Abstract
For a brief period from the 1930s through the early 1940s, public health advocates made pneumonia a leading public health concern. Predicated on the need for antipneumococcal antiserum, but also incorporating physician reeducation, state “pneumonia control programs” were established nationwide.
However, with the advent of penicillin and the sulfonamides, the pneumonia control programs soon collapsed. Pneumonia reverted to the domain of the private practitioner, which was devoid of state oversight. With the emergence of pneumococcal antibiotic resistance in the 1990s, the possibility again arose that pneumonia could become a public health concern, given the nationwide need to curb unnecessary antibiotic usage and to encourage vaccination. An understanding of the history of pneumonia’s changing status could shed light on current attempts to reformulate the disease and elucidate the contested domains of private practice and public health.
BY NOVEMBER OF 1937, when he convened a national committee to plan an attack on pneumonia, then the leading infectious cause of death in the country, Surgeon General Thomas Parran had placed pneumonia alongside tuberculosis and venereal disease as one of the nation’s foremost public health concerns.1 Yet by the end of World War II, pneumonia—William Osler’s “Captain of the Men of Death”—had completely reverted to the domain of the private practitioner, where it had resided prior to the 1930s and has largely remained since.2 Understanding the forces that have mediated such an ongoing transformation offers insights not only into our current limitations in combating pneumonia as a national problem but also into the nature of the contested domains of private practice and public health.
SEROTHERAPY AND THE TRANSFORMATION OF PNEUMONIA INTO A PUBLIC HEALTH CONCERN
The transformation of pneumonia into a public health concern in America was contingent on the rise of antipneumococcal antiserum as a therapeutic modality. Following the advent of the germ theory of disease, immunology itself emerged as a science in the last decades of the 19th century. If the late 1870s and early 1880s marked the onset of the discovery of infectious agents of disease, the late 1880s and early 1890s witnessed the beginning of the medical attack on such pathogens through applied humoral immunology. Over the ensuing decades, antidiphtheria and antitetanus antitoxins would serve as the most famous representatives of the subsequent applied immunological “specifics,” arrayed alongside such novel chemotherapeutic approaches to infectious diseases as Paul Ehrlich’s Salvarsan. Perhaps no such therapy, however, so clearly embodied the rise and limitations of antimicrobial therapy in the decades between the golden age of microbiology and the antibiotic era as antipneumococcal antiserum.
In 1892, William Osler famously wrote of pneumonia, “It is a self-limited disease, and has its course uninfluenced in any way by medicine.”3 One year earlier, however, the first attempt to treat pneumococcal pneumonia with rabbit serum (generated through inoculating rabbits with pneumococci) had taken place in Germany.4 By 1913, after 2 decades of mixed results, serotherapy directed against the pneumococcus would be redefined through the efforts of Rufus Cole and his colleagues at the newly constructed Hospital of the Rockefeller Institute. Reclassifying pneumococci into 4 serological “types,”5 they argued that serologically specific pneumococci apparently called for type-specific therapy; focusing on the treatment of the lethal and prevalent type I pneumococcus with type-specific horse serum, Cole and his colleagues could report a reduction in mortality from more than 25% to 7.5%.6
By the late 1920s, type I–specific antipneumococcal serotherapy had been proved efficacious in the large hospitals of the northeast—especially if given early in the disease’s course—through one of the first collaborative controlled clinical trials performed in this country (in part funded by the Metropolitan Life Insurance Company, which had lost more than $24 million in excess death benefits in the wake of the 1918–1919 influenza epidemic and had become one of the leading contributors to the campaign against respiratory disease in the first half of the 20th century).7
Nevertheless, at the very least, the treatment was labor intensive, expensive, and seemingly hospital dependent (to say nothing of the potential for serum reactions). When a pneumonia patient was admitted to the hospital, cultures would be obtained from the blood and the sputum (if no sputum could be coughed up, a direct lung puncture would be performed). Next, the sputum would be injected into the peritoneal cavity of a mouse and incubated; after 4 to 5 hours, the exudate contained therein would be extracted and centrifuged, and the organisms obtained would undergo what would come to be known as “typing” via agglutination reactions with type-specific diagnostic antiserum. If appropriate, antiserum would then be administered to the patient.8
Moreover, by the 1920s, such a modality exposed larger schisms within the profession, as clinicians argued over the perceived roles in the care of the pneumonia patient of “specific” therapy (i.e., therapy relying on “magic bullets” against seemingly localizable disease entities) vs physiological support of the patient as a whole, of the laboratory vs the bedside, of hospital vs home, and of science vs art.9 Thus, serotherapy and public health advocates (in particular, members of the Massachusetts Department of Public Health) realized that bringing type-specific antipneumococcal antiserum from the large metropolitan hospital to the home and the local hospital—where most patients in the early stages of the disease were seen—would entail a dramatic transformation of pneumonia into a public health concern owing to the need for centralized funding of the expensive modality, the provision of accessible “typing” stations and serum depot centers, and physician and patient reeducation.10
The earliest self-conscious effort to transform pneumonia into a public health concern began with a “fascinating administrative experiment” in resource distribution—the Massachusetts Pneumonia Study and Service, initiated by the Massachusetts Department of Public Health in 1931.11 Roderick Heffron, appointed the program’s field director, would later state his amazement that pneumonia’s public health aspects had not long been apparent prima facie. As he remarked,
Few if any diseases exact such a toll at the economic prime of life. It is therefore extremely fitting that in any consideration of public health some attention should be given to this disease. Yet almost without exception it has been completely neglected save for a passing remark of regret as to the futility of its control.12
If the medical profession could be directed to treat only appropriate cases, and treat them early, then the department
could very possibly bring the cost of the product [antiserum] to a level at which its continued production at public expense would be justified.13
By the winter of 1931 to 1932, the program was in progress. Ten intervention areas beyond Boston (which itself included 8 participating hospitals) were first chosen, not on the basis of geographic distribution (although they extended across the state) but on the basis of the range of organizational problems they posed.14 Each of these areas boasted its own serum supply and laboratory for performing sputum typing for local physicians. (By 1933, moreover, the “Neufeld test,” relying on the quellung reaction, in which type-specific diagnostic antisera could be used to “type” pneumococci in flecks of sputum at the bedside, had been developed).15 Furthermore, intensive statewide education for physicians was initiated, with a variety of “media used to spread this propaganda”15: from intensive full-day courses, to meetings in local towns and among district medical societies, to the distribution of thousands of flyers and reprints.15 To administer serum, a practitioner visiting his or her patient would have to call a state-appointed “collaborator,”16 who would confirm the diagnosis, obtain blood cultures and facilitate typing of the sputum, and either administer the serum directly or give the practitioner the appropriate serum (itself free of charge) to treat the patient “under competent guidance.”16
By the end of 1933, Heffron could congratulate himself:
It is gratifying to realize that these efforts have not been in vain, for at the present time there exists a much more widespread realization that “Something Can Be Done” for pneumonia, than has exited [sic] in this state for many years . . . . The demand for pneumococcus typing has increased approximately four fold. The demand for antipneumococcic serum has about paralleled this. If serum were to be distributed without restriction to all physicians desiring it, our total present budget would undoubtedly be insufficient to finance its production.17
But the clause “without restriction” referred not only to the volume but also to the manner of serum distribution: while the program’s goal was “decentralization,”18 its initial manifestation looked suspiciously centralized. The chief concern of local general practitioners hinged on the usage in each “area” of the 2 or more physician “collaborators” as the designated representatives of the state effort. Early grumblings by practitioners regarding the usurpation of their authority and earnings by the collaborators developed into an emerging stand against the encroachment of public health into a formerly private disease. From the center, Heffron and Gaylord Anderson, deputy commissioner of the Department of Public Health, would refer to the public–private dynamics engendered as epitomizing “a properly balanced public health program.”19 Nonetheless, while Heffron at the time had cited the “very successful” relationship thus engendered,20 final tabulation of the program, “In some respects this was a precarious system, and much depended on the local situation, medical and otherwise, and the popularity, quality, and integrity of the physicians designated as collaborators . . . . In some instances other physicians feared losing their patients to the collaborator called.”21 Moreover, private physicians’ reluctance to seek consultation with collaborators was a deterrent to serum administration, and as only 10% of all type I and (by this time) type II cases were estimated to have been treated under the collaborator system, Heffron concluded that “the collaborator system might possibly be regarded as only 10 per cent effective.”22
Thus, by the time Heffron submitted his proposal for the period 1934 to 1935, the limits of public health encroachment on private practice were becoming apparent. For an alternative model, he would this time turn to another public health effort—that concerning infantile paralysis. In the case of polio, any physician could administer state-provided convalescent serum—provided one had first performed a lumbar puncture and demonstrated spinal fluid characteristic of the disease.23 As an analog, any physician who obtained a positive type I or II pneumococcal sample within the first 4 days since the onset of a case of pneumonia could receive serum free of charge from the state.
