Abstract
Objectives. We investigated the effectiveness of a group-based exercise intervention to improve balancing ability among older adults delivered in natural settings by staff in local community organizations.
Methods. The main component of the intervention consisted of biweekly group-based exercise sessions conducted over 12 weeks by a professional, coupled with home-based exercises. In a quasiexperimental design, 10 community organizations working with older adults offered the intervention to groups of 5 to 15 persons concerned about falls, while 7 organizations recruited similar groups to participate in the control arm of the study. Participants (98 experimental and 102 control) underwent balance assessments by a physiotherapist at registration and 3 months later.
Results. Eighty-nine percent of participants attended the 3-month measurement session (n=177). A linear regression analysis showed that after adjusting for baseline levels of balance and demographic and health characteristics, the intervention significantly improved static balance and mobility.
Conclusion. Structured, group-based exercise programs offered by community organizations in natural settings can successfully increase balancing ability among community-dwelling older adults concerned about falls.
Falls contribute significantly to morbidity among older adults (aged 65 years and older),1,2 and balance problems are an important risk factor for falls.3 Despite evidence showing that specific exercise programs can improve balancing ablility, little is known about the success of these programs when broadly delivered in a community context.
Since the mid-1990s, randomized controlled trials have demonstrated that it is possible to reduce the incidence of falls among older adults with physical exercise interventions to improve balance.4–6 Although initial studies focused mainly on intensive individual programs, more recent studies have examined group programs.7,8 These studies were conducted in contexts where research method constraints prevailed over those related to result implementation (generalization). Unfortunately, interventions shown to be effective in tightly controlled efficacy studies do not necessarily yield similar effects when delivered on a large scale in clinical or community settings.9 The pivotal issue is how to disseminate interventions, found to be effective, in real-life contexts without jeopardizing components essential to their efficacy.
Given the demonstrated efficacy of exercise interventions in improving balance and reducing falls and the dearth of information on their effectiveness in real-life settings, the purpose of this study was to determine the effectiveness of a group-based exercise intervention designed to improve balance among older adults. Our hypothesis was that even when delivered in a natural setting by personnel and staff in local older-adult centers and community health organizations, a group-based exercise intervention may improve balance among older adults concerned about falls.
The Intervention
Stand Up! is a multifaceted fall-prevention program developed for older independent adults who have a history of falls or are worried about their balance, but who can safely exercise in a group. Intervention objectives are to improve balance and leg strength, to initiate adoption and maintenance of regular physical activity, and to promote home safety and safe behaviors. The main component of this intervention consists of biweekly group-based exercise sessions spanning a 12-week period coupled with home-based exercises. The exercise program is designed to enhance various systems involved in balance, such as proprioception, leg strength, and ankle mobility.10 The program includes movements derived from tai chi and leg-strengthening exercises with elastic bands of varying thickness. Participants are also invited to exercise on their own at home, at least once a week, with the help of a poster depicting 12 exercises. Another component of the program not analyzed by our study consists of weekly 30-minute group discussions on safe behaviors and home modifications. Intervention activities were conducted by a fitness or rehabilitation professional who had access to a detailed intervention guide11 and had followed a 1-day training session.
The 12-week session costs about Can $1900 (US $1400). This amount averages out to Can $125 (US $95) per participant, if a group is composed of 15 older adults. In several regions of the province of Quebec, health authorities provide some financial support.
An earlier version of Stand Up! included an extra weekly tai chi group session, which meant the group met 3 times a week, but did not include home exercises. In a small quasi-experimental study, this earlier version of the program was found to be effective in increasing balance.12 However, a survey of community organizations revealed that the tai chi component was often omitted from program implementation because it required the involvement of a tai chi expert. Therefore, the program was redesigned in 2002 to take into consideration constraints of community organizations while maintaining elements essential to the efficacy of the program. We assessed the revised version of this program.
METHODS
To minimize interference with regular activities of the community organizations, a quasiexperimental design was used, thus providing an appropriate test of the effectiveness of the intervention when delivered in a real-world setting.
Participants and Recruitment
In winter 2002, 10 community organizations that provided services to older adults in the Montreal area (Quebec, Canada) were invited to offer the program (hereafter termed “experimental organizations”), and 7 similar organizations were asked to recruit participants for the control arm of the study (hereafter “control organizations”). The latter agreed to wait until the study was completed before offering the program in their localities. A total of 200 participants were recruited by all 17 organizations, in clusters of 5 to 17 people. Recruitment of experimental and control group participants was matched for seasonality. Older adults recruited by experimental organizations received the Stand Up! Program, whereas those recruited in control organizations did not.
