Abstract
Objectives. We examined the prevalence of psychiatric illness among 3 homeless populations in St. Louis, Mo, in approximately 1980, 1990, and 2000. The 3 studies were conducted with the same systemic research methodology.
Methods. We compared selected demographics and lifetime substance abuse and dependence and other mental illness among the 3 populations.
Results. Among the homeless populations we studied, the prevalence of mood and substance use disorders dramatically increased, and the number of minorities within these populations has increased.
Conclusions. The prevalence of psychiatric illness, including substance abuse and dependence, is not static in the homeless population. Service systems need to be aware of potential prevalence changes and the impact of these changes on service needs.
Addressing the public health concerns of the homeless population is a major challenge for service providers and policymakers. This population suffers from multiple risk factors, including disproportionately high rates of mental illness and substance use and abuse. Understanding the risk factors and their changing roles is essential for the development of effective policies and programs that address these concerns.
Comparing homeless populations across studies and over time has been impeded by methodological difficulties,1,2 including inconsistent definitions of homelessness, varied sampling strategies and locations, and disparate measurement instruments. Differences in population prevalence estimates of homelessness vary by tens of millions because of sampling: low estimates are generated from samples of current homeless-shelter users only (current prevalence, literal homelessness),3 and high estimates are generated from samples of individuals with any lifetime episode of unstable housing (lifetime prevalence, marginal housing).4
This situation complicates efforts to weigh risk factors for homelessness, such as mental illness or substance abuse, across populations and over time. Despite controls for sampling variation, only questionable reliability has emerged in comparisons of standardized and clinician-based estimates of risk.5 Reasonably reliable cross-sectional prevalence estimates and risk factors have emerged from adequately designed population studies over the last decade,2,6–16 but the effects of time have not been adequately tested in these studies. The homeless population is always described at a discrete time point, which conceptualizes homelessness as a static phenomenon. Changes in the demographics of the homeless population over time may have critical implications for service and public health policy implementation.
Housing and labor markets,17–21 erosion of public benefits,21 and deinstitutionalization19,21,22 all have been identified as risk factors for homelessness. Changes in these forces over time may shape the evolving complexion of the homeless population and may contribute to the level of mental illness or substance abuse within it. A substantial body of research has shown that economics and federal and state policies powerfully affect risks for homelessness.23
Longitudinal data on the homeless population are generally unavailable. Therefore, the evolving dynamics of this population’s demographics are most readily examined by comparing available data from different time periods. Although longitudinal studies represent the gold standard for examining changes in prevalence of risk factors in the homeless population, separate studies that employ similar sampling methods and instrumentation conducted at different times offer an alternative approach. This rationale forms the basis of our study, which capitalizes on population data from 3 studies conducted in St Louis, Mo, at 3 different time points approximately a decade apart. These 3 studies utilized the same methodology with systematic sampling and structured psychiatric interviews, which yielded full psychiatric diagnoses that met American Psychiatric Association (APA) criteria. The purpose of our study is to compare selected demographics and relative prevalence of lifetime psychiatric and substance abuse and dependence diagnoses among 3 homeless populations that were systematically assessed by structured interviews in approximately 1980, 1990, and 2000.
METHODS
Sampling
Two of the data sets for our analyses are products of homeless-population studies conducted a decade apart in St Louis. The first of the 2 data sets was collected between April 1989 and September 1991 as part of an epidemiological study (referred to as the 1990 study in this report). A more recent data set includes 396 index interviews conducted between October 1999 and May 2001 as part of a longitudinal study of service utilization and substance abuse in the homeless population (referred to as the 2000 study in this report). Both studies, conducted in the same parts of the city of St Louis by the same research team, used the same sampling process, with the exception of sampling differences regarding gender. The 1990 data set consists of 2 samples recruited separately by gender with a preplanned ratio of 600 men to 300 women. The 2000 study recruited men and women randomly to reflect their numbers among shelter users and homeless people from public areas in the greater pool of the available population. Statistical sampling methods were used to select these men and women.