By 1935, with the collaborator system dismantled, the Department of Public Health could regard the “experiment” in distribution a success. Despite persisting limits to serum utilization, nearly 1000 patients had been treated by nearly 400 physicians in 98 towns and 80 hospitals.24 Twenty-two percent of the patients had been treated at home.25 Type I mortality in particular was reduced from the expected baseline of nearly 25% to 11.1% when serum was administered within the first 4 days of illness and to 8.3% for such patients aged between 10 and 49 years (comprising 83% of all type I patients). In what was to become a widely repeated exercise, Heffron concluded by calculating that if the benefits of types I and II anti-pneumococcal serotherapy were to be extended nationwide, more than 18 000 fatalities per year could be avoided.26
Nevertheless, the shift in the public–private dynamics of such control was already apparent by the end of the Commonwealth Fund’s involvement in the Massachusetts program, as private practitioners were glad to accept free typing and serum—without the intrusion of state direction. When New York State followed Massachusetts in 1935 with a “pneumonia control program” of its own,27 such limits on state intrusion became still more starkly evident because of practitioners’ resistance even to being told when and how to type their sputum specimens before receiving serum from the state.28 Thus, by the time the New York State commissioner of public health, Thomas Parran—who had formulated the state’s pneumonia control program as a “complicated” union between the state public health department and medical society29—was chosen by Franklin Delano Roosevelt to become the nation’s surgeon general in 1936, the limits to public health incursion into the domain of the private practitioner had been made quite evident.
Nevertheless, as surgeon general, Parran would continue to elevate pneumonia to the status of national public health priority; at the same time, in the wake of the New Deal, he attempted to elevate the domain of the public health system vis-à-vis an increasingly entrenched organized medical profession.30 At a general level, Parran presented the increase in the US Public Health Service’s domain as the result of contemporary medical technology’s outpacing of the means of distribution:
In our grandfather’s time the country doctor riding horseback around the countryside, could carry in his saddlebags most of the medical needs of that day. How different today! . . . The mere acquisition of knowledge in itself means little unless it be translated into action . . . . There is no need for the present wide gap between what we know and what we do to promote the public health.”31
Such concerns were crystallized in the attempt to control pneumonia. Speaking in early 1938, he would relate the efforts of a village to cure a patient:
In recent years we have been concerned about another great killer, pneumonia. Just two days ago, I was in a western Pennsylvania town, and the doctor who was to meet me at the train was delayed on a case treating a patient who was ill with pneumonia. He had taken the sputum to the laboratory and found it to be type eight. He telegraphed to Harrisburg and in five hours he had his serum. Serum was given to the patient and he said it was like a miracle the way the temperature came down and the way the patient has improved. But to get that result there was needed a whole working laboratory for typing, and all the various types serving [sic] available twenty-four hours a day.32
Yet Parran had been quick to note that the success of such endeavors remained fundamentally dependent on the dynamics established between the state and its physicians. Six months into his tenure as surgeon general, he had asserted:
Do not mistake me—this wide interest of a health officer does not mean that the health department itself needs to operate or to direct many of the community measures for better health. He should be responsible only for those health services, which the individual citizen, the medical profession, the voluntary hospital, and other community agencies are unable to provide. He is concerned, however, that they be provided. This brings up many and complicated problems of relationship between the medical profession and the health department.33
The outcome of such joint problem solving was that “the public health may be promoted by using community resources to put better tools in the hands of the practicing physician.”34
The very public health–private practitioner dynamics exhibited by the Massachusetts and New York programs would thus be normalized to form the foundation of the ensuing programs throughout the country.35 Still, Parran, Roderick Heffron, and their colleagues would temporarily achieve their objective and transform pneumonia into a national public health concern, mediated chiefly through the federal funding of state programs. Indeed, by 1940, approximately two thirds of the states and territories in the country would develop pneumonia-control programs, with federal funding increasing nearly 60-fold from 3 years previously.36
In some states, the development was dramatic. In Illinois, for example, the post–New Deal largesse of federal funding for general state public health efforts appeared after 1936 “almost like manna from heaven and in amounts only dreamed of a year or so previously,” leading to an expansion of Illinois’s entire state public health ethos and infrastructure at the same time that it led to one of the most vigorous pneumonia control programs in the nation.37 In fact, the rapidity of such expansion—as Harry Dowling has noted, some states simply “rushed to start [a program] and thus become eligible for a share of the funds”—caused concern among such a serotherapy advocate (and public health supporter) as Rufus Cole, who feared it would lead to dilution of the intensive treatment of pneumonia.38 For most of the pneumonia vanguard, however, these were welcome problems, to be solved with the continued transformation of physician attitudes.39
Along with physicians, the public would also have to be educated. The primary source of such public education emerged from the national efforts of the US Public Health Service, often in conjunction with the Metropolitan Life Insurance Company (Figures 1 ▶–4 ▶ ▶ ▶).40 Their most visible production was a 12-minute film, A New Day, which debuted at Radio City Music Hall in December 1937 and was ultimately seen by more than 17 million people at 65 000 presentations nationally.41 Starring Gilbert Emery as Dr Mason—who successfully diagnoses an ailing mother’s type I pneumococcal pneumonia and saves her through the use of antiserum—the film was sent to theaters with recommended “exploitation hints” and attached media.42 Pneumonia was thus reformulated in literally dramatic fashion before the nation at large. It was presented as a specific emergency, one requiring that the public, physicians, and the public health apparatus unite to provide in timely fashion the wonders of modern therapeutics.
