Abstract
Objectives. To investigate the effect of disability severity and the contribution of self-rated health and depressive symptoms to 10-year mortality.
Methods. Longitudinal data were collected from 1141 men aged 70 to 89 years from the Finland, Italy, and the Netherlands Elderly Study from 1990 to 2000. Disability severity was classified into 4 categories: no disability, instrumental activities, mobility, and basic activities of daily living. Self-rated health and depressive symptoms were classified into 2 and 3 categories, respectively. Multivariate Cox proportional hazard models were used to calculate mortality risks.
Results. Men with severe disability had a risk of mortality that was more than 2-fold higher (hazard ratio [HR]=2.41; 95% confidence interval [CI]=1.84, 3.16) than that of men without disability. Men who had severe disability and did not feel healthy had the highest mortality risk (HR = 3.30; 95% CI = 2.52, 4.33). This risk was lower at lower levels of disability and higher levels of self-rated health. The same trend was observed for depressive symptoms.
Conclusions. For adequate prognoses on mortality or for developing intervention strategies, not only physical aspects of health but also other health outcomes should be taken into account.
The prediction of mortality in elderly people is a subject with a huge body of knowledge. There is little debate about the importance of functional disability as a predictor of mortality. However, there are still unresolved questions in the pathway from disability to mortality that are important for enhancing insight into long-term prognosis, planning health care facilities, or for developing intervention strategies.
First, disabilities in different domains (i.e., in instrumental activities,1–4 in mobility,5 and in basic activities6–10) are known to be associated with mortality risk. These earlier studies are restricted to only one of the disability domains. These domains reflect differences in severity levels of disability, but the relative impact of these domains on mortality is unknown. An earlier study that incorporated disability in both mobility and basic activities reported that men with disability in basic activities and mobility had a higher risk of mortality than those with disability in mobility only.11 In another study about the association between disability and mortality, it was recommended to use different severity levels of disability (e.g., instrumental activities, mobility, and basic activities) as predictors of mortality.7 Although it seems plausible that mortality risk increases with the severity of the disability, no earlier study incorporated the three severity levels in one classification, and it is not known whether there is a gradual or exponential increase in risk. In earlier studies in which disability severity was classified in instrumental activities, mobility, and basic activities, disability severity was strongly associated with other health outcomes, such as performance-based functional limitations and chronic diseases.12,13
In addition to physical aspects of health, subjective aspects also may play a role in the association with mortality. It is known from earlier research that factors such as self-rated health and depressive symptoms are associated with disability14–17 as well as with mortality.1,18–21 However, it is unclear how the combination of disability and more subjective health aspects contributes to the mortality risk. A person’s actual health and mood probably contribute to the mortality risk besides disability.
The aim of the present study was to investigate severity levels of disability as predictor of mortality. Furthermore, we assessed how different combinations of levels of disability and self-rated health and levels of disability and depressive symptoms contributed to mortality during a 10-year follow-up period. We had the opportunity to investigate the different associations in three European countries (i.e., Finland, the Netherlands, and Italy).
METHODS
Study Population
The present study has a longitudinal design and used data of the Finland, Italy, and the Netherlands Elderly (FINE) Study, collected in 1989, 1991, and 1990, respectively, with a mortality follow-up to 2000. The FINE Study started in 1985 as a continuation of the Seven Countries Study,22 focusing on elderly men born between 1900 and 1920. In 1985, there were 716 participants from Finland, 887 from the Netherlands, and 682 from Italy.
Around 1990, 1416 men were examined (response rates: Finland, 90% of 523 survivors; the Netherlands, 78% of 718 survivors; Italy, 79% of 493 survivors). Six percent of the men were removed because of missing values on disability, 6% because of missing values on self-rated health, 6% because of missing values on depressive symptoms, and 2% because of missing values on both. In total, 1141 men were left for the analyses.
