Abstract
Objectives. I assessed recent trends in prevalence of any contact with mental health professionals and nonuse of mental health care or prescription medications owing to cost among adults with significant psychological distress.
Methods. In samples drawn from the National Health Interview Survey of 1997–2002, multiple logistic regression analysis was used to examine the association of survey year with mental health professional contacts and nonuse of mental health care or prescription medications owing to cost.
Results. The prevalence of any contact with mental health professionals increased from 29.1% in 1997 to 35.5% in 2002 (P<.05). The prevalence of nonuse of services because of cost also increased—from 15.6% to 20.0% for mental health care (P<.05) and from 27.7% to 34.1% for medication use (P<.001). Age, racial/ethnic, income, and insurance status disparities in receiving care persisted over the study period.
Conclusions. The number of individuals in need of mental health care who contacted mental health professionals grew in recent years, as did the number of individuals who encountered cost barriers to such care. Barring dramatic improvements in health insurance coverage, more individuals will likely face such barriers in coming years.
The burden of unmet need for mental health care in the community figured prominently in 2 recent, highly publicized government reports: the President’s New Freedom Commission on Mental Health report1 and the surgeon general’s report on mental health.2 While drawing attention to existing deficiencies, disparities, and barriers, both reports put forward a hopeful vision for the future of mental health care in the United States and proposed ways to realize that vision. Consistent with this view, some studies suggested improvements in the community care of serious mental conditions in recent years.3–5 The introduction of new medications with fewer side effects, the development and dissemination of evidence-based guidelines for treatment of common mental disorders, and changes in public attitudes toward mental illness6 may have contributed to these trends.
However, anecdotal reports and observations by administrators involved in the day-to-day workings of the mental health care system present a less optimistic picture.7,8 A recent commentator described how cuts in the public hospital beds across the country, disenrollment of many providers from Medicaid, and rising costs of medications have led to a crisis in access to mental health care for individuals who need such care.7 These problems are likely compounded by the general problems affecting the US health care system, such as the growing overall cost of medical care, the enduring problem of the uninsured and the underinsured, and the endemic social disparities in access and distribution of resources.9
Because of the paucity of systematic recent data, the overall impact of these conflicting influences on access to needed mental health services in the community is difficult to surmise. My study addresses this deficiency in data by examining recent trends in prevalence of any contact with mental health professionals and in financial barriers to care among individuals in need of such services in the community. Three specific study questions were posed regarding samples of individuals with psychological problems drawn from the general population: (1) Did the proportion of individuals who had any contact with a mental health professional in the past year change between 1997 and 2002? (2) Did the proportion of individuals who reported forgoing mental health care because of cost change in these years? (3) Did the proportion of individuals who reported forgoing use of prescription medications because of cost change in these years?
METHODS
Samples
Data for this study were drawn from 6 years of the National Health Interview Survey (NHIS) conducted between 1997 and 2002. The design of NHIS has been described previously in much detail.10–12 final response rates for sample adult interviews = 69.6%–80.4%). All interviews were conducted with the Computer-Assisted Personal Interviewing system.11,12
Assessments
Significant psychological distress.
Need for mental health care was operationalized by the presence of significant psychological distress, as ascertained by K6, a standardized screening instrument.13,14 K6 rating is the summary score of 6 items, assessing nonspecific psychological distress over the past 30 days (contact author for available appendix). Items are rated on a Likert scale from “none” (= 0) to “all the time” (= 4). The summary K6 score, thus, can range from 0 to 24.
K6 was developed by means of modern item response theory methods to select items with optimal sensitivity in the 90th to 99th percentile range of psychological distress in the general population with consistent psychometric properties across sociodemographic groups.13,14 In a 2-stage clinical reappraisal study, K6 was shown to have acceptable psychometric properties to detect serious mental illness (SMI) in the community.13 SMI was defined as a condition meeting the criteria of 1 of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV ) disorders as ascertained by the Structured Clinical Interview for DSM-IV (SCID)15 and a score of 60 or less on the Global Assessment of Functioning Scale (GAF).16 In receiver operating characteristics (ROC) curve analyses,17 K6 had an area under curve of 0.86. Area under curve can be interpreted as the probability of correctly distinguishing a randomly chosen individual with SMI from another randomly chosen individual without SMI.18
On the basis of ROC curve analysis, a score of ≥ 13 on K6 was selected as the optimal cut-point that equalizes false-positive and false-negative results.13 This cutpoint is associated with a sensitivity of 0.36, a specificity of 0.92, and a total classification accuracy of 0.92. This cutpoint was used in the present study to define significant psychological distress, signifying need for mental health care. Although, because of low sensitivity, many cases of SMI may not be detected; because of high specificity, the vast majority of the cases that are detected would meet the DSM-IV/SCID criteria for SMI.