FIGURE 1—
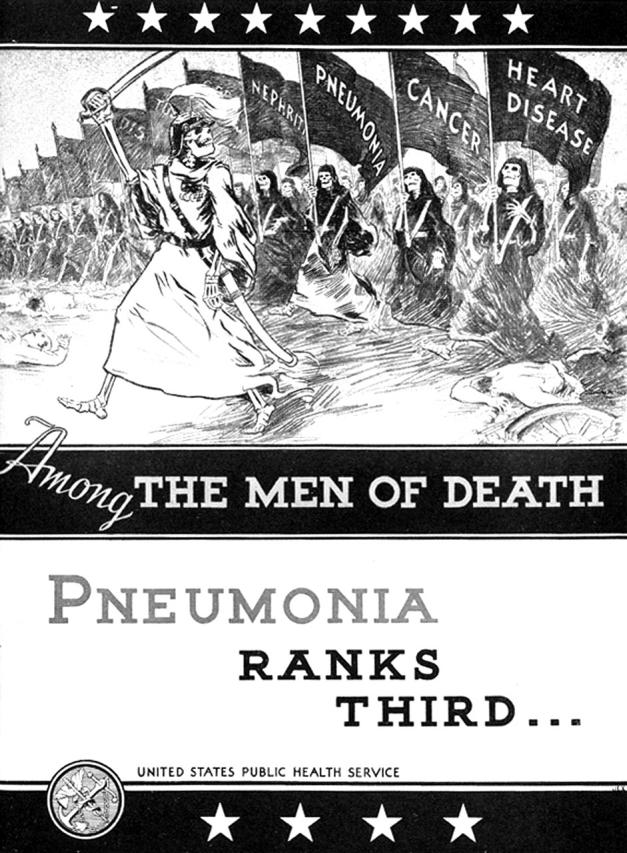
Despite the ascent of chronic diseases such as heart disease and cancer to become the nation’s leading causes of death by the late 1930s, pneumonia remained the leading infectious cause of death in the nation. Illustration from 1940 US Public Health Service brochure.
FIGURE 2—
Pneumonia was explicitly reformulated as an “emergency” in the 1930s, as pressing as appendicitis, to which it was often compared. Illustration from 1940 US Public Health Service brochure.
FIGURE 3—
Given the logistics of serotherapy, the treatment of the individual patient was transformed into a “community” responsibility. Illustration from 1940 US Public Health Service brochure.
FIGURE 4—
In an era of intense resistance to encroachment by the American Medical Association on the private practitioner’s domain, the US Public Health Service attempted to portray its role as one of friendly guide, rather than usurper of practice. Illustration from 1940 US Public Health Service brochure.
THE DECLINE OF PNEUMONIA AS A PUBLIC HEALTH CONCERN
Strong state pneumonia control programs were likewise quick to use various media, from written pamphlets to radio and live presentations, to inform both professional and lay audiences. Such state publicity efforts, however, would be highly variable, reflecting the size and scope of the pneumonia-control programs themselves. Indeed, “control” itself ranged from the provision of specific treatments to the indigent and the central monitoring of consequent therapeutic efficacy to merely ensuring that statewide laboratories were capable of round-the-clock pneumococcal typing (for the application of commercial serum).43
By early 1939, sulfapyridine—the first effective antipneumococcal sulfonamide—had been introduced nationwide, representative of the emerging chemotherapeutic revolution as applied to pneumonia. State responses again varied, and the relative degrees to which their public health departments either clung to serotherapy or recommended its abandonment reflected (and to some degree drove) the heterogeneity of such a transition among practitioners nationally.44 Serum would be advocated by its supporters first as a known therapeutic in contrast to the novel sulfonamides, later as a component of an ideal serum–sulfa combination therapy, and still later as a backup in case of sulfa intolerance or inefficacy.45 Yet by the onset of American involvement in World War II, serum had lost substantial ground in the first 2 categories,46 and by the end of the war, penicillin had rendered it obsolete as a sulfa backup.47
As members of Tennessee’s public health department would note, the affordability of the sulfa drugs and the apparent simplicity of their administration eroded the very basis for the existence of the pneumonia control programs.48 And with such forces in motion, the pneumonia control programs themselves collapsed, with none surviving the wartime effort.49 Pneumonia reverted to a private disease, apparently not requiring state oversight. As William Watt Graham Maclachlan, a prominent Pittsburgh pneumonia expert, would remark before Pennsylvania’s state medical society in 1942,
Now that the sulfonamides are being used so generously for, one might say, almost everyone who has pneumonia, the State’s interest has been satisfied. What we do now, as individual physicians, is to study carefully the results of these drugs on our cases.50
To some extent, such a process reflected the general fate of the public health system during World War II and its aftermath.51 Even within the public health system, however, pneumonia increasingly lost its standing as an issue worthy of national or statewide concern. Despite persistent claims by certain pneumonia control leaders that
to be more widely effective, the therapeutics of pneumonia, in the light of modern scientific knowledge, should be planned on a statewide basis . . . [such that] the lag between known medical science and its application be reduced to a minimum.52
Parran himself thought that pneumonia would return to the domain of the individual provider by the end of the war.53 And with pneumonia apparently having “ceased to be a major menace” since the advent of the sulfa drugs,54 Parran would, in 1944, exclude pneumonia from a list of disease entities meriting further dedicated research at his envisioned “national institutes for clinical research in . . . fields in which there is a large element of public interest.”55
In this setting, the failure of clinicians to “type” (or even obtain sputum cultures for) their pneumonia cases became further emblematic of pneumonia’s own transformation back into a private disease, increasingly managed with the use of less rigidly specific chemotherapeutics or antibiotics alone.56 Much of the sense of urgency attached to the treatment of pneumonia was itself stripped away; a sense of complacency toward pneumonia was not only permitted, but even advocated, in many presentations.57 As Russell Cecil, who had investigated the treatment of pneumonia for more than 2 decades and had headed the advisory committee of the original New York state pneumonia control program, noted in early 1940, “It would seem that the captaincy of the men of death is being passed on rather rapidly these days. I don’t think pneumonia will rank as more than a sergeant in another year or so.”58
Concerns regarding such a reconfiguration were voiced by pneumonia control veterans such as David Rutstein and Roderick Heffron.59 These warnings, however, were scarcely heeded; if anything, pleas that pneumonia continue to be regarded with concern, occurring against the backdrop of decreased reliance on sputum culture data, contributed to the extension of sulfa administration to upper respiratory tract infections as well. As a Virginia practitioner declared before his local medical society, in a near-hysterical invocation of military analogy (and with a hit clearly aimed at centralized oversight):
And now I am starting in 1941 to use sulfathiazole and sulfa-pyridine prophylactically. And why not? It has not been proven to work that way! Not scientific, you say! Remember we are front line soldiers; when we see the enemy we do not have to wait for orders from headquarters through a long line of red tape. We must go for him, without waiting for the attack! Again, it seems to me, that is common sense medicine. What do we fear in grippe or a bad cold? Pneumonia. What do we fear in whooping cough and other contagious diseases, or post-operative? Pneumonia. If pneumonia develops, we have a remedy of proven value. Why wait? Can you tell when pneumonia is going to develop? If it does develop, you would use sulfathiazole or sulfapyridine with confidence. Then why not get the jump on those tough, little bacteria? Kill them before they get a foothold. Why wait for the attack? Bomb their channel ports! Wipe out their bases of supply! Prevent their starting out in the blood stream; meet force with force!60
Again, a cadre of clinicians pleaded with their colleagues to avoid such increasingly common—and potentially harmful—overextension of sulfa administration. By the end of World War II, not only had the potential benefits of “prophylactic” therapy in upper respiratory tract infections failed to materialize,61 but the potential for such practices to lead to resistant organisms had become apparent to certain clinicians as well.62