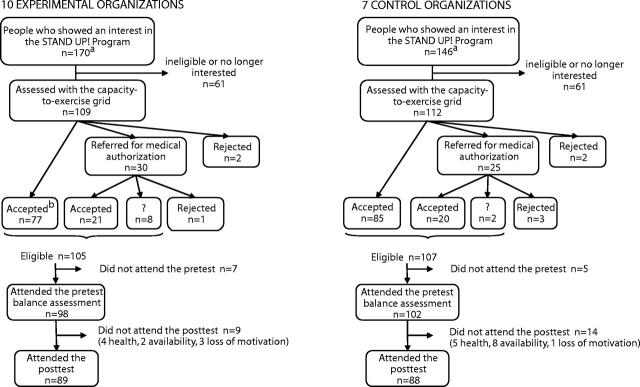
Experimental and control organizations were invited to target the population for which Stand Up! was developed, namely older adults who had already had a fall or were worried about their balance or about falling. A capacity-to-exercise grid included in the Stand Up! Program Guide11 provides a series of questions that determine whether the potential participant can perform relatively demanding exercises within a group, should have prior medical authorization, or should be referred to a program involving lower doses of exercise. A minimum age of 60 years was required to participate in this study. Figure 1 ▶ illustrates the study design, as well as participant flow through the study. The unit of intervention assignment was the group. The sample was representative of organizations interested in offering the program and of individuals who would register for it. The number of groups included was determined by the budget available for the study. We believe that the sample is adequate to test whether or not an intervention is effective in a real-world setting. With a sample size of 200 subjects, the study has an 80% power to detect a 15% difference in balance improvement.
FIGURE 1—
Study design and flow of participants through the study.
Physical Performance Measures
The main outcome of this evaluation was balance. We measured the following 3 dimensions of balance: (1) static balance (one-legged stance test with eyes open and closed,13,14 and tandem stance test);14,15 (2) stability limits (functional reach13,16 and lateral reach tests);17,18 and (3) mobility (tandem walk test).19 Another motor function tested was the strength of lower extremity muscles (sit-to-stand).20,21 Furthermore, we used 2 measurements of vitality to describe the targeted population: 4-meter maximal walking speed14,22 and grip strength with the Jamar dynamometer (Sammons Preston, Bolingbrook, Ill).23,24 These tests were chosen because they have been shown to be valid and reliable, sensitive to change, and easy and safe to administer in a community setting. Test-retest reliability for all of these physical performance measures was established in previous studies with similar groups.13,14,17,25
Each participant was assessed by the same trained physiotherapist who was blinded to group membership. Time trials were limited to a maximum of 60 seconds. Two trials were carried out for each test, and the better score was used in analyses. Participant assessments were conducted at a location in the neighborhood of each group to maintain a high study participation rate.
Demographic, Health, and Other Data
Participants’ demographic and health data were collected in face-to-face interviews with a questionnaire covering such factors as physical health, including self-perceived health status,26 medical consultations,27 health problems, and medications; mental health and vitality28; number of falls in the year preceding baseline assessment27; balance self-confidence29; and frequency and variety of physical activities in the previous month.30
A representative from each organization was asked how participants were recruited and assessed so that the research team could describe the recruitment process. In addition, experimental organizations provided data about the program set-up (e.g., training of the session leader, cost for participation in the program, and number of sessions offered). The session leader monitored and recorded the participants’ attendance at each exercise session.
Statistical Analysis
To assess the effectiveness of the intervention, data were analyzed on an intention-to-treat basis. At the beginning of the study, we compared the demographics, health, balance, and strength of the 2 groups. We then calculated raw changes in levels of balance by subtracting measurements taken at baseline from those taken at the end of the program 3 months later.