Contact with mental health professionals.
Any contact with mental health professionals in the past year was assessed by 1 question out of a set of questions about health care received from various providers:
“During the past 12 months have you seen or talked to any of the following health care providers about your own health?
. . . A mental health professional such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker.”
Cost barriers to mental health care.
The following 2 questions out of a set of questions were used to assess cost barriers to mental health care:
“During the past 12 months, was there any time when you needed any of the following, but didn’t get it because you couldn’t afford it?
. . . Prescription medicines
. . . Mental health care or counseling.”
As is evident from the question above, prescription medications included all medications and were not limited to psychotropic medications.
Data Analysis
Before conducting the analyses, the data from the 6 years were combined according to the method recommended by the National Center for Health Statistics.12 Analyses were conducted with multivariate binary logistic regression models to adjust for variations in characteristics of samples across survey years. Three regression analyses were run in which the association of survey year (entered as a continuous variable ranging from 1 to 6) and each of the outcomes of interest were examined. The binary outcomes of interest were the following: any contact with a mental health professional, nonuse of mental health care/counseling because of cost, and forgone prescription medications because of cost. Variables of gender, race/ethnicity, age, household income compared with the federal poverty level (FPL), and current insurance type were also entered into each model to control for their effects. In addition to testing individual regression coefficients, the contributions of multicategory variables (e.g., race/ethnicity, insurance type) were examined with joint-hypothesis tests. Next, to assess whether or not time trends in contacts and in barriers were similar across sociodemographic groups, interaction terms between survey year and each variable were also tested. Regression analyses were limited to participants with significant psychological distress.
NHIS survey uses a complex sampling design. Therefore, frequency weights, strata, and primary sampling units were used in Stata 8.0 software19 to adjust the parameter estimates and their standard errors.
RESULTS
Characteristics of Participants With Significant Psychological Distress
Overall, 3.2% (N = 6640) of the participants across the 6 years were categorized as experiencing significant psychological distress. Compared with other survey participants, those with significant psychological distress were more likely to be female (65.1% vs 55.7%), from minority racial/ethnic groups (28.6% vs 24.1%), and in the 45- to 64-year age group (36.1% vs 28.6%). Participants with significant psychological distress were also more likely than other survey participants to fall in the < 100% or 199%-to-200% FPL income groups (27.6% compared with 10.0%, for the < 100% FPL group, and 22.7% compared with 14.4%, for the 199%–200% FPL group). All comparisons were statistically significant at the P < .001 level.
Contact With Mental Health Professionals
Between 1997 and 2002, the proportion of NHIS participants with significant psychological distress who reported that they had had any contact with a mental health professional in the past year grew from 29.1% to 35.5%. This change was statistically significant in the multiple regression model (Table 1 ▶). None of the interaction terms between participant characteristics and survey year in this regression model was statistically significant. However, there were significant main effects for race/ethnicity, age, and insurance. Participants from minority racial/ethnic groups were less likely than the non-Hispanic Whites (the reference group) to have had any contact with a mental health professional, as were participants in the ≥ 65-year age group compared with those in the 18- to 24-year age group (the reference group) and participants without insurance compared with those with private insurance coverage (the reference group), whereas participants in the 25- to 44-year age group were more likely than those in the 18- to 24-year age group to have had any contacts, as were participants with public insurance compared with those with private insurance (Table 1 ▶).
