies have focused primarily on somatic diseases (such as cardiovascular disease) in males and on psychiatric disorders (such as depression) in women. This is despite reports that the help-seeking behaviors of men for depression are negatively affected by common risk factors for suicide, such as low income and unemployment. It will be important to establish whether efforts such as those implemented by the National Institutes of Mental Health to destigmatize help-seeking behavior among men68 will also be effective in reducing suicide for this subpopulation.
We have demonstrated that men in the middle years of life contribute disproportionately to the total public-health burden of suicide mortality. Our review of the prevention literature suggests that the substantial burden faced by this group has not been translated into a well-defined or well-funded public health priority. Yet, among men of this age group, suicide is responsible for greater premature mortality than other important and well-funded public health problems. It is timely, given the recent release of the report from the president’s commission5 and the important declaration of the surgeon general in 19991 regarding the urgency of suicide prevention, to have more balanced, data-driven discussions regarding the challenges posed by this problem and the difficult task of setting priorities when considering how to spend the nation’s funds. By expanding the “metrics of suicide,” we hope to expand the dimensions of what needs to be a well-informed, continuing public debate.
Acknowledgments
The study was funded in part by National Institute of Mental Health (grants K01 MH066317 [K. L. Knox], R13 MH62073 [E. D. Caine], and P20 MH071897 [E. D. Caine]).
Human Participant Protection No protocol approval was required for this study.
Peer Reviewed
Contributors Both K. L. Knox and E. D. Caine originated the study. K. L. Knox carried out the analyses and was the lead author. Both authors contributed to the final interpretation and conclusions presented and the final revision of the article.
References
- 1.The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: US. Department of Health and Human Services, Public Health Service; 1999.
- 2.National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville, MD: US. Department of Health and Human Services, Public Health Service; 2001. [PubMed]
- 3.Committee on Pathophysiology & Prevention of Adolescent & Adult Suicide, Board on Neuroscience and Behavioral Health, Institute of Medicine. Reducing Suicide: A National Imperative. Washington, DC: National Academy Press; 2002.
- 4.Suicide Prevention and Intervention: Summary of a Workshop. Washington, DC: National Academy Press, 2001. [PubMed]
- 5.New Freedom Commission on Mental Health, Achieving the Promise: Transforming Mental Health Care in America. Final Report. Rockville, MD: US Dept of Health and Human Services; 2003. Pub. No. SMA-03–3832.
- 6.Fremouw WJ, dePerczel M, Ellis TE. Suicide Risk: Assessment and Response Guidelines. New York: Pergamon Press; 1990.
- 7.Conner KR, Cox C, Duberstein PR, Tian L, Nisbet PA, Conwell Y. Violence, alcohol, and completed suicide: a case-control study. Am J Psych. 2000;158(10): 1701–1705. [DOI] [PubMed] [Google Scholar]
- 8.Conner KR, Duberstein PR, Conwell Y. Domestic violence, separation, and suicide in young men with early onset alcoholism: reanalyses of Murphy’s data. Suicide Life Threat Behav. 2000;30:354–359. [PubMed] [Google Scholar]
- 9.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the adverse childhood experiences study. JAMA. 2001;286:3089–3096. [DOI] [PubMed] [Google Scholar]
- 10.Conner KR, Li Y, Meldrum S, Duberstein PR, Conwell Y. The role of drinking in suicidal ideation: analyses of Project MATCH data. J Stud Alcohol. 2003;64:402–408. [DOI] [PubMed] [Google Scholar]
- 11.Brent DA, Johnson BA, Perper J, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psych. 1994;33:1080–1086. [DOI] [PubMed] [Google Scholar]
- 12.Coppen A. Lithium in unipolar depression and the prevention of suicide. J Clin Psych. 2000;61:52–56. [PubMed] [Google Scholar]
- 13.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. A J Psych. 1999;156:181–189. [DOI] [PubMed] [Google Scholar]
- 14.Moscicki Ek. Epidemiology of suicidal behavior. Suicide Life Threat Behav. 1995;25:1–17. [PubMed] [Google Scholar]
- 15.Brent DA, Baugher M, Bridge J, et al. Age-and sex-related risk factors for adolescent suicide victims. Arch Gen Psych. 1996;53:1145. [DOI] [PubMed] [Google Scholar]
- 16.Maris RW. Suicide prevention in adults (age 30–65). Suicide Life Threat Behav. 1995;25:171–179. [PubMed] [Google Scholar]
- 17.Kessler RC, Borges G, Walters EE. Prevalence of risk factors for life time suicide attempts in the National Comorbidity Survey. Arch Gen Psych. 1999; 56(7):617–626. [DOI] [PubMed] [Google Scholar]
- 18.Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am J Geriat Psych. 1998; 6:122–126. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Suicide prevention evaluation in a Western Athabaskan American Indian Tribe—New Mexico, 1988–1997. MMWR Morb Mortal Wkly Rep. 1998; 47(No. 13):257–261. [PubMed] [Google Scholar]
- 20.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health. 2004;94:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kochanek KD, Smith BL. Deaths: preliminary data for 2002. Nat Vital Stat Rep. February 1, 2004;52(13). [PubMed]
- 22.Griffith EEH, Bell C. Recent trends in suicide and homicide among blacks. JAMA. 1989;262(16):2265–2269. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Suicide among Black Youths—United States, 1980–1995. MMWR Morb Mortal Wkly Rep. 1998; 47(N0.10);193–196. [PubMed] [Google Scholar]
- 24.Conwell Y. Suicide in the elderly. In: Schneider LS, Reynolds III CF, Lebowitz BD, Friedhoff AJ, eds. Diagnosis and Treatment of Depression in Late Life. Washington, DC: American Psychiatric Press; 1994:397–418.