The 2 studies recruited participants randomly from all overnight and daytime shelters located in the city of St Louis that serve the homeless in numbers proportionate to the size of each shelter’s roster, as well as from locations on systematically searched streets and other public areas where homeless people are known to congregate. In both studies, individuals were considered homeless if they had no stable residence and were living in a public shelter or in an unsheltered location without a personal mailing address, such as on the streets, in a car, in an abandoned building, or in a bus station. Individuals who resided in inexpensive hotels for less than 30 days also were included. Marginally housed persons, such as those living with friends or relatives or those living in single-room-occupancy facilities, were not included. Fourteen consecutive days of literal homelessness were required for inclusion in the 2000 study.
A third data set included in our comparative analysis consists of data extracted from the St Louis site’s first wave of the National Institute of Mental Health (NIMH)–sponsored Epidemiologic Catchment Area (ECA) study, which was collected between April 1981 and March 1982 (referred to as the 1980 ECA study in this report). ECA subjects were selected from 2 regions of the St Louis area: the city itself and a section of northeastern St Louis County that borders on the city of St Louis. These regions were selected for their economic similarity to the area from which the homeless data were collected. The excluded region was a 3-county area of suburban communities, small towns, and rural areas in St Charles, Lincoln, and Warren Counties.24 Not included in the ECA subsample were those who were institutionalized, such as in nursing homes, board and care homes or boarding homes, prison or jail, mental retardation facilities, mental hospitals, chronic hospitals, and residential treatment centers.
Individuals were considered to have a lifetime history of homelessness if they responded affirmatively to either of 2 questions from the antisocial personality disorder section of the Diagnostic Interview Schedule: (1) “Have you ever traveled around for a month or more without having any arrangements ahead of time and not knowing how long you were going to stay or where you were going to work?” and (2) “Has there ever been a period when you had no regular place to live for at least a month or so?” From the St Louis ECA data set of 828 men and 1395 women, 69 men and 81 women provided an affirmative response to at least 1 of these 2 questions and identified an episode approximating homelessness at some time in their lives. The 1980 ECA study differs from the other 2 studies in its definition of homelessness (lifetime in the 1980 ECA study vs current episode of homelessness in the other 2 studies) and a sample not identified on the basis of current homelessness (although individuals included were subselected for our study’s analyses by history of homelessness).
Nearly 7% of the 1980 ECA study sample met our study’s working definition of homelessness, and more ECA men (9.8%) than women (5.0%) had been homeless (χ2 = 19.31, df = 1, P ≤ 0.001). Multiple linear regression analysis that used gender as a covariate independent variable revealed that those with a history of homelessness were younger than the rest of the study population (45.6 (SD = 46.4) versus 32.5 (SD = 24.9); β = −10.62, t = 6.43, df = 2220, P = .001).
Instruments
Trained interviewers used the Diagnostic Interview Schedule (DIS) to obtain psychiatric diagnoses in all 3 studies. The 1980 ECA study used the DIS in Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III)24; the 1990 study used the DIS in the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition (DSM-III-R)25; and the 2000 study used the DIS in the Diagnostic and Statistical Manual of Mental Orders, Fourth Edition (DSM-IV)26. The first 2 studies used the DIS to diagnose substance use disorders; the 2000 study used the Composite International Diagnostic Interview/Substance Abuse Module (CIDI/SAM).
Data Analysis
We used SAS software (SAS Institute Inc, Cary, NC) to perform data analyses. The 1980 ECA study data set oversampled African Americans and the elderly, which was corrected by weighting to estimate population prevalence.27 The same weighting procedure was applied to our analyses of the 1980 ECA study data set. Findings from all 3 data sets are presented separately by gender, because 1 of the 3 samples (the 1990 sample) was not collected randomly by gender (that predetermined numbers of 600 men and 300 women) and thus does not permit comparisons over time by gender. For comparisons of both numeric and categorical variables to manage the noninteger values generated by the weighting procedure, weighted means and standard errors were generated with PROC SURVEYMEANS in the SAS software. We computed z scores of the differences among groups by dividing the difference in the calculated weighted means by the square root of the sum of the squares of the standard errors.
RESULTS
Demographics
Table 1 ▶ shows detailed demographics for men and women separately. With 1 exception (“other” females), the proportion of minorities had increased by 1990, and these levels were maintained over the next decade. The 2000 study shows an increase in the mean ages of both men and women. Never-married status of men increased to about 50% by 1990 and remained at that level over the next decade. By 2000, the ranks of men in the lowest education category had increased relative to previous decades. The proportion of employed men and women had decreased by 1990 and then increased to partly regain previous levels by 2000.