We performed linear regression analyses for each outcome variable using forward inclusion according to the following steps: (1) assessment of the effect of group membership with control for baseline scores; (2) control for a series of covariates chosen from the literature, including demographic variables (age, gender, and level of education), physical health (perceived health status, number of medical consultations during the previous 3 months, number of health problems, and classes of medications with side effects known to impede balance), mental health, history of falls and balance self-confidence, and frequency and diversity of physical activity; and (3) test of modifier effects of covariates on intervention effects by adding interaction terms. Statistical assumptions underlying linear regression were not violated except for 1 outcome variable, namely, the one-legged stance with eyes open variable, which showed a ceiling effect. Alternative analyses (nonparametric regression and time-to-event analysis) produced similar results. For the sake of brevity, only the results of the linear regression are presented here. Similarly, given that the unit of assignment was the group, and the final data set had a nested structure (repeated measures nested within persons nested within groups that were designated either experimental or control), we also replicated the linear regression analyses with multilevel modeling techniques. Results were identical to those found with linear regression analyses. Because the focus of our study was on whether people can improve their balance rather than on differential effects across groups, we elected to present results of linear regression analyses. Data were analyzed with SPSS (Chicago, Ill) software, version 11.0.31
RESULTS
Recruitment
As shown in Figure 1 ▶, most interested individuals (73.3%) were immediately accepted as participants in the study, once the capacity-to-exercise questionnaire had been administered. However, medical authorization was requested in nearly one fourth of the candidates. In 7% of cases, a physician determined that the person should not participate in the intervention.
A total of 212 older adults were eligible for the study, but 12 did not attend the baseline evaluation. Of the 200 registrants at baseline (98 at intervention sites and 102 at control sites), 88.5% attended the 3-month measurement session (n = 177). The 23 subjects lost to follow-up did not differ statistically from maintainers with respect to demographics and health data at baseline, except that a larger proportion of the former lived alone and had poorer balance than did of subjects who attended the posttest session (one-legged stance [right leg]—eyes open and closed, Wilcoxon test, P < .05).
Characteristics at Baseline
At baseline, the mean age of participants was 73.9 years, and 84% were women. More than half of study participants lived alone, and almost 40% reported having fallen in the year before baseline assessment. Comparison of intervention and control participants at baseline did not reveal statistically significant differences in demographics, health, physical activity, or vitality indicators. Intervention and control participants also had similar balance levels at baseline, except for their scores on lateral reach (both sides). Table 1 ▶ shows that the subjects varied widely in age, education, and health status. The individuals who signed up for the intervention were proportionately older than the elderly population living in the region of Montreal. Only 12.5% of subjects were aged 60 to 64 years, whereas this age group represented 23% of people aged 60 years and over in Montreal. However, the proportion of participants aged 65 years and over corresponded with their proportion among the elders in Montreal. The intervention also drew proportionately more women (84%), representing a higher share than in the elderly population (60%).
TABLE 1—
Baseline Demographic, Health, and Physical Performance Characteristics of Intervention and Control Groups
| Experimental (n = 98) | Control (n = 102) | All (n = 200) | |
| Demographics | |||
| Age, y | |||
| Mean (SD) | 73.6 (7.4) | 74.2 (7.4) | 73.9 (7.4) |
| Range | 60–91 | 61–90 | |
| Female, % | 83.7 | 84.3 | 84.0 |
| Live alone, % | 55.1 | 59.8 | 57.5 |
| Education, % | |||
| Primary level | 28.9 | 20.6 | 24.6 |
| High school level | 42.3 | 44.1 | 43.2 |