TABLE 1—
Correlates of Any Contact With Mental Health Professional, Not Affording Mental Health Care, and Not Affording Medications Among 6640 Participants of 1997–2002 NHIS With Significant Psychological Distress (K6 Score ≥ 13)
| Had Any Contact With a Mental Health Professional | Could Not Afford Mental Health Care in the Past Year | Could Not Afford Medications in the Past Yeara | ||||||||||
| B | SE | t test | AOR | B | SE | t test | AOR | B | SE | t test | AOR | |
| Survey year | 0.04 | 0.02 | 2.49* | 1.04 | 0.04 | 0.02 | 2.02* | 1.04 | 0.08 | 0.02 | 4.58*** | 1.09 |
| Gender | ||||||||||||
| Male | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . |
| Female | 0.03 | 0.07 | 0.51 | 1.03 | 0.20 | 0.08 | 2.54* | 1.22 | 0.30 | 0.08 | 3.94*** | 1.35 |
| Race/ethnicity | ||||||||||||
| Non-Hispanic White | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . |
| Non-Hispanic Black | –0.55 | 0.09 | 6.12*** | 0.58 | –0.21 | 0.11 | 1.99* | 0.81 | –0.08 | 0.09 | 0.90 | 0.92 |
| Hispanic | –0.58 | 0.08 | 7.33*** | 0.56 | –0.69 | 0.11 | 6.17*** | 0.50 | –0.55 | 0.10 | 5.63*** | 0.58 |
| Other | –0.45 | 0.20 | 2.27* | 0.64 | –0.36 | 0.21 | 1.69 | 0.70 | 0.14 | 0.17 | 0.85 | 1.15 |
| Joint-hypothesis test | Design-based F = 23.40*** | Design-based F = 13.09*** | Design-based F = 11.67*** | |||||||||
| Age, y | ||||||||||||
| 18–24 | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . |
| 25–44 | 0.32 | 0.12 | 2.67** | 1.37 | 0.21 | 0.14 | 1.50 | 1.24 | 0.17 | 0.12 | 1.41 | 1.19 |
| 45–64 | 0.10 | 0.12 | 0.78 | 1.10 | –0.00 | 0.14 | 0.03 | 0.99 | 0.16 | 0.13 | 1.21 | 1.17 |
| ≥ 65 | –1.48 | 0.17 | 8.68*** | 0.23 | –1.62 | 0.24 | 6.73*** | 0.20 | –1.20 | 0.19 | 6.46*** | 0.30 |
| Joint-hypothesis test | Design-based F = 59.51*** | Design-based F = 25.67*** | Design-based F = 32.48*** | |||||||||
| Household income, % FPLb | ||||||||||||
| < 100% | –0.10 | 0.10 | 1.02 | 0.91 | 0.19 | 0.12 | 1.58 | 1.20 | 0.73 | 0.09 | 7.79*** | 2.08 |
| 100–199% | –0.09 | 0.09 | 1.06 | 0.91 | 0.34 | 0.12 | 2.94** | 1.41 | 0.67 | 0.09 | 7.18*** | 1.95 |
| ≥ 200% | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . |
| Joint-hypothesis test | Design-based F = 0.99 | Design-based F = 3.60* | Design-based F = 32.33*** | |||||||||
| Current health insurance coverage | ||||||||||||
| Medicaid | 0.68 | 0.08 | 8.46*** | 1.97 | –0.19 | 0.11 | 1.71 | 0.83 | –0.12 | 0.10 | 1.21 | 0.89 |
| Medicare | 0.43 | 0.10 | 4.38*** | 1.54 | 0.29 | 0.13 | 2.26* | 1.34 | 0.56 | 0.10 | 5.69*** | 1.75 |
| No coverage | –0.39 | 0.09 | 9.04*** | 0.68 | 1.24 | 0.09 | 13.43*** | 3.46 | 1.44 | 0.07 | 18.59*** | 4.23 |
| Private/otherc | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . | Ref. | . . . | . . . | . . . |
| Joint-hypothesis test | Design-based F = 65.85*** | Design-based F = 76.75*** | Design-based F = 121.20*** | |||||||||
Note. B = regression coefficient; SE = standard error; AOR = adjusted odds ratio obtained in logistic regression analyses.
a These data present main effects of various predictors before entering the interaction term age × survey year.
bAcross the years, family incomes for 22.0% of NHIS participants could not be ascertained. However, these cases were not excluded from the analyses. Instead, they were combined with the reference group ( ≥ 200% FPL), which is the largest income group. The impact of this decision on the results of the analyses was assessed by entering a dummy variable for missing data into the regression models along with dummy variables for the < 100% FPL and 100%-to-199% FPL income groups. The dummy variable for missing income data was not significant in any of the models, justifying the decision to include them in the ≥ 200% FPL income group for these analyses.
c Includes employer-sponsored insurance, other private insurance, VA, Tricare, and other military insurance.