TABLE 1—
Homeless-Population Demographics, by Decade and Gender: St Louis, Mo: 1980, 1990, and 2000
| Males | Females | |||||
| 1980 ECA Study (n = 81) | 1990 Study (n = 600) | 2000 Study (n = 298) | 1980 ECA Study (n = 69) | 1990 Study (n = 300) | 2000 Study (n = 98) | |
| Race | ||||||
| Non-Hispanic Black | 26.0 | 69.8*** | 71.1*** | 30.5 | 84.0*** | 81.4*** |
| Non-Hispanic White | 72.1 | 27.5*** | 20.1***a | 63.2 | 12.0*** | 14.4*** |
| Other | 2.0 | 2.7 | 8.7**c | 6.3 | 4.0 | 4.1 |
| Age, y | ||||||
| 18–24 | 14.6 | 11.8 | 3.4**c | 43.6 | 32.4 | 26.5**c |
| 25–44 | 52.1 | 69.8* | 51.7c | 43.4 | 62.9* | 55.1 |
| 45–64 | 22.5 | 16.7 | 44.0**b | 9.0 | 4.0 | 17.4c |
| ≥ 65 | 10.8 | 1.7 | 1.0* | 4.0 | 0.7 | 1.0 |
| Mean years | 39.7 | 35.9 | 43.1b | 31.1 | 29.0 | 34.5c |
| Standard deviation | 18.1 | 10.8 | 9.3 | 13.9 | 8.6 | 11.0 |
| Median years | 33 | 34 | 43 | 26 | 27 | 35 |
| Marital status | ||||||
| Married | 35.0 | 4.2*** | 5.4*** | 27.2 | 7.0* | 6.1* |
| Widowed | 8.8 | 2.5 | 3.0 | 6.3 | 2.7 | 7.1 |
| Separated | 8.1 | 16.8** | 14.1 | 8.7 | 20.0** | 12.2 |
| Divorced | 17.6 | 22.0 | 25.8 | 14.2 | 10.0 | 13.3 |
| Never married | 30.7 | 54.5*** | 51.7** | 43.7a | 60.3 | 61.2 |
| Education | ||||||
| High school diploma or GED | 63.1 | 57.3 | 75.4c | 64.0 | 49.7 | 57.7 |
| Mean years | 12.1 | 11.7 | 12.0 | 11.5 | 11.4 | 11.5 |
| Standard deviation | 3.1 | 2.4 | 2.3 | 2.3 | 1.8 | 2.1 |
| Median years | 12 | 12 | 12 | 12 | 12 | 12 |
| Current full-time employment | 50.3 | 10.7*** | 24.7***c | 19.3 | 6.6* | 16.5a |
Note. Compared with the 1980 Epidemiologic Catchment Area study, *P ≤ .05, **P ≤ .01, and ***P ≤ .001; compared with the 1990 study, aP ≤ .05, bP ≤ .01, and cP ≤ .001.
Psychiatric Disorders
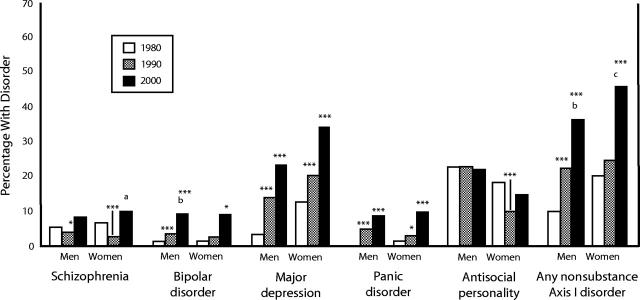
Figures 1 ▶ and 2 ▶ show lifetime prevalence rates of psychiatric disorders by gender for each of the 3 studies. Over the past 2 decades, the prevalence of schizophrenia changed very little among both men and women. Bipolar disorder, major depression, and panic disorder generally increased over the 2 decades, but antisocial personality disorder did not change appreciably. Overall, nonsubstance Axis I disorders (DSM-IV) increased among both men and women over the past 2 decades, and major depression accounted for the majority of these disorders at all 3 assessment points.
FIGURE 1—
Lifetime prevalence rates of psychiatric disorders, by cohort and gender.