| College/university level | 28.9 | 35.3 | 32.2 |
| Health | |||
| Self-perceived, % | |||
| Poor/medium | 25.8 | 13.8 | 19.6 |
| Good/very good | 56.7 | 73.5 | 65.3 |
| Excellent | 17.5 | 12.7 | 15.1 |
| Mental health, mean score (SD) | 77.7 (16.2) | 76.7 (16.3) | 77.2 (16.2) |
| Medical consultations, last 3 months, mean (SD) | 1.3 (1.3) | 1.5 (1.5) | 1.4 (1.4) |
| Number of health problems. mean (SD) | 2.0 (1.4) | 2.0 (1.3) | 2.0 (1.3) |
| Number of medication classes, mean (SD) | 3.4 (1.9) | 3.4 (1.8) | 3.4 (1.9) |
| Falls in last year, % | |||
| 0 falls | 61.2 | 61.8 | 61.5 |
| 1 fall | 22.4 | 24.5 | 23.5 |
| 2 falls or more | 16.3 | 13.7 | 15.8 |
| Balance-related self confidence,a mean (SD) (score range: 12.5–100) | 81.8 (15.1) | 79.4 (17.1) | 80.6 (16.2) |
| Physical activity, mean (SD) | |||
| Diversity score | 4.16 (1.9) | 4.15 (2.1) | 4.15 (2.0) |
| Frequency score | 16.4 (8.8) | 15.5 (7.5) | 16.0 (8.2) |
| Vitality indicators, mean (SD) | |||
| Walking speed, s | 2.85 (1.4) | 2.85 (1.0) | 2.85 (1.2) |
| Grip strength, kg, R | 24.6 (8.4) | 22.7 (7.0) | 23.6 (7.8) |
| Outcomes (physical performance), mean (SD) | |||
| Static balance, s | |||
| One-legged stance—eyes open, L | 11.2 (15.8) | 12.2 (15.9) | 11.7 (15.8) |
| One-legged stance—eyes open, R | 14.3 (18.7) | 11.9 (14.7) | 13.0 (16.8) |
| One legged stance—eyes closed, L | 2.8 (3.3) | 2.5 (2.2) | 2.6 (2.8) |
| One-legged stance—eyes closed, R | 2.7 (1.9) | 2.5 (2.2) | 2.6 (2.1) |
| Tandem stance | 28.1 (24.2) | 27.9 (24.2) | 28.0 (24.1) |
| Limits of stability, cm | |||
| Functional reach | 24.3 (6.8) | 24.7 (6.7) | 24.5 (6.7) |
| Lateral reach, L* | 14.2 (5.0) | 12.8 (4.1) | 13.5 (4.6) |
| Lateral reach, R* | 14.9 (5.3) | 13.5 (4.0) | 14.2 (4.7) |
| Mobility, s | |||
| Tandem walk | 16.8 (10.8) | 18.0 (9.6) | 17.4 (10.2) |
| Strength, s | |||
| Sit-to-stand | 12.8 (6.3) | 12.7 (4.3) | 12.7 (5.4) |
Notes: L = left; R = right.
aIn a separate paper, we will report the results of a current study on the psychometric properties of a modified version of the Activities-Specific Balance Confidence (ABC) Scale.
*Means of experimental and control groups statistically different (t test, P < .05).
Outcome Measurement
Intervention participants improved more than control participants on all static balance indicators except one (lateral reach both sides; Table 2 ▶). For example, intervention participants improved their balance by 5.3 seconds from baseline in the one-legged stance with eyes open (left; from 12.1 to 17.4), whereas the performance of control participants declined by 2.4 seconds (from 13.1 to 10.7). Intervention participants also showed greater improvement in mobility and strength indicators. Taking into account intragroup variability at baseline, effect sizes were small to medium in magnitude in favor of intervention participants except on the limits of stability indicators where mixed results were observed.
TABLE 2—
Balance and Strength Evolution 3 Months After Baseline
| Experimental (n = 89) | Control (n = 88) | Experimental | Control | |||
| Baseline T1 Mean (SD) | 3 months T2 Mean (SD) | Baseline T1 Mean (SD) | 3 months T2 Mean (SD) | Effect Size (3 Months-Baseline)/SDb | Effect Size (3 Months-Baseline)/SDb | |
| Static balance, s | ||||||
| One-legged stance—eyes open, L | 12.1 (16.3) | 17.4 (19.7) | 13.1 (16.8) | 10.7 (14.7) | 0.33 | −0.14 |
| One-legged stance—eyes open, R | 15.3 (19.2) | 20.0 (21.0) | 12.8 (15.5) | 13.4 (16.3) | 0.24 | 0.04 |
| One-legged stance—eyes closed, L | 2.8 (3.5) | 3.5 (3.9) | 2.6 (2.3) | 2.4 (1.8) | 0.20 | −0.09 |
| One-legged stance—eyes closed, R | 2.8 (1.9) | 3.6 (3.9) | 2.6 (2.3) | 2.6 (2.8) | 0.42 | 0.00 |
| Tandem stance | 28.0 (23.8) | 33.8 (24.8) | 28.5 (24.7) | 31.2 (24.3) | 0.24 | 0.11 |
| Limits of stability, cm | ||||||
| Functional reach | 24.9 (6.7) | 25.5 (6.6) | 24.8 (6.5) | 24.7 (6.4) | 0.09 | −0.02 |
| Lateral reach, L | 14.5 (4.9) | 15.3 (5.0) | 12.7 (4.2) | 14.0 (4.5) | 0.16 | 0.31 |
| Lateral reach, R | 15.3 (5.3) | 15.8 (5.0) | 13.4 (4.0) | 14.3 (4.6) | 0.09 | 0.23 |
| Mobility, s | ||||||
| Tandem walka | 16.9 (11.0) | 12.0 (5.9) | 18.2 (10.1) | 15.3 (8.0) | −0.45 | −0.29 |
| Strength, s | ||||||
| Sit-to-standa | 12.6 (6.5) | 11.4 (4.1) | 12.3 (3.3) | 11.7 (3.5) | −0.18 | −0.19 |
Notes: L = left; R = right.
a The best scores are the lowest.
bSD of baseline scores.