* P < .05; **P < .01; ***P < .001.
Cost-Related Barriers to Mental Health Care
Between 1997 and 2002, the proportion of NHIS participants with significant psychological distress who reported that they could not afford mental health care grew from 15.6% to 20.0%. This change was statistically significant in the multiple regression analysis (Table 1 ▶). None of the interaction terms between participant characteristics and survey year in this regression model was statistically significant. However, there were significant main effects for gender, race/ethnicity, age, income, and insurance. Participants from racial/ethnic minority groups compared with non-Hispanic Whites and participants in the ≥ 65-year age group compared with those in the 18- to 24-year age group were less likely to report not affording mental health care, whereas females compared with males, participants in the 100%-to-199% FPL income group compared with those in the ≥ 200% FPL income group (the reference group), and participants without insurance or with Medicare compared with those with private insurance, were more likely to report not being able to afford mental health care (Table 1 ▶).
Further analyses showed that the increase in the proportion of participants who reported not affording mental health care was limited to the group who had not had any contacts with a mental health professional in the past year. In this group, 11.4% in 1997 compared with 17.2% in 2002 reported not affording mental health care (P<.05). No significant differences across the years were noted among participants who had had any contact with a mental health professional, 25.7% of whom in 1997 and 25.0% in 2002 reported not affording mental health care. As these numbers indicate, overall, a larger proportion of participants who had had any contact with a mental health professional compared with those who had no such contact reported occasions of forgoing mental health care because of cost (25.3% vs 13.3%, respectively; P<.001).
Cost-Related Barriers to Prescription Medications
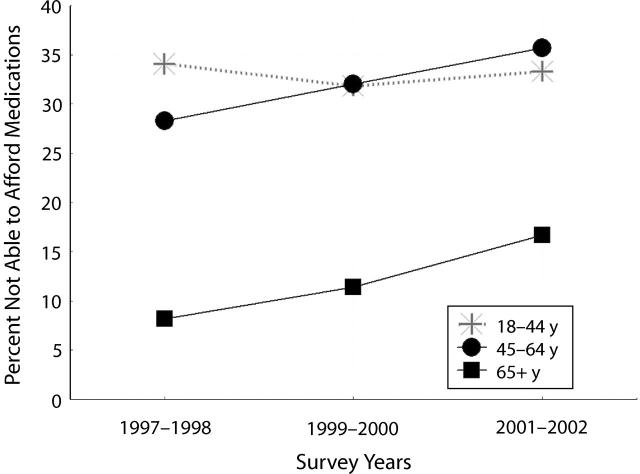
Between 1997 and 2002, the proportion of NHIS participants with significant psychological distress who reported that they could not afford medications grew from 27.7% to 34.1%. This increase was statistically significant in the multiple regression model including all survey years and adjusting for various sociodemographic characteristics of the samples (Table 1 ▶). Furthermore, the interaction between age and survey year was statistically significant (P < .001). Further regression analyses within each age group showed that the increase in the proportion of participants who reported not being able to afford medications was significant only in the 45- to 64-year and the ≥ 65-year age groups (both at P < .001 level) and was not significant in the 2 other age groups. This interaction effect is depicted in Figure 1 ▶.
FIGURE 1—
Percentage of 1997–2002 National Health Interview Survey participants who reported not being able to afford medications in the past year, by age group.
In addition, there were significant main effects for gender, race/ethnicity, age, income, and insurance on cost-related barriers to medications (Table 1 ▶). Hispanic participants compared with the non-Hispanic Whites and participants in the ≥ 65-year age group compared with those in the 18- to 24-year age group were less likely to report not affording medications. The main effect for the ≥ 65-year age group changed little after entering the interaction term with survey year in the regression model (B = −1.54, SE = 0.32, t = 4.83, P < .001, adjusted odds ratio = 0.21). As is apparent in Figure 1 ▶, individuals in the ≥ 65-year age group were consistently less likely to report not affording medications across survey years. Female participants compared with males, those in the < 100% and 100%-to-199% FPL income groups, compared with the ≥ 200% FPL income group, and participants without health insurance or with Medicare compared with those with private health insurance, were more likely to report not affording medications (Table 1 ▶).