Nevertheless, by the end of World War II, these clinicians’ ability to police or persuade their fellow practitioners regarding the treatment of respiratory tract infections had been markedly curtailed. By the mid-1950s, a study of a community in South Dakota found that 92% of the population had received antibiotics during the preceding 5 years, more than half of them for apparently inappropriate reasons.63 As James Whorton has indicated, another long-standing pneumonia researcher, Maxwell Finland, and his colleagues would in this setting attack such “omnibiotic” administration, and fellow pneumonia-control veteran Hobart Reimann lamented in 1961 that “an estimated 90 per cent of the use of antimicrobics is unnecessary.”64
From the 1950s through the 1970s, however, clinicians’ attention was drawn less to the potential for the selection of resistant pneumococcal strains than for unwarranted adverse effects from such drugs. Indeed, the pneumococcus, in particular, had been considered “solidly ensconced as free of resistance, especially to penicillin G [which had superceded sulfadiazine as the drug of choice for lobar pneumonia by the late 1940s].”65 The first requests for “limiting the injudicious use of antimicrobial agents” as a means of containing pneumococcal antimicrobial resistance would appear by the early 1980s66; with pneumococcal penicillin resistance remaining at low levels throughout the decade (3.6% by 1987); however, concerns regarding the potential linkage between unfettered antibiotic overuse and the development of increasing pneumococcal antibiotic resistance remained muted.67
THE POTENTIAL REEMERGENCE OF PNEUMONIA AS A PUBLIC HEALTH CONCERN
By the early 1990s, however, the wider issue of antimicrobial resistance—among pathogens ranging from Mycobacterium tuberculosis to agents of nosocomial infection—would become a cause celebre. Pneumococcal pneumonia would serve to epitomize and even galvanize such broader clinical concerns.68 Amidst dire general warnings of an impending “crisis,” and even a “postanti-microbial era,”69 the early 1990s indeed witnessed a particular (if gradual) increase in pneumococcal resistance to penicillin and representatives of other antimicrobial classes. In this setting, increasing pneumococcal antibiotic resistance, perceived to have derived in large part from antibiotic overuse, would be recast not only as a stain on rational therapeutics but as a potential public health concern, mandating increased surveillance and reporting of resistance on the one hand and judicious avoidance of over-prescribing for upper respiratory tract infections on the other.70 As had happened 6 decades earlier, “effective partnerships involving clinicians, public health officials, and patients” were called for, along with institutionally based “antibiotic control programs” themselves.71 While the envisioned partnerships would represent almost the converse of the earlier pneumonia control programs, with their glorification of antimicrobial agents, they would, like their predecessors, require not only greater physician education and oversight but also pneumonia’s transformation into a public health issue.72
The challenges faced by such a potential inculcation of rational therapeutics, however, remain apparent, and the fate of the pneumococcus remains emblematic of the consequences of antibiotic-prescribing habits broadly. In a study analyzing data of outpatient prescribing for colds, upper respiratory tract infections, and bronchitis for the year 1992, more than half of patients diagnosed with colds or upper respiratory tract infections were prescribed antibiotics73; when the same group analyzed national data from 1998, 55% of all antibiotic prescriptions rendered were still inappropriate.74 By the same year, pneumococcal penicillin resistance had climbed to 24% among “invasive” disease isolates, with 14% of such isolates found to be multidrug resistant.75
Moreover, in the post–World War II era, resistance to thinking of pneumonia as a community concern has been paralleled by the apparently inadequate application of pneumococcal vaccination. In the nearly 60 years since its introduction in the mid-1940s, the pneumococcal polysaccharide vaccine has repeatedly failed to achieve the widespread application envisioned by its supporters.76 The reasons for such failure have changed over time—in the 1940s, the fact that the vaccine was introduced during the advent of curative antibiotics; in the 1970s and 1980s, the difficulties in proving the mortality benefits of the reconfigured vaccine through randomized controlled trials among “high-risk” groups.77 Another possible factor, however, was the postwar view of pneumonia as a disease involving infected individuals to be treated, rather than a preventable disease and hence a public health concern.
By the 1990s, the perceived emerging failure of antipneumococcal therapy in the wake of increasing pneumococcal resistance would lead to increasing rates of pneumococcal vaccination. Indeed, by the end of the decade, Robert Breiman, of the Centers for Disease Control and Prevention, could optimistically cite such an influence as fomenting “a new romance” with preventive vaccination among clinicians whose “love affair with therapeutics” had begun to wilt.78 Still, even though the pneumococcal polysaccharide vaccine has been considered relatively efficacious (and cost-effective) in the prevention of pneumococcal bacteremia by most clinicians polled and by voices of considerable authority among the medical profession,79 the “new romance” has itself yet to fully flower. By 2001, national vaccination rates for those aged 65 years and older remained at approximately 60%, far below the national objective to have more than 90% of this age group immunized by 2010.80
Since 1979, vaccine supporters have lamented the “information gap” among both clinicians and their patients that precludes more widespread application of the vaccine.81 Remedies, both physician focused and patient focused, have been proposed, and attempts to have the vaccine administered in nonoffice settings—for example, among high-risk patients being discharged from hospitals—have been implemented in some locations. To date, however, only partial gains have been reported.82
Instead, given the persisting “ownership” of pneumonia and upper respiratory diseases by private practitioners today, a coordinated effort to educate private practitioners and patients regarding such vaccination will probably be necessary for continued gains in pneumococcal vaccination rates in this century (assuming, of course, the absence of major advances in vaccine development or other unforeseen developments that would render the benefits of application obvious enough to transform practice patterns in their own right). Such an effort will be needed also to curtail inappropriate antibiotic usage. The contingent nature of pneumonia’s changing status as a public health concern throughout the 20th century demonstrates the potential fluidity of the boundary between private practice and public health and the legitimacy of pneumonia’s re-transformation into such a public health concern. At the same time, it demonstrates the degree to which a partnership among private practitioners, public health advocates, and the lay public will be necessary to ensure the success of such a transformation.
Acknowledgments
The research for this article was supported by the John D. Stoeckle Center for Primary Care Innovation at Massachusetts General Hospital, the Department of Social Medicine at Harvard Medical School, the National Library of Medicine (grant 1 G13 LM 07271-01), and Marshall A. Wolf and the Brigham and Women’s Hospital Internal Medicine Residency Program.
