Abstract
Objectives. We examined age, period, and cohort (APC) effects on temporal trends in stillbirths among Black and White women in the United States.
Methods. We conducted a cohort study of Black and White women who delivered a singleton live-born or stillborn infant during 1981 through 2000. We analyzed stillbirth rates at 20 or more weeks of gestation within 7 age groups, 4 periods, and 10 “central” birth cohorts after adjusting for confounders.
Results. In both racial groups, women younger than 20 years or 35 years or older were at increased risk of stillbirth; risks decreased over successive periods in all age groups. Birth cohort had no impact on stillbirth trends among Blacks and only a small, nonsignificant effect among Whites. Analyses of various APC combinations showed that Blacks were at a 1.2- to 2.9-fold increased risk for stillbirth relative to Whites. Attributable fractions for stillbirth because of age, period, and cohort effects were 16.5%, 24.9%, and 0.1%, respectively, among Black women and 14.5%, 36.2%, and 2.1%, respectively, among White women.
Conclusions. Strong effects of age and period were observed in stillbirth trends, but these factors do not explain the persistent stillbirth disparity between Black and White women.
During the past few decades, rates of stillbirth at 20 or more weeks of gestation have declined substantially in Western countries. In the United States, for instance, the stillbirth rate declined by 52% between 1970 (14.0 per 1000 total births) and 1998 (6.7 per 1,000 total births), with the rate of decline more evident during earlier than more recent decades.1,2 However, disparities in rates of stillbirth remain, with Black women in the United States at an approximately 2-fold greater risk of delivering a stillborn fetus than White women.2
In assessments of stillbirth trends, the goal of an age, period, and cohort (APC) analysis is to disentangle the complex associations of maternal age, historical trends (period effects), and life course factors (maternal birth cohort effects). Several studies have shown that risks of stillbirth increase at the extremes of maternal age3,4 and decrease at successively more recent time periods.2 However, these studies have inevitably failed to shed light on how differences in stillbirth rates vary by maternal age across generations.
An APC analysis might help provide an understanding of how age, period, and birth cohort have affected temporal trends in stillbirth. For instance, trends in stillbirths that are strongly associated with maternal age would support the hypothesis of a biological effect related either to aging or to selective fertility.5 A strong period effect would suggest general improvements in maternal health, access to pre-natal care, antepartum surveillance, or other aspects of obstetric management, including increases in rates of routine labor induction or cesarean section. A period effect might also raise the question of changes in the registration of stillbirths, particularly at very short lengths of gestation (20–25 weeks). On the other hand, the presence of a cohort effect, although rarely examined, might lead to an understanding of the effects of persistent or cumulative (maternal) exposure to risk factors during the fetal period or childhood on stillbirth trends.
METHODS
Cohort Composition
We used data available for the period 1981 through 2000 from the US live birth and fetal death registration files. These files, assembled by the National Center for Health Statistics, comprise births that occur in the 50 states and the District of Columbia.6 Stillbirth is defined as fetal death at 20 or more completed weeks of gestation. In 95% of births, gestational age is based on most recent menstrual period. In the remainder of births, gestational age is either replaced with a clinical estimate (also contained in the birth records) or imputed.7 Clinical estimates of gestation are based on birth attendants’ estimates, and they typically are calculated via either the Dubowitz8 or Ballard9 technique. The National Center for Health Statistics calculates imputations and replacements before public release of the data.6,7
Data Exclusions
Data were abstracted from singleton deliveries in the United States resulting in a live birth or fetal death between 1981 and 2000. We excluded the following data file categories: maternal age younger than 15 years or 50 years or older (n=218526), because of the low number of pregnancies involving a stillbirth in these extremes of the maternal age distribution; birthweight below 500 g (n=259511); birthweight data missing (n=127586); and gestational age less than 20 completed weeks (n=508577) or missing (n=1768733). Percentages of births with missing data on gestational age declined over time but were generally higher among Black women than among White women within each period. After these exclusions, the final cohort comprised 71037685 singleton live births and stillbirths.
