Abstract
Objectives. We compared access and utilization of health services among American Indians/Alaska Natives (AIANs) with that among non-Hispanic Whites.
Methods. We used data from the 1997 and 1999 National Survey of America’s Families to estimate odds ratios for several measures of access and utilization and the effects of Indian Health Service (IHS) coverage.
Results. AIANs had less insurance coverage and worse access and utilization than Whites. Over half of low-income uninsured AIANs did not have access to the IHS. However, among the low-income population, AIANs with only IHS access fared better than uninsured AIANs and as well as insured Whites for key measures but received less preventive care.
Conclusions. The IHS partially offsets lack of insurance for some uninsured AIANs, but important needs were potentially unmet.
Although the health status of American Indians and Alaska Natives (AIANs) improved after the establishment of the Indian Health Service (IHS) in 1955, significant health disparities persist.1–3 The federal government attempts to meet its commitment to provide health care for AIANs through a system of hospitals and clinics on or near reservations, managed by the IHS and, more recently, by Indian tribes.4 IHS facilities provide primary care services free of charge, and limited free specialty services are available through contracts with private providers.5 However, services available through the IHS vary widely across tribes, and IHS hospitals are not available in all service areas.6 Many communities have small clinics and must contract out for all specialty care, x-ray services, and other diagnostic tests and routine preventive care such as mammograms. Services can vary and may be limited by significant shortfalls in funding.5
The IHS serves approximately 1.5 million people, but it does not serve all of the 4.1 million individuals whom the Census Bureau reports as being American Indian or Alaska Native, either alone or in combination with other races.7 Some of these self-identified AIANs are ineligible for the IHS, primarily because they are not members or descendants of federally recognized tribes. In addition, most AIANs live in urban areas away from their home reservations and cannot access IHS services, forcing them to rely on other sources of coverage or become uninsured.8
Previous studies have documented lower public and private coverage, poorer health status, and greater unmet needs among AIANs because of factors such as income, education, and the availability and utilization of IHS services.9–12 However, these studies used surveys from the 1980s and early 1990s. More updated information is needed, because there have been significant changes in the organization and financing of the IHS, with approximately half of the IHS budget now managed by tribes.13 In addition, little research has been conducted to determine the impact of various sources of coverage on the health care of this population.
Data from the 1997 and 1999 National Survey of America’s Families (NSAF) provide more recent information on insurance coverage, access, and utilization as well as race and ethnicity. In this study, we conducted an analysis to answer the following questions: (1) How do AIANs and non-Hispanic Whites (hereafter “Whites”) compare regarding socioeconomic/demographic characteristics? (2) How do AIANs and Whites compare regarding insurance coverage? (3) Are differences in access to care and utilization related to differences in socioeconomic/demographic characteristics between AIANs and Whites? (4) What role does the IHS play in affecting access and utilization among otherwise uninsured AIANs?
METHODS
The NSAF is a nationally representative survey of the noninstitutionalized civilian population younger than 65 years that draws its sample from all 50 states (plus the District of Columbia). In addition, NSAF oversamples low-income households (those with family incomes below 200% of the federal poverty level) and households in 13 states.14 This analysis is based on combined data from the 1997 and 1999 rounds of NSAF to allow adequate sample sizes to detect with precision differences between AIANs and Whites. The 2 years of data have combined sample sizes of nearly 2500 AIANs and about 125 000 Whites. The sample was weighted to population totals, and weights were adjusted for the design features of the sample, including nonresponse and undercoverage.