Peer Reviewed
References
- 1.See Pneumonia: Mortality and Measures for Prevention (Washington, DC: US Treasury Department and US Public Health Service, 1938); “Parran Urges Funds for War on Pneumonia,” Washington Post, November 13, 1937; “Progress of Programs for Pneumonia Control,” Bulletin of Lederle Laboratories 6 (1938): 118–119. [Google Scholar]
- 2.For earlier assessments of pneumonia’s brief transformation into a national public health concern, see Harry F. Dowling, “Frustration and Foundation: Management of Pneumonia Before Antibiotics,” Journal of the American Medical Association 220 (1972): 1341–1345; Harry F. Dowling, “The Rise and Fall of Pneumonia-Control Programs,” Journal of Infectious Diseases 127 (1973): 201–206.4553966 [Google Scholar]
- 3.Osler William, The Principles and Practice of Medicine (New York: D. Appleton and Company, 1892), 529.
- 4.Klemperer G. and F. Klemperer, “Versuche uber Immunisiring und Heilung bei der Pneumokokkeninfection,” Berlin Klinische Wochenschrift 28 (1891): 833–835; as discussed in Edwin A. Locke, “The Serological Treatment of Lobar Pneumonia,” Boston Medical and Surgical Journal 190 (1924): 196–203. [Google Scholar]
- 5.Dochez A. R. and L. J. Gillespie, “A Biologic Classification of Pneumococci by Means of Immunity Reactions,” Journal of the American Medical Association 61 (1913): 727–730. Cole had been influenced in this regard through visiting Fred Neufeld’s laboratory in Berlin, where Neufeld had already begun such subclassification. See Rufus Cole to F. Neufeld, April 22, 1910; F. Neufeld to Rufus Cole, April 3, 1912; both in the Rufus Cole Papers, American Philosophical Society, Philadelphia (hereafter called RCP). Regarding parallel efforts by F. Spencer Lister in South Africa at the time, see Robert Austrian, “Of Gold and Pneumococci: A History of Pneumococcal Vaccines in South Africa,” Transactions of the American Clinical and Climatological Association 89 (1977): 141–161. Regarding the prevalence of pneumococci as agents of lobar pneumonia, see Oswald T. Avery, H. T. Chickering, Rufus Cole, and A. R. Dochez, Acute Lobar Pneumonia: Prevention and Serum Treatment (New York: Rockefeller Institute for Medical Research, 1917), 7. [Google Scholar]
- 6.Avery et al., Acute Lobar Pneumonia, 79.
- 7.Cecil Russell L. and W D. Sutliff, “The Treatment of Lobar Pneumonia With Concentrated Antipneumococcus Serum,” Journal of the American Medical Association 91 (1928): 2035–2042; William H. Park, Jesse G. M. Bullowa, and Milton B. Rosenblüth, “The Treatment of Lobar Pneumonia With Refined Specific Antibacterial Serum,” Journal of the American Medical Association 91 (1928): 1503–1508; Maxwell Finland, “The Serum Treatment of Lobar Pneumonia,” New England Journal of Medicine 202 (1930): 1244–1247. Regarding Metropolitan Life’s involvement, see An Epoch in Life Insurance: A Third of a Century of Achievement. Thirty-Three Years of Administration of the Metropolitan Life Insurance Company (New York: Metropolitan Life Insurance Company, 1924), 226–227. See also Milton J. Rosnenau to Lee K. Frankel, June 20, 1919; Lee K. Frankel to Milton J. Rosenau, June 24, 1919; both in Lee Frankel Papers, Box 13, American Jewish Historical Society. [Google Scholar]
- 8.Cole Rufus and A. R. Dochez, “Report of Studies on Pneumonia,” Transactions of the Association of American Physicians 28 (1913): 606–616. [Google Scholar]
- 9.See, for example, Brooks Harlow, “The Treatment of Pneumonia,” Medical Clinics of North America 5 (1922): 993–1006; H. T. Nippert, “Treatment of Pneumonia,” Minnesota Medicine 6 (1923): 534–538; L. A. Nippert, “Prognosis and General Management of the Pneumonias,” Journal-Lancet 41 (1921): 66–71. [Google Scholar]
- 10.Heffron Roderick, “Massachusetts Pneumonia Program,” New England Journal of Medicine 206 (1932): 328–329. [Google Scholar]
- 11.For “fascinating administrative experiment,” see George H. Bigelow [commissioner of the Massachusetts Department of Health], “Progress Report on Lobar Pneumonia Service Study,” submitted with George H. Bigelow to Barbara Quin, October 24, 1931, Folder 1728, Box 184, RG 18.1, Rockefeller Archive Center, Sleepy Hollow, NY (hereafter called RAC). For an insightful, yet less sanguine assessment of the Massachusetts Pneumonia Study and Service than that presented here, see Harry M. Marks, The Progress of Experiment: Science and Therapeutic Reform in the United States, 1900–1990 (New York: Cambridge University Press, 1997), 60–65.
- 12.Heffron Roderick and Gaylord W. Anderson, “Two Years’ Study of Lobar Pneumonia in Massachusetts,” Journal of the American Medical Association 101 (1933): 1286–1289. [Google Scholar]
- 13.Bigelow George, “The Serum Treatment of Pneumonia,” New England Journal of Medicine 205 (1931): 242–246. [Google Scholar]
- 14.Heffron Roderick, “A Study of Lobar Pneumonia in Massachusetts: Preliminary Report,” New England Journal of Medicine 207 (1932): 153–159. [Google Scholar]
- 15.Heffron Roderick, “Final Report of Massachusetts Pneumonia Study and Service,” Commonhealth 24 (1937): 6–68. See also “The Massachusetts Pneumonia Program: A Report to the Commonwealth Fund of Eighteen Months’ Progress,” mailed “under separate cover” from George H. Bigelow to Barbara Quin, August 22, 1932, and received August 24, 1932, Folder 1729, Box 184, RG 18.1, RAC. [Google Scholar]
- 16.Lord Frederick, in Heffron, “A Study of Lobar Pneumonia in Massachusetts,” 157.
- 17.In “The Massachusetts Pneumonia Program: A Report to the Commonwealth Fund of Approximately Three Year’s [sic] Work,” accompanying Henry D. Chadwick to Barbara Quin, October 13, 1933, Folder 1731, Box 184, RG 18.1, RAC.
- 18.See George H. Bigelow to Barbara Quin, August 22, 1932, Folder 1729, Box 184, RG 18.1, RAC.
- 19.Heffron and Anderson, “Two Years’ Study of Lobar Pneumonia in Massachusetts,” 1286.
- 20.Heffron, “A Study of Lobar Pneumonia in Massachusetts,” 156.
- 21.Heffron, “Final Report of Massachusetts Pneumonia Study and Service,” 51.
- 22.Ibid, 52.
- 23.“Plan of Pneumonia Study for 1934 and 1935,” accompanying Henry D. Chadwick to Barbara Quin, October 13, 1933, Folder 1731, Box 184, RG 18.1, RAC. For the history of the treatment of poliomyelitis with antiserum, see Naomi Rogers, Dirt and Disease: Polio Before FDR (New Brunswick, NJ: Rutgers University Press, 1992), 96–105.