DISCUSSION
The strengths of the NHIS data are representative sampling of the US population and the large sample size, as well as the use of the same questions for assessing psychological distress, contact with mental health professionals, and barriers across survey years.20 Nevertheless, these data have limitations and the results of the present study are constrained by these limitations. First, a large share of the mental health care provided in the community is delivered by primary care physicians and informal providers. NHIS does not collect information on these sources of mental health care. Nor does NHIS collect information on the number of visits with mental health professionals or the treatments received in these visits. Second, medication use and the type of medications were not assessed. Therefore, it is not clear what proportion of participants could not afford psycho-tropic medications specifically. Third, K6 items mostly assess depression and anxiety symptoms. Unfortunately, NHIS does not include measures of other forms of psychopathology. Fourth, perceived need for mental health care was not assessed. Individuals who perceive a stronger need for mental health care are more likely to seek care, or to seek a larger volume of care, and also more likely to face the barriers that limit access to such care. Thus, perceived need may explain the finding that individuals who had any contacts with mental health professionals were also more likely to report not affording such care. Finally, the questions about barriers asked if the participant had forgone “needed” mental health care or medications. Cultural factors likely influence how participants conceptualize and report “need” in this context.21 However, while these factors could potentially bias comparisons across racial/ethnic groups, it is unlikely that the time trends found in this study could be significantly biased because the same sampling and assessment methodology was used across survey years.
Despite these limitations, the findings of the study reveal important recent trends in access to outpatient specialty mental health care sector. The observed recent increase in the proportion of individuals with significant psychological distress who had any contact with a mental health professional is encouraging and suggests improvements in access. However, it is disconcerting that, as recently as 2002, about two thirds of adults with significant psychological distress received no professional mental health care.
The proportion of participants with significant psychological distress who reported not affording mental health services also grew. This increase was limited to those participants who had not had any contacts with mental health professionals in the past year, suggesting that financial barriers prevented these individuals from seeking such care. Cost of health care in the United States has grown at a faster pace than other consumer goods.9 As a result, cost is now a major barrier to access to mental health care.22 It is also notable that, even among individuals who had any contact with a mental health professional, a large proportion reported not affording mental health care/counseling. Thus, even in this group, cost barrier presents a major limitation to access to further needed care.
The well-known insurance, racial/ethnic, age, and income disparities in use of mental health services persisted through the study period. The effect of current insurance status on affordability of mental health care/counseling and prescription medications was larger than the effects of any other variable, as a cursory examination of odds ratios associated with this variable in Table 1 ▶ suggests. Furthermore, of all disparities in access to health services, the disparities due to lack of health insurance coverage or undercoverage are potentially the most straightforward to address administratively. Although ideological disagreements among policymakers and cost considerations preclude implementation of a universal health plan in near future, piecemeal solutions are possible. Currently, many states provide state-sponsored medication insurance plans for the near-poor. Extension of these plans to all states may ameliorate the cost barriers to medications in these income groups.
Racial/ethnic disparities in contact with mental health professionals persisted with little change across the survey years, as evidenced by the significant main effects and nonsignificant interaction terms in regression models. This finding is consistent with the results of the 2002 National Survey on Drug Use and Health (NSDUH), which reported significantly lower rates of 12-month treatment for mental health problems among minority groups,22 and it echoes recently voiced concerns about the lingering racial/ethnic disparities in access to mental health care.23,24 Furthermore, black and Hispanic participants were less likely to report not affording mental health care, and Hispanic participants were less likely to report not affording medications. It is unlikely that these findings indicate fewer cost barriers among the racial/ethnic minorities. The findings may simply indicate less demand for such services among minority groups. Unless an individual seeks needed services, he or she will not face barriers to such services.
Individuals in the ≥ 65-year age group were less likely to have contacts with mental health professionals than younger individuals. This may be because of less perceived need or better ability to cope with psychological distress in this age group. It may also be because of use of other formal or informal providers for mental health problems. For example, data from the Epidemiological Catchment Area (ECA) study suggest that older individuals with current psychiatric disorders are less likely than younger individuals to receive care in the mental health specialty sector and more likely to receive mental health treatment from general medical providers.25 Unfortunately, other sources of mental health care besides mental health professionals were not assessed in the NHIS survey. Perhaps as a result of less demand, the ≥ 65-year age group were also less likely to report that mental health care/counseling was unaffordable.