Note. Compared with the 1980 Epidemiologic Catchment Area study, *P ≤ .05, **P ≤ .01, ***P ≤ .001; compared with the 1990 study, aP ≤ .05, bP ≤ .01, cP ≤ .001.
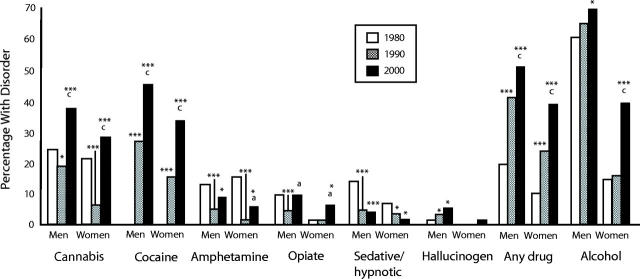
FIGURE 2—
Lifetime prevalence of specific substance abuse/dependence diagnoses, by cohort and gender.
Note. Compared with the 1980 Epidemiologic Catchment Area study, *P ≤ .05, **P ≤ .01, ***P ≤ .001; compared with the 1990 study, aP ≤ .05, bP ≤ .01, cP ≤ .001.
Alcohol use disorder was already highly prevalent among homeless men in 1980, and it increased little over the next 2 decades. Among women, alcohol use disorder was comparatively much less prevalent but was increasing more substantially over the 2 decades of evaluation. The prevalence of drug use disorder increased dramatically among both men and women over the past 2 decades, and among women, the increase was higher than the prevalence of alcohol use disorder. In 2000, 84% of men and 58% of women had an alcohol or other drug use disorder. Also in 2000, substance use disorders accounted for the vast majority of psychopathology (prevalence of any psychiatric disorder was 88% among men and 69% among women). In 1980, the abused drug of choice was cannabis, but it was surpassed over the next 2 decades by cocaine, which had not been found among homeless men or women in 1980. The popularity of amphetamine and sedative-hypnotic abuse decreased after 1980. Opioid abuse remained relatively unchanged over the 2 decades and was the third most prevalent abused drug of choice in 2000.
A few changes were evident in ages of onset of disorders. Among men, age of onset of bipolar disorder increased substantially, especially after 1990. The age of onset of bipolar disorder among men increased to near the age of onset of cocaine use disorder, which is consistent with the often comorbid occurrence of bipolar disorder with cocaine use disorder among men (38% of cases in 1990 and 54% in 2000). Major depression also increased among men relative to 1980, whereas age of onset of alcohol and drug use disorders (and specifically cannabis) declined. Among women, age of onset of schizophrenia decreased and age of cocaine use disorder increased relative to 1980.
DISCUSSION
Trends Over Time
These 3 data sets suggest an evolution of the characteristics of the homeless population in St Louis over 2 decades. There are more minorities in the homeless population. Mood and substance use disorders have dramatically increased, especially drug use disorders (predominantly cocaine) among women. Major depression is the main diagnosis in the nonsubstance diagnosis category, and substance use disorders, especially alcohol, represent the vast majority of all disorders. Cocaine abuse was not evident in 1980, when the abused drug of choice was cannabis, but by 1990, it had established itself as the abused drug of choice and retained this distinction in 2000.
Methodological Limitations
Our examination of the 3 homeless-population data sets, which were collected in the same place with the same assessment tool at 3 different times, has substantial limitations. The question of whether the apparent changes observed in the St Louis homeless population represent national trends remains open and is a central limitation of our study. However, inferential evidence (similarities in prevalence rates found in St Louis and those found elsewhere) suggests that specific differences found in St Louis may prove informative to providers elsewhere.
The 1980 ECA study was a community sample collected for other purposes that happened to contain people with a history of homelessness that we retrospectively approximated. The 1980 and 1990 studies used essentially identical sampling methods, although the 1990 sample had an arbitrary male to female ratio of 2 to 1 that compromised our ability to examine gender differences. The inherent nonuniformity of sampling prohibits the ability to draw strictly straight-line inferences from the data. Because the lifetime (not current) definition of homelessness in the 1980 ECA study called for analysis of lifetime rather than current psychiatric diagnosis, examination of the impact of recent symptoms on current homelessness was not possible. In the other 2 studies, entry into homelessness generally occurred more than 1 year prior to interview, which reduced the relevance of current symptoms to the prevalence focus of the research question.