Statistical Analysis
Birth periods were grouped in 5-year intervals (1981–1985, 1986–1990, 1991–1995, 1996–2000), as was maternal age (15–19 years through 45–49 years). A synthetic birth cohort calculated according to mother’s year of birth was derived from data on year (period) of birth and mother’s age (maternal birth cohort category = period – age). A limitation of our analysis was that combinations of 5-year maternal age and 5-year period groupings did not correspond to exact 5-year birth cohorts. In other words, women aged 20 to 24 years who delivered during the 1981 to 1985 period were primarily members of the 1961 through 1965 birth cohort, although some of these women may have been born as early as 1957 and some as late as 1965. To avoid the confusion resulting from this imprecision, we denote maternal birth cohort as central birth year, that is, 1963 in the example just cited (although denoting the central year as 1962 would produce results identical to using 1963) rather than 1961 to 1965.
We used logistic regression models adjusted for number of pregnancies (1, 2, or ≥3), maternal education (<12, 12, 13–15, or ≥16 completed years of school), marital status (married or single), and prenatal care (defined as lack of care or initiation of care after the first trimester) to estimate APC effects on stillbirth trends. We corrected all model-based variance estimates for overdispersion.10 APC effects were modeled as categorical covariates; thus, age contained 6 terms in the regression model, period contained 3, and cohort contained 9. From this model, we derived stillbirth rates and odds ratios, after adjusting for confounders, using 25 to 29 years as the reference category for maternal age, 1996 to 2000 as the reference for period, and 1953 as the reference for central birth cohort.
The outlined model implicitly assumed that stillbirth rates follow a binomial distribution and that rates are multiplicative on the logistic scale. A unique feature of such an analysis is that any 2 of the effects assessed are sufficient to derive the third; the exact linear dependency among the 3 effects is unique to any APC analysis. To overcome this limitation, we constrained the effect of the 1977 central birth cohort (i.e., women born in 1975–1979) to zero in the regression models.11 We tested the validity of this assumption by replicating the models after setting the 1933 central birth cohort (i.e., 1931–1935) to zero. Although the regression estimates were numerically different from those produced by the previous models, the overall qualitative results remained unchanged (data not shown).
We examined whether APC effects helped explain Black–White disparities in stillbirth trends by assessing changes in the estimate of the log-odds ratio for race between 2 nested models, one containing the race term (along with confounders) and the other including the race term and APC factors (along with confounders). If APC factors account in part for racial disparities in stillbirth trends, then we should detect a significant difference in the log-odds ratio for the race term between these 2 models.
Finally, we calculated attributable fractions for stillbirth in relation to maternal age, period, and maternal birth cohort using the relation
 |
(1) |
where pi refers to the proportion of the source population grouped in the ith exposure category and RR is the relative risk of stillbirth.12 The attributable fraction was interpreted as the proportion of stillbirths that could be attributed to the exposure in question (e.g., maternal age). Thus, while odds ratios quantified the strengths and magnitudes of association between particular exposures and stillbirth, attributable fractions were measures of the public health effects of the exposures on outcomes.
RESULTS
Rates of stillbirth at 20 or more weeks of gestation gradually declined between 1981 and 2000 among both Black and White women. Rates decreased by 33% (from 9.8 to 6.6 per 1000 births) among Blacks and by 46% (from 5.9 to 3.2 per 1000 births) among Whites. These patterns were similar when stillbirth trends were restricted to births occurring at 28 or more weeks of gestation.
Trends in stillbirth rates (at 20 or more weeks) according to age, period, and maternal birth cohort are shown in Table 1 ▶. Among Black women, maternal age had the strongest influence on stillbirth trends (deviance χ26 = 71.2, P < .001), followed by period (deviance χ23 = 25.7, P < .001); among White women, however, period had the strongest influence on rates (deviance χ23 = 87.7, P < .001), followed by maternal age (deviance χ26 = 67.8, P < .001). Maternal birth cohort had virtually no influence on stillbirth trends among Blacks and only a small effect of borderline significance (P = .055) among Whites.
