Abstract
Objectives. We evaluated the effect of depression on risk, on the basis of standardized assessment, for developing activities of daily living (ADL) disability.
Methods. Depression-related risk on 2-year ADL disability is estimated from 6871 participants in a population–based national sample aged 54–65 years and free of baseline ADL disability. We evaluated the effects of factors amenable to clinical and public health intervention that may explain the relationship between depression and incident disability.
Results. The odds of ADL disability were 4.3 times greater for depressed adults than their non-depressed peers (95% confidence interval=3.1, 6.0). Among depressed adults, 18.7% of African Americans, 8.0% of Whites, and 7.8% of His-panics developed disability within 2 years. The attributable population fraction because of depression is 17.3% (95% confidence interval=11%, 24%). Concurrent health factors moderated depression-associated risk.
Conclusions. Elevated risk of ADL disability onset because of depression, in a cohort whose medical costs will imminently be covered via Medicare, is attenuated by factors amenable to public health intervention. Prevention and/or public health/policy programs that lead to more accessible and effective mental health and medical care could reduce the development of ADL disability among depressed adults.
Disability has large economic and societal costs among older adults.1–3 Medical spending among the elderly is related more strongly to the presence of disability than to remaining life expectancy.4,5 Among pre-retirement adults, limitations in life activities are strong determinants of job loss and the ability to find employment.6,7 Investigations of precursors for disability show depression is a leading cause.8–11 Numerous clinical, community, and epidemiological studies show that depressed adults have a higher frequency of disability than their non-depressed peers.8–18 However, these studies did not use representative national samples, thereby limiting the generalizability of those findings. Furthermore, race-specific estimates of increased risk from depression for future functional loss are scarce.
We attempted to answer three questions regarding differences related to depression as a risk factor for developing (incident) disability with a national sample of pre-retirement adults. First, to what extent do people with depression have increased risk for disability onset compared with their non-depressed peers in this pre-retirement cohort? Second, what are the race-specific risks from depression for incident disability? Third, to what extent are depression-related risks for developing disability explained by sociodemographic, health, or economic factors? Because greater burdens of health conditions,17,19–22 and fewer economic resources,19,23–25 are associated with both depression and disability, these factors may be entangled in observed differences on incident functional limitation. The influence of such factors will be evaluated on the risk attributed to depression for the development of disability in activities of daily living (ADL). Development of ADL disability is a serious concern because such impairment jeopardizes a person’s ability to live independently.
We addressed these questions with longitudinal data from the Health and Retirement Study (HRS). Because depression is both a risk factor and a product of disability, we separate out its predictive role by evaluating the impact of depression on the development of ADL disability among adults initially free of ADL task limitations. In contrast to studies that relied on clinical or community samples to evaluate the impact of depression on incident functional limitations, resulting in findings that cannot be generalized to other populations,26 we used a national probability sample. This largely pre-retirement HRS sample of older Americans (aged 54–65) is of particular interest because of the deleterious consequences from depression on function and health22,26 in a cohort at peak earnings potential whose medical costs will imminently be covered by public insurance via Medicare.
METHODS
Overview
We analyzed public data from the HRS, a prospective survey of community-dwelling pre-retirement adults. Biennial HRS interviews of this national probability sample began in 1992 and are ongoing.27 The third (1996) interview, used for the baseline of these analyses, included a one-time assessment for 12-month major depressive episodes with a short form of the Composite International Diagnostic Interview (CIDI-SF).28 The 1996 HRS cohort included 7922 self-respondents from the 1931–1941 birth cohort (aged 54–65 years at the time of the interview). Another 503 proxy interviews were handled analytically as 1996 HRS non-respondents. To make statements about incident ADL disability, we limited our analyses to a cohort of 6871 older adults without baseline ADL task limitations who lived for at least 2 years after the initial interview, excluding by design 416 persons reporting baseline ADL disability, and 141 decedents. For analytical purposes, we omitted an additional 451 non-respondents to the 1998 interview and 43 persons with insufficient baseline data on income, ethnicity/race, ADL, or marital status.