In Table 3 ▶, unstandardized regression coefficients indicate the number of seconds or centimeters of change associated to being part of the experimental group. Assessment of the effect of group membership, with control only for balance at baseline (reduced model), revealed intervention group improvements in 4 indicators of static balance and mobility. After adjusting for demographic, health, and physical activity characteristics (complete model), the intervention effects on 5 of the balance assessments were statistically significant: one-legged stance eyes open (both sides), one-legged stance eyes closed (left), tandem stance, and tandem walk. As for strength, change among participants in the intervention was positive, but results were not statistically significant. Results of the linear regression analysis with the complete model suggest that the program—and not differences in composition of experimental and control groups—was responsible for improving balance in the experimental group. The proportion of variance explained by group membership (partial η2) was highest for static balance and mobility indicators.
TABLE 3—
Balance and Strength Evolution After Control for Covariates
| Reduced Modela | Complete Modelb | ||||||||
| Outcome Variables | Unstandardized Coefficient βc | P | R2 | Unstandardized Coefficient βc | 95% CI | Standardized Coefficient βc | P | R2 | Partial η2 d |
| Static balance, s | |||||||||
| One-legged stance—eyes open, L | 7.44 | < .01 | 0.51 | 7.48 | (3.79, 11.18) | 0.21 | < .01 | 0.62 | 10.9% |
| One-legged stance—eyes open, R | 4.43 | .02 | 0.56 | 5.12 | (1.21, 9.03) | 0.14 | .01 | 0.61 | 3.8% |
| One-legged stance—eyes closed, L | 1.00 | < .01 | 0.48 | 0.97 | (0.26, 1.68) | 0.16 | .01 | 0.52 | 5.4% |
| One-legged stance—eyes closed, R | 0.54 | .19 | 0.41 | 0.64 | (−0.21, 1.49) | 0.09 | .14 | 0.44 | 1.3% |
| Tandem stance | 4.00 | .12 | 0.54 | 5.16 | (0.22, 10.09) | 0.11 | .04 | 0.63 | 2.3% |
| Limits of stability, cm | |||||||||
| Functional reach | 0.79 | .32 | 0.41 | 0.48 | (−1.07, 2.02) | 0.04 | .55 | 0.51 | 0.5% |
| Lateral reach, L | 0.16 | .81 | 0.29 | 0.20 | (−1.16, 1.56) | 0.02 | .77 | 0.35 | 0.2% |
| Lateral reach, R | 0.39 | .58 | 0.21 | 0.56 | (−0.86, 1.98) | 0.06 | .44 | 0.30 | 0.6% |
| Mobility, s | |||||||||
| Tandem walk | −3.55 | .01 | 0.13 | −3.80 | (−6.48, −1.12) | −0.21 | .01 | 0.26 | 4.9% |
| Strength, s | |||||||||
| Sit-to-stand | −0.46 | .26 | 0.54 | −0.54 | (−1.34, 0.26) | −0.07 | .19 | 0.60 | 0.8% |
Notes: L = left; R = right.
aReduced model included baseline measure and group membership.
bThe variables included in the complete model of the linear regression analysis are as follows: measures of balance at baseline, a series of demographic variables (age, gender, and level of education), a series of physical health variables (perceived health status, number of medical consultations during the last 3 months, number of health problems, and number of medication classes), mental health, fall history and balance self-confidence, and practice of physical activity (frequency and diversity).
cβ = regression coefficient of the group membership variable (evolution attributable to membership in the experimental group).
dPartial η2 = proportion of the variance explained by group membership (experimental/control).
Finally, interaction terms testing the modifying effects of age, history of falls, perceived health status, and baseline level of balance showed no consistent pattern. However, the following interaction effects were statistically significant: (1) for static balance, baseline values in the one-legged stance left with eyes closed modified intervention effects, with improvement being most pronounced among individuals with the highest baseline initial scores (P = .001); (2) for limits of stability, history of falling modified intervention effects on lateral reach (left; P = .03), with people who had experienced the most falls improving the least; (3) for mobility, age modified the intervention effect (P = .03), with improvements being superior among older people, and perception of health also modified intervention effects (P = .04), with higher improvements among persons judging their health to be neither poor nor excellent; and (4) for strength, baseline values in the sit-to-stand modified intervention effects, with more pronounced improvements among individuals with weakest scores at baseline (P < .001).