It is also notable that in the ≥ 65-year and the 45- to 64-year age groups, the proportion of subjects who reported not affording prescription medications grew between 1997 and 2002. As middle-aged and older individuals are more likely than other groups to use medications, these findings likely reflect the inordinate cost burden imposed on these age groups by the rapid rise of medication prices. Between 1997 and 2002, the national spending on prescription drugs more than doubled.26 Partly in response to the growing cost burden of medications for older age groups, the US Congress recently passed a Medicare prescription drug bill.27,28 Future research needs to assess the impact of this initiative on affordability of medications for the Medicare enrollees.
Income level had no impact on the probability of contact with a mental health professional. This is encouraging and suggests that use of mental health services is not significantly impeded by income inequality. However, participants in the 100%-to-199% income groups were more likely than those in the ≥ 200% income group to report forgoing mental health care because of cost and almost twice as likely to forgo medications. A similar effect with regard to affording medications was observed in the < 100% FPL income group. These findings, especially with regard to access to medications are cause for concern. In recent years, many new psychotropic medications with better side effect profiles have been introduced. However, the rapidly growing prices of these new medications increasingly limits their benefits only to population groups who can afford them.
The findings with regard to the effect of gender are puzzling. Female participants were not more likely to have any contact with a mental health professional, whereas they were more likely to forgo mental health care and medications because of cost. In past studies, females with mental health problems were generally more likely to perceive a need for professional help and to receive such help.29,30 However, females may be more likely to receive such help from general medical providers rather than from mental health professionals.31 Future research needs to explore trends in the use of medical services and informal providers for mental health complaints.
In conclusion, the trends in the use and cost barriers to mental health care presented here reflect the effects of the counteracting forces briefly discussed in the introduction of the paper. On the one hand, the demand for mental health care among individuals suffering from psychological problems seems to have increased in recent years. On the other hand, the growing costs of mental health care and prescription medications, without a corresponding increase in health insurance coverage, has led to a growing cost barrier to such services. Although the problem of unmet need for care and cost barriers is not unique to mental health care, the trends may be more pronounced in this area, as a recent report from the Community Tracking Study did not reveal significant increases in unmet need or cost barriers to medical care between 1997 and 2001.32
Barring unforeseeable developments—such as drastic improvements in the coverage of public insurance plans—the trends of the recent past are likely to continue in the near future. The demand for mental health care will likely grow, but so will the cost barriers to such care. It is also unlikely that the endemic socioeconomic disparities in access to needed mental health care will significantly decline in the near future. The technological advances in treatment of mental disorders will benefit most those individuals who can pay for these services or who are covered by generous insurance plans, whereas the growing demand for such services among the poor and the uninsured will increasingly face financial barriers.
Acknowledgments
This study was partly funded by a Research Scientist Career Development Award (K01-MH01754) from the National Institute of Mental Health, Bethesda, Md.
Human Participant Protection This report was based on secondary analyses of public access data from the National Health Interview Survey. The survey was conducted by the National Center for Health Statistics, Center for Disease Control and Prevention, Hyattsville, Md, and approved by the NCHS institutional review board.
Peer Reviewed
References
- 1.New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America. Final Report. Rockville, Md: US Dept of Health and Human Services; 2003. DHHS publication SMA 03-3832. Available at: http://www.mentalhealthcommission.gov/reports/FinalReport/downloads/downloads.html. Accessed August 18, 2005.
- 2.Mental Health: A Report of the Surgeon General. Rockville, Md: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 1999.
- 3.Olfson M, Marcus SC, Druss B, et al. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–209. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095–3105. [DOI] [PubMed] [Google Scholar]
- 5.Zuvekas SH. Trends in mental health services use and spending, 1987–1996. Health Aff. 2001;20: 214–224. [DOI] [PubMed] [Google Scholar]
- 6.Phelan JC, Link BG, Stueve A, et al. Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? J Health Soc Beh. 2000;41:188–207. [Google Scholar]
- 7.Appelbaum PS. The “quiet” crisis in mental health services. Health Aff. 2003;22:110–116. [DOI] [PubMed] [Google Scholar]
- 8.Cypres A, Landsberg G, Spellman M. The impact of managed care on community mental health outpatient services in New York State. Adm Policy Ment Health. 1997;24:509–521. [DOI] [PubMed] [Google Scholar]
- 9.Feldstein PJ. Health Policy Issues: An Economic Perspective on Health Reform. 2nd ed. Chicago, Ill: Health Administration Press; 1999.