- 24.Heffron, “Final Report of Massachusetts Pneumonia Study and Service,” 39.
- 25.Ibid, 40.
- 26.Heffron Roderick, “The Campaign Against Pneumonia,” New England Journal of Medicine 214 (1936): 222–223. [Google Scholar]
- 27.See George H. Ramsey to Barbara S. Quinn [sic], September 10, 1935, as well as accompanying “Proposal for a Pneumonia Control Program in New York State,” Folder 2374, Box 249, RG 18.1, RAC.
- 28.Marks, Progress of Experiment, 65–66; Clarence Scamman to Barbara Quin, March 14, 1936; Clarence Scamman, “Report of Attendance at New York State Pneumonia Committee Meeting at Saratoga Springs,” June 23, 1936; both in Folder 2375, Box 249, RG 18.1, RAC; George Ramsey to Barbara Quin, September 24, 1936; George H. Ramsey, “Report on Pneumonia Control Program of the New York State Department of Health,” August 15, 1936; Barry C. Smith to George Ramsey, September 25, 1936; Barbara S. Quin to Edward S. Godfrey, September 21, 1936; all in Folder 2376, Box 249, RG 18.1, RAC.
- 29.Thomas Parran to Drs. Paul Brooks, Edward Godfrey, Augustus Wadsworth, and George Ramsey, May 7, 1935, Box 16, FF 147, Thomas Parran Papers, Archives Service Center, University of Pittsburgh (hereafter called TPP).
- 30.Burrow James G., A.M.A.: Voice of American Medicine (Baltimore, MD: Johns Hopkins University Press, 1963), 191–204; Daniel S. Hirshfield, The Lost Reform: The Campaign for Compulsory Health Insurance in the United States From 1932 to 1943 (Cambridge, MA: Harvard University Press, 1970); Paul Starr, The Social Transformation of American Medicine: The Rise of a Sovereign Profession and the Making of a Vast Industry (New York: Basic Books, 1982), 260–261, 270–279; Jonathan Engel, Doctors and Reformers: Discussion and Debate Over Health Policy, 1925–1950 (Columbia, SC: University of South Carolina Press, 2002), 60–65.
- 31.Parran Thomas, “Expanding Frontiers of Health [broadcast, New York Medical Society, WABC, New York City, April 29, 1936],” Box 35, FF 408, TPP.
- 32.Parran Thomas, “Address [Missouri Public Health Association, May 14, 1938],” Box 38, FF 487, TPP. Pennsylvania’s state pneumonia control program, among the largest in the nation, had originated in 1937.
- 33.Parran Thomas, “Public Health Today [address given before International Medical Assembly of the Inter-State PostGraduate Association, St. Paul, October 14, 1936],” Box 35, FF 412, TPP.
- 34.Ibid. Parran had actually continued this particular speech by noting that “pneumonia control furnishes a notable example of the need for cooperative effort.”
- 35.See, for example, Heathman Lucy S., O. McDaniel, and A. J. Chesley, “Pneumonia in Minnesota: What Can Be Done About It?” Minnesota Medicine 20 (1937): 2–3; 66th Annual Report of the Commissioner of the Michigan Department of Health for the Fiscal Year Ending June 30, 1938 (Lansing, MI: Franklin Dekleine Company, 1940), 75; Roy L. Cleere, in Claude D. Head, “Serum Therapy in Pneumococci Pneumonia and Reduction in Pneumonia Mortality,” Rocky Mountain Medical Journal 36 (1939): 22–23; Illinois Department of Public Health, 22nd Annual Report of the Department of Health, July 1, 1938–June 30, 1939, 70; Annual Report of State Department of Health, Commonwealth of Virginia for the Year Ending June 30, 1940 (Richmond, VA: Division of Purchase and Printing), 27–28; Harrison F. Flippin, “Modern Control of Pneumonia,” Journal of the Missouri State Medical Association 38 (1941): 398–400. [Google Scholar]
- 36.Dowling, “Rise and Fall of Pneumonia-Control Programs,” 203; Annual Report of the Surgeon General of the Public Health Service of the United States for the Fiscal Year 1937 (Washington, DC: US Public Health Service, 1937), 17; Annual Report of the Surgeon General of the Public Health Service of the United States for the Fiscal Year 1940 (Washington, DC: US Public Health Service, 1940), 17.
- 37.Illinois Department of Public Health, 22nd Annual Report of the Department of Health, 7; See also Howard A. Lindberg, “The Illinois Pneumonia Control Program,” Illinois Medical Journal 76 (1939): 85–90. [Google Scholar]
- 38.Dowling, “Rise and Fall of Pneumonia-Control Programs,” 203; Rufus Cole to Wheelan Sutliff, December 9, 1937; Rufus Cole to Roderick Heffron, January 30, 1937; both in RCP.
- 39.Roderick Heffron to Maxwell Finland, December 22, 1937, Maxwell Finland Papers, Countway Medical Library, Harvard Medical School, Boston.
- 40.See, for example, New Methods for Pneumonia Control: Reproduction of Charts Shown in the Scientific Exhibit at the Annual Meeting of the American Medical Association, San Francisco, June 13–17, 1938 (New York: Metropolitan Life Insurance Company, 1938); Pneumonia: Some Important Facts Regarding Treatment and Control (Washington, DC: US Public Health Service, 1940).
- 41.“The Pneumonia Film, ‘A New Day,’ ” Journal of the American Medical Association 110 (1938): 514; “Teaching Health With Metropolitan Films,” Metropolitan Underwriter 13 (October 1943): 14–15. [Google Scholar]
- 42.A New Day in Health Protection, 2–5, Box 160605, Metropolitan Life Insurance Company Archives; Press Book: A New Day, 4–9, Box 160605, Metropolitan Life Insurance Company Archives, New York. By 1939, the film had been updated to include a potential role for sulfapyridine alongside serotherapy in the treatment of pneumonia. In American Council on Education, Selected Educational Motion Pictures, a Descriptive Encyclopedia (Washington, DC: American Council on Education, 1942), 207–208.
- 43.Georgia, Idaho, and Kansas, for example, provided only typing services. See State of Georgia Department of Public Health, Annual Report, 1938, 64; Idaho Department of Public Welfare, Division of Public Health, Biennial Report, 1937–1938, 15; Biennial Report of the Department of Public Welfare of the State of Idaho, 1939–1940, 22; State Board of Health of the State of Kansas, 20th Biennial Report, July 1, 1938, to June 30, 1940, 140; Kansas State Board of Health, Twenty-First Biennial Report, July 1, 1940, to June 30, 1942, 75. At the other end of the spectrum of “control,” in Massachusetts, by 1937, “physicians who have reported deaths from pneumonia and whose names were not found on the list of those who had requested serum, were circularized and given an opportunity to ask that a number of our staff call upon them to explain the pneumonia program.” In Commonwealth of Massachusetts, [23rd] Annual Report of the Department of Public Health for the Year Ended November 30, 1937, 8.