Outcome Variable
We ascertained ADL disability, on the basis of the Institute of Medicine classification,29 from responses to questions asking about the inability to perform functional tasks at the personal level. Examples of basic ADL disability include the inability to dress, toilet, bathe, eat, walk across a room, and transfer in and out of bed. Disability in an ADL task expected to last ≥ 3 months was on the basis of affirmative responses to inability, avoidance, receiving help, or using equipment to perform the task. This assessment captures chronic dependence in basic self-care tasks that could jeopardize a person’s ability to live independently. The study cohort was restricted to those reporting no 1996 ADL disability. We identified ADL disability onset by the report of ≥ 1 ADL task disabilities at the subsequent 1998 interview.
Explanatory Variables
Depression refers to a major depression episode30 measured by means of a short form of the World Health Organization CIDI (CIDI-SF).31 The full World Health Organization CIDI has excellent validity and reliability32,33 among individuals of different nationalities and is currently the most widely accepted method to determine the prevalence of psychiatric disorders in the United States using lay interviewers.34 The CIDI-SF retains only those questions needed to ascertain diagnoses described in the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition (DSM-III-R ) of the American Psychiatric Association using a 12-month time frame to capture current depression, reorganize questions to minimize interview burden, and establish reliability.35,36 Following recommended guidelines, a major depressive episode is attributed to a CIDI-SF score of ≥ 3 symptoms from a 0–7 scale.37
Sociodemographic characteristics included race/ethnicity, age, gender, and marital status (married, divorced/widowed, never married/other), family structure (children, grandchildren, parents, parental caregiver), and whether a person lived alone. We used HRS ethnicity/race information to classify people into four mutually exclusive groups: (non-Hispanic) African American, Hispanic, (non-Hispanic) White, and other.
We assessed health needs from self-reported information on chronic conditions, functional limitations, and higher-level instrumental activities of daily living (IADL) disability. Chronic conditions were ascertained from a self-report of a physician diagnosis of conditions that included arthritis or rheumatism (hereafter called arthritis), cancer, cardiovascular disease (hypertension, heart attack, coronary artery disease, congestive heart failure, angina, other heart disease, stroke), diabetes, or lung disease. Obesity was defined as body mass index ≥ 30 (weight [kg])/(height [m]),2 calculated from self-reported height and weight. We determined functional limitations from reports of difficulty, inability, or avoidance of four physical tasks (walking several blocks, climbing several flights of stairs without resting, pulling or pushing large objects, lifting or carrying weights > 10 pounds). We ascertained IADL disability from affirmative responses to inability, avoidance, receiving help with tasks including hot meal preparation, shopping, using the telephone, taking medication, or managing money.
Economic access factors included education, wealth, and family income and health insurance. Education, a measure of human capital, was dichotomized as ≥ 12 versus fewer completed years of education. For analytical purposes, family income (all sources received by the respondent and spouse/partner during the preceding year) and wealth were dichotomized using the lowest 1996 HRS population-weighted quartiles of $19768 and $47000, respectively. If only partial income or wealth information was provided, dichotomized values were on the basis of imputed estimates developed at the University of Michigan.38 Health insurance information distinguished private insurance holders from reliance solely on Medicaid, Medicare, and other health insurance (e.g., insurance through the Department of Veterans Affairs).
Statistical Analysis
The HRS is a national probability sample. All analyses use person-weights, stratum, and sampling error codes for the 1996 HRS data developed at the University of Michigan39 to provide valid inferences to the US population.
Multiple logistic regression analyses model the relationship of depression to the probability of ADL disability onset with control for sociodemographic, health, and economic explanatory factors. Logistic regression odds ratios and 95% confidence intervals (CIs) are estimated by Taylor series methods with between-cluster robust estimation to adjust for the complex sampling design using SUDAAN software.40,41 Direct standardization methods42 illustrate the mediating effect of explanatory factors on the relationship between depression and incident ADL disability onset, in reference to the non-depressed HRS sub-population. The attributable risk is the absolute risk difference in ADL onset rates. The population attributable fraction of incident ADL disability because of depression is estimated by the formula [Ie—Iu] × [Prev/Ic], where ADL is incident disability among persons exposed to the risk factor (depression), Iu is ADL disability incidence in the unexposed group, Prev is the risk factor prevalence, and Ic is ADL disability incidence in the cohort.43
Analyses are restricted to 1996–1998 HRS respondents. Non-respondents compared with respondents tended to disproportionately be African American (12.3% vs 9.0%) or Hispanic (9.9% vs 6.8%) adults. We adjusted for potential bias because of non-response by handling respondents as an additional sampling stage to obtain adjusted sampling weights, by means of standard sampling methodology.42 All statistical testing was done at a nominal 5% α significance level.