- 10.Barnes PM, Adams PF, Schiller JS. Summary health statistics for the US population: National Health Interview Survey, 2001. Vital Health Stat 10. 2003;No. 217. [PubMed]
- 11.1997 National Health Interview Survey (NHIS) Public Use Data Release. NHIS Survey Description. Hyattsville, Md: National Center for Health Statistics; 2000. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/1997/srvydesc.pdf (PDF file). Accessed August 18, 2005.
- 12.2002 National Health Interview Survey (NHIS) Public Use Data Release. NHIS Survey Description. Hyattsville, Md: National Center for Health Statistics; 2003. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2002/srvydesc.pdf (PDF file). Accessed August 18, 2005.
- 13.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in nonspecific psychological distress. Psychol Med. 2002;32:959–976. [DOI] [PubMed] [Google Scholar]
- 15.First MB, Spitzer RL, Gibbon, M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Nonpatient Edition (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 1997.
- 16.Endicott J, Spitzer RL, Fleiss JL, et al. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disorders. Arch Gen Psychiatry. 1976;33:766–771. [DOI] [PubMed] [Google Scholar]
- 17.Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8:283–298. [DOI] [PubMed] [Google Scholar]
- 18.Hanley J, McNeil B. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. [DOI] [PubMed] [Google Scholar]
- 19.Stata, Version 8.0 [computer program]. College Station, Tex: Stata Corp; 2003.
- 20.Berk ML, Schur CL. Measuring access to care: improving information for policymakers. Health Aff. 1998; 17:180–186. [DOI] [PubMed] [Google Scholar]
- 21.Rogler LH. Methodological sources of cultural insensitivity in mental health research. Am Psychol. 1999; 54:424–433. [DOI] [PubMed] [Google Scholar]
- 22.Reasons for not receiving treatment among adults with serious mental illness. The NSDUH Report. October 3, 2003. Available at: http://www.drugabusestatistics.samhsa.gov/2k3/MHnoTX/MHno.TX.htm. Accessed August 18, 2005.
- 23.Alegría M, Canino G, Ríos R, et al. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psych Serv. 2002;53:1547–1555. [DOI] [PubMed] [Google Scholar]
- 24.Mental Health: Culture, Race, and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. [PubMed]
- 25.George LK, Blazer DG, Winfield-Laird I, et al. Psychiatric disorders and mental health service use in later life: evidence from the Epidemiologic Catchment Area Program. In: Brody JA, Maddox GL, eds. Epidemiology and Aging: An International Perspective. New York: Springer; 1988:189–219.
- 26.Levit K, Smith C, Cowan C, et al. Health spending rebound continues in 2002. Health Aff. 2004;23: 147–159. [DOI] [PubMed] [Google Scholar]
- 27.Greenberg D. Congress glumly moves towards Medicare drug benefit: but the cost is expected to be very high, and coverage limited. Lancet. 2003; 361:2216. [DOI] [PubMed] [Google Scholar]
- 28.Pauly MV. The new Medicare drug benefit: much ado about little? LDI Issue Brief. 2004;9:1–6. [PubMed] [Google Scholar]
- 29.Veroff J, Kulka RA, Douvan E. Mental Health in America: Patterns of Help-Seeking from 1957 to 1976. New York, NY: Basic Books; 1981.
- 30.Rabinowitz J, Gross R, Feldman D. Correlates of a perceived need for mental health assistance and differences between those who do and do not seek help. Soc Psychiatry Psychiatr Epidemiol. 1999;34:141–146. [DOI] [PubMed] [Google Scholar]
- 31.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety or substance disorders. Arch Gen Psychiatry. 2002;59:77–84. [DOI] [PubMed] [Google Scholar]
- 32.Strunk BC, Cunningham PJ. Treading Water: Americans’ Access to Needed Medical Care, 1997–2001. Washington, DC: Center for Studying Health System Change; March 2002. Tracking report no. 1. Available at: http://www.hschange.com/CONTENT/421/421.pdf (PDF file). Accessed August 18, 2005. [PubMed]