Abstract
Objectives. I tested the hypothesis that Black men with high levels of distrust (i.e., mild paranoia) are at greater risk of hospitalization for mental health problems than their White counterparts.
Methods. Secondary analysis was conducted of data from a subsample of 180 men in an epidemiological study. Mental health hospitalization was the outcome and ethnicity/race, mild paranoia, and their interaction were main predictors in a logistic regression analysis. The ethnicity/race by mild paranoia interaction tested the study hypothesis.
Results. The ethnicity/race by mild paranoia interaction was statistically significant. Contrary to the hypothesis, Black men with mild paranoia were less likely to be hospitalized.
Conclusions. Black men’s lack of trust regarding the mental health system may cause them not to seek services. Factors critical to increasing their trust are acknowledgment of racial biases in the mental health system and sincere efforts to eliminate racial disparities in mental health treatment.
Prevalence studies of inpatient samples have revealed that paranoid schizophrenia is a common diagnosis given to Blacks.1,2 Several researchers attribute these findings to biases associated with racial stereotypes, especially those about Black men. The stereotype that Black men are prone to violence contributes to the misdiagnosis of paranoid schizophrenia.3,4 Racial stereotypes of violence often operate at the unconscious level in mental health clinicians’ diagnostic judgments about Black men.5 The racial stereotyping of Black men, which has been euphemistically labeled “racial profiling,” has now been publicly acknowledged by criminal justice and other governmental agencies.6 These racist experiences or cultural stereotypes in American society and their consequences contribute to the development of what has been referred to in the past as “healthy cultural paranoia,” or the more contemporary term of “cultural mistrust,” on the part of Black men.7,8 Healthy cultural paranoia or cultural mistrust is Black Americans’ distrust of White society as a defense against threats of racism and discrimination. Paranoia can therefore be viewed either as a symptom of psychopathology or as a type of cultural coping response in Black men.
Moreover, given the prominent role of paranoia in the diagnosis and treatment of severe mental illness, studies focusing on such symptoms are warranted. Mental health service providers must be able to distinguish between cultural and pathological aspects of Black men’s coping responses to deliver competent interventions. Clinicians need to become familiar with these cultural coping response styles to provide effective treatment for Black men. Recent advances in the study of paranoia may help mental health professionals to develop a better understanding of cultural paranoia and mistrust. There is increasing theoretical and empirical support for the notion that paranoid symptoms fall along a continuum of severity extending from mild, reality-based expressions of lack of trust, suspiciousness, and self-consciousness to the florid delusions found in schizophrenia.9,10 Moreover, Whaley11,12 has demonstrated empirically that cultural influences on paranoid thinking occur at the mild end of the continuum. The failure to recognize milder forms of paranoia, such as distrust, as nonpathological may contribute to the high rate of psychiatric hospitalizations for Black men. The purpose of this study was to examine the interaction between ethnicity/race and level of mild paranoia in terms of the risk of hospitalization for mental health problems of Black men relative to their White counterparts. I hypothesized that Black men with high levels of distrust (i.e., nonpathological paranoia) would be at greater risk than their White counterparts of hospitalization for mental health problems.
METHODS
Participants
The participants were a subsample of 180 men from an epidemiological study of risk factors for depression and schizophrenia.13 This subsample included 119 (66%) Whites and 61 (34%) Blacks. Of the total subsample, 136 men (76%) were “well” or did not have a diagnosed mental disorder. Demographic and clinical characteristics by ethnicity/race are presented in Table 1 ▶.
