Abstract
Rural communities in the United States are served by relatively fewer health care professionals than urban or suburban areas.
I review the geographic distribution of 6 classes of health professionals and describe the multiple government and private policies and programs intended to affect their geographic distribution. These programs can be classified into 3 categories—coercive, normative, and utilitarian—that characterize the major policy levers used to influence practice location decisions.
Health workforce policies must be normative to ensure equity for rural communities, but goals in this area can be achieved only through a balance of utilitarian and coercive mechanisms.
THE SALIENT CHARACTERISTIC of the distribution of rural and urban health practitioners is the clustering of practitioners in more urban locales. This situation is most pronounced in the case of specialists, but it applies in many instances to generalists as well. The argument that this constitutes an inequitable distribution of fundamental goods has been described by New-house and colleagues as “conventional wisdom” but also as “generally misguided,” in that it simply reflects rational choices made by practitioners.1 Economists have viewed the relatively unequal distribution of practitioners as resulting from market forces associated with preference and demand.1–3 This argument implies that policies that influence practitioners to locate in less desirable areas are reacting to “market failure.” I describe the rural–urban distribution of selected groups of health professionals and categorize programs that attempt to change these distributions in relation to market orientations.
PHYSICIANS
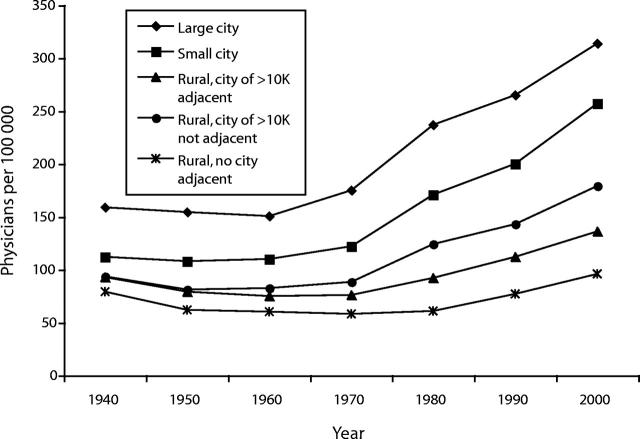
The uneven distribution of medical practitioners began to be observed early in the 20th century,4 and data show that it has persisted and increased over time. Figure 1 ▶ illustrates how the rural–urban gap in the relative national supply of physicians has increased. This trend has been accompanied by a decrease in the percentage of physicians practicing as generalists, from 59% in 1949 to 32% in 2000.5,6 The degree of geographic inequality and its causes vary according to different professions, as well as according to disciplines within professions.
FIGURE 1—
Active physicians per 100 000 population, by year and location (urban or rural).
Physicians are the most cited example of the unequal distribution of practitioners,7