RESULTS
Baseline characteristics from the 6871 members of the 1996 HRS cohort (aged 54–65 years) at risk for developing ADL disability are shown in Table 1 ▶. A total of 7.0% of this cohort met the study criteria for depression at the baseline interview (African Americans, 6.6%; Hispanics, 8.3%; Whites, 6.9%). Depressed adults were similar in race/ethnicity to the non-depressed cohort members. However, as expected, persons with depression were more likely to live alone, report chronic conditions (particularly cancer and lung disease), report IADL disability or multiple functional limitations, and have fewer economic resources in terms of income, wealth, or reliance on government health insurance (e.g., Medicaid) compared with those who were not depressed.
TABLE 1—
Baseline Depression and ADL Disability Onset among 6871 Participants in the 1996 HRS at Risk of Incident ADL by Baseline Characteristics
| Sample Size | |||
| n | Population, % | Depression Population, % | |
| Overall | 6871 | 100.00 | 7.00 |
| Sociodemographic factors | |||
| Race/ethnicity | |||
| African American | 1027 | 9.05 | 6.64 |
| Hispanic | 549 | 6.80 | 8.34 |
| White | 5178 | 82.10 | 6.88 |
| Other | 117 | 2.05 | 9.05 |
| Female gender | 3853 | 52.22 | 8.97 |
| Male gender | 3018 | 47.78 | 4.85 |
| Lives alone | 1001 | 14.21 | 10.63 |
| Health Factors | |||
| Chronic conditions | |||
| None | 1491 | 23.11 | 3.30 |
| Arthritis | 3317 | 47.11 | 9.31 |
| Cancer | 486 | 7.12 | 10.13 |
| Diabetes | 829 | 10.86 | 9.03 |
| Cardiovascular disease | 3362 | 47.34 | 9.20 |
| Lung disease | 531 | 7.85 | 14.71 |
| Obesity | 1732 | 23.36 | 8.62 |
| Higher-level impairment | |||
| Functional limitation | |||
| One | 1458 | 20.70 | 6.51 |
| Multiple | 1750 | 24.00 | 16.08 |
| IADL disability | 254 | 3.76 | 17.58 |
| Economic Factors | |||
| Education < 12 y | 1735 | 23.49 | 9.46 |
| Household income lowest quartile | 1770 | 23.20 | 11.90 |
| Family wealth lowest quartile | 1788 | 23.24 | 11.90 |
| Health insurance | |||
| Private (employer/other) | 5309 | 79.22 | 5.52 |
| Government onlya | 824 | 11.08 | 15.27 |
| No health insurance | 722 | 9.42 | 9.83 |
| Missing | 16 | 0.28 | 4.15 |
aMedicare/Medicaid, other federal agency.
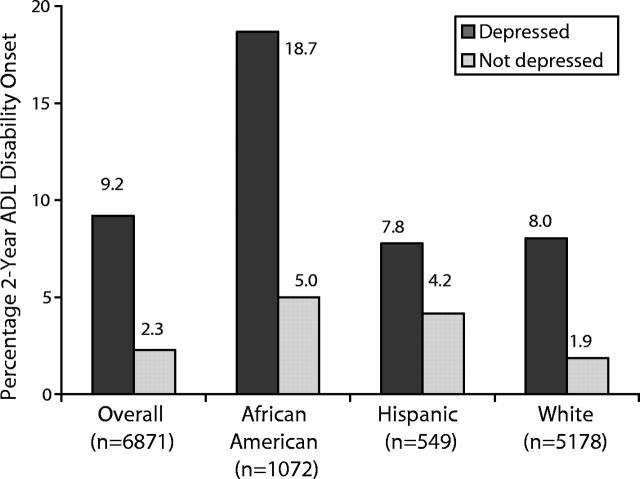
Overall, 2.8% of this cohort, free of ADL disability at baseline, reported limitations 2 years later. Substantially higher 2-year ADL incident disability rates (9.2% vs 2.3%; attributable risk, 6.9%) were experienced by those with baseline depression compared with those without depression (Figure 1 ▶). The depression population attributable fraction was 17.3% (95% CI=11.0, 23.6), indicating that nearly one in five new cases of ADL disability in this cohort is associated with depression.