The criteria used for psychiatric diagnoses have evolved somewhat over time (from DSM-III to DSM-III-R to DSM-IV). The higher prevalence of several disorders identified with DSM-IV criteria in the 2000 study is especially noteworthy, because that diagnostic prevalence with DSM-IV has been found to be nearly 20% less than with DSM-III-R.29
Directional causality of relationships between mental illness and homelessness cannot be determined with the data available; therefore, the results cannot directly inform the debate on the degree to which mental illness may lead to homelessness and the degree to which homelessness may precipitate further mental illness. The findings from our study should spur additional research to further address these questions and to inform policy discussions.
Implications for Service Delivery
The results of our study discount a static understanding of the homeless population. Therefore, to be responsive to this population, providers must attend to its changing needs. Service networks and community responses that are based on outdated prevalence estimates run a substantial risk of providing services that are not appropriate for current service needs. Our findings reinforce a generally recognized appreciation of the central role of substance abuse within mental health issues in the homeless population, which again suggests the need for more attention within the package of homelessness services for assessing and treating substance abuse and dependence. These analyses suggest that this may be especially true for women whose prevalence of substance abuse has increased across all diagnostic categories. In particular, cocaine use disorders among men and women, and alcohol abuse among women, deserve greater intervention.
Because of the increase in major depression, mental health services should build upon rather than displace the current attention to services for psychiatric illnesses, such as schizophrenia. Because a portion of the major depression in the homeless population may represent confounding with aspects of the homeless condition (with a demonstrated link between exposure to the elements and the likelihood of this disorder),5 it also is possible that a portion of the increase in bipolar disorder may be confounded with the precipitous increase in cocaine abuse/dependence (on the basis of its frequent overlap among the same individuals) and the increase in age of onset of cocaine abuse/dependence. More research is needed to further explore these possibilities.
Shifts in social policies may inadvertently contribute to the changing complexion of the homeless population’s demographics with regard to race, substance abuse and dependence, and other mental illness.19–21 For populations dealing with substance abuse and dependence, increased risk for homelessness might be an unintended end product of social policies aimed at alleviating poverty. It has been repeatedly argued that US policy on deinstitutionalization has contributed to the overall prevalence of mental illness in the homeless population.30–34 Testing causality would require minimally longitudinal methods and a nonhomeless poverty comparison group that are not provided in the data for our report. Further research is needed to determine the degree to which social policy modifies the risk for homelessness through these various factors. In the meantime, policymakers are advised to be vigilant for negative effects of policy change on specific subpopulations.
Future Research Directions
Results from our study clearly point to several directions for future research. Replication of previous prevalence studies is needed in other urban environments, and these studies should use similar methods for assessing adequacy of service needs for each environment. Of course, longitudinal study of sufficient duration, including a comparison group, is most ideal for direct testing of changes in prevalence of psychiatric disorders within the homeless population over time. Finally, the potential impact of specific social policy on both prevalence of homelessness and its demographics might be studied through the prospective observation of initial entry into homelessness among samples at high risk for homelessness. Although a host of policies may provide material for such research, the policy of lifetime limits on welfare benefits is an ideal candidate for studying direct impact on homelessness.
CONCLUSIONS
The findings of our study, although inconclusive because of methodological limitations, suggest that prevalence of mental illness and substance abuse and dependence is not static over time in the homeless population. Furthermore, changes are not monolithic, but they particularly apply to certain diagnoses and descriptive characteristics. Service systems need to be cognizant of the potential for prevalence changes and how these changes translate into evolving service needs. Building on these findings, our study speculates that social and economic policies may contribute to differential risks for homelessness among minorities as well as among those with addiction or major depression.