TABLE 1—
Sociodemographic and Clinical Variables, by Ethnicity/Race, for an Epidemiological Study Subsample of 180 Men
| Black (n = 61) | White (n = 119) | Test Statistic | |
| Mental health hospitalization, no. (%) | χ2 = 8.84, P < .005 | ||
| Hospitalization | 15 (25%) | 10 (8%) | |
| Nonhospitalization | 46 (75%) | 109 (92%) | |
| Mean age, y (SD) | 38.09 (10.34) | 40.61 (11.00) | t = .45, P = NS |
| Marital status, no. (%) | χ2 = 1.49, P = NS | ||
| Never married | 17 (28%) | 43 (36%) | |
| Divorced | 14 (23%) | 21 (18%) | |
| Married | 30 (49%) | 55 (46%) | |
| Education, no. (%) | χ2 = 30.42, P < .001 | ||
| Less than high school graduate | 20 (33%) | 16 (14%) | |
| High school graduate | 37 (61%) | 48 (40%) | |
| College graduate | 4 (6%) | 55 (46%) | |
| Family income (in $), no. (%) | χ2 = 15.95, P < .001 | ||
| 0–6999 | 17 (28%) | 16 (14%) | |
| 7000–14 999 | 20 (33%) | 20 (17%) | |
| 15 000–24 999 | 16 (26%) | 48 (40%) | |
| ≥ 25 000–50 000 | 8 (13%) | 35 (29%) | |
| Mean occupational prestige score (SD) | 36.32 (12.68) | 46.14 (13.69) | t = 4.63, P < .001 |
| Diagnosis of mental disorder, no. (%) | χ2 = 2.25, P = NS | ||
| Case | 19 (31%) | 25 (21%) | |
| Noncase | 42 (69%) | 94 (79%) | |
| Mild paranoia (distrust), no. (%) | χ2 = 1.89, P = NS | ||
| Low | 21 (35%) | 54 (46%) | |
| High | 39 (65%) | 64 (54%) | |
| Moderate paranoia (perceived hostility of others), no. (%) | χ2 = .48, P = NS | ||
| Low | 25 (42%) | 56 (48%) | |
| High | 34 (58%) | 61 (52%) | |
| Severe paranoia (false beliefs and perceptions), no. (%) | χ2 = .15, P = NS | ||
| Low | 21 (35%) | 44 (38%) | |
| High | 39 (65%) | 72 (62%) | |
| Mean social desirability score (SD) | 0.63 (0.20) | 0.55 (0.20) | t = 2.76, P < .01 |
Note. NS = not significant.
Measures
Hospitalization for mental health problems.
One item included in a methodological study of the Psychiatric Epidemiology Research Interview (PERI)14 asked respondents whether they have ever been hospitalized for a mental health problem. Fifty-eight (32%) respondents said “never,” 10 (6%) reported 1 hospitalization, and 15 (8%) reported more than 1 hospitalization. The remaining 97 (54%) respondents had missing data for the question. All respondents with missing data and “never” responses were treated as nonhospitalizations, and responses of “once” and “more than once” were collapsed into a single hospitalization category. Thus, mental health hospitalization was coded as a dichotomous variable of 155 (86%) nonhospitalizations and 25 (14%) hospitalizations.
Continuum of paranoia.
Self-reports of mild, moderate, and severe paranoia were assessed, respectively, by the scales of Distrust, Perceived Hostility of Others, and False Beliefs and Perceptions of the PERI.14 The continuum of paranoia captured in these 3 scales has been shown to be reliable and valid.11,12 Individual scale scores are derived by summing the item scores and dividing the total score by the number of items, yielding a range of 0–4. A median split procedure was performed on the scales of Distrust, Perceived Hostility of Others, and False Beliefs and Perceptions to derive categorical classifications of high (i.e., greater than or equal to the median) and low (i.e., less than the median) scale scores.11
Social desirability.
Social desirability, defined as the tendency of individuals to respond in ways that make a favorable impression on others, was measured with the 30-item scale developed by Crowne and Marlowe.15 Social desirability is measured in the PERI via items with the responses “True,” “False,” or “Don’t Know” (scored as 2, 0, and 1, respectively). Half of the statements describe desirable traits, and the other half describe undesirable traits. “True” for desirable traits and “False” for undesirable traits were scored in the same direction. Total scores, based on the sum of the item scores divided by the total number of items, range from 0 to 2, with higher total scores reflecting greater social desirability (i.e., a greater tendency to behave in a socially desirable manner).
Diagnosis of mental disorder.
Clinical records and unstructured clinical interviews were used to make reliable research diagnoses under the supervision of members of the Biometrics Unit of the New York State Psychiatric Institute.16 The psychiatric patient group for the risk-factor study that focused on schizophrenia (mainly DSM-III schizophrenia) and depression included 96 men with depression and 65 men with nonorganic, nonaffective psychotic disorders, or “schizophrenia-like” disorders.13 The subsample included 20 men with depression (40% Black, 60% White) and 24 men with schizophrenia-like disorders (46% Blacks, 54% Whites).