More information about the FINE Study and its populations has been reported elsewhere.23
Disability
Disability was measured by a standardized questionnaire about daily routine activities.24 Three domains were assessed: (1) instrumental activities of daily living (3 items): preparing meals, doing light housework, and doing heavy housework; (2) mobility (4 items): moving outdoors, using stairs, walking 400 meters, and carrying a heavy object 100 meters; (3) basic activities of daily living (6 items): walking indoors, getting in and out of bed, using toilet, washing and bathing, dressing and undressing, and feeding oneself.
The participants were classified as being disabled on a certain item if they reported a need for help or were not able to perform that activity. Disability in a domain was defined as disability in at least one item of the domain. The domains were found to be hierarchically ordered.24 Men who were disabled in basic activities were also disabled in mobility and instrumental activities of daily living. Men who were disabled in mobility were also disabled in instrumental activities of daily living. The following severity levels of disability status were distinguished: no disability (0); mild disability, disability in instrumental activities only (1); moderate disability, disability in instrumental activities and mobility (2); and severe disability, disability in instrumental activities, mobility, and basic activities of daily living (3). Almost 3% of the men did not fit the hierarchy. Fourteen men who reported disabilities in mobility, but not in instrumental activities of daily living, were classified in category 2. Nineteen men who reported to need help with instrumental and basic activities of daily living but not with mobility were classified in category 3.
Self-Rated Health
Global self-rated health was assessed with a single-item question: “We would like to know what you think about your health,” with 4 answer categories: healthy (1), rather healthy (2), moderately healthy (3), and not healthy (4). For the analyses, self-rated health was dichotomized as healthy and not healthy by combining category 1 with 2 and category 3 with 4.
Depressive Symptoms
Depressive symptoms were measured by the Self-Rating Depression Scale (SDS) developed by Zung.25 The questionnaire consisted of 20 items developed from clinical diagnostic criteria most commonly used to characterize depressive disorders in terms of mood and biological and psychological disturbances. The items were scored from 1 to 4 on frequency of occurrence of the symptoms. An index for the Self-Rating Depression Scale was derived by dividing the sum of the items score by 80 and multiplying it by 100, resulting in a range from 25 to 100.
Chronic Diseases
Information on prevalence of chronic diseases was collected for the following chronic conditions: myocardial infarction, stroke, angina pectoris, heart failure, intermittent claudication, cancer, diabetes mellitus, and asthma and chronic obstructive pulmonary disease. Diagnoses were obtained from a questionnaire and verified by written information from general practitioners or hospital registries. In the analyses, one variable was used for the absence or presence of chronic diseases.
Mortality (1990–2000)
In 2000, the vital status of the participants was checked through municipality registries. For Finland, the censor date was January 2000; for the Netherlands and the Italian cohort Montegiorgio, the censor date was June 2000; and, for the Italian cohort Crevalcore, the censor date was March 2000. Three men were lost to follow-up. These men were censored on the date of the last examination. For the 10-year follow-up, survival time was calculated according to the examination date, which was around 1990.
Causes of death were obtained from general practitioners or hospital registries and were checked for consistency by one clinical epidemiologist of our research group.
Statistical Analyses
SAS PROC PHREG was used to generate proportional hazards model estimates of mortality in relation to severity levels of disability, with survival time as a dependent variable. The severity levels of disability were entered into the model as dummy variables. The same analyses were performed with the two categories of self-rated health and tertiles of depressive symptoms as independent variables. The cutoff points for the tertiles of depressive symptoms were 40 and 50.
The independent associations between mortality and different health aspects (i.e., disability, self-rated health, and depressive symptoms) were studied by including these 3 variables in 1 model. We tested the interaction between disability and the more subjective health aspects by including interaction terms in the model.
In addition, we constructed 6 strata by cross-tabulating disability and self-rated health, and 9 strata for disability and depressive symptoms. For these analyses, the 2 most severe levels of disability were put together. A Cox proportional hazards model was used to determine the relationship between the strata and survival time. The combinations of no disability with good self-rated health and of no disability with the lowest tertile of depressive symptoms were defined as reference category in the analyses.