TABLE 2—
Age of Onset of Psychiatric Disorders Among Homeless Populations, by Decade and Gender: St Louis, Mo: 1980, 1990, and 2000
| Males | Females | |||||
| Mean age of onset, SD | 1980 (n = 81) | 1990 (n = 600) | 2000 (n = 298) | 1980 (n = 69) | 1990 (n = 300) | 2000 (n = 98) |
| Schizophrenia | 19.5 (99.4) | 20.8 (9.3) | 23.1 (11.7) | 28.3 (35.3) | 16.4 (9.5)*** | 18.9 (11.8)** |
| Bipolar disorder | 18.0 (. . .) | 21.0 (7.5)* | 27.3 (12.1)***c | 19.1 (25.0) | 18.6 (4.1) | 22.9 (7.7) |
| Major depression | 20.5 (41.0) | 27.0 (8.9)* | 27.5 (11.4)* | 15.3 (48.0) | 23.5 (8.5)*** | 20.0 (9.8) |
| Panic disorder | . . . (. . .) | 23.9 (11.4) | 26.8 (12.9) | 14.4 (42.1) | 20.6 (14.0) | 21.5 (10.9) |
| Any nonsubstance Axis I disorder | 22.4 (88.8) | 24.3 (9.8) | 23.8 (12.1) | 19.7 (60.5) | 22.3 (9.5) | 18.3 (10.5)a |
| Antisocial personality disorder | 19.2 (7.6) | 21.0 (9.1) | 21.2 (7.6) | 20.7 (9.2) | ||
| Alcohol use disorder | 21.6 (53.5) | 20.0 (7.0) | 19.3 (6.7)* | 18.5 (19.4) | 19.6 (4.9)* | 19.9 (9.7) |
| Amphetamine use disorder | 21.6 (5.5) | 19.1 (5.0) | 24.0 (7.0) | 19.8 (2.4) | ||
| Cannabis use disorder | 20.1 (6.4) | 17.1 (5.4)a | 21.2 (6.1) | 17.8 (7.5) | ||
| Cocaine use disorder | 27.9 (7.0) | 28.7 (7.9) | 24.5 (5.6) | 28.4 (8.9)a | ||
| Hallucinogen use disorder | 18.4 (5.7) | 25.0 (21.4) | 18.0 (. . .) | 17.0 (. . .) | ||
| Opioid use disorder | 21.7 (6.2) | 24.4 (16.0) | 22.8 (6.5) | 22.1 (8.1) | ||
| Sedative use disorder | 22.6 (5.5) | 20.7 (7.0) | 9.5 (5.1) | 14.0 (. . .) | ||
| Any drug use disorder | 18.5 (37.7) | 23.1 (7.4)*** | 21.8 (10.1)* | 18.6 (35.9) | 22.3 (5.3) | 21.0 (8.6) |
Note. Compared with the 1980 Epidemiologic Catchment Area study, *P ≤ .05, **P ≤ .01, and ***P ≤ .001; compared with the 1990 study, aP ≤ .05, bP ≤ .01, and cP ≤ .001.
Acknowledgments
This paper was supported by grant R01–DA–10713 from the National Institute on Drug Abuse. An earlier version of these results was presented at the 2001 American Public Health Association Annual Meeting in Atlanta, Ga.
Human Participant Protection All 3 of these studies met the Washington University Human Studies Committee requirements prior to their inception.
Contributors C. S. North and D. E. Pollio designed and received funding for the study, gathered data, directed the data analysis, and collaborated in writing the article. K. M. Eyrich performed data analysis and assisted with writing the article. E. L. Spitznagel assisted with the study design, advised the analysis of the data, and assisted with writing the article.
Peer Reviewed
References
- 1.Rossi PH, Wright JD, Fisher GA, et al. The urban homeless: estimating composition and size. Science. 1987;235:1336–1341. [DOI] [PubMed] [Google Scholar]
- 2.Susser E, Conover S, Struening EL. Problems of epidemiologic method in assessing the type and extent of mental illness among homeless adults. Hosp Comm Psychiatry. 1989;40:261–265. [DOI] [PubMed] [Google Scholar]
- 3.US Dept of Housing and Urban Development. A Report to the Secretary on the Homeless and Emergency Shelters. Washington, DC: Office of Policy Development and Research; 1984.
- 4.Link B, Phelan J, Breshnahan M, et al. Lifetime and 5-year prevalence of homelessness in the United States: new evidence on an old debate. Am J Orthopsychiatry. 1995;65:347–354. [DOI] [PubMed] [Google Scholar]
- 5.North CS, Pollio DE, Thompson SJ, et al. A comparison of clinical and structured interview diagnoses in a homeless mental health clinic. Community Ment Health J. 1997;33(6):531–543. [DOI] [PubMed] [Google Scholar]
- 6.Farr RK, Koegel P, Burnam A. A study of homelessness and mental illness in the skid row area of Los Angeles: a report to NIMH. Rockville, Md: National Institute of Mental Health; 1986.