- 25.Minino AM, Arias E, Kochanek KD, et al. Deaths: Final data for 2000. Nat Vital Stat Rep. 2002;50(15). [PubMed]
- 26.Arias E, Smith BL. Deaths: Preliminary data for 2001. Nat Vital Stat Rep. 2003;51(5). [PubMed]
- 27.Knox KL, Litts DA, Talcott GW, Feig JC, Caine ED. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the US Air Force: cohort study. BMJ. 2003;327:1376–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. 2nd ed. New York: John Wiley & Sons; 2002.
- 29.Centers for Disease Control and Prevention. Premature mortality in the United States: public health issues in the use of years of potential life lost. MMWR Morb Mortal Wkly Rep. 1986;35(2S): 1s–11s. [PubMed] [Google Scholar]
- 30.US. Census Bureau. Available at: http://www.census.gov/hhes/income/histinc/p08.html. Accessed February 7, 2004.
- 31.National Center for Injury Prevention and Control. Costs of Intimate Partner Violence Against Women in the United States. Atlanta, GA: Centers for Disease Control and Prevention; 2003.
- 32.Max W, Rice DP, Sung H-Y, Michel M. Valuing human life: estimating the present value of lifetime earnings, 2000. Available at: http://repositories.cdlib.org/ctcre/esarm/PVLE2000. Accessed February 7, 2004.
- 33.Palmer C, Revicki D, Halpern M, Hatziandreu E. The cost of suicide and suicide attempts in the United States. Clin Neuropharmaco. 1995;18(3): S25–S33. [Google Scholar]
- 34.Centers for Disease Control and Prevention, National Centers for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) [online]. Available at: http://www.cdc.gov/ncipc/wisqars. Accessed February 1, 2005.
- 35.Centers for Disease Control and Prevention. Years of potential life lost before ages 65–85—United States 1989–1990. Atlanta, GA. MMWR Morb Mortal Wkly Rep. 1992;41: 313–315. [PubMed] [Google Scholar]
- 36.Centers for Disease Control. Leads from the morbidity and mortality weekly report, Atlanta, GA. Firearm-related years of potential life lost before age 65 years—United States, 1980–1991. MMWR Morb Mortal Wkly Rep. 1994; 272:1246–1248. [Google Scholar]
- 37.Selik RM, Chu SY. Years of potential life lost because of HIV infection in the United States. AIDS. 1997;11: 1635–1639. [DOI] [PubMed] [Google Scholar]
- 38.Romeder JM, McWhinnie JR. Potential years of life lost between ages 1 and 70: an indicator of premature mortality for health planning. Int J Epidemiol. 1977;6:143–51. [DOI] [PubMed] [Google Scholar]
- 39.A Health Status Indicator for Targeting Federal Aid to States (GAO report no. GAO/HEHS-97–13). Gaithersburg, MD: General Accounting Office; 1996.