Compliance and Attendance Rates
The attendance rate for group exercise sessions was 78%. Seventy percent of intervention participants attended more than three fourths of the sessions (16 of 22 sessions). Five people dropped out during the first 2 weeks of the program. Regarding self-reported home exercise compliance, 78% of participants in the experimental group indicated they exercised at home at least once a week, as recommended by the Stand Up! program.
DISCUSSION
Summary of Results
The purpose of this study was to determine the effectiveness of a group-based exercise intervention designed to improve balance among older adults when delivered in a real-world setting by local community organizations. Results showed that a structured, group-based exercise program offered by personnel and staff at older-adult community centers and health clinics successfully increased static balance and mobility among older adults concerned about falls.
These findings are consistent with those of previous researchers7,8,32 who reported that group-based (therefore, not individually prescribed) exercises targeting balance can actually improve balance among older adults. However, to our knowledge, this is the first study to demonstrate that intervention effects on balance are possible when the intervention is managed by community organizations and when participants register because they are concerned about their balance or worried about falls. In previous studies, interventions were carried out in research contexts, and participants were randomly assigned either to intervention or placebo groups. Participants either came from a sample drawn from electoral lists7 or were referred by their physicians or other health professionals.8 In our study, community organizations were responsible for recruiting participants and delivering the intervention. We believe this is an important step in moving efficacious interventions into community health promotion programs (for fall prevention) and making them widely accessible.
Strengths of the Study
Our effectiveness study measured the impact of an intervention tested under normal conditions in the field33 with a rigorous methodology and valid indicators for several dimensions of the outcome. The 10 intervention organizations represented a broad range of environments, and the study obtained a high follow-up rate of 88.5%. Finally, an effort was made to document participation in the study and participants’ attendance in the intervention without disturbing the natural dynamics of the setting.
Limitations
The question arises whether the 10 organizations that offered the program are different and perhaps more dynamic than the control organizations (early adopter effect). Given that all of the organizations—even the control organizations—showed a marked interest in offering the program, we believe that the early adopter effect was minimal.
As in any nonrandomized study design, one cannot completely exclude the possibility of a confounding variable not controlled by the analysis. However, given the similarity of the experimental and control organizations, similar manner in which the subjects were selected, pairing of experimental and control groups for season, rigorous measurement process for balance (e.g., rigorous protocol, supervised measuring, and blind testing) and analysis strategies chosen, it is likely that participation in the Stand Up! program is, indeed, responsible for improvements in the group that received the intervention. Furthermore, some authors believe that randomized controlled trials are not the ideal model when interventions are complex or designed for a variety of settings.33,34
Generalizability of the Results
With respect to the intervention, this program can be used elsewhere and is likely to have similar effects when offered to a similar target population. A complete intervention guide is available, making it easy to use in different settings. More broadly, we have shown that group-based exercises programs can effectively enhance balance. To do so, these programs must do the following: (1) focus on the various systems involved in balance; (2) respect known principles of the biomechanical model for efficacy, such as intensity of training, overloading, and progression35; (3) succeed in obtaining high attendance rates; and (4) be adapted to the realities of local community organizations.