Procedure
The group of well Black and White men was a subsample of a random sample drawn from the population of the Washington Heights community of New York City. The full sample was selected by the following 3-step procedure: (1) a random sample of households was generated with telephone directories; (2) the eligibility of households was determined by age (19–59 years) and ethnicity/race (Blacks were oversampled); and (3) up to 2 opposite-sex respondents were randomly selected from each eligible household. Psychiatric patients were recruited mainly from the outpatient clinic and from an inpatient community service program at Columbia–Presbyterian Medical Center in the same New York City community. Patients between 19 and 59 years of age with a recent episode of psychiatric disorder established and dated to within a year of the interview were deemed eligible.
RESULTS
Selected sociodemographic and clinical variables were compared between Black and White respondents (Table 1 ▶). Bivariate analyses revealed significant ethnic/racial differences in the recoded mental health hospitalization variable. The unadjusted odds ratio indicated that Black men (25%) were 3.54 times more likely than White men (8%) to be hospitalized for mental health problems. Bivariate analyses also showed significant ethnic/racial differences in education, family income, and occupational prestige (Table 1 ▶). All of these indicators of socioeconomic status showed White men to be more socially advantaged than Black men. Black respondents also scored significantly higher than White respondents on the measure of social desirability. However, no significant ethnic/racial differences were evident for age, marital status, symptoms of paranoia, or diagnosed mental disorder.
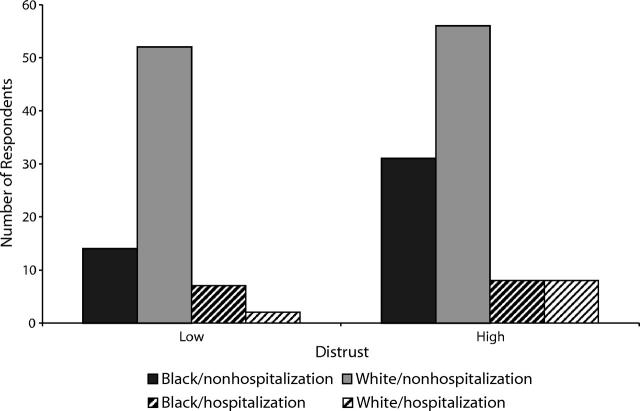
Logistic regression analysis was performed on mental health hospitalization (0 = nonhospitalization, 1 = hospitalization) with ethnicity/race (1 = White, 2 = Black), mild paranoia (0 = low, 1 = high), and the interaction between these 2 variables controlling for sociodemographics, moderate and severe levels of paranoia, a diagnosis of mental disorder, and social desirability. The ethnicity/race–by–mild paranoia interaction tested the hypothesis that Black men exhibiting mild or nonclinical paranoia were more likely than their White counterparts to be hospitalized for mental health problems. The results of the regression analysis are presented in Table 2 ▶. The logit model was statistically significant (−2 log likelihood = 77.77; χ213 = 55.51; P < .001), with an overall classification accuracy of 91%. We found significant ethnic/racial main effects and ethnicity/race–by–mild paranoia interactions. Black men were more than 49 times more likely than White men to have had a mental health hospitalization. The ethnicity/race–by–mild paranoia interaction is depicted in Figure 1 ▶. Black men with high levels of mild paranoia were less likely to be hospitalized. Married men were significantly less likely to be hospitalized than never-married men. There was also a greater risk of mental health hospitalization among men with diagnosed mental disorders.