NSAF provides data that allow assessment of health care access and utilization. The last national targeted survey of AIAN health care access and utilization was the Survey of American Indians and Alaska Natives of the 1987 National Medical Expenditure Survey. Although the sample size was nearly 7000 persons, the Survey of American Indians and Alaska Natives included only American Indian households in which at least 1 member of the household was eligible for IHS coverage.15 National Health Interview Surveys conducted at roughly the same time as the NSAF included only about 700 AIANs per year.16 More recent Medical Expenditure Panel Surveys have annual samples of AIANs of about 300 to 600 people.17
Health insurance coverage was classified into 4 mutually exclusive categories: employer/other (including employer-sponsored coverage, privately purchased coverage, coverage that could not be classified elsewhere, and Medicare); public/state (including Medicaid, State Children’s Health Insurance Program, and state health insurance programs); IHS only (AIANs who have no other source of coverage and who report the IHS as a source of coverage); and uninsured (Whites without coverage and AIANs who did not report IHS coverage and had no private or public coverage). We separated AIANs who reported only the IHS as a source of coverage from AIANs who were uninsured but did not report the IHS as a source of coverage to explore differences between these 2 subgroups.
This analysis used a range of health care access and utilization measures. Measures of access to care included having a usual source of care that was not a hospital emergency room (ER) at the time of the survey and having unmet needs in the prior 12 months for prescription drug, dental, or medical/surgical care (defined as not getting or postponing getting care when it was needed). Respondents were also asked 3 questions regarding perceptions of care: satisfaction with the quality of medical care the family received during the last 12 months (respondents who were “somewhat dissatisfied” or “very dissatisfied” were categorized as not satisfied); confidence that family members could get care if they needed it (respondents who were “not too confident” or “not confident at all” were categorized as not confident), and experiences with doctors or other health professionals who listened carefully and explained things in an understandable way during the last 12 months (respondents who indicated they “sometimes” or “never” experienced this were categorized as having communication problems with their providers). In addition, we used 6 measures of health care utilization during the 12 months before the survey: (1) had a doctor or health professional visit; (2) had an ER visit; (3) had a Papanicolaou test (women only); (4) had a breast physical examination (women only); (5) had a dental visit (those older than 3 years only); and (6) had a well-child visit (children only).
Using t tests, we compared the socioeconomic and demographic characteristics and patterns of insurance coverage of AIANs and Whites. We explored insurance coverage by income group because public insurance coverage is largely only available to lowerincome groups. We present access and use differentials between AIANs and Whites as odds ratios. For example, the odds ratio for having an ER visit measures the odds of AIANs having an ER visit relative to the same odds for Whites. The odds ratios are presented both as they were observed in the sample and after we controlled for differences in characteristics between the 2 groups with multivariate logistic models.
Additional results about the relations between insurance coverage or the IHS and access and utilization are based on regression-adjusted means derived from a 2-step process. First, we estimated logistic regression models that control for differences in socioeconomic status and demographic characteristics, including age, education level, poverty level, gender, health status, disability status, community type (urban vs rural), and insurance status. Second, we predicted values of the dependent variables for each race/insurance coverage group, using insured Whites as a comparison group. Variances of estimates were adjusted to account for the survey’s complex sample design. Because only about 40% of the raw sample of AIANs in NSAF had incomes above 200% of the federal poverty level and because very few in this group reported the IHS as their only source of care, our assessment of the IHS is limited to those with low incomes.
RESULTS
Socioeconomic and Demographic Characteristics
AIANs were younger, less well educated, and poorer than Whites (Table 1 ▶). Thirty-eight percent of AIANs were children, compared with 28% of Whites (P < .01). Twenty percent of AIANs lived in families in which no adult graduated from high school, whereas this was the case for only 6% of Whites (P < .01). Furthermore, only a quarter of Whites were in families with incomes below 200% of the federal poverty level, whereas 55% of AIANs had low incomes (P < .01).