FIGURE 1—
Two-year rates in the onset of ADL limitations by baseline depression status stratified by race/ethnicity from HRS participants aged 54–65.
ADL disability incidence was ~2–2.5 times greater among minorities (African Americans, 5.9%; Hispanics, 4.5%) compared with Whites (2.3%). Depression was a strong risk factor for the development of disability across all racial/ethnic groups. The rates of incident ADL disability were approximately four times greater for depressed African Americans (18.7% vs 5.0%; attributable risk, 13.5%) and Whites (8.0% vs 1.9%, attributable risk, 6.1%) and almost doubled for His-panics (7.8% vs 4.2%, attributable risk, 3.2%) compared with their non-depressed peers. The depression population attributable fraction in African Americans (15.4%; 95% CI= 1.9, 28.9) and Whites (18.4%; 95% CI= 10.6, 26.1) were similar and lower among Hispanics (6.7%; 95% CI= −9.3, 22.7). The numbers of depressed people of other race/ethnicities (n=12) were too small to validly estimate ADL disability incidence.
Some factors related to higher depression frequency, such as living alone, greater health burdens, and fewer economic resources, may also be risk factors for developing ADL disability. We evaluated the potential contribution of such factors to explain the increased risk of ADL disability onset among people with depression. For this purpose, we calculated standardized ADL disability incidence rates for people with and without depression (Table 2 ▶). Standardized disability incidence rates first adjust for sociodemographic factors and then additionally control for health (factors potentially amenable to clinical and pubic health intervention) and economic (factors potentially amenable to public policy intervention) factors. Two-year ADL disability onset in the non-depressed reference group was 23.0 per 1000, consistent with Figure 1 ▶. The standardized 2-year ADL disability incidence related to depression, 92.0 per 1000, was reduced 7% (to 85.1 per 1000) when sociodemographic factors were taken into account. Controlling additionally for chronic conditions reduced the standardized incidence another 27% (to 60.1 per 1000). Further adjustment for functional limitation and higher-level IADL disability reduced the depression standardized ADL disability rate 15% more (to 46.6 per 1000). Together, chronic conditions and higher-level limitation health factors explained over half the excess disability incidence related to depression. Finally, adjustment for economic differences reduced rates 3% more (to 43.5 per 1000). These findings show that substantial excess risk from depression is related to the greater burden of health needs experienced by depressed adults compared with their non-depressed peers.
TABLE 2—
Two-Year Standardized Rates in the Onset of ADL Disability by Baseline Depression Status with and without Adjustment Factors
| Adjustment Factors | Not Depressed | Depressed |
| Unadjusted | 23.03 | 91.95* |
| Sociodemographica | 23.03 | 85.07* |
| Chronic conditionsb | 23.03 | 60.10* |
| Higher-level impairmentsc | 23.03 | 46.62* |
| Economic factorsd | 23.03 | 43.45* |
Note. The onset rate is per 1000 respondents.
aControl for sociodemographic factors (race/ethnicity, age, gender, marital status, live alone, children, grandchildren, living parent(s), caregiver for parent(s)).
bControl for sociodemographics plus chronic conditions (arthritis, cancer, cardiovascular disease [heart disease, hypertension, stroke], diabetes, lung, stroke, obesity).
cControl for sociodemographics plus chronic conditions plus higher-level impairment (functional limitations, IADL disability).
dControl for sociodemographics plus chronic conditions plus higher-level impairment plus economic factors (education, income, wealth, private/other/missing, government, no health insurance).
* P ≤ .05.