- 44.Compare, for instance, the proserum leanings of the Massachusetts program with the pro-sulfa leanings of the Tennessee program. In Commonwealth of Massachusetts, 26th Annual Report of the Department of Public Health of Massachusetts, 51; Tennessee Department of Public Health and the Tennessee State Medical Association, Pneumonia: Its Etiology, Diagnosis, and Treatment (1940), 15–16, 30–31.
- 45.As a representative sample, see Bullowa Jesse G. M., Norman Plummer, and Maxwell Finland, “Sulfapyridine in the Treatment of Pneumonia,” Journal of the American Medical Association 112 (1939): 570; Maxwell Finland, “The Treatment of Pneumonia,” Canadian Medical Association Journal 41 (1939): 554–560; Norman Plummer, “The Treatment of Pneumonia,” Journal of the Indiana State Medical Society 35 (1942): 608–613. [Google Scholar]
- 46.Plummer Norman, James Liebmann, Saul Solomon, W. H. Kammerer, Mennasch Kalkstein, and Herbert K. Ensworth, “Chemotherapy Versus Combined Chemotherapy and Serum in the Treatment of Pneumonia: A Study of 607 Alternated Cases,” Journal of the American Medical Association 116 (1941): 2366–2371. [Google Scholar]
- 47.Tillett William S., Margaret J. Cambier, and James E. McCormick, “The Treatment of Lobar Pneumonia and Pneumococcal Empyema With Penicillin,” Bulletin of the New York Academy of Medicine 20 (1944): 142–178; Norman Plummer, “The Treatment of Lobar Pneumonia,” Bulletin of the New York Academy of Medicine 20 (1944): 73–86. [PMC free article] [PubMed] [Google Scholar]
- 48.Biennial Report of the Department of Public Health, State of Tennessee, for the Fiscal Years 1943–1945, 58.
- 49.From 1941 to 1945, federal support of the state pneumonia control programs declined from $523 225 to $40 802. No funding was provided beyond 1945. See Annual Report of the Surgeon General of the Public Health Service of the United States for the Fiscal Year 1941 (Washington, DC: US Public Health Service, 1941), 14; Annual Report of the Surgeon General of the Public Health Service of the United States for the Fiscal Year 1945 (Washington, DC: US Public Health Service, 1945), 153.
- 50.William Watt Graham Maclachlan, in Bernard J. McCloskey, “Five Years of Pneumonia Control in Cambria County, Pennsylvania,” Pennsylvania Medical Journal 46 (1943): 478–483. [Google Scholar]
- 51.Fee Elizabeth, “The Origins and Development of Public Health in the United States,” in Roger Detels, Walter W. Holland, James McEwan, and Gilbert S. Omenn, eds., Oxford Textbook of Public Health, Third Edition, vol. I: The Scope of Public Health (New York: Oxford University Press, 1997), 46–47.
- 52.Bortz Edward L., “Therapeutics of Pneumonia on a Statewide Basis,” Journal of the American Medical Association 121 (1943): 107–113. [Google Scholar]
- 53.Parran Thomas, “Health Is on the March [Office of War Information radio transcription, January 28, 1942],” Box 45, FF 645, TPP; Parran, “The Expanding Field of Public Health and Preventive Medicine [Annual Congress on Medical Education and Licensure, American Medical Association, February 14, 1944],” Box 45, FF 648, TPP; Parran, “State of the Nation’s Health [State and Territorial Health Officers Conference, March 21, 1944],” Box 45, FF 652, TPP; Parran, “The Health of the Nation [hearings before Subcommittee on Appropriation, March 28, 1944],” Box 45, FF 653, TPP.
- 54.Parran Thomas, “New Frontiers in Medicine [commencement exercises, University of Utah, September 10, 1944],” Box 46, FF 681, TPP.
- 55.Parran, “The Expanding Field of Public Health and Preventive Medicine.”
- 56.See Marvin Horace P., Franklin D. Owings, and Edward K. Edelson, “Pneumonia Therapy With Sulfathiazole in Military Practice,” Military Surgeon 91 (1942): 55–58; Maine C. Anderson, “In View of Present Day Treatment, Are Typing and Serums Necessary?” Journal of the Omaha Midwest Clinical Society 5 (1944): 48–49. [Google Scholar]
- 57.See Copley Edward Lee, “Pneumonia in Virginia: A Series of Fifty-Three Cases,” Southern Medicine and Surgery 104 (1942): 142; Charles P. Wofford, “Present-Day Management of Pneumonia,” Journal of the Tennessee State Medical Association 35 (1942): 123–125; “Only Pneumonia,” Science News Letter 48 (1945): 380; “Pneumonia,” Life Magazine, February 13, 1950, p. 13. [Google Scholar]
- 58.Cecil Russell L., in Edward L. Bortz, “Pneumonia in Pennsylvania,” Transactions of the American Clinical and Climatological Association 56 (1940): 103–120. [PMC free article] [PubMed] [Google Scholar]
- 59.See, for example, David D. Rutstein to W. G. Campbell, February 7, 1939, Sulfapyridine New Drug Application, Volume III, Food and Drug Administration Records, Rockville, Md.; Roderick Heffron to Barry Smith, April 7, 1942, Folder 521, Box 36, RG 18.1, RAC.
- 60.McIlwane William B., “The Use of Sulfapyridine and Sulfathiazole in General Practice,” Virginia Medical Monthly 68 (1941): 410–411. [Google Scholar]
- 61.Stainsby Wendell J., “Pneumonia in General Practice,” Pennsylvania Medical Journal 47 (1943): 562–563; O. H. Robertson, “Newer Knowledge Concerning the Inception of Pneumonia and Its Bearing on Prevention,” Annals of Internal Medicine 18 (1943): 1–14. [Google Scholar]
- 62.Drummond W. F., in C. P. Herrington, “Chemotherapy in Pneumonia,” New Orleans Medical and Surgical Journal 93 (1941): 348–353; Morton Hamburger, Jr., L. H. Schmidt, Clara L. Sesler, J. M. Ruegsegger, and Eda S. Grupen, “The Occurrence of Sulfonamide-Resistant Pneumococci in Clinical Practice,” Journal of Infectious Diseases 73 (1943): 12–30; Richard A. Kern, “Abuse of Sulfonamides in the Treatment of Acute Catarrhal Fever,” United States Naval Academy Bulletin 44 (1945): 686–694. [Google Scholar]
- 63.Nolen William A. and Donald E. Dille, “Use and Abuse of Antibiotics in a Small Community,” New England Journal of Medicine 257 (1957): 33–34. Upper respiratory tract infections were excluded from the list of disease entities considered appropriately treated with antibiotics, and the 3 anecdotal examples used for demonstration by the authors all entailed the use of antibiotics for upper respiratory tract infections. [DOI] [PubMed] [Google Scholar]
- 64.See Whorten James, “‘Antibiotic Abandon: The Resurgence of Therapeutic Rationalism,” in John Parascandola, ed., The History of Antibiotics: A Symposium (Madison, Wisc: American Institute of the History of Pharmacy, 1980), 129–130; Maxwell Finland, “Clinical Uses of the Presently Available Antibiotics,” Antibiotics Annual (1953–1954): 10–26; Hobart A. Reimann, “The Misuse of Antimicrobics,” Medical Clinics of North America 45 (1961): 849–856. [DOI] [PubMed]
- 65.Finland Maxwell, “Increased Resistance in the Pneumococcus,” New England Journal of Medicine 284 (1971): 212–214. [DOI] [PubMed] [Google Scholar]
- 66.Ward Joel, “Antibiotic-Resistant Streptococcus pneumoniae: Clinical and Epidemiologic Aspects,” Reviews of Infectious Diseases 3 (1981): 254–266. [DOI] [PubMed] [Google Scholar]
- 67.Spika John S., Richard R. Facklam, Brian D. Plikaytis, and Margaret J. Oxtoby, “Antimicrobial Resistance of Streptococcus pneumoniae in the United States, 1979–1987,” Journal of Infectious Diseases 163 (1991): 1273–1278. [DOI] [PubMed] [Google Scholar]
- 68.An ISI Essential Science Indicators search, conducted in 2003, of the “most-cited papers on antibiotic resistance in the past decade,” found 3 of the top 4 papers cited to concern pneumococcal resistance. In “Antibiotic Resistance—Top Papers,” available at http://www.esi-topics.com/anti-res/papers/a1.html, accessed February 2003.