TABLE 2—
Results of Logistic Regression Analysis of Mental Health Hospitalization
| Predictor | β (SE) | Odds Ratio (95% Confidence Interval) |
| Ethnicity | 3.91** (1.51) | 49.69 (2.60, 950.62) |
| Mild paranoia (distrust) | 0.97 (1.27) | 2.63 (0.22, 31.52) |
| Ethnicity × mild paranoia | −3.64* (1.62) | 0.03 (0.00, .63) |
| Age | 0.03 (0.03) | 1.03 (0.97, 1.10) |
| Marital status | ||
| Never married | 0 | |
| Divorced | 0.15 (0.78) | 1.16 (0.25, 5.32) |
| Married | −2.18* (0.97) | 0.11 (0.02, 0.75) |
| Education | ||
| Less than high school graduate | 0 | |
| High school graduate | −0.33 (0.85) | 0.72 (0.14, 3.81) |
| College graduate | −0.83 (1.20) | 0.44 (0.04, 4.59) |
| Family income, $ | ||
| 0–6999 | 0 | |
| 7000–14 999 | −0.37 (0.81) | 0.69 (0.14, 3.41) |
| 15 000–24 999 | −0.54 (0.94) | 0.58 (0.09, 3.68) |
| 25 000–50 000 | −1.02 (1.36) | 0.36 (0.03, 5.21) |
| Occupational prestige | −0.02 (0.03) | 0.98 (0.93, 1.03) |
| Diagnosis of mental disorder | 2.30** (0.73) | 9.95 (2.37, 41.83) |
| Moderate paranoia (perceived hostility of others) | −94 (0.88) | 0.39 (0.07, 2.19) |
| Severe paranoia (false beliefs and perceptions) | 2.14 (1.15) | 8.47 (0.89, 80.92) |
| Social desirability | −0.92 (1.81) | 0.40 (0.01, 13.69) |
| Constant | −5.35 (2.60) | 0.01 |
Note. Each subcategory with a zero in the β column is the reference category for a given variable.
*P < .05; **P < .01.
FIGURE 1—
Number of respondents by ethnicity/race, hospitalization status, and level of distrust.
DISCUSSION
This study tested the hypothesis that Black men with high levels of mild or nonclinical paranoia were more likely to be hospitalized than their White counterparts for mental health problems. Our findings did not support this hypothesis. Two possible explanations can be offered for this result. First, mental health gatekeepers may not recommend hospitalization for mildly symptomatic Black men as frequently as they do for mildly symptomatic White men. However, this interpretation is at odds with the fact that ethnicity/race increased the chance of mental health hospitalization for Black men independent of demographic and clinical variables. In addition, there is a body of literature indicating a greater risk for hospitalization among Blacks relative to Whites3,4,17,18
Second, Black men with high levels of distrust or mild paranoia may be less likely to seek help for mental health problems. Consequently, a lower number of Black men would be available for hospitalization. In a community study of ethnic/racial differences in treatment seeking for depression, Sussman, Robins, and Earls19 found that Black respondents tended to delay treatment for a much longer period than did White respondents. Some reasons given by Black respondents were distrust of treatment and fear of hospitalization. A more recent meta-analytic study revealed a link between cultural mistrust and lack of mental health service utilization among Blacks.20 Both interpersonal distrust and cultural mistrust are forms of nonclinical paranoia that are positively correlated.12 Black males’ apprehension about seeking mental health services is understandable, given the finding that they are significantly more likely to be hospitalized for mental health problems irrespective of their level of psychopathology or diagnosed mental disorder.
These findings have implications for the mental health treatment of Black men. Ethnic/racial differences in the hospitalization of men independent of serious mental illness may reflect biases in clinical judgments about Black men. Violent behavior is a key symptom in the decision to hospitalize an individual for mental health problems. Black men are stereotyped as more violent than any other race–gender group in the perceptions both of the public and of mental health providers.3–5,21,22 Training programs must address the cultural biases and racial stereotypes that mental health professionals have toward Blacks in general, and toward Black men in particular. Black men’s lack of trust in the mental health system is another concern that deserves attention. The issue of trust is also likely to be an important topic of discussion early in the mental health treatment of many Black men.20,23 Critical factors to increasing their trust are, first, acknowledgment of racial biases in the mental health system and, second, sincere efforts to eliminate racial disparities in mental health treatment.
Acknowledgments
The research project upon which this study is based was supported by a Young Investigator Award (1993-1995) from the National Alliance for Research on Schizophrenia and Depression and NIMH grant 1 R01 MH55561-01A1 to the author.
Human Participant Protection The research project upon which this study is based was approved by the New York State Psychiatric Institute.