Although disability is assumed to reflect the impact of medical chronic conditions, these conditions might also act as a confounding factor in the association between disability and mortality. We therefore adjusted for the presence of chronic diseases in some analyses. Furthermore, all analyses were adjusted for age and country.
The analyses were performed using SAS, version 8.2 (SAS Inc., Cary, NC), the tests were two-tailed, and P≤ .05 was considered to be statistically significant.
RESULTS
The prevalence of severe disability was about 3 times higher in Finland and Italy (11–12%) than in the Netherlands (4%) (Table 1▶). In addition, a large variation was observed in self-rated health. In Finland, only 17% of the men felt healthy, and in the Netherlands and Italy, more than 80%. Men in Italy scored three to seven points higher on depressive symptoms compared with men in Finland and the Netherlands, respectively.
TABLE 1—
Characteristics of European Elderly Men at the Baseline Survey and 10-Year Mortality
| Finland (n = 324) | Netherlands (n = 469) | Italy (n = 348) | |
|---|---|---|---|
| Mean age, years (SD) | 76.4 (4.8) | 75.7 (4.5) | 77.8 (4.0) |
| Disability severity, % | |||
| No disability | 53 | 52 | 45 |
| Mild disability | 29 | 32 | 34 |
| Moderate disability | 7 | 12 | 9 |
| Severe disability | 11 | 4 | 12 |
| Self-rated health, % | |||
| Healthy | 17 | 89 | 82 |
| Not healthy | 83 | 11 | 18 |
| Depressive symptoms (range 25–100) | |||
| Mean score (SD) | 47.6 (10.5) | 43.7 (10.0) | 50.9 (11.9) |
| Prevalence of chronic diseases, % | 60 | 58 | 87 |
| Deceased between 1990 and 2000, % | 60 | 59 | 49 |
In 2000, among the Italian men, there were 10% less deceased men than in Finland and the Netherlands. After adjustment for the shorter follow-up time in this country, this difference became even larger. The leading cause of death was cardiovascular disease (51%), followed by cancer (26%) and stroke (14%). In Italy, the prevalence of chronic diseases was almost 30% higher than in the other countries, caused primarily by a higher prevalence of asthma and chronic obstructive pulmonary disease.
Although health outcomes differed largely between the three countries, the associations with mortality did not differ statistically significantly and are therefore presented for the three countries together.
Disability Severity, Self-Rated Health, and Depressive Symptoms As Predictors of Mortality
Disability, self-rated health and depressive symptoms were associated with each other. The prevalence of men who felt not healthy increased significantly from 27% among men without disability to 62% among men with severe disability. The mean score of depressive symptoms increased from 43.2 to 60.2 between these disability levels. The mean score of depressive symptoms was 44.7 for those who felt healthy and 51.7 for those who felt unhealthy.
Severity level of disability seemed to be a strong predictor of mortality (Table 2▶). The basic model showed that although mild disability was already associated with a 34% increased risk of mortality, disability at a moderate or severe level was associated with a 2.5- and a 3-fold higher risk, respectively (Table 2▶). Addition of self-rated health and depressive symptoms to the model resulted in lower risk ratios of disability severity, but the associations were still statistically significant. Addition of the prevalence of chronic diseases into the model also slightly decreased the hazard ratios. The independent contribution of the prevalence of chronic diseases to mortality was statistically significant (hazard ratio [HR] = 1.59; 95% confidence interval [CI] = 1.32, 1.92).