TABLE 1—
Socioeconomic and Demographic Characteristics of Whites and American Indians/Alaska Natives: National Survey of America’s Families, 1997 and 1999
| Non-Hispanic Whites, % | American Indians/Alaska Natives, % | Pa | |
| Age, y | |||
| 0–17 | 28 | 38 | <.01 |
| 18–35 | 28 | 29 | .56 |
| 36–54 | 33 | 27 | <.01 |
| 55–64 | 11 | 6 | <.01 |
| Gender | |||
| Female | 50 | 52 | .42 |
| Male | 50 | 48 | .42 |
| Educationb | |||
| < High school | 6 | 20 | <.01 |
| High school | 28 | 31 | .08 |
| ≥ Some college | 66 | 48 | <.01 |
| Family Income, % federal poverty level | |||
| <100 | 9 | 30 | <.01 |
| 100–199 | 15 | 25 | .03 |
| 200–299 | 18 | 20 | .19 |
| ≥ 300 | 57 | 25 | <.01 |
| County of residence | |||
| Outside MSA | 24 | 44 | <.01 |
| Inside MSA | 76 | 56 | <.01 |
| Health status | |||
| Fair or poor | 8 | 16 | <.01 |
| Excellent, very good, or good | 92 | 84 | <.01 |
| Health condition that limits work or usual activities | |||
| Has limiting condition | 12 | 20 | <.01 |
| No limiting condition | 88 | 80 | <.01 |
| Population size, weighted, millions | 166 | 2 | |
| Sample size, unweighted | 126695 | 2449 | |
Note. MSA = metropolitan statistical area.
aP values are for the difference between non-Hispanic Whites and American Indians/Alaska Natives.
bEducation is defined as the highest level of education attained among the adults in the family.
Compared with Whites, the health status of AIANs was worse. Sixteen percent of AIANs were in fair or poor health, compared with just 8% of Whites (P < .01), and they were more likely to have functional limitations that inhibited their work or usual activities (20% of AIANs vs 12% of Whites; P < .01).
Sources of Coverage and Care
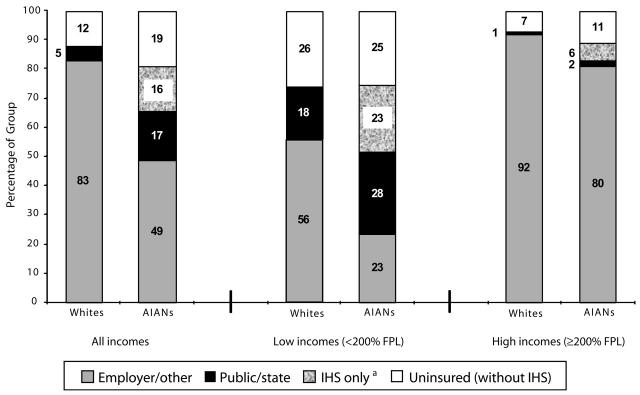
AIANs had much lower rates of employer/other coverage (49% of AIANs vs 83% of Whites; P < .01) and higher rates of public/state coverage (17% of AIANs vs 6% of Whites; P < .01) (Figure 1 ▶). Sixteen percent of AIANs reported IHS coverage only, and an additional 19% were uninsured and did not report the IHS as a source of coverage. Using the Census Bureau definition of being uninsured (uninsured even if they have IHS coverage), we found that AIANs had an uninsurance rate of 35%, almost 3 times the 12% rate for Whites (P < .01). Only about half of uninsured AIANs reported having access to IHS care.
FIGURE 1—
Sources of Coverage and Care, by Income, Whites and American Indians/Alaska Natives, 1997 and 1999.
Note. FPL = federal poverty level; AIANs = American Indians/Alaska Natives; IHS = Indian Health Service.
a “IHS only” includes American Indians/Alaska Natives who are uninsured and indicated that the Indian Health Service (IHS) was their only source of coverage.
Among low-income families, the rate of employer/other coverage for AIANs (23%) was less than half that of Whites (56%) (P < .01). Twenty-three percent of low-income AIANs had IHS coverage only, and an additional 25% were uninsured without the IHS. For those with higher incomes, differences between AIANs and Whites were smaller. However, following Census Bureau definitions, higher-income AIANs were more than twice as likely to be uninsured than higher-income Whites. Very few higher-income AIANs (6%) reported IHS coverage only.