Large risk reductions related to health factors in standardized rates may be partially attributable to an association between health and economic characteristics. Sensitivity analyses that entered health factors last after control for economic factors still showed these factors reduced excess disability incidence rates related to depression by one-third. Other sensitivity analyses repeated Table 2 ▶ analyses using a more stringent criterion (CIDI-SF≥ 5) recommended by some researchers35 to ascertain major depression. Under this definition, the unadjusted 2-year rate for incident ADL disability among adults with baseline depression increased to 110.6 per 1000, depression persisted as an independent risk factor for developing ADL limitations, and health factors substantially explained elevated depression risk.
We measured the effect of depression on the onset of ADL disability adjusting for sociodemographic, health need, and economic factors by the magnitude of adjusted odd ratios estimated from sequential multiple logistic regression models (Table 3 ▶). Depression remained a strong and significant risk factor (adjusted odds ratio=2.0; CI=1.3, 3.1) for the development of ADL disability after control for differences in sociodemographics, health, and economic factors. The full multiple logistic model (data not shown) also indicated that ADL disability onset was significantly more likely among African Americans (adjusted odds ratio=1.7; CI=1.2, 2.4) after accounting for other risk factors.
TABLE 3—
Depression Odds Ratio for 2-Year ADL Disability Onset (n = 6871)
| Adjustment Factors | Odds Ratio | 95% CI |
| Unadjusted | 4.30 | 3.07, 6.00 |
| Sociodemographica | 4.01 | 2.81, 5.73 |
| Chronic conditionsb | 2.83 | 1.89, 4.25 |
| Higher-level impairmentc | 2.19 | 1.46, 3.30 |
| Economic accessd | 2.04 | 1.34, 3.09 |
aControl for sociodemographic factors (race/ethnicity, age, gender. marital status, live alone, children, grandchildren, living parent(s), caregiver for parent(s)).
bControl for sociodemographics plus chronic conditions (arthritis, cancer, cardiovascular disease [heart disease, hypertension, stroke], diabetes, lung, stroke, obesity).
cControl for sociodemographics plus chronic conditions plus higher-level impairment (physical, IADL).
dControl for sociodemographics plus chronic conditions plus higher-level impairment plus economic factors (education, income, wealth, private/other/missing, government, no health insurance).
Recognizing that depression is more common among women than men and among minorities than Whites (Table 1 ▶), additional analyses (data not shown) investigated whether the effect of depression on ADL disability onset differed by gender or by race. Depression interaction terms with gender and racial/ethnicity added to the full multiple logistic regression model were not statistically significant. This analysis indicates that the effect of depression on ADL disability onset is similar across gender and racial/ethnic groups after control for differences in sociodemographic, health need, and economic factors.
DISCUSSION
We have provided evidence of a substantial national public health burden related to depression in the development of ADL disability among US adults aged 54–65 years. Nearly 1 of every 5 new cases of ADL disability is associated with depression. Almost 1 in 10 depressed adults who previously had no ADL disability reported dependence in ≥ 1 ADL tasks within 2 years, which is an impressively high disability incidence rate among a relatively young group of older adults.
Depression increases the odds of developing ADL disability across racial/ethnic and gender groups, demonstrating the importance of treating depression for all adults. The risk for developing ADL disability within 2 years was more than four times greater for depressed adults compared with their non-depressed peers and remained significant after control for differences in other investigated risk factors. However, the prospect of developing ADL disability is particularly devastating for depressed African Americans. Almost 1 in 5 depressed African Americans developed disability compared with only 1 in 20 of their non-depressed peers. Although the effect of depression on the increase in the odds for developing disability is similar for older African Americans and Whites, the attributable risk was more than doubled in African Americans compared with Whites. From a public health viewpoint, African Americans start with the greatest risk for developing disability; the addition of depression substantially accentuates the disability toll among African Americans. The high disability incidence rates among depressed African Americans make depression an important target for public health efforts to reduce disparities in disability.
Although the relationship between depression and functional limitations is fairly well established, the direction of this relationship is potentially complex because of the nature of depression.44 Experiencing limits in functioning may increase stress, thereby producing depressive reactions.45 Alternatively, it may be that persons experiencing depression have a greater risk for the development of functional impairments as a secondary effect of the retarding effects of depression (e.g., less physical activity, lower compliance with treatment recommendations46,47). This national study provides methodologically strong evidence on depression as a precursor of ADL disability, which is important information to promote depression as a public health priority for intervention and prevention programs.