TABLE 1—
Stillbirth Rates (per 1000 Births), by Age, Period, and Central Maternal Birth Cohort: United States, 1981 to 2000
| Maternal Age, y | ||||||||
| Period | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | Birth Cohort |
| Black women | ||||||||
| ↗ 31.5 | 1933 | |||||||
| ↗ 22.4 | ↗ 23.2 | 1937 | ||||||
| ↗ 14.6 | ↗ 19.8 | ↗ 36.3 | 1943 | |||||
| ↗ 10.8 | ↗ 12.6 | ↗ 17.6 | ↗ 27.0 | 1947 | ||||
| ↗ 8.8 | ↗ 9.8 | ↗ 12.4 | ↗ 12.9 | 1953 | ||||
| ↗ 8.3 | ↗ 8.6 | ↗ 9.9 | ↗ 9.6 | 1957 | ||||
| ↗ 8.8 | ↗ 8.2 | ↗ 8.2 | ↗ 7.6 | 1963 | ||||
| 1981–1985 | ↗ 8.1 | ↗ 7.3 | ↗ 6.8 | 1967 | ||||
| 1986–1990 | ↗ 7.7 | ↗ 6.9 | 1973 | |||||
| 1991–1995 | ↗ 6.9 | 1977 | ||||||
| 1996–2000 | ||||||||
| White women | ||||||||
| ↗ 25.8 | 1933 | |||||||
| ↗ 14.0 | ↗ 19.1 | 1937 | ||||||
| ↗ 8.3 | ↗ 10.8 | ↗ 14.3 | 1943 | |||||
| ↗ 5.6 | ↗ 6.1 | ↗ 8.8 | ↗ 11.3 | 1947 | ||||
| ↗ 4.8 | ↗ 4.4 | ↗ 5.5 | ↗ 6.5 | 1953 | ||||
| ↗ 5.1 | ↗ 4.0 | ↗ 4.0 | ↗ 4.3 | 1957 | ||||
| ↗ 6.1 | ↗ 4.4 | ↗ 3.7 | ↗ 3.2 | 1963 | ||||
| 1981–1985 | ↗ 5.3 | ↗ 4.1 | ↗ 3.1 | 1967 | ||||
| 1986–1990 | ↗ 4.8 | ↗ 3.5 | 1973 | |||||
| 1991–1995 | ↗ 4.3 | 1977 | ||||||
| 1996–2000 | ||||||||
Note. The arrows on the diagonal, from lower left in the first column to upper right in the last column under “maternal age,” indicate the period during which when the birth occurred, and the horizontal rows represent the progression of the maternal birth cohort.
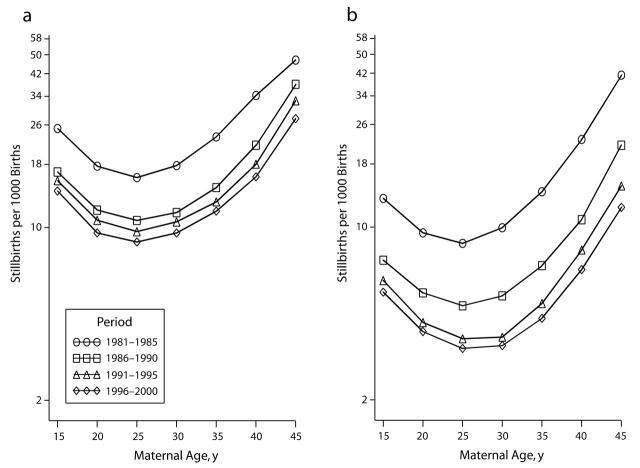
Figure 1 ▶ shows the associations between maternal age and stillbirth within the 4 periods. Extremes of maternal age (less than 20 and 35 years or above) were associated with increased (adjusted) stillbirth rates within each of the 4 periods, the risk becoming steeper at 35 years and above among both Black and White women. Stillbirths consistently declined at increasingly more recent birth periods within strata of maternal age.
FIGURE 1—
Adjusted maternal age-specific trends in rates of stillbirth at 20 or more weeks of gestation (per 1000 births), by period, for (a) Black and (b) White women in the United States, 1981 to 2000.