TABLE 2—
Disability Severity, Self-Rated Health, and Depressive Symptoms as Predictors of 10-Year Mortality, Adjusted for Age and Country
| HR (95% CI) |
|||
|---|---|---|---|
| Unadjusted for the Other Health Outcomesa | Adjusted for the Other Health Outcomesb | Adjusted for Other Health Outcomes and Chronic Diseasesc | |
| Disability severity | |||
| No disability | 1.00 | 1.00 | 1.00 |
| Mild disability | 1.34 (1.11, 1.61) | 1.24 (1.03, 1.50) | 1.18 (0.98, 1.43) |
| Moderate disability | 2.45 (1.90, 3.15) | 2.22 (1.72, 2.87) | 2.06 (1.59, 2.67) |
| Severe disability | 3.02 (2.34, 3.89) | 2.41 (1.84, 3.16) | 2.28 (1.74, 3.00) |
| Self-rated health | |||
| Healthy | 1.00 | 1.00 | 1.00 |
| Not healthy | 1.63 (1.35, 1.98) | 1.23 (1.01, 1.51) | 1.19 (0.97, 1.46) |
| Depressive symptoms | |||
| Lowest tertile | 1.00 | 1.00 | 1.00 |
| Middle tertile | 1.29 (1.05, 1.59) | 1.19 (0.97, 1.46) | 1.17 (0.95, 1.44) |
| Highest tertile | 1.90 (1.56, 2.32) | 1.44 (1.15, 1.79) | 1.42 (1.14, 1.77) |
Note. HR = hazard ratio; CI = confidence interval.
aDisability severity, self-rated health and depressive symptoms in 3 different models.
bIndependent association: disability severity, self-rated health, and depressive symptoms together in 1 model.
c Independent association: disability severity, self-rated health, and depressive symptoms together in 1 model, adjusted for chronic diseases.
In addition, self-rated health was predictive of mortality (Table 2▶). After addition of disability severity and depressive symptoms to the model, the mortality risk in the not healthy category was 23% higher than in the healthy category. Addition of the prevalence of chronic diseases into the model slightly decreased the risk of self-rated health on mortality to 19%.
For depressive symptoms, a similar trend was observed (Table 2▶). Men in the highest tertile of depressive symptoms had a 42% higher mortality risk than men in the lowest tertile, after adjustment for disability, self-rated health, and prevalence of chronic diseases.
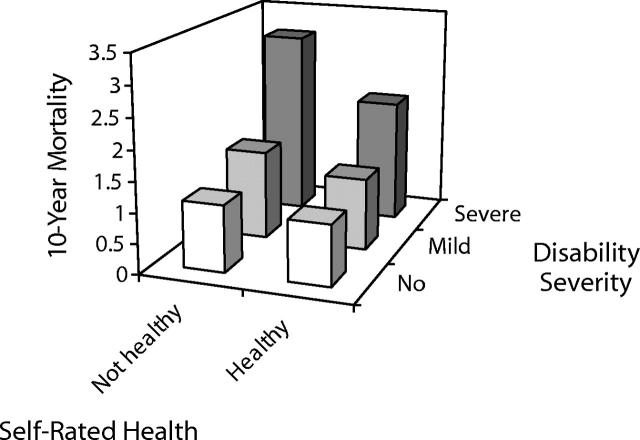
Combination of Disability and Self-Rated Health
When participants were classified into 6 groups according to categories of disability severity and self-rated health, mortality risks varied markedly (Figure 1▶). The highest risk was observed among those who had severe disability and did not feel healthy (HR = 3.30; 95% CI = 2.52, 4.33). This risk decreased with lower disability levels and with higher levels of self-rated health.
FIGURE 1—
Mortality risk for six different combinations of disability severity and self-rated healtha
Note. a Hazard ratio on z-axis, with men with no disability who felt healthy as reference group, adjusted for age, country, and chronic diseases
Among those with mild or severe disability, significant associations between self-rated health and mortality were observed (Figure 1▶). Men with mild disability who did not feel healthy had a hazard ratio of 1.36 (95% CI = 0.95, 1.93) compared with those who felt healthy. Among men with severe disability, those who did not feel healthy had a 45% higher risk (95% CI = 1.02, 2.04) than those who felt healthy.