The finding that depression was an independent predictor for developing ADL disability after accounting for sociodemograhic, health, and economic factors is consistent with findings from the older cohorts (65 years and older) of the Established Populations for Epidemiological Studies of the Elderly (EPESE).10,22 Similar to those studies, only a small part of the association of depression with subsequent ADL disability was explained by sociodemographic factors. The current study demonstrated that chronic conditions accounted for a substantial portion of the association between depression and future ADL disability among this nationally representative cohort (aged 54–65 years). Accounting for functional limitations and IADL disability further attenuated the relationship of depression to incident ADL disability. Together, chronic conditions, functional limitations, and IADL disability explained as much as half the excess risk associated with depression.
Despite its strengths, several limitations common to secondary databases may affect the present findings. CIDI-SF assessment ascertains major depressive episodes within the past 12 months but does not distinguish between episodes that involve major depressive disorder, bipolar disorder, or psychotic disorder.28 Baseline factors were assessed cross-sectionally, so it is not known among those factors (especially health-related ones) which may be consequences or causes of depression. Self-reported measurement of limitations in function and IADL disability may not be as sensitive as objective measures (e.g., strength, balance, walking speed), which may result in underestimates of the portion of depression-related disability that is attributable to such factors. Our study lacked measures of disease severity. Also, the 1996 wave of the HRS was representative of people aged 55–65 years but not of those outside of this age range. Finally, we excluded decedents, which may result in underestimates of the relationship between depression and subsequent disability onset, because persons who pass through a period of disability before death are not observed.
Disability is a major driver of health care costs.4,5 Findings from this study show that nearly 1 of every 5 new cases of ADL disability is associated with depression in this cohort, whose medical costs will imminently be covered by public insurance via Medicare. These results point to the importance of treating depression in all adults to prevent the development of disability. Public health strategy should particularly target the treatment of depression among African Americans, for whom the risk of developing ADL disability is greatest. The powerful relationship of depression to incident ADL problems is partially explained by chronic illnesses, functional limitations, and IADL disability; these health problems are also amenable to medical and public health intervention. These results add ammunition to the call to address the prevention and effective treatment of chronic conditions and functional limitations as important components in the management of depression in older adults.14,48–50 The importance of managing a spectrum of clinical issues points to the value of systems–based medicine that evaluates depression and function, in addition to the presenting illness;51 such issues are often overlooked in an environment of specialized medicine.52,53 Public health and/or public policy programs that promote prevention and effective treatment of depression, chronic conditions, and functional impairments among adults may prevent the development of ADL disability, interrupting a costly spiral of health decline.
Acknowledgments
This work was supported by National Institutes of Health (NIH)/National Institute for Arthritis and Musculoskeletal Diseases grant P60 AR48098 and NIH/National Institute of Child Health and Human Development grant R01-HD45412.
We gratefully acknowledge the editorial contributions of Margaret Ring Gillock, MS. The Health and Retirement Study was sponsored by the National Institute on Aging and conducted by the University of Michigan.
Human Participant Protection This study received exemption from Human Subjects Review by the Northwestern University institutional review board for these analyses of public data.
Peer Reviewed
References
- 1.Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health.1996;17:25–46. [DOI] [PubMed] [Google Scholar]
- 2.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2000.