Note. Rates were adjusted for maternal birth cohort, gravidity, maternal education, marital status, and prenatal care.
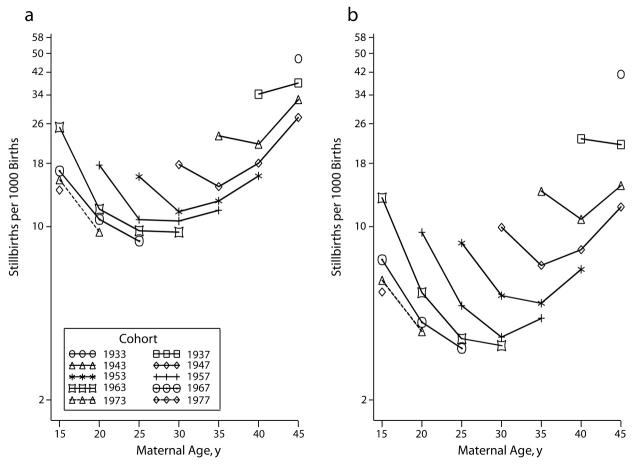
Stillbirth trends according to maternal age within (central) birth cohort strata are shown in Figure 2 ▶. Stillbirth rates among Black and White women born between the central birth cohort years of 1942 and 1957 (i.e., actual years of birth between 1937 and 1961) showed a J-shaped relation with maternal age. Among Black and White women born in the earlier birth cohorts (1937 or earlier), adjusted stillbirth rates declined monotonically with advancing maternal age.
FIGURE 2—
Adjusted maternal age-specific trends in rates of stillbirth at 20 or more weeks of gestation (per 1000 births), by birth cohort for (a) Black and (b) White women in the United States, 1981 to 2000.
Note. Rates were adjusted for period of delivery, gravidity, maternal education, marital status, and prenatal care.
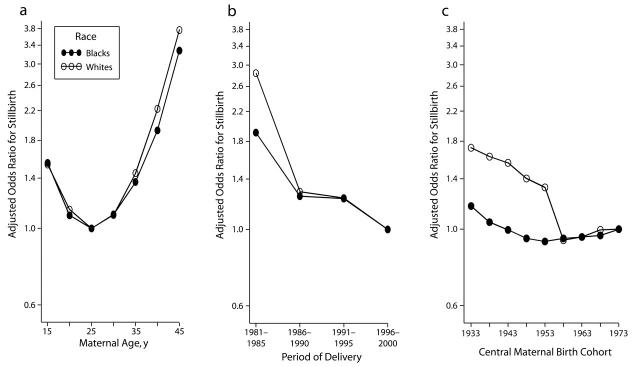
The associations between maternal age, period, and maternal birth cohort and adjusted stillbirth risk are shown in Figure 3 ▶. The adjusted stillbirth odds ratio exhibited a J-shaped pattern for maternal age among both Blacks and Whites. Relative to women delivering in the 1996 to 2000 period, adjusted odds ratios for stillbirth among those delivering in the 1981 to 1985 period were 2.9 (95% confidence interval [CI]=2.7, 3.1) among Whites and 1.9 (95% CI=1.6, 2.2) among Blacks. Thereafter, adjusted odds ratios declined at increasingly more recent periods. White women born in the earlier birth cohorts (i.e., up to 1952–1957, or the 1953 central birth year) were at increased risk of stillbirth relative to those born during 1971 to 1975 (the 1973 central birth year), but adjusted odds ratios were close to 1.0 thereafter. Maternal birth cohort exhibited virtually no association with stillbirth risk among Blacks, and the same was true among Whites in the more recent cohorts. Attributable fractions for stillbirth because of maternal age, period, and maternal birth cohort effects were 16.5%, 24.9%, and 0.1%, respectively, among Blacks and 14.5%, 36.2%, and 2.1%, respectively, among Whites.
FIGURE 3—
Adjusted odds ratios of stillbirths in relation to (a) maternal age, (b) period of delivery, and (c) maternal birth cohort: Black and White women in the United States, 1981 to 2000.
