Abstract
Native Americans served by the Aberdeen, Billings, and Bemidji areas of the Indian Health Service (IHS) have a cancer mortality rate approximately 40% higher than that of the overall US population. The National Cancer Institute has funded Rapid City Regional Hospital to provide clinical trials, behavioral research, a genetic protocol, patient navigator services (assisting patients with health care coordination and financial issues and helping them to understand their options), and community education for members of 3 western South Dakota tribes.
Challenges faced by the project included obtaining multiple approvals from 3 tribes, 4 IHS facilities, and 5 institutional review boards; travel distances; lack of screening; red tape of referrals; and refusal by some payers to cover clinical trials. Building trust through ongoing communication and community presence is key to a successful project.
IN THE UNITED STATES, various subpopulations experience different rates of cancer detection, treatment, participation in clinical trials, and outcomes.1–4 In particular, the population of Native Americans served by the 10-state Billings, Aberdeen, and Bemidji service areas of the Indian Health Service (IHS) suffers from a cancer mortality rate approximately 40% higher than that of the overall US population.5 Researchers from the IHS analyzed cancer mortality data from the death certificate database of the National Center for Health Statistics, which were adjusted for racial miscategorization and the age structure of the population, and then summarized the results for 1994 through 1998. Although their rates of breast cancer mortality were approximately 15% lower than for Whites, Native Americans in this 10-state Northern Plains region had significantly higher average annual age-adjusted mortality rates for colorectal cancer (58% higher), lung cancer (62%), cervical cancer (79%), and prostate cancer (49%).5
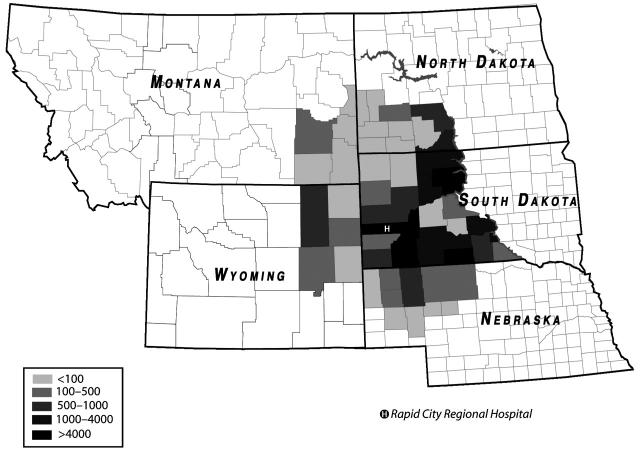
Rapid City Regional Hospital, in the Black Hills of western South Dakota, provides secondary and tertiary cancer care for an estimated 60 000 Native Americans living within a 200-mile radius of Rapid City (Figure 1 ▶). Most of these tribal members live in the IHS Aberdeen Area (North Dakota, South Dakota, Iowa, and Nebraska). In 1996 through 1998, the life expectancy at birth (both genders) for Native Americans in the Aberdeen Area was 65.4 years, compared with 70.6 years for all IHS areas (1996–1998) and 76.5 years for the general US population (1997).6
FIGURE 1—
Native American population, by county, for the region using Rapid City Regional Hospital.
Source. 2000 US Census data.
The local population served by Rapid City Regional Hospital is growing very rapidly, with nearly 50% of the population aged younger than 18 years, according to data from the 2000 US Census. In 1996 through 1998, the leading causes of death in the Aberdeen Area were diseases of the heart (21% of deaths), malignant neoplasms (15%), unintentional injuries (14%), diabetes mellitus (8%), and chronic liver disease and cirrhosis (6%).6
A retrospective chart review was performed for 93 Native American radiation therapy patients treated at the hospital’s Cancer Care Institute between January 1998 and October 2002.7 The median one-way distance patients traveled was 109 miles (ranging from 5 to 215 miles). Thirty-seven percent of Native American patients traveled at least 150 miles each way. Of 61 Native American patients treated with curative intent, 28% had treatment delays (i.e., missed days) of 6 or more days and 15% had delays of 11 or more days. Thirty of the patients (half) experienced grade 2 radiation treatment toxicities, and 10 had grade 3 radiation treatment toxicities.
Statistics from Rapid City Regional Hospital’s Tumor Registry (1990–2000) indicate that Native Americans are more likely than other patients to present with advanced (stage III or IV) disease, which leads to lower survival rates (Table 1 ▶).7 For colorectal, breast, prostate, cervical, and lung cancer, approximately 50% of Native Americans arrived at the hospital with advanced cancer, as opposed to 36% of non–Native Americans.