The P value for interaction between disability and self-rated health was 0.11.
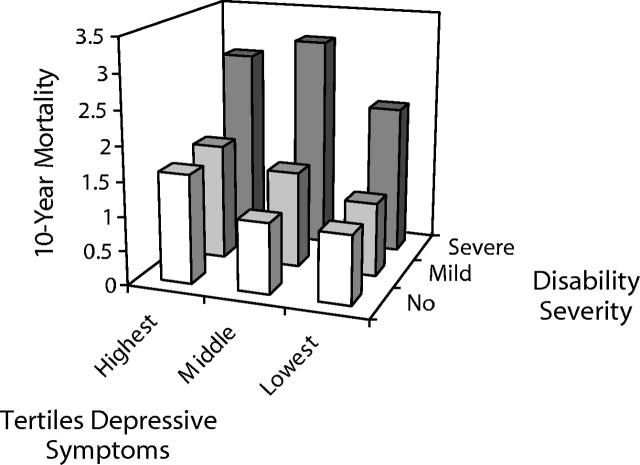
Combination of Disability and Depressive Symptoms
Men with severe disability in the two highest tertiles of depressive symptoms had a 3-fold higher risk of mortality compared with men without disability in the lowest tertile of depressive symptoms (Figure 2▶). This risk decreased with lower levels of disability severity and was also lower among men with severe disability in the lowest tertile of depressive symptoms (HR = 2.16; 95% CI = 1.33, 3.51).
FIGURE 2—
Mortality risk for nine different combinations of disability severity and depressive symptomsa
Note. aHazard ratio on z-axis, with men with no disability who were in the lowest tertile of depressive symptoms as reference group, adjusted for age, country, and chronic diseases
In the lowest levels of disability severity, dose-response relationships between depressive symptoms and mortality were found. Among men with no disability, those in the highest tertile of depressive symptoms had a hazard ratio of 1.62 (95% CI = 1.19, 2.20), with the lowest tertile as reference group. Men with mild disability in the highest tertile of depressive symptoms had a 59% higher mortality risk (95% CI = 1.11, 2.30) than those in the lowest tertile.
The P value for interaction between disability and depressive symptoms was 0.34.
DISCUSSION
The present study was designed to investigate disability severity and its combination with self-rated health and depressive symptoms as risk factors for mortality among men aged 70 to 89 years at baseline, from Finland, the Netherlands, and Italy. The results showed that severity levels of disability, self-rated health, and depressive symptoms were independent predictors of 10-year mortality. The combinations of disability with self-rated health or with depressive symptoms were strongly associated with mortality. For several levels of disability, dose-response relationships between self-rated health or depressive symptoms and mortality were observed.
Selection for better health was caused by nonresponse and by removing men with missing values. Men removed because of missing values on self-rated health or depressive symptoms had more disabilities than men included in the study. Furthermore, men removed because of missing values for disability, self-rated health, and depressive symptoms, or who were nonrespondent, had a higher mortality rate than men who were included. The exclusions might have led to underestimation of the strength of the associations.