Note. Odds ratios were adjusted for gravidity, maternal education, marital status, and prenatal care. The reference categories were 25 to 29 years for maternal age, 1996 to 2000 for period, and 1953 for central birth cohort.
We assessed the extent to which APC effects helped explain Black–White disparities in stillbirth trends by comparing the log-odds ratio for the race term between 2 (closely nested) logistic regression models. In the first model (containing a race term in addition to the confounders), the odds ratio for stillbirth among Black versus White women was 2.4 (95% CI = 2.1, 2.7); in the second model (containing race, age, period, cohort, and the confounders), the odds ratio was 2.3 (95% CI = 2.1, 2.6). This comparison indicates that APC factors explained very little of the Black–White disparity in stillbirth risks.
DISCUSSION
Over the past 3 decades, stillbirth rates have declined substantially in the United States,2 similar to the declines observed in several other Western societies.4,13–15 These trends have been largely attributed to improvements in general socioeconomic conditions, including higher maternal education levels, better access to and improvements in general prenatal and intrapartum care, declining rates of smoking and substance use during pregnancy, and improvements in medical care.16 The chief findings from our study are the following: (1) an overall 33% to 44% decline in stillbirth rates; (2) higher stillbirth rates at the extremes of maternal age; (3) declining stillbirth rates in successive periods; (4) no significant birth cohort effect; (5) no age, period, or birth cohort effects on prevailing race disparities in stillbirths; and (6) large attributable fractions for maternal age and period of delivery.
Once the general effects of maternal age and birth cohort (and other confounders) were adjusted, we found that period of birth had a strong influence on stillbirth trends. This finding corroborates previous observations of a temporal decline in stillbirth rates in the United States3 as well as in other Western countries.4,13–15 The doubling in labor inductions in the United States in recent years, from 9.5% to 19.4% between 1990 and 1998,17 may have played an important role in the declining stillbirth rate.
We observed that, before adjustment for gravidity, maternal age had the strongest influence on stillbirth trends among both Blacks and Whites, followed by birth cohort; period had virtually no influence.18 The reversal in the relative contributions of maternal birth cohort effects to stillbirth trends before and after adjustment for number of pregnancies may be attributable to at least 3 distinct factors. One is that mothers with previous losses (stillbirths or infant deaths) may have been overrepresented among older mothers and those of higher parity,5 thereby leading to distortions in stillbirth rates in these maternal age–gravida categories. Another factor that may be partly responsible for the confounding effect of gravidity is that women born in the earlier birth cohorts may have had more pregnancies than those born in the later cohorts. Finally, the gravidity effect may be partly because of the association between higher number of pregnancies and low socioeconomic status.
This finding of a stronger birth cohort effect than period effect on stillbirth trends before adjustment for gravidity was also reported in an APC analysis of stillbirths (1955–1979) in Italy19 and in Norway over the span of a century (1866–1975).20 However, the recent period effects in declining stillbirths resulting from the recent trends in labor induction and fetal surveillance were absent among the older cohorts in these studies.16 An APC analysis of perinatal mortality (stillbirths plus neonatal deaths) of Norwegian births covering a shorter and more recent period (1967–1991) than the earlier Norwegian study20 showed virtually no cohort effects,21 although plausible trends in stillbirths may have been attenuated given that stillbirths and neonatal deaths were combined.
Possible Biases and Residual Confounding
Several limitations of our study merit discussion. First, a number of determinants of stillbirth, especially smoking and drug use, have been declining in the United States.22 Examination of these factors was beyond the scope of this study. Second, because we examined stillbirth trends over 2 decades, it is likely that a small proportion of women contributed more than 1 pregnancy during the study, and previous studies indicate an increased risk of stillbirth among women with a prior stillbirth.23 Failure to account for this “clustering” phenomenon in stillbirth risk may have biased the variance estimates from our regression models,24 thus overstating or understating the relative contributions of APC effects on stillbirth trends. Finally, the possibility of an intergenerational influence (immeasurable in our study) of stillbirth risk may have affected our results to some extent. Stillbirths or, more generally, pregnancy losses tend to cluster within families, suggesting a genetic contribution.25–27
Public Health Implications
In addition to strong maternal age and period effects on stillbirth trends, we noted substantial attributable fractions for stillbirths. For instance, attributable fractions associated with a maternal age of 35 years or above were 5.1% and 3.0% among Whites and Blacks, respectively. These attributable fractions translate to 1768 and 301 potentially preventable stillbirths, respectively, among White and Black women in the United States. While these factors cannot be altered, targeting advanced maternal age to decrease stillbirths may prove beneficial.