TABLE 1—
Percentages of Native Americans and Non–Native Americans Presenting at Rapid City Regional Hospital With Advanced (Stage III or IV) Cancer: Tumor Registry Data, 1990–2000
| Cancer Type | % Presenting With Stage III or IV Disease (n) | |
| Native American | Non–Native American | |
| Lung | 72 (92/127) | 68 (669/989) |
| Breast | 16 (12/75) | 10 (111/1127) |
| Colorectal | 48 (26/54) | 40 (298/739) |
| Prostate | 44 (22/50) | 30 (281/945) |
| Cervix | 53 (8/15) | 26 (13/51) |
A sizeable literature exists on the barriers to equal health-related behaviors, health care, and outcomes for minority groups in the United States. In a review of the published literature through 1996, Guidry et al. identified barriers such as communication problems between patients and providers, lack of information on side effects, cost of treatment, difficulty in obtaining and maintaining insurance coverage, and absence of social support networks.8 Other studies on the barriers to healthy behavioral choices and to timely and effective health care for minority groups have identified additional problems, including the need for social support9; poor communication between patient and provider regarding different understandings of health and disease10; fear, language barriers, and lack of education and acculturation11; perceived racial, economic, and gender bias12; lack of a regular doctor13; lack of cultural competence on the part of nurses14; and low levels of health literacy.15
Barriers to timely and effective cancer diagnosis and treatment for Native Americans in western South Dakota include the following: lack of knowledge of the disease, its screening, and treatment; logistical problems (e.g., transportation, finances, family care, communications) in accessing cancer-related health care; lack of trust, hope, or emotional support concerning cancer treatment and recovery; and the red tape involved in dealing with multiple health care entities, which leads to problems in obtaining test results, understanding options, being referred, and making payments. Taken together, these data and barriers indicate that in our region, cancer outcomes for Native Americans are significantly poorer than those for non–Native Americans. We have outlined obstacles to and solutions for a cancer research program attempting to resolve these disparities.
THE PROJECT
The National Cancer Institute’s Cancer Disparities Research Partnership (CDRP) program has funded 6 sites across the United States to research and reduce cancer mortality disparities among various minority populations. Rapid City Regional Hospital’s CDRP grant, “Enhancing Native American Participation in Radiation Therapy Trials,” provides clinical trials, behavioral research, a genetic protocol, Patient Navigator services, travel assistance, and community education for members of 3 Lakota tribes in western South Dakota (Oglala, Rosebud, and Cheyenne River Sioux tribes) as well as the Native American population in Rapid City. The 5-year project was initiated in late 2002.
KEY FINDINGS.
Native Americans in the IHS Northern Plains Region have significantly higher age-adjusted rates of cancer mortality than the general US population.
Native Americans in western South Dakota present with more advanced stages of cancer than do non–Native Americans in the region.
The Cancer Disparities Research Partnership project at Rapid City Regional Hospital is positioned to have a significant impact on cancer health care for the Native American population of western South Dakota.
Building trust requires going through the full tribal and IHS approval process, including taking time to educate and to answer questions.
Building trust also requires a commitment to providing needed services in the community over time and in a culturally appropriate way.
The goal of this grant project is to reduce cancer mortality rates for Native Americans in the region. Specific objectives that support this goal are as follows:
To document the major factors responsible for cancer health disparities in the Native American population served by Rapid City Regional Hospital;
To determine whether shorter, but equally effective, courses of treatment will enhance the acceptability and completion rate of radiotherapy; and
To ascertain whether there may be a genetic basis for anecdotal reports that Native Americans experience increased radiation toxicities.
With a staff of 10 (including 4 field staff members), 2 collaborating partner institutions (University of Wisconsin–Madison and Mayo Clinic–Rochester), numerous consultants, and 8 unique research protocols, this large project is positioned to significantly affect the approach to cancer-related health care for the Lakota Nation.
OBSTACLES TO OVERCOME
The project has had to overcome a number of serious obstacles. The most immediate of these has been the need to obtain multiple approvals for each research protocol. Clinical protocols (brachytherapy and to-motherapy radiation treatment trials) have each required the approval of 4 institutional review boards (IRBs): those of the University of Wisconsin, the Rapid City Regional Hospital, the Aberdeen Area IHS, and the national IHS. Survey and Patient Navigator protocols have each required the approval of 3 IRBs: those of the Rapid City Regional Hospital, the Aberdeen Area IHS, and the national IHS. The genetic protocol will require approval from 5 IRBs (those already named and the Mayo Clinic IRB). Furthermore, before considering these protocols, the IRB of the Aberdeen Area IHS requires resolutions of support from each of the 3 tribes involved, from the chief executive officers at the IHS hospitals on the 3 reservations and in Rapid City, and from the 18-member Aberdeen Area Tribal Chairmen’s Health Board. Arguably, IHS IRB approvals were not required because we are not using any IHS staff, data, or patient records for the research; however, we felt these approvals were extremely important for maintaining good relationships and ensuring broad-based community support for our project.