As far as we know, there are few investigations of the association between different disability domains and mortality. Bernard et al.26 investigated the three domains separate from each other and found an association between disability and mortality only for the instrumental and basic activities. Khokhar et al.11 showed that men with disabilities in basic activities and mobility (severe disability) had a higher risk of mortality than men with disabilities in mobility only (moderate disability). These results were in accordance with our findings. Our study, using one additional disability domain (instrumental activities), showed that the classification of disability severity based on three domains (i.e., instrumental activities, mobility, and basic activities of daily living) was strongly associated with mortality. According to an earlier study concerning mobility disability, self-reported disability predicted mortality as well as more objective measurements of disability, such as gait speed.27
After adjustment for self-rated health and depressive symptoms, disability was still a significant predictor of mortality. In accordance with earlier studies, self-rated health21,26,28,29 and depressive symptoms,1 independent of disability, also were associated with mortality. Disability, however, had a stronger association with mortality than self-rated health and depressive symptoms in the present study. In contrast, earlier studies showed the strongest association for self-rated health and mortality.26,28 These divergent findings might have been caused by differences in the measurement or distribution of self-rated health. Furthermore, these studies had a shorter follow-up period (3–5 years), and self-rated health30 and depressive symptoms1 are known to be better predictors of mortality in short-term studies (3–5 years). However, it is also possible that our classification of disability, encompassing several domains, was a better predictor of mortality than that in the other studies, in which the disability domains were investigated separately. In addition, the present study was restricted to male subjects from three European countries, whereas the other studies included both genders and other countries.
Although there were differences in disability, self-rated health, and depressive symptoms among the three countries, the associations between these health aspects and mortality were not different and can therefore be generalized to European men. Women have a higher risk of disability than men7 and a lower risk of mortality.1 Furthermore, depression seemed to be associated with a higher mortality risk in men than in women.31 Some studies found that self-rated health is a better predictor of mortality in men,28,32,33 and other studies have found the reverse.9 Considering these results, it is not justified to generalize our results to women.
We assumed that disability reflects the consequences of several underlying diseases and might therefore be associated with mortality. The prevalence of chronic diseases was associated with both disability and mortality and may therefore confound the association between disability and mortality. It is also possible that adjustment for these diseases removes the association between disability and mortality. We therefore reported the associations of disability, self-rated health, and depressive symptoms with mortality, both adjusted and unadjusted for the prevalence of chronic diseases. The strength of the association between disability and mortality only slightly decreased after adjustment, which shows that disability is associated with mortality also independent of these chronic diseases. Disability seems to reflect more aspects of overall health and functioning than the disability impact of chronic diseases alone.
The interaction terms between disability and self-rated health or depressive symptoms were not statistically significant, which means that the association of self-rated health and depressive symptoms with mortality did not differ among the levels of disability severity. At the lower levels of disability, however, clear dose-response relationships were observed between depressive symptoms and mortality that were not present at the most severe disability level. Nevertheless, men with severe disability had a high mortality risk, and the small numbers of men in these different categories made it difficult to interpret the findings. In contrast, self-rated health was associated with mortality only in the higher levels of disability. These results suggest that positive health perceptions (self-rated health) and less depressive symptoms may postpone mortality.
Knowledge about risk factors for mortality in old age is important for enhancing insight into prognosis, planning long-term facilities, and developing intervention strategies. First, disability is an important risk factor. Men with only mild disability have an increased mortality risk, and further deterioration of disability should be countered effectively to prevent a much higher risk. Second, although depressive symptoms are often unrecognized,34 depression as well as self-rated health are both important. Intervention strategies should therefore focus not only on prevention of deterioration of physical disability but also on reinforcing mental functioning. Interventions on disability, self-rated health, and depressive symptoms will not only postpone mortality but also improve quality of life.
From the results of the present study, we conclude that, in elderly men, the risk of mortality increases with severity level of disability. Furthermore, self-rated health and depressive symptoms increase the mortality risk at different levels of disability. This knowledge may be helpful for enhancing insight into long-term prognosis, planning health care facilities, and developing intervention strategies.
Peer Reviewed
Contributors C.L. van den Brink designed the study, performed the analyses, interpreted the results, and wrote the article. M.A.R. Tijhuis, G.A.M. van den Bos, and D. Kromhout supervised all aspects of the study; they were involved with conception and design of the study, interpretation of the data, and reviewing drafts of the article. D. Kromhout was also involved with acquisition of the data. S. Giampaoli and A. Nissinen were involved with acquisition of the data and reviewed drafts of the article.