One of the overarching goals of Healthy People 2010 is to reduce health disparities, including those related to pregnancy outcomes.28,29 Not only are these goals far from being met,29 but disparities associated with some health indicators have actually widened.30 Although overall rates of stillbirth have been declining, the rate among women 35 years or older has actually been increasing, more so in the case of Whites than Blacks. Efforts to better understand the biological mechanisms of the aging process that are associated with stillbirth risk may be beneficial. Finally, although both maternal age and period effects are important in explaining temporal trends in stillbirth rates among Black as well as White women, they do not help explain the persistent Black–White disparity in stillbirths in the United States.
Acknowledgments
Portions of this article were presented at the 15th Annual Meeting of the Society for Pediatric and Perinatal Epidemiologic Research, Atlanta, Ga, June 10–11, 2003.
We thank Drs Darios Getahun, John Smulian, and Anthony Vintzileos, Department of Obstetrics, Gynecology, and Reproductive Sciences, UMDNJ–Robert Wood Johnson Medical School, for their comments and suggestions that helped improve the article. We also thank Susan Fosbre for help during preparation of the article.
Human Participant Protection This study was approved by the UMDNJ–Robert Wood Johnson Medical School institutional review board.
Peer Reviewed
Contributors C.V. Ananth and M.S. Kramer originated the idea for the study. C.V. Ananth assembled the data, performed all statistical analysis, and wrote the article. S. Liu, W.L. Kinzler, and M.S. Kramer reviewed the analysis, helped with interpretation of the findings, and reviewed the article.
References
- 1.Martin JA, Hoyert DL. The national fetal death file. Semin Perinatol. 2002;26:3–11. [DOI] [PubMed] [Google Scholar]
- 2.Hsieh HL, Lee KS, Khoshnood B, Herschel M. Fetal death rate in the United States, 1979–1990: trend and racial disparity. Obstet Gynecol. 1997;89:33–39. [DOI] [PubMed] [Google Scholar]
- 3.Raymond EG, Cnattingius S, Kiely JL. Effects of maternal age, parity, and smoking on the risk of stillbirth. Br J Obstet Gynaecol. 1994;101:301–306. [DOI] [PubMed] [Google Scholar]
- 4.Fretts RC, Boyd ME, Usher RH, Usher HA. The changing pattern of fetal death, 1961–1988. Obstet Gynecol. 1992;79:35–39. [PubMed] [Google Scholar]
- 5.Skjaerven R, Wilcox AJ, Lie RT, Irgens LM. Selective fertility and the distortion of perinatal mortality. Am J Epidemiol. 1988;128:1352–1363. [DOI] [PubMed] [Google Scholar]
- 6.MacDorman MF, Atkinson JO. Infant mortality statistics from the linked birth/infant death data set—1995 period data. Month Vital Stat Rep. February 26, 1999;47(23):1–23. [PubMed] [Google Scholar]
- 7.Taffel S, Johnson D, Heuse R. A method of imputing length of gestation on birth certificates. Vital Health Stat 2. 1982;93:1–11. [PubMed] [Google Scholar]
- 8.Dubowitz LM, Dubowitz V, Goldberg C. Clinical assessment of gestational age in the newborn infant. J Pedatr. 1970;77:1–10. [DOI] [PubMed] [Google Scholar]
- 9.Ballard JL, Novak KK, Driver M. A simplified score for assessment of fetal maturation of newly born infants. J Pediatr. 1979;95:769–774. [DOI] [PubMed] [Google Scholar]
- 10.Liang K-Y, McCullagh P. Case studies in binary dispersion. Biometrics. 1993;49:623–630. [PubMed] [Google Scholar]
- 11.Holford TR. Understanding the effects of age, period, and cohort on incidence and mortality rates. Annu Rev Public Health. 1991;12:425–427. [DOI] [PubMed] [Google Scholar]