- 3.VonKorff M, Ormel J, Katon W, Lin EHB. Disability and depression among high utilizers of health care: a longitudinal analysis. Arch Gen Psychiatry.1992;49:91–100. [DOI] [PubMed] [Google Scholar]
- 4.Cutler DM. Disability and the future of Medicare. N Engl J Med.2003;349:1084–1085. [DOI] [PubMed] [Google Scholar]
- 5.Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. N Engl J Med.2003;349:1048–1055. [DOI] [PubMed] [Google Scholar]
- 6.Yelin EH, Katz PP. Making work more central to work disability policy. Milbank Q.1994;72:593–619. [PubMed] [Google Scholar]
- 7.Wray LA. The role of ethnicity in the disability and work experience of preretirement-age Americans. Gerontologist.1996;36:287–298. [DOI] [PubMed] [Google Scholar]
- 8.Penninx BW, Guralnik JM, Bandeen-Roche K, et al. The protective effect of emotional vitality on adverse health outcomes in disabled older women. J Am Geriatr Soc.2000;48:1359–1366. [DOI] [PubMed] [Google Scholar]
- 9.Fried LP, Young Y, Rubin G, Bandeen-Roche K. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol.2001;54:889–901. [DOI] [PubMed] [Google Scholar]
- 10.Bruce ML, Seeman TE, Merrill SS, Blazer DG. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health.1994;84:1796–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ormel J, Vonkorff M, Oldehinkel AJ, Simon G, Tiemens BG, Uestuen TB. Onset of disability in depressed and non-depressed primary care patients. Psychol Med.1999;29:847–853. [DOI] [PubMed] [Google Scholar]
- 12.Beekman AT, Deeg DJ, van Tilburg T, Smit JH, Hooijer C, van Tilburg W. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord.1995;36:65–75. [DOI] [PubMed] [Google Scholar]
- 13.Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA.1989;262:914–919. [PubMed] [Google Scholar]
- 14.Steffens DC, Hays JC, Krishnan KR. Disability in geriatric depression. Am J Geriatr Psychiatry.1999;7:34–40. [PubMed] [Google Scholar]
- 15.Ormel J, VonKorff M, vanden Brink W, Katon W, Brilman E, Oldehinkel T. Depression, anxiety, and disability show synchrony of change. Am J Public Health.1993;83:385–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Callahan CM, Wolinsky FD, Stump TE, Nienaber NA, Hui SL, Tierney WM. Mortality, symptoms, and functional impairment in late-life depression. J Gen Intern Med.1998;13:746–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJ, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. JAMA.1998;279:1720–1726. [DOI] [PubMed] [Google Scholar]
- 18.Gallo JJ, Rabins PV, Lyketsos CG, Tien AY, Anthony JC. Depression without sadness: functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc.1997;45:570–578. [DOI] [PubMed] [Google Scholar]
- 19.Black SA, Markides KS, Miller TQ. Correlates of depressive symptomatology among older community-dwelling Mexican Americans: the Hispanic EPESE. J Gerontol B Psychol Sci Soc Sci.1998;53:S198–S208. [DOI] [PubMed] [Google Scholar]
- 20.Fernandez ME, Mutran EJ, Reitzes DC, Sudha S. Ethnicity, gender, and depressive symptoms in older workers. Gerontologist.1998;38:71–79. [DOI] [PubMed] [Google Scholar]
- 21.Aneshensel CS, Huba GJ. Depression, alcohol use, and smoking over one year: a four-wave longitudinal causal model. J Abnorm Psychol.1983;92:134–150. [DOI] [PubMed] [Google Scholar]
- 22.Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health.1999;89:1346–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krause N, Goldenhar LM. Acculturation and psychological distress in three groups of elderly Hispanics. J Gerontol.1992;47:S279–S288. [DOI] [PubMed] [Google Scholar]
- 24.Moscicki EK, Locke BZ, Rae DS, Boyd JH. Depressive symptoms among Mexican Americans: the Hispanic Health and Nutrition Examination Survey. Am J Epidemiol.1989;130:348–360. [DOI] [PubMed] [Google Scholar]
- 25.Kington RS, Smith JP. Socioeconomic status and racial and ethnic differences in functional status associated with chronic diseases. Am J Public Health.1997; 87:805–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnan KR, Delong M, Kraemer H, et al. Comorbidity of depression with other medical diseases in the elderly. Biol Psychiatry.2002;52:559–588. [DOI] [PubMed] [Google Scholar]
- 27.Heeringa S, Connor J. Technical Description of the Health and Retirement Study Sample Design. HRS Documentation. Ann Arbor, MI: Population Studies Center; 1995. HRS documentation report DR-002.
- 28.Documentation of Affective Functioning Measures in the Health and Retirement Survey. Ann Arbor, MI: University of Michigan, Survey Research Center; 2000. Publication DR-005.
- 29.Institute of Medicine. Disability in America: Toward A National Agenda for Prevention. Washington, DC: National Academy of Sciences; 1991.