- 40.Stack S. Suicide: a fifteen year review of the sociological literature. Suicide Life Threat Behav. 2000;30: 145–162. [PubMed] [Google Scholar]
- 41.Arnesen T, Nord E. The value of DALY life: problems with ethics and validity of disability adjusted life years. BM. 1999;319:1423–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gould MS, Greenbergt T, Velting Dm, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psych. 2003;42(4):386–405. [DOI] [PubMed] [Google Scholar]
- 43.Zenere FJ, Lazarus PJ. The decline of youth suicidal behavior in an urban, multicultural public school system following the introduction of a suicide prevention and intervention program. Suicide Life Threat Behav. 1997;27(4): 387–402. [PubMed] [Google Scholar]
- 44.Eggert LL, Thompson EA, Herting JR, Nicholas LJ. Reducing suicidal potential among high-risk youth: tests of a school-based prevention program. Suicide Life Threat Behav. 1995;25(2): 276–296. [PubMed] [Google Scholar]
- 45.Randell BP, Eggert LL, Pike KC. Immediate post intervention effects of two brief youth suicide prevention interventions. Suicide Life Threat Behav. 2001;31(1):41–61. [DOI] [PubMed] [Google Scholar]
- 46.Metha A, Weber B, Webb LD. Youth suicide prevention: a survey and analysis of policies and efforts in 50 states. Suicide Life Threat Behav. 1998; 28(2):150–164. [PubMed] [Google Scholar]
- 47.Conwell Y. Management of suicidal behavior in the elderly. Psychiatr Clin North Am. 1997;20(3):667–683. [DOI] [PubMed] [Google Scholar]
- 48.Bruce ML, Pearson J. Designing and intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial). Dialogues Clin Neurosci. 1999;1: 100–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bruce ML, Ten Have TR, Reynolds CF, et al. Alexopoulos GS. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. JAMA. 2004;291(9):1081–1091. [DOI] [PubMed] [Google Scholar]
- 50.Lebowitz BD, Pearson JL, Schneider LS, et al. Diagnosis and treatment of depression in late life: consensus statement update. JAMA. 1997;278: 1186–1190. [PubMed] [Google Scholar]
- 51.Brown G, Bruce M, Pearson J. High-risk management guidelines for elderly suicidal patients in primary care. Int J Geriatr Psychiatry. 2001;16: 593–601. [DOI] [PubMed] [Google Scholar]
- 52.Heart Disease and Stroke Statistics—2003 Update. Dallas, TX: American Heart Association; 2002.
- 53.Bennett S, Coggan C, Adams P. Problematising depression: young people, mental health and suicidal behaviors. Soc Sci Med. 2003;57: 289–299. [DOI] [PubMed] [Google Scholar]
- 54.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: A consensus statement. JAMA. 2003;289:3161–3166. [DOI] [PubMed] [Google Scholar]
- 55.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997; 170:205–228. [DOI] [PubMed] [Google Scholar]
- 56.Neeleman J, Wessely S, Wadsworth M. Predictors of suicide, accidental death, and premature natural death in a general population birth cohort. Lancet. 1998;351:93–97. [DOI] [PubMed] [Google Scholar]
- 57.The Global Burden of Disease. Geneva, Switzerland: World Health Organization; 2002.
- 58.Goldney RD, Wilson D, Dal Grande E, Fisher LJ, McFarlane AC. Suicidal ideation in a random community sample: attributable risk because of depression and psychosocial and traumatic events. Aust N Z J Psychiatr. 2000;34:98–106. [DOI] [PubMed] [Google Scholar]
- 59.Stewart WF, Ricci JA, Chee E. Hahn SR, Morganstein D. Cost of lost productive work time among UW workers with depression. JAMA. 2003;289: 3135–3144. [DOI] [PubMed] [Google Scholar]
- 60.Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Year Book Psychiatry Appl Mental Health. 1999;5:214–215. [Google Scholar]
- 61.Goldberg RJ, Steury S. Depression in the workplace: costs and barriers to treatment. Psychiatric Services. 2001;52: 1639–1643. [DOI] [PubMed] [Google Scholar]
- 62.Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA. 1990;264:2524–2528. [PubMed] [Google Scholar]
- 63.Rabinowitz ZJ, Gross R. Felman D. Correlates of a perceived need for mental health assistance and differences between those who do and do not seek help. Soc Psychiatry Psychiatr Epidemio. 1999;34:141–146. [DOI] [PubMed] [Google Scholar]
- 64.Riska E, Ettore E. Mental distress—gender aspects of symptoms and coping. Acta Oncol. 1999;38:757–761. [DOI] [PubMed] [Google Scholar]
- 65.Hobfall SE, Dunahoo CL, Ben-Porath Y, Zmonnier J. Gender and coping: the dual-axis model of coping. Am J Community Psychol. 1994;22:49–82. [DOI] [PubMed] [Google Scholar]
- 66.Bech P, Raaback OL, Rasmussen NA, Selin E, Rutz W, Zieran F. Male depression: stress and aggression as pathways to major depression. In: Dawson A, Tylee A, eds. Depression: Social and Economic Timebomb. London: BMJ Books; 2004:63–66.
- 67.Moller-Leimkuhler AM. Barriers to help-seeking by men: a review of socio-cultural and clinical literature with particular reference to depression. J Affect Disord. 2002;71:1–9. [DOI] [PubMed] [Google Scholar]
- 68.National Institutes of Mental Health. Real Men, Real Depression. Available at: http://menanddepression.nimh.nih.gov. Accessed February 7, 2004.