- 12.Meittinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol. 1974;99:325–332. [DOI] [PubMed] [Google Scholar]
- 13.Huang DY, Usher RH, Kramer MS, Yang H, Morin L, Fretts RC. Determinants of unexplained antepartum fetal deaths. Obstet Gynecol. 2000;95:215–221. [DOI] [PubMed] [Google Scholar]
- 14.Eriksson AW, Fellman J. Seasonal variation of livebirths, stillbirths, extramarital births and twin maternities in Switzerland. Twin Res. 2000;3:189–201. [DOI] [PubMed] [Google Scholar]
- 15.Glinianaia SV, Pharoah P, Sturgiss SN. Comparative trends in cause-specific fetal and neonatal mortality in twin and singleton births in the North of England, 1982–1994. Br J Obstet Gynaecol. 2000;107:452–460. [DOI] [PubMed] [Google Scholar]
- 16.Thompson LA, Goodman DC, Little GA. Is more neonatal intensive care always better? Insights from a cross-national comparison of reproductive care. Pediatrics. 2002;109:1036–1043. [DOI] [PubMed] [Google Scholar]
- 17.Zhang J, Yancey MK, Henderson CE. US. national trends in labor induction, 1989–98. J Reprod Med. 2002;47:120–124. [PubMed] [Google Scholar]
- 18.Ananth CV, Liu S, Kinzler WL, Kramer MS. Effects of age, period and birth cohorts on stillbirth trends in the United States and Canada. Paper presented at: 15th Annual Meeting of the Society for Pediatric and Perinatal Epidemiologic Research, June 10–11, 2003, Atlanta, Ga.
- 19.Parazzini F, Vecchia CL, Mezzanotte G, Fedele L. Maternal cohort, time of stillbirth, and maternal age effects in Italian stillbirth mortality. J Epidemiol Community Health. 1990;44:152–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liestol K. A note on the influence of factors early in development on later reproductive function. Ann Hum Biol. 1981;8:559–565. [DOI] [PubMed] [Google Scholar]
- 21.Wilcox AJ, Skjaerven R, Irgens LM. Harsh social conditions and perinatal survival: an age-period-cohort analysis of the World War II occupation of Norway. Am J Public Health. 1994;84:1463–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Demissie K, Rhoads GG, Ananth CV, et al. Trends in preterm birth and neonatal mortality among blacks and whites in the United States from 1989 to 1997. Am J Epidemiol. 2001;154:307–315. [DOI] [PubMed] [Google Scholar]
- 23.Samueloff A, Xenakis EM, Berkus MD, Huff RW, Langer O. Recurrent stillbirth: significance and characteristics. J Reprod Med. 1993;38:883–886. [PubMed] [Google Scholar]
- 24.Zeger SL, Liang K-Y. An overview of methods for the analysis of longitudinal data. Stat Med. 1992;11: 1825–1839. [DOI] [PubMed] [Google Scholar]
- 25.Preston FE, Rosendaal FR, Walker ID, et al. Increased fetal loss in women with heritable thrombophilia. Lancet. 1996;348:913–916. [DOI] [PubMed] [Google Scholar]
- 26.Martinelli I, Taioli E, Cetin I, et al. Mutations in coagulation factors in women with unexplained late fetal loss. N Engl J Med. 2000;343:1015–1018. [DOI] [PubMed] [Google Scholar]
- 27.Levine JS, Branch DW, Rauch J. The antiphospholipid syndrome. N Engl J Med. 2002;346:752–763. [DOI] [PubMed] [Google Scholar]
- 28.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2001.
- 29.Hogue CJ, Vasquez C. Toward a strategic approach for reducing disparities in infant mortality. Am J Public Health. 2002;92:552–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alex andander GR, Kogan MD, Nabukera S. Racial differences in prenatal care use in the United States: are disparities decreasing? Am J Public Health. 2002;92:1970–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]