Human Participant Protection In 1985 in Finland, the research was approved by the Ethics Committee of the Kuopio University Hospital and in the Netherlands by the Medical Ethics Committee of the University of Leiden. In Italy, the research was approved by an Ethical Committee at the local level. More information about the FINE Study and its populations has been reported elsewhere.
References
- 1.Ganguli M, Dodge HH, Mulsant BH. Rates and predictors of mortality in an aging, rural, community-based cohort: the role of depression. Arch Gen Psychiatry.2002;59:1046–1052. [DOI] [PubMed] [Google Scholar]
- 2.Ginsberg GM, Hammerman-Rozenberg R, Cohen A, Stessman J. Independence in instrumental activities of daily living and its effect on mortality. Aging (Milano). 1999;11:161–168. [PubMed] [Google Scholar]
- 3.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults. JAMA.1998;279:585–592. [DOI] [PubMed] [Google Scholar]
- 4.Reuben DB, Rubenstein LV, Hirsch SH, Hays RD. Value of functional status as a predictor of mortality: results of a prospective study. Am J Med.1992;93: 663–669. [DOI] [PubMed] [Google Scholar]
- 5.Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc.2000;48: 493–498. [DOI] [PubMed] [Google Scholar]
- 6.Nybo H, Petersen HC, Gaist D, et al. Predictors of mortality in 2,249 nonagenarians—the Danish 1905-cohort survey. J Am Geriatr Soc.2003;51:1365–1373. [DOI] [PubMed] [Google Scholar]
- 7.Von Strauss E, Aguero-Torres H, Kareholt I, Winblad B, Fratiglioni L. Women are more disabled in basic activities of daily living than men only in very advanced ages: A study on disability, morbidity, and mortality from the Kungsholmen Project. J Clin Epidemiol.2003;56:669–677. [DOI] [PubMed] [Google Scholar]
- 8.De Andino RM, Conde-Santiago G, Mendoza MM. Functional disability and mental impairment as predictors of mortality in community-dwelling elderly Puerto Ricans. P R Health Sci J.1995;14:285–287. [PubMed] [Google Scholar]
- 9.Grant MD, Piotrowski ZH, Chappell R. Self-reported health and survival in the longitudinal study of aging, 1984–1986. J Clin Epidemiol.1995;48: 375–387. [DOI] [PubMed] [Google Scholar]
- 10.Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. Changes in functional status and the risks of subsequent nursing home placement and death. J Gerontol.1993;48:S94–S101. [PubMed] [Google Scholar]
- 11.Khokhar S, Stern Y, Bell K, et al. Persistent mobility deficit in the absence of deficits in activities of daily living: a risk factor for mortality. J Am Geriatr Soc.2001;49:1539–1543. [DOI] [PubMed] [Google Scholar]
- 12.van den Brink CL, Tijhuis M, Kalmijn S, et al. Self-reported disability and its association with performance-based limitation in elderly men: a comparison of three European countries. J Am Geriatr Soc.2003;51: 782–788. [DOI] [PubMed] [Google Scholar]
- 13.Hoeymans N, Feskens EJ, Kromhout D, van den Bos GA. The contribution of chronic conditions and disabilities to poor self-rated health in elderly men. J Gerontol A Biol Sci Med Sci.1999;54:M501–M506. [DOI] [PubMed] [Google Scholar]
- 14.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry.2003;160: 1147–1156. [DOI] [PubMed] [Google Scholar]
- 15.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry.2001;9:102–112. [PubMed] [Google Scholar]
- 16.Gama EV, Damian JE, Perez de Molino, J et al. Association of individual activities of daily living with self-rated health in older people. Age Ageing.2000;29: 267–270. [DOI] [PubMed] [Google Scholar]