The project’s approach to this daunting task has been one of patience, persistence, and relationship building. Staff members meet frequently with and make periodic presentations to tribal councils, tribal health boards, IHS decisionmakers, community leaders, and the Aberdeen Area Tribal Chairmen’s Health Board. Working groups were held on each reservation and in Rapid City to receive input on survey questions. A biweekly to monthly radio show allowed us to talk about the importance of early detection and treatment for cancer. A community genetics education curriculum was being developed to explain the value of the cancer-related genetic test we plan to offer.
We have received approval for all of our 8 protocols from all the relevant IRBs and tribal entities and from the Aberdeen Area Tribal Chairmen’s Health Board. We gained the necessary support from the tribes by explaining our research protocols, making the case for their usefulness to individual cancer patients and to the tribe, answering questions openly, and providing frequent updates to decisionmakers and community members. For each tribal resolution of support, we included language ensuring that research results would be shared with the tribe. We could not, however, share raw data, because this would constitute a violation of confidentiality. Therefore, we shared results in the form of quarterly written updates that were presented to tribal councils and the Tribal Chairmen’s Health Board each time we met with them. Moreover, our IHS IRB approvals required us to obtain tribal approvals prior to publications about the study. For example, we have letters of approval from all 3 tribes for this article.
Another set of obstacles reflects the barriers that face Native Americans needing cancer treatment: long travel distances; lack of screening opportunities; lack of education about cancer; IHS funding shortfalls; the red tape of patient referrals; payment problems involving the IHS, Medicare, Medicaid, the Department of Veterans Affairs, TRICARE (military health care program), and private insurers; and the refusal of some payers to cover clinical trials. Our staff mitigate these issues on a daily basis, with help from the tribes, the IHS, contract health offices, the National Breast and Cervical Cancer Early Detection Program, nonprofit organizations such as the American Cancer Society, and others. Constant networking, communication, and brainstorming allow us to keep everyone in the loop and look for creative ways to resolve the various roadblocks that arise. The long travel distances from the reservation to the Cancer Care Institute are mitigated through a grant fund that provides money to cancer patients for gas, food, and lodging as part of our Patient Navigator program. Sophisticated telemedicine equipment provided by the grant will be used for patient consultations so that lengthy trips can be avoided where possible.
A third obstacle is the fact that Rapid City Regional Hospital had not received federal research grants in the past and thus had not developed either the necessary infrastructure for administering grants or a culture that supports research. Other hospitals located close to rural Native American populations are likely to face the same situation. The National Cancer Institute’s CDRP program anticipated this problem, providing for advice and mentoring from 2 experienced partner institutions (University of Wisconsin–Madison and Mayo Clinic–Rochester).
Perhaps the most fundamental obstacle to this project is the historical reality of relationships between the Lakota and non–Native American (White) populations over the past century and a half. Many Native Americans in western South Dakota have had experiences or heard stories that led them to doubt their welcome in Rapid City and at Rapid City Regional Hospital. Some Native Americans, particularly those with a more traditional perspective, do not trust Western medicine, medical research, or genetic testing.
Building trust, therefore, is an essential component of all our activities. Trust requires openness, honesty, culturally appropriate messages, culturally integrated staff, services that people can appreciate, long-term commitments, consistency, patience, and time. As Lakota people often say, “We have to do this in a good way.” Without such trust, none of our research studies would receive the approvals required to begin, let alone the necessary community cooperation required to succeed. If the project succeeds in developing effective programs that help lower cancer mortality rates, it will constitute a milestone in reconciliation as well as in the interrelated challenge of reducing health care disparities.
Acknowledgments
We gratefully acknowledge the funding and support of the Cancer Disparities Research Partnership, Radiation Research Program, National Cancer Institute (contract N01-CO-12400). Administrative support and facilities are provided by Rapid City Regional Hospital.