Health Care Access and Utilization
AIANs reported more problems accessing health care than Whites and had lower rates of utilization (first 3 columns of Table 2 ▶). Although both groups were equally likely to have a usual source of care, AIANs reported higher levels of unmet need, largely due to differences in unmet dental needs.
TABLE 2—
Health Care Access and Utilization of Whites and American Indians/Alaska Natives: National Survey of America’s Families, 1997 and 1999
| Non-Hispanic Whites, % | American Indians/Alaska Natives, % | Unadjusted Odds Ratio | Adjusted Odds Ratio Without Incomea | Adjusted Odds Ratio With Incomeb | |
| Access/perceptions of care | |||||
| Has usual source of care | 88 | 87 | 0.84 | 0.89 | 1.03 |
| Any unmet need last year | 17 | 20 | 1.24*** | 1.17* | 1.02 |
| Unmet medical care need last year | 7 | 7 | 1.05 | 0.93 | 0.83 |
| Unmet drug need last year | 4 | 5 | 1.18 | 0.96 | 0.83 |
| Unmet dental need last year | 11 | 14 | 1.28** | 1.24* | 1.08 |
| Not confident of access to care | 7 | 11 | 1.71*** | 1.33 | 1.10 |
| Not satisfied with quality of medical care | 10 | 16 | 1.78*** | 1.57*** | 1.43*** |
| Doctor sometimes/never listened and explained (1999 only) | 17 | 26 | 1.70*** | 1.47*** | 1.38** |
| Utilization | |||||
| Any health professional or doctor visit last year | 80 | 74 | 0.73*** | 0.78** | 0.86 |
| Any emergency room visit last year | 21 | 34 | 1.94*** | 1.51*** | 1.41*** |
| Had Pap test last year (women only) | 65 | 57 | 0.71** | 0.91 | 1.00 |
| Had breast physical exam last year (women only) | 59 | 51 | 0.72** | 0.94 | 1.03 |
| Any dental visit last year (excluding 0- to 2-year-olds) | 74 | 64 | 0.60*** | 0.78** | 0.93 |
| Any-well child care last year (children only) | 63 | 60 | 0.88 | 1.10 | 1.08 |
| Population size, weighted, millions | 165.9 | 2.3 | |||
| Sample size, unweighted | 126695 | 2449 | |||
aAdjusted odds ratios after control for survey year, age, education, gender, health and disability status, and residential location.
bAdjusted odds ratios after control for survey year, age, education, gender, health and disability status, residential location, and family income.
*P < .10; **P < .05; ***P < .01.
More AIANs reported lacking confidence in their family’s access to care (odds ratio [OR] = 1.71; P < .01) or being dissatisfied with the quality of care their family received (OR = 1.78; P < .01). Perceptions of care interactions were also worse for AIANs; 26% reported poor communication with providers, compared with 17% of Whites (OR = 1.70; P < .01).
AIANs were less likely than Whites to use basic medical care, including health professional/doctor visits (OR = 0.73; P < .01) and dental visits (OR = 0.60; P < .01). The probability of having a visit to an ER was higher for AIANs than for Whites (OR = 1.94; P < .01), possibly signaling problems accessing community-based ambulatory care. AIAN women were less likely to receive preventive care (OR = 0.71; P < .05 for Pap tests; and OR = 0.72; P < .05 for breast examinations). However, for children, there was no statistical difference between the groups in the likelihood of having well-child care.
The final 2 columns of Table 2 ▶ show adjusted odds ratios for access and utilization differences between AIANs and Whites when we controlled for all factors in Table 1 ▶ except income (column 4) and then when we included income (column 5). We treated income separately because of the prominent role it can play in determining insurance status.