- 7.Sosin MR, Colson P, Grossman S. Homelessness in Chicago: Poverty and Pathology, Social Institutions and Social Change. Chicago, Ill: University of Chicago Press; 1988.
- 8.Koegel P, Burnam MA. Alcoholism among homeless adults in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45:1011–1018. [DOI] [PubMed] [Google Scholar]
- 9.Koegel P, Burnam MA, Farr RK. The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45:1085–1092. [DOI] [PubMed] [Google Scholar]
- 10.Breakey WR, Fischer PJ, Kramer M, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262(10):1352–1357. [PubMed] [Google Scholar]
- 11.US Dept of Housing and Urban Development Interagency Council on the Homeless. The 1989 Annual Report of the Interagency Council on the Homeless. Washington, DC: Government Printing Office; 1989.
- 12.Smith EM, North CS, Spitznagel EL. A systematic study of mental illness, substance abuse, and treatment in 600 homeless men. Ann Clin Psychiatry. 1992;4(2):111–120. [Google Scholar]
- 13.Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805–821. [DOI] [PubMed] [Google Scholar]
- 14.Robertson MJ, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. Am J Public Health. 1997;87:221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sosin MR, Bruni M. Homelessness and vulnerability among adults with and without alcohol problems. Subst Use Misuse. 1997;32:939–968. [DOI] [PubMed] [Google Scholar]
- 16.Susser E, Betne P, Valencia E, et al. Injection drug use among homeless adults with severe mental illness. Am J Public Health. 1997;87:854–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rossi PH, Wright JD. The determinants of homelessness. Health Aff. 1987;6:19–32. [DOI] [PubMed] [Google Scholar]
- 18.McChesney KY. Family homelessness: a systemic problem. J Soc Issues. 1990;46:191–205. [Google Scholar]
- 19.Jencks C. The Homeless. Cambridge, Mass: Harvard University Press; 1994.
- 20.O’Flaherty B. Making Room: The Economics of Homelessness. Cambridge, Mass: Harvard University Press; 1996.
- 21.Blau J. The Visible Poor: Homelessness in the United States. New York, NY: Oxford University Press; 1992.
- 22.Mechanic D. Evolution of mental health services and areas for change. New Dir Ment Health Serv. 1987;36:3–13. [DOI] [PubMed] [Google Scholar]
- 23.Aviram U. Community care of the mentally ill: continuing problems and current issues. Community Ment Health J. 1990;26:69–88. [DOI] [PubMed] [Google Scholar]
- 24.Diagnostic and Statistical Manual of Mental Disorders, Third Edition. Washington, DC: American Psychiatric Association; 1980.
- 25.Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition. Washington, DC: American Psychiatric Association; 1987.
- 26.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC; American Psychiatric Association; 1994.
- 27.Leaf P, Myers JK, McEvoy LT. Procedures used in the Epidemiologic Catchment Area Study. In: Robins LN, Regier DA, ed. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: The Free Press; 1991:11–32.
- 28.Narrow WE, Rae DS, Robins LN, et al. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry. 2002;59:115–123. [DOI] [PubMed] [Google Scholar]
- 29.Bassuk EL, Lamb HR. Homelessness and the implementation of deinstitutionalization. New Dir Ment Health Serv. 1986;30:7–14. [DOI] [PubMed] [Google Scholar]
- 30.Belcher JR. Relationship between the deinstitutionalization model, psychiatric disability, and homelessness. Health Soc Wk. 1988;13:145–153. [DOI] [PubMed] [Google Scholar]
- 31.Durham ML. The impact of deinstitutionalization on the current treatment of the mentally ill. Int J Law Psychiatry. 1989;12:117–131. [DOI] [PubMed] [Google Scholar]
- 32.Belcher JR. Moving into homelessness after psychiatric hospitalization. J Soc Serv Res. 1991;14:63–77. [Google Scholar]
- 33.Bachrach LL. What we know about homelessness among mentally ill persons: an analytical review and commentary. Hosp Comm Psychiatry. 1992;43:453–464. [DOI] [PubMed] [Google Scholar]
- 34.Goldman HH. Deinstitutionalization and community care. Harvard Rev Psychiatry. 1998;6:219–222. [DOI] [PubMed] [Google Scholar]