We thank the key individuals who have been instrumental in designing the research described in this report: Minesh Mehta of the University of Wisconsin Comprehensive Cancer Center; Norm Coleman, Frank Govern, and Rosemary Wong of the Radiation Research Program, National Cancer Institute; Christen Osburn of SAIC-Frederick, Inc (government contractor); Judith Kaur of Mayo Clinic–Rochester Comprehensive Cancer Center; Linda Burhansstipanov of Native American Cancer Research Corporation; and Petra Helbig of Rapid City Regional Hospital. We especially appreciate the efforts of our staff who are on the front lines daily, building community trust and confronting cancer: Kevin Molloy, Cathey Ducheneaux, and Mary Reiner, Rapid City; Caroline Spotted Tail, Rosebud; Raylene LeBeau, Cheyenne River; and Scotty Crawford, Pine Ridge.
Human Participant Protection All 8 study protocols received resolutions of support from the Oglala Sioux Tribal Council, the Rosebud Sioux Tribal Council, the Cheyenne River Sioux Tribal Council, the Pine Ridge Indian Hospital CEO, the Cheyenne River Public Health Service Hospital CEO, the Rosebud IHS Hospital CEO, the Rapid City Public Health Service Indian Hospital CEO, and the Aberdeen Area Tribal Chairmen’s Health Board, and have received approvals as required from institutional review boards at the University of Wisconsin, Rapid City Regional Hospital, Aberdeen Area IHS, and National IHS. The retrospective chart review referred to in Table 1 ▶ was approved by Rapid City Regional Hospital’s institutional review board.
Peer Reviewed
Note. The opinions expressed in this report are those of the authors and do not necessarily reflect the views of the Indian Health Service.
Contributors D. Rogers wrote and edited the report and manages the implementation of nonclinical aspects of the research. D. G. Petereit conceived of the idea for the research and directs the research and contributed ideas for and revised the report.
References
- 1.Bobinski MA. Health disparities and the law: wrongs in search of a right. Am J Law Med. 2003;29: 363–380. [PubMed] [Google Scholar]
- 2.Geiger HJ. Racial and ethnic disparities in diagnosis and treatment: a review of the evidence and a consideration of causes. In: Smedley BD, Smith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine, National Academies Press; 2003:415–454. [PubMed]
- 3.Sateren WB, Trimble EL, Abrams J, et al. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. J Clin Oncol. 2002;20:2109–2117. [DOI] [PubMed] [Google Scholar]
- 4.Hayes MA, Smedley BD. The Unequal Burden of Cancer: An Assessment of NIH Research and Programs for Ethnic Minorities and the Medically Underserved. Washington, DC: Institute of Medicine, National Academies Press; 1999. [PubMed]
- 5.Espey DK, Paisano RE, Cobb N. Cancer Mortality Among American Indians and Alaska Natives: Regional Differences, 1994–1998. Rockville, Md: Indian Health Service; 2003. IHS publication 97-615-28.
- 6.2000–2001 Regional Differences in Indian Health. Rockville, Md: Indian Health Service, US Dept of Health and Human Services; 2002.
- 7.Petereit DG, Rogers D, Helbig P, et al. Geographic distance from the cancer center may be a treatment barrier for American Indians undergoing radiotherapy. Paper presented at: Intercultural Cancer Council 9th Biennial Symposium on Minorities, the Medically Underserved and Cancer; March 24–28, 2004; Washington, DC.
- 8.Guidry JJ, Greisinger A, Aday LA, Winn RJ, Vernon S, Throckmorton TA. Barriers to cancer treatment: a review of published research. Oncol Nurs Forum. 1996;23:1393–1398. [PubMed] [Google Scholar]
- 9.Cook GC, Wilson ME. Social support and cancer screening in African American, Hispanic, and Native American women. Cancer Pract. 1998;6: 31–37. [DOI] [PubMed] [Google Scholar]
- 10.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18:146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Otero-Sabogal R, Owens D, Canchola J, et al. Mammography rescreening among women of diverse ethnicities: patient, provider, and health care system factors. J Health Care Poor Underserved. 2004;15:390–412. [DOI] [PubMed] [Google Scholar]
- 12.La Veist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57: 146–161. [DOI] [PubMed] [Google Scholar]
- 13.Cornelius LJ, Smith PL, Simpson GM. What factors hinder women of color from obtaining preventive health care? Am J Public Health. 2002;92: 535–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzalez RI, Gooden MB, Porter CP. Eliminating racial and ethnic disparities in health care. Am J Nurs. 2000;100:56–58. [PubMed] [Google Scholar]
- 15.Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol. 2002; 186:938–943. [DOI] [PubMed] [Google Scholar]