- 17.Hoeymans N, Feskens EJM, Kromhout D, van den Bos GAM. Ageing and the relationship between functional status and self-rated health in elderly men. Soc Sci Med.1997;45:1527–1536. [DOI] [PubMed] [Google Scholar]
- 18.Kushiro W, Yokoyama T, Date C, et al. Association of activities of daily living and indices of mental status with subsequent 20-year all-cause mortality in an elderly Japanese population. Nurs Health Sci.2002; 4(3 Suppl):A5.12153423 [Google Scholar]
- 19.Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol.2000;152:874–883. [DOI] [PubMed] [Google Scholar]
- 20.Schoevers RA, Geerlings MI, Beekman AT, et al. Association of depression and gender with mortality in old age. Results from the Amsterdam Study of the Elderly (AMSTEL). Br J Psychiatry.2000;177:336–342. [DOI] [PubMed] [Google Scholar]
- 21.Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality—Additional studies, 1995–1998. Res Aging.1999;21: 392–401. [Google Scholar]
- 22.Keys A, Aravanis C, Blackburn H, et al. Epidemiological studies related to coronary heart disease: characteristics of men aged 40–59 in seven countries. Acta Med Scand Suppl.1966;460:1–392. [PubMed] [Google Scholar]
- 23.Bijnen FC, Feskens EJM, Caspersen CJ, et al. Physical activity and cardiovascular risk factors among elderly men in Finland, Italy, and the Netherlands. Am J Epidemiol.1996;143:553–561. [DOI] [PubMed] [Google Scholar]
- 24.Hoeymans N, Feskens EJ, van den Bos GAM, Kromhout D. Measuring functional status: cross-sectional and longitudinal associations between performance and self-report (Zutphen Elderly Study 1990–1993). J Clin Epidemiol.1996;49:1103–1110. [DOI] [PubMed] [Google Scholar]
- 25.Zung WWK. A self-rating depression scale. Arch Gen Psychiatry.1965;12:63–70. [DOI] [PubMed] [Google Scholar]
- 26.Bernard SL, Kincade JE, Konrad TR, et al. Predicting mortality from community surveys of older adults: the importance of self-rated functional ability. J Gerontol B Psychol Sci Soc Sci.1997;52:S155–S163. [DOI] [PubMed] [Google Scholar]
- 27.Melzer D, Lan TY, Guralnik JM. The predictive validity for mortality of the index of mobility-related limitation—results from the EPESE study. Age Ageing.2003;32:619–625. [DOI] [PubMed] [Google Scholar]
- 28.Helmer C, Barberger-Gateau P, Letenneur L, Dartigues J. Subjective health and mortality in French elderly women and men. J Gerontol B Psychol Sci Soc Sci.1999;54:S84–S92. [DOI] [PubMed] [Google Scholar]
- 29.Scott WK, Macera CA, Cornman CB, Sharpe PA. Functional health status as a predictor of mortality in men and women over 65. J Clin Epidemio.1997;50: 291–296. [DOI] [PubMed] [Google Scholar]
- 30.Benyamini Y, Blumstein T, Lusky A, Modan B. Gender differences in the self-rated health-mortality association: is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologis.2003;43:396–405. [DOI] [PubMed] [Google Scholar]
- 31.Anstey K, Luszcz M. Mortality risk varies according to gender and change in depressive status in very old adults. Psychosom Me.2002;64:880–888. [DOI] [PubMed] [Google Scholar]
- 32.Deeg DJ, Kriegsman DM. Concepts of self-rated health: specifying the gender difference in mortality risk. Gerontologist. 2003;43:376–386; discussion 372–5. [DOI] [PubMed] [Google Scholar]
- 33.Kivinen P, Sulkava R, Halonen P, Nissinen A. Self-reported and performance-based functional status and associated factors among elderly men: the Finnish cohorts of the Seven Countries Study. J Clin Epidemio.1998;51:1243–1252. [DOI] [PubMed] [Google Scholar]
- 34.Tylee A. Depression in the community: physician and patient perspective. J Clin Psychiatr. 1999;60 Suppl 7:12–16; discussion 17–8. [PubMed] [Google Scholar]