- 69.Neu Harold C., “The Crisis in Antibiotic Resistance,” Science 257 (1992): 1064–1073; Mitchell L. Cohen, “Epidemiology of Drug Resistance: Implications for a Post-Antimicrobial Era,” Science 257 (1992): 1050–1055. See also Calvin M. Kunin, “Resistance to Antimicrobial Drugs—A Worldwide Calamity,” Annals of Internal Medicine 118 (1993): 557–561. [DOI] [PubMed] [Google Scholar]
- 70.Breiman Robert F., Jay C. Butler, Fred C. Tenover, John A. Elliott, and Richard R. Facklam, “Emergence of Drug-Resistant Pneumococcal Infections in the United States,” Journal of the American Medical Association 271 (1994): 1831–1835; Daniel B. Jernigan, Martin S. Cetron, and Robert F. Breiman, “Minimizing the Impact of Drug-Resistant Streptococcus pneumoniae (DRSP): A Strategy From the DRSP Working Group,” Journal of the American Medical Association 275 (1996): 206–209.8196139 [Google Scholar]
- 71.Schwartz Benjamin, David M. Bell, and James M. Hughes, “Preventing the Emergence of Antimicrobial Resistance: A Call for Action by Clinicians, Public Health Officials, and Patients,” Journal of the American Medical Association 278 (1997): 944–945; Neu, “The Crisis in Antibiotic Resistance,” 1072. [DOI] [PubMed] [Google Scholar]
- 72.Simberkoff Michael S., “Drug-Resistant Pneumococcal Infections in the United States: A Problem for Clinicians, Laboratories, and Public Health,” Journal of the American Medical Association 271 (1994): 1875–1876; Joseph F. Plouffe, Robert F. Breiman, and Richard R. Facklam, “Bacteremia With Streptococcus pneumoniae: Implications for Therapy and Prevention,” Journal of the American Medical Association 275 (1996): 194–198.8196147 [Google Scholar]
- 73.Gonzales Ralph, John F. Steiner, and Merle A. Sande, “Antibiotic Prescribing for Adults With Colds, Upper Respiratory Tract Infections, and Bronchitis by Ambulatory Care Physicians,” Journal of the American Medical Association 278 (1997): 901–904. [PubMed] [Google Scholar]
- 74.Gonzales Ralph, Daniel C. Malone, Judith H. Maselli, and Merle A. Sande, “Excessive Antibiotic Use for Acute Respiratory Infections in the United States,” Clinical Infectious Diseases 33 (2001): 757–762. A further study of such national data from 1997 to 1999 would find that 46% of patients with the common cold or a non-specific upper respiratory tract infection would still be given antibiotics. More than half of them were prescribed broad-spectrum agents. Michael A. Steinman, C. Seth Landefeld, and Ralph Gonzales, “Predictors of Broad-Spectrum Antibiotic Prescribing for Acute Respiratory Tract Infections in Adult Primary Care,” Journal of the American Medical Association 289 (2003): 719–725.11512079 [Google Scholar]
- 75.Whitney Cynthia G., Monica M. Farley, James Hadler, et al., “Increasing Prevalence of Multidrug-Resistant Streptococcus pneumoniae in the United States,” New England Journal of Medicine 343 (2000): 1917–1918. “Invasive” disease “was defined by the isolation of S. pneumoniae from a normally sterile body site.” [DOI] [PubMed] [Google Scholar]
- 76.See, for example, Austrian Robert, “A Reassessment of Pneumococcal Vaccine,” New England Journal of Medicine 310 (1984): 651–653; Jay C. Butler, Eugene D. Shapiro, and George M. Carlone, “Pneumococcal Vaccines: History, Current Status, and Future Directions,” American Journal of Medicine 107 (1999): 69S–76S. [DOI] [PubMed] [Google Scholar]
- 77.Austrian Robert, “Pneumococcal Infection and Pneumococcal Vaccine,” New England Journal of Medicine 297 (1977): 938–939; Robert Austrian, “Some Observations on the Pneumococcus and on the Current Status of Pneumococcal Disease and Its Prevention,” Reviews of Infectious Disease 3 (1981): S1–S17; Michael S. Simberkoff, Anne P. Cross, Mohamed Al-Ibrahim, et al., “Efficacy of Pneumococcal Vaccine in High-Risk Patients: Results of a Veterans Administration Cooperative Study,” New England Journal of Medicine 315 (1986): 1318–1327. [DOI] [PubMed] [Google Scholar]
- 78.Breiman Robert F., “Editorial Response: Prevention of Pneumococcal Disease—A New Romance Begins,” Clinical Infectious Diseases 26 (1998): 1124. [DOI] [PubMed] [Google Scholar]
- 79.Fedson David S., “Influenza and Pneumococcal Immunization Strategies for Physicians,” Chest 91 (1987): 436–443; Tammy A. Mieczkowski and Stephen A. Wilson, “Adult Pneumococcal Vaccination: A Review of Physician and Patient Barriers,” Vaccine 20 (2002): 1383–1392.3816320 [Google Scholar]
- 80.“Trends in Morbidity and Mortality: Pneumonia, Influenza, and Acute Respiratory Conditions,” American Lung Association [Best Practices and Program Services, Epidemiology and Statistics Unit, September 2002], available at www.lungusa.org, accessed September 2002.
- 81.Regarding clinicians, see Pantell Robert H. and Thomas J. Stewart, “The Pneumococcal Vaccine: Immunization at a Crossroad,” Journal of the American Medical Association 241 (1979): 2272–2274; W. R. Barclay, “Vaccination to Prevent Pneumonia,” Journal of the American Medical Association 241 (1979): 2299. Regarding the public, see Jane E. Sisk and Richard K. Riegelman, “Cost Effectiveness of Vaccination Against Pneumococcal Pneumonia: An Update,” Annals of Internal Medicine 104 (1986): 79–86.439296 [Google Scholar]
- 82.For a recent review of such proposals and attempts, see Mieczkowski and Wilson, “Adult Pneumococcal Vaccination,” 1388–1389.