- 30.Mental Health: A Report of the Surgeon General. Rockville, MD: US Dept of Health and Human Services; 1999.
- 31.Wittchen H-U. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res.1994;28:57–84. [DOI] [PubMed] [Google Scholar]
- 32.Tacchini G, Coppola MT, Musazzi A, Altamura AC, Invernizzi G. Multinational validation of the Composite International Diagnostic Interview (CIDI) [in Italian]. Minerva Psichiatr.1994;35:63–80. [PubMed] [Google Scholar]
- 33.Wittchen HU. Reliability and validity studies of the WHO–Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res.1994;28:57–84. [DOI] [PubMed] [Google Scholar]
- 34.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Co-morbidity Survey. Arch Gen Psychiatry.1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 35.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr.1999;11:139–148. [DOI] [PubMed] [Google Scholar]
- 36.Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). Int J Methods Psychiatr Res.1998;7:171–185. [Google Scholar]
- 37.Nelson CB, Kessler RC, Mroczek D. Scoring the World Health Organization’s Composite International Diagnostic Interview Short Form (CIDI-SF; v1.0 NOV98). Available at: http://www3.who.int/cidi.
- 38.Smith JP. Wealth inequality among older Americans. J Gerontol B Psychol Sci Soc Sci.1997;52(Spec No.): 74–81. [DOI] [PubMed] [Google Scholar]
- 39.Health and Retirement Study. Sampling Weights Revised for Tracker 2.0 and Beyond. Ann Arbor, MI: University of Michigan, Survey Research Center; 2002.
- 40.Shah BV, Barnwell BG, Bieler GS. SUDAAN User’s Manual Release 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997.
- 41.Williams R. A note on variance estimation for cluster-correlated data. Biometrics.2000;56:218–219. [DOI] [PubMed] [Google Scholar]
- 42.Korn EL, Graubard BI. Analysis of Health Surveys. New York: John Wiley and Sons, Inc; 1999.
- 43.Rothman KJ. Epidemiology: An Introduction. New York: Oxford Press; 2002.
- 44.Graney MJ. The reciprocal relationship between disability and depression. J Am Geriatr Soc.2000;48:452–453. [DOI] [PubMed] [Google Scholar]
- 45.Mazure CM, Maciejewski PK, Jacobs SC, Bruce ML. Stressful life events interacting with cognitive/personality styles to predict late-onset major depression. Am J Geriatr Psychiatry.2002;10:297–304. [PubMed] [Google Scholar]
- 46.Farmer ME, Locke BZ, Moscicki EK, Dannenberg AL, Larson DB, Radloff LS. Physical activity and depressive symptoms: the NHANES I Epidemiologic Follow-up Study. Am J Epidemiol.1988;128:1340–1351. [DOI] [PubMed] [Google Scholar]
- 47.Elliott R, Sahakian BJ, McKay AP, Herrod JJ, Robbins TW, Paykel ES. Neuropsychological impairments in unipolar depression: the influence of perceived failure on subsequent performance. Psychol Med.1996;26:975–989. [DOI] [PubMed] [Google Scholar]
- 48.Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community: themes for the new century. Psychiatr Serv.1999;50:1158–1166. [DOI] [PubMed] [Google Scholar]
- 49.Katz IR. Depression as a pivitor component in secondary aging: opportunities for research, treatment, and prevention. In: Lomranz J, ed. Handbook of Aging and Mental Health: An Integrative Approach. New York: Plenum Press; 1998:463–482.
- 50.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry.2001;9:102–112. [PubMed] [Google Scholar]
- 51.Valenstein M, Vijan S, Zeber JE, Boehm K, Buttar A. The cost-utility of screening for depression in primary care. Ann Intern Med.2001;134:345–360. [DOI] [PubMed] [Google Scholar]
- 52.Wenger NS, Solomon DH, Roth CP, et al. The quality of medical care provided to vulnerable community-dwelling older patients. Ann Intern Med.2003;139:740–747. [DOI] [PubMed] [Google Scholar]
- 53.Fried LP. Establishing benchmarks for quality care for an aging population: caring for vulnerable older adults. Ann Intern Med.2003;139:784–786. [DOI] [PubMed] [Google Scholar]