With respect to participants (at the individual level), subjects registering in this study were quite heterogeneous in terms of demographics and health status at baseline. Subgroup analysis revealed few significant interaction effects, indicating that the program is probably equally effective across subgroups of older adults differing in age, history of falls, perceived health status and balance at baseline, and who chose to engage in this type of program. With aging, balance deficits are progressive; therefore, self-selection of people concerned with their balance and worried about falls seems appropriate. Given that individuals who did not attend the posttest were more frail than those who remained in the study, we must be cautious when generalizing program results to people who are the most frail. However, this latter group represents only 11.5% of people registered in the study. For maximum effect, the population needs to be neither too fit nor too frail.5
Program Effect on Falls
The program model postulates that, among older adults who are aware of mild difficulties with their balance, improving balance can reduce the overall number of falls and fall injuries. It was not possible to record falls appropriately (e.g., monthly phone calls or weekly postcards) in the context of this study. However, a recent randomized controlled trial8 showed that with an improvement in balance of the magnitude observed in the present study, the fall rate of intervention participants was 40% lower than that of control participants. Given that the intervention in the study by Barnett et al.8 comprised only exercises, it is likely that the reduction in falls observed by Barnett et al.8 is related to the degree of balance improvement. It is reasonable to anticipate that improvements in balance observed in the present study would also translate into a reduction in falls. In addition, the most recent literature suggests that specific balance and strength exercise programs are effective in reducing the risk of falling. However, their optimal intensity and frequency remain to be determined.1,36
Several issues pertaining to fall prevention await additional research. For example, it would be useful if future trials examined how long the effects of exercise interventions last, under what conditions, and to what extent organizations continue offering the program. In this regard, analyses pertaining to the maintenance of intervention effects on balance 9 months after the end of the program are currently underway for future publication. Additional research is also required to discuss the pertinence of allotting public funds to such a program or having insurers pay for it.
Conclusions
The study design was that of a plausibility evaluation.33,34 We examined the impact of an intervention on an intermediate variable (balance) and ruled out alternative explanations by including a control group and by controling for the main confounding variables. The intervention assessed—the Stand Up! program—reconciles the requirements to implement a program that is of appropriate intensity to actually improve balance while being flexible enough to be delivered in community settings. The intervention appears to be powerful enough to exert an impact on balance in a variety of clienteles in an array of settings.
These results should interest community organizations that already offer physical activity programs and that are actively involved in fall prevention. It should also be of value to clinicians who adopt the recommendations of Tinetti et al.1 and would like to refer patients more than 75 years of age to such programs. Finally, these results could also benefit public health authorities seeking effective methods for reducing risk factors for falls in an aging population.
Acknowledgments
This research was funded by the Canadian Institutes of Health Research (Health Services Research-Population and Public Health) (grant MOP 53123). It was also supported by the Montréal Public Health Department (Direction de santé publique de Montréal).
We are grateful for the dedication and support of Carole Genest, Jennifer Duplantie, and Martine Comeau, who were involved in data collection, coding, and data management. We also thank Sylvie Gauthier, who helped with revising prose and style of this article. We thank study participants who gave their time to complete questionnaires and perform balance tests. We also thank the many community organizations, interviewers, and physiotherapists who collaborated in the study.
Human Participant Protection Ethical approval for this study was obtained from the research ethics committee of the Regional Health and Social Services Board, Montreal, Quebec.
Peer Reviewed
Contributors Y. Robitaille, S. Laforest, L. Gauvin, M. Parisien, F. Trickey, and N. Damestoy conceptualized the study. Y. Robitaille was principal investigator and supervised all aspects of its implementation. S. Laforest assisted in its implementation and led the development of questionnaires and balance measurements. M. Fournier conducted the analyses and assisted in interpretation. L. Gauvin actively assisted in analyses, interpretation, and write-up of the article. M. Parisien conceptualized data collection and contributed to the implementation of the study. H. Corriveau contributed to all matters related to physical performance measurements. F. Trickey specifically contributed by networking with community organizations. All authors reviewed drafts of the article.
References
- 1.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. [DOI] [PubMed] [Google Scholar]
- 2.Vyrostek SB, Annest JL, Ryan GW. Surveillance for fatal and nonfatal injuries—United States, 2001. MMWR Surveill Summ. 2004;53:1–57. [PubMed] [Google Scholar]
- 3.de Rekeneire N, Visser M, Peila R, et al. Is a fall just a fall: correlates of falling in healthy older persons. The Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:841–846. [DOI] [PubMed] [Google Scholar]
- 4.Province MA, Hadley EC, Hornbrook MC, et al. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA. 1995;273:1341–1347. [PubMed] [Google Scholar]
- 5.Gardner MM, Robertson MC, Campbell AJ. Exercise in preventing falls and fall related injuries in older people: a review of randomised controlled trials. Br J Sports Med. 2000;34:7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;4:CD000340. [DOI] [PubMed] [Google Scholar]
- 7.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32: 407–414. [DOI] [PubMed] [Google Scholar]
- 9.Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93: 1261–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duncan PW, Chandler J, Studenski S, Hughes M, Prescott B. How do physiological components of balance affect mobility in elderly men? Arch Phys Med Rehabil. 1993;74:1343–1349. [DOI] [PubMed] [Google Scholar]
- 11.Trickey F, Parisien M, Laforest S, Genest C, Robitaille Y. STAND UP! A programme to fall for. Montréal: Direction de santé publique, Régie régionale de la santé et des services sociaux de Montréal-Centre; 2003.