Peer Reviewed
References
- 1.Mukherjee S, Shukla S, Woodle J, Rosen AM, Olarte S. Misdiagnosis of schizophrenia in bipolar patients: a multiethnic comparison. Am J Psychiatry. 1983;140:1571–1574. [DOI] [PubMed] [Google Scholar]
- 2.Strakowski SM, Shelton RC, Kolbrener ML. The effects of race and comorbidity on clinical diagnosis in patients with psychosis. J Clin Psychiatry. 1993;54:96–102. [PubMed] [Google Scholar]
- 3.Loring M, Powell B. Gender, race, and DSM-III: A study of the objectivity of psychiatric diagnostic behavior. J Health Soc Behav. 1988;29:1–22. [PubMed] [Google Scholar]
- 4.Rosenfield S. Race differences in hospitalization: psychiatric versus labeling perspectives. J Health Soc Behav. 1984;25:14–23. [PubMed] [Google Scholar]
- 5.Abreu JM. Conscious and nonconscious Black stereotypes: impact on first impression and diagnostic ratings by therapists. J Consult Clin Psychol. 1999;67:387–393. [DOI] [PubMed] [Google Scholar]
- 6.Garyali V. “The color of suspicion”: race profiling or racism? J Am Acad Psychiatry Law. 1999;27:630–632. [PubMed] [Google Scholar]
- 7.Terrell F, Terrell SL. An inventory to measure cultural mistrust among blacks. West J Black Stud. 1981;5:180–184. [Google Scholar]
- 8.Ridley CR. Clinical treatment of the nondisclosing black client: a therapeutic paradox. Am Psychol. 1984;39:1234–1244. [DOI] [PubMed] [Google Scholar]
- 9.Fenigstein A, Vanable PA. Paranoia and self-consciousness. J Pers Soc Psychol. 1992;62:129–138. [DOI] [PubMed] [Google Scholar]
- 10.Zigler E, Glick M. Is paranoid schizophrenia really camouflaged depression? Am Psychol. 1988;43:284–290. [DOI] [PubMed] [Google Scholar]
- 11.Whaley AL. Ethnicity/race, paranoia, and psychiatric diagnoses: clinician bias versus sociocultural differences. J Psychopathol Behav Assess. 1997;19:1–20. [Google Scholar]
- 12.Whaley AL. Psychometric analysis of the cultural mistrust inventory with a black psychiatric inpatient sample. J Clin Psychol. 2002;58:383–396. [DOI] [PubMed] [Google Scholar]
- 13.Dohrenwend BP, Shrout P, Link BG, Martin JL, Skodol AE. Overview and initial results from a risk-factor study of depression and schizophrenia. In: Barrett J, Rose RM, eds. Mental Disorders in the Community. New York, NY: Guilford; 1986:184–215.
- 14.Dohrenwend BP, Shrout P, Egri G, Mendelsohn FS. Measures of nonspecific psychological distress and other dimensions of psychopathology in the general population. Arch Gen Psychiatry. 1980;37:1229–1236. [DOI] [PubMed] [Google Scholar]
- 15.Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Clin Psychol. 1960;24:349–354. [DOI] [PubMed] [Google Scholar]
- 16.Skodol AE, Williams JBW, Spitzer RL, Gibbon M, Kass F. Identifying common errors in the use of DSM III through diagnostic supervision. Hosp Community Psychiatry. 1984;35:251–255. [DOI] [PubMed] [Google Scholar]
- 17.Lindsey KP, Paul GL. Involuntary commitments to public mental institutions: issues involving the overrepresentation of blacks and assessment of relevant functioning. Psychol Bull. 1989;106:171–183. [DOI] [PubMed] [Google Scholar]
- 18.Snowden LR, Cheung FK. Use of inpatient mental health services by members of ethnic minority groups. Am Psychol. 1990;45:347–355. [DOI] [PubMed] [Google Scholar]
- 19.Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Soc Sci Med. 1987;24:187–196. [DOI] [PubMed] [Google Scholar]
- 20.Whaley AL. Cultural mistrust and mental health services for African Americans: a review and meta-analysis. Counseling Psychol. 2001;29:513–531. [Google Scholar]
- 21.Whaley AL. Racism in the provision of mental health services: a social-cognitive analysis. Am J Orthopsychiatry. 1998;68:47–57. [DOI] [PubMed] [Google Scholar]
- 22.Whaley AL, Link BG. Racial categorization and stereotype-based judgments about homeless people. J Appl Soc Psychol. 1998;28:189–205. [Google Scholar]
- 23.Whaley AL. Cultural mistrust: an important psychological construct for diagnosis and treatment of African Americans. Professional Psychol. 2001;32:555–562. [Google Scholar]