As column 4 shows, most of the significant differentials in access and use between AIANs and Whites were reduced in magnitude but remained statistically significant when we controlled for characteristics other than income. The only exceptions to this were the probability of not being confident in their ability to get care and the probabilities of having a breast examination or a Pap test. However, when we added the control for income (column 5), only 3 of the 10 odds ratios that were significant in column 3 remained significant. Although this suggested that income and the other factors explained most of the differences in access and use between AIANs and Whites, AIANs remained more likely to be dissatisfied with their care, to have problems with provider communication, and to have an ER visit.
Access, Utilization, and The IHS
Table 3 ▶ compares access and utilization by insurance status for low-income AIANs and Whites. Insured AIANs and insured Whites had similar levels of access, utilization, and perceptions when other differences between these groups were held constant. The only statistically significant differences were related to the probability of having an ER visit (36% for insured AIANs compared with 29% for insured Whites; P = .02) and being dissatisfied with quality of care (17% for insured AIANs compared with 12% for insured Whites; P = .05).
TABLE 3—
Health Care Access and Utilization of Low-Income Whites and American Indians/Alaska Natives, by Health Insurance Status, Adjusted Percentagesa: National Survey of America’s Families, 1997 and 1999
| Insured | Uninsured/IHS | ||||
| Non-Hispanic Whites, % | American Indians/Alaska Natives, % | Non-Hispanic Whites, % | American Indians/Alaska Natives, % | ||
| Uninsured | IHS Onlyb | ||||
| Access/perceptions of care | |||||
| Has usual source of care | 90 | 89 | 73 | 74 | 89c |
| Any unmet need last year | 20 | 19 | 34 | 19 | 20 |
| Unmet medical care need last year | 7 | 6 | 18 | 9 | 6 |
| Unmet drug need last year | 6 | 6 | 10 | 4 | 3d |
| Unmet dental need last year | 14 | 13 | 24 | 12 | 18 |
| Not confident of access to care | 9 | 10 | 25 | 19 | 17 |
| Not satisfied with quality of medical care | 12 | 17 | 20 | 19 | 15 |
| Doctor sometimes/never listened and explained (1999 only) | 20 | 24 | 27 | 25 | 26 |
| Utilization | |||||
| Any health professional or doctor visit last year | 82 | 80 | 61 | 54 | 78e |
| Any emergency room visit last year | 29 | 36 | 26 | 18 | 35e |
| Had Pap test last year (women only) | 56 | 62 | 42 | 40 | 41f |
| Had breast physical exam last year (women only) | 54 | 57 | 35 | 43 | 33 |
| Any dental visit last year (excluding 0- to 2-year-olds) | 68 | 63 | 48 | 51 | 71e,f |
| Any well-child care last year (children only) | 64 | 66 | 42 | 43 | 60 |
Note. IHS = Indian Health Service; AIANs = American Indians/Alaska Natives. Boldface numbers indicate significant difference from insured non-Hispanic Whites (P < .05). Boldface italic numbers indicate significant difference from insured non-Hispanic Whites (P < .10).
aRegression-adjusted means after control for differences in socioeconomic and demographic characteristics, including age, education level, poverty level, gender, health status, disability status, and community type.
b“IHS only” includes AIANs who are uninsured but indicated that the IHS was their only source of coverage.
cIndicates significant difference from uninsured AIANs (P < .10).
dIndicates significant difference from insured AIANs (P < .05).
eIndicates significant difference from uninsured AIANs (P < .05).
fIndicates significant difference from insured AIANs (P < .10).
Uninsured Whites and uninsured AIANs were also similar, but both groups fared much worse than insured Whites. Both groups were less likely to have a usual source of care, less likely to have health professional/doctor and dental visits, less likely to receive Pap tests, and less confident and satisfied with care than insured Whites. However, uninsured AIANs (19%) and insured Whites (20%) were equally as likely to report unmet needs, whereas uninsured Whites (34%) were significantly more likely than insured Whites to do so. When we controlled for other differences, these findings showed that insurance status had a greater effect than race on access and utilization for some measures, but that differences remained between uninsured AIANs and uninsured Whites with respect to unmet needs.