- 12.Trickey F, Robitaille Y, Laforest S, Gosselin C, Parisien M. Prévenir les chutes chez les aînés: évaluation du programme PIED. Rapport synthèse. Montréal: Direction de la santé publique de Montréal-Centre, Régie régionale de la santé et des services sociaux; 1999.
- 13.Franchignoni F, Tesio L, Martino MT, Ricupero C. Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging (Milan). 1998;10:26–31. [DOI] [PubMed] [Google Scholar]
- 14.MacKnight C, Rockwood K. Assessing mobility in elderly people. A review of performance-based measures of balance, gait and mobility for bedside use. Rev Clin Gerontol. 1995;5:464–486. [Google Scholar]
- 15.El Kashlan HK, Shepard NT, Asher AM, Smith-Wheelock M, Telian SA. Evaluation of clinical measures of equilibrium. Laryngoscope. 1998;108: 311–319. [DOI] [PubMed] [Google Scholar]
- 16.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45:M192–M197. [DOI] [PubMed] [Google Scholar]
- 17.Brauer S, Burns Y, Galley P. Lateral reach: a clinical measure of medio-lateral postural stability. Physiother Res Int. 1999;4:81–88. [DOI] [PubMed] [Google Scholar]
- 18.Newton RA. Balance screening of an inner city older adult population. Arch Phys Med Rehabil. 1997; 78:587–591. [DOI] [PubMed] [Google Scholar]
- 19.Dargent-Molina P, Favier F, Grandjean H, et al. Fall-related factors and risk of hip fracture: the EPI-DOS prospective study. Lancet. 1996;348:145–149. [DOI] [PubMed] [Google Scholar]
- 20.Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills. 1995;80:163–166. [DOI] [PubMed] [Google Scholar]
- 21.Ostchega Y, Harris TB, Hirsch R, Parsons VL, Kington R, Katzoff M. Reliability and prevalence of physical performance examination assessing mobility and balance in older persons in the US: data from the Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2000;48:1136–1141. [DOI] [PubMed] [Google Scholar]
- 22.Smidt GL. Gait in Rehabilitation. New York: Churchill Livingston, 1990.
- 23.Mathiowetz V. Reliability and validity of grip and pinch strength measurements. Phys. Rehabil. Med. 1991;2:201–212. [Google Scholar]
- 24.Desrosiers J, Bravo G, Hebert R, Dutil E. Normative data for grip strength of elderly men and women. Am J Occup Ther. 1995;49:637–644. [DOI] [PubMed] [Google Scholar]
- 25.Weiner DK, Bongiorni DR, Studenski SA, Duncan PW, Kochersberger GG. Does functional reach improve with rehabilitation ? Arch. Phys. Med. Rehabil. 1993;74: 796–800. [DOI] [PubMed] [Google Scholar]
- 26.Bellerose C, Lavallée C, Chénard L, Levasseur M. Et la santé, ça va en 1992–1993? Rapport de l’Enquête sociale et de santé 1992–1993, volume 1. Montréal: Santé Québec, ministère de la Santé et des Services sociaux, Gouvernement du Québec; 1995.
- 27.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–354. [DOI] [PubMed] [Google Scholar]
- 28.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30: 473–483. [PubMed] [Google Scholar]
- 29.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–M34. [DOI] [PubMed] [Google Scholar]
- 30.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. [DOI] [PubMed] [Google Scholar]
- 31.SPSS for Windows, Rel. 11.01. Chicago: SPSS Inc; 2001.
- 32.Suzuki T, Kim H, Yoshida H, Ishizaki T. Randomized controlled trial of exercise intervention for the prevention of falls in community-dwelling elderly Japanese women. J Bone Miner Metab. 2004;22:602–611. [DOI] [PubMed] [Google Scholar]
- 33.Victora CG, Habicht JP, Bryce J. Evidence-based public health: moving beyond randomized trials. Am J Public Health. 2004;94:400–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Habicht JP, Victora CG, Vaughan JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol. 1999;28:10–18. [DOI] [PubMed] [Google Scholar]
- 35.American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. [DOI] [PubMed] [Google Scholar]
- 36.Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328:680. [DOI] [PMC free article] [PubMed] [Google Scholar]