The comparison of AIANs with only IHS coverage to insured Whites showed very few statistically significant differences in access and utilization between these groups when other factors were held constant. In fact, AIANs who reported only IHS coverage had higher rates of access and utilization than uninsured AIANs without the IHS. They were more likely to have a usual source of care (89% for those with IHS coverage compared with 74% for those without it; P = .06) and to have had health professional/doctor (78% vs 54%; P < .01) and dental visits (71% vs 51%, P = .04). Having access to the IHS increased access and utilization for AIANs who would otherwise be uninsured. Despite these differences, there were no significant differences related to unmet needs or perceptions of care.
AIANs with only IHS coverage did not do as well as insured Whites for all the indicators we examined. There was evidence of deficiencies in preventive health care. AIAN women with IHS coverage only were less likely to have had a breast physical examination (33%) than insured White women (54%; P = .09). Thus, there were gaps in the services to which the IHS population gained access, even when we controlled for other differences.
DISCUSSION
The NSAF provides an opportunity to answer questions about current patterns of health coverage, access, and utilization by nonelderly AIANs relative to similar-aged Whites and to inform policy discussions about the IHS. The NSAF study population was unique in that more than half of AIANs surveyed resided in urban areas, reflecting the demographic profile of the AIAN population today.8
Data from the NSAF reveal that large disparities persist in the socioeconomic conditions, health, and health care of AIANs relative to Whites. These findings are consistent with both the IHS and census data1,7 and suggest that the gains in socioeconomic well-being that occurred among AIANs in the past decade were not sufficient to close the health care gap between AIANs and Whites.
The NSAF also shows that AIANs were more likely to be uninsured than Whites. The uninsurance rate of AIANs is also higher than that of African Americans and is comparable to the uninsurance rate of Hispanics.18 These higher rates for AIANs are troubling because uninsured people, regardless of race/ethnicity, have less access to routine care for chronic conditions and care for serious medical conditions.19 Although many assume that the IHS services are available to most, if not all, AIANs, just under half of low-income uninsured AIANs reported having access to the IHS. Higher rates of uninsured low-income AIANs are largely a function of lower rates of private coverage. Although these findings are consistent with those of other studies,12 factors underlying the lower rates of private coverage deserve further investigation. However, given the large proportion of AIANs who had low incomes, it is likely that public approaches to expanding sources of coverage and care will need to be considered to reduce the disparity.
In examining the relationship between insurance coverage and access to and use of health services, we found little difference between low-income AIANs and Whites. For both race/ethnicity groups, the insured fared better than the uninsured when we held socioeconomic and demographic factors constant. Another recent study found small differences in satisfaction with care between Whites and American Indians with similar coverage.20 However, our study provides evidence that AIANs with access to the IHS are more likely to receive health care services than other uninsured AIANs. With the exception of preventive services, AIANs with access only to the IHS had patterns of access and use that were similar to those of Whites and AIANs with coverage. At least 1 other study reported similar findings.12
The role of the IHS seems to be similar to the role of the Department of Veterans Affairs, which also provides health care for eligible and enrolled veterans and has been shown to increase access and utilization for those veterans who are otherwise uninsured.9 Although the IHS has undergone a significant reorganization in the past few years with downsizing of administrative functions and an increased role of tribes in managing their health care services, the effects of this reorganization were probably not realized at the time of the data collection for the NSAF. However, the trend toward tribal management of Indian health programs has been associated with increased flexibility in funding sources and increased programs and services in some areas.6 This could have a role in making IHS coverage similar to private insurance in some programs. However, IHS coverage varies widely among Indian health programs and should not be assumed to be equivalent to defined benefits packages of private insurance.
Given the cross-sectional nature of these data, we need to use some caution before concluding that the IHS actually improves health care access and use among otherwise uninsured low-income AIANs. It is possible that low-income AIANs who use IHS facilities may have a greater propensity to seek out care or use health services, and this could bias our estimate of the effects of the IHS in the positive direction. Although our estimates of the effects of the IHS control for health status, income, and education—key determinants of the demand for health care—we recognize that there may also be unmeasured determinants of the demand for care. Even if these unmeasured factors are partly responsible for the IHS estimates in this study, these findings still show, not surprisingly, that low-income AIANs with access to the IHS report higher rates of having a usual source of care and higher rates of utilization than low-income uninsured AIANs without such access.
However, women with access to only the IHS still had lower rates of preventive care, which is consistent with other studies.21 This may reflect the relative lack of resources for preventive care in the IHS, which was initially designed to address more acute and emergent conditions. Low rates of breast examinations among AIAN women with access only to an IHS provider could be related to the scarcity of mammography equipment in some IHS service areas.5
Although the NSAF is an important new data source that can be used to analyze health care among AIANs, it is not without some limitations. First, the design of the NSAF survey only allows an assessment of the IHS among otherwise uninsured AIANs. According to estimates for 1999 from the Current Population Survey, 15% of AIANs with other types of coverage also reported access to the IHS.22 Other research has shown that AIANs with IHS and other coverage may have higher utilization rates than those with the IHS alone.12 Second, NSAF sample sizes do not allow an analysis of potential differences in the role of the IHS between AIANs living in rural areas and those living in urban areas. However, in this sample, only 20% of those reporting IHS coverage only were in metropolitan statistical areas, indicating that the IHS-only group was mostly rural. Finally, given that the NSAF only provides general information on health status and disabilities, we cannot examine variations in outcomes for people with some specific conditions that are disproportionately present among AIANs.
Documented disparities in health coverage and care show that AIANs continue to be at a disadvantage in the US health system. Although these data do not present a comprehensive picture of how well the health care needs of AIANs are being met, they raise a number of issues for policymakers. First, AIANs lack insurance coverage at much higher rates than Whites, and efforts are needed to reduce these disparities in coverage. Second, the IHS provides a valuable source of basic health care for some AIANs who lack coverage, but there are clearly gaps in preventive care that need to be addressed. Because the IHS is funded through congressional appropriations rather than as an entitlement, it is subject to the constraints of the federal legislative process. Thus, as currently structured and funded, the IHS will be a critical component of efforts to meet the health care needs of AIANs, but a more comprehensive strategy will be needed.
Acknowledgments
We are grateful for financial support provided by the Henry J. Kaiser Family Foundation. We thank Angela Yip for her skillful research assistance and Tim Waidmann for his helpful comments.
Human Participant Protection Data analyzed for this manuscript were obtained from telephone interviews as part of the National Survey of America’s Families, sponsored by the Urban Institute. The survey has undergone institutional review board approval, and all participants consented to being interviewed.
Note. The views expressed here are those of the authors and should not be attributed to the Urban Institute or its board or sponsors, the University of Arizona, or the Henry J. Kaiser Family Foundation.
Contributors S. Zuckerman and J. Haley were responsible for study design and data analysis. Y. Roubideaux and M. Lillie-Blanton contributed the policy background and context for the findings. All authors contributed to the interpretation of the results and the writing of the article.
Peer Reviewed
References
- 1.Indian Health Service. Trends in Indian Health: 1998–99. Rockville, Md: US Department of Health and Human Services, Indian Health Service; 1999.
- 2.Grossman DC, Baldwin LM, Casey S, Nixon B, Hollow W, Hart LG. Disparities in infant health among American Indians and Alaska Natives in US metropolitan areas. Pediatrics. 2002;109:627–633. [DOI] [PubMed] [Google Scholar]
- 3.Keppel KG, Pearcy HN, Wagener DK. Trends in racial and ethnic-specific rates for the health status indicators: United States, 1990–98. Healthy People 2000 Stat Notes. 2002;23:1–16. [PubMed] [Google Scholar]
- 4.Dixon M, Roubideaux Y. Introduction. In: Dixon M, Roubideaux Y, eds. Promises to Keep: Public Health Policy for American Indians and Alaska Natives in the 21st Century. Washington, DC: American Public Health Association; 2001:xix–xxi.
- 5.Dixon M. Access to care for American Indians and Alaska Natives. In: Dixon M, Roubideaux Y, eds. Promises to Keep: Public Health Policy for American Indians and Alaska Natives in the 21st Century. Washington, DC: American Public Health Association; 2001:61–87.
- 6.Dixon M. The unique role of tribes in the delivery of health services. In: Dixon M, Roubideaux Y, eds. Promises to Keep: Public Health Policy for American Indians and Alaska Natives in the 21st Century. Washington, DC: American Public Health Association; 2001:31–59.
- 7.Ogunwale SU. The American Indian and Alaska Native Population: 2000. Washington, DC: US Census Bureau; 2002.
- 8.Forquera, R. Challenges in serving the growing population of urban Indians. In: Dixon M, Roubideaux Y, eds. Promises to Keep: Public Health Policy for American Indians and Alaska Natives in the 21st Century. Washington, DC: American Public Health Association; 2001:122–134.
- 9.Washington DL, Harada ND, Villa VM, et al. Racial variations in the Department of Veterans Affairs ambulatory care use and unmet health care needs. Mil Med. 2002;167:235–241. [PubMed] [Google Scholar]
- 10.Beauregard K, Cunningham P, Cornelius L. Access to Health Care: Findings from the Survey of American Indians and Alaska Natives. Rockville, Md: Public Health Service; 1991. Agency for Health Care Policy and Research Publication 91–0028. Research Findings 9.
- 11.Cunningham P, Schur C. Health Care Coverage: Findings from the Survey of American Indians and Alaska Natives. Rockville, Md: Public Health Service; 1991. Agency for Health Care Policy and Research Publication 91–0027. Research Findings 8.
- 12.Brown ER, Ojeda VD, Wyn R, Levan R. Racial and Ethnic Disparities in Access to Health Insurance and Health Care. Los Angeles, Calif: UCLA Center for Health Policy Research; 2000.
- 13.Indian Health Service Year 2002 Profile. Washington, DC: US Department of Health and Human Services; 2002.
- 14.Kenney GM, Scheuren F, Wang K. 1997 NSAF Survey Methods and Data Reliability. Washington, DC: Urban Institute; 1999. National Survey of America’s Families Methodology Series, Report No. 1.
- 15.Cunningham PJ. Access to care in the Indian Health Service. Health Aff. 1993;12:224–233. [DOI] [PubMed] [Google Scholar]
- 16.Urban Institute tabulations of the 1997 and 1998 National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed November 6, 2002.
- 17.Agency for Healthcare Research and Quality. Household Component Analytical Tool (MEPSnet/HC). 2001. Available at: http://www.meps.ahrq.gov/mepsnet/HC/MEPSnetHC.asp. Accessed November 6, 2002.
- 18.Mills RJ. Health insurance coverage: 2001. 2002. Available at: http://www.census.gov/prod/2002pubs/p60–220.pdf. Accessed April 11, 2003.
- 19.Institute of Medicine. Coverage Matters: Insurance and Health Care. Washington, DC: National Academy Press; 2001.
- 20.Morales LS, Elliott MN, Weech-Maldonado R, Spritzer KL, Hays RD. Differences in CAHPS adult survey reports and rating by race and ethnicity: an analysis of the National CAHPS benchmarking data 1.0. Health Serv Res. 2001;36:595–617. [PMC free article] [PubMed] [Google Scholar]
- 21.Lefkowitz DC, Underwood C. Personal Health Practices: Findings from the Survey of American Indians and Alaska Natives. Rockville, Md: Public Health Service; 1991. Agency for Health Care Policy and Research Publication. 91–0034. Research Findings 10.
- 22.Urban Institute tabulations of the 2000 Current Population Survey. Available at: http://www.census.gov/hhes/www/hlthins.html. Accessed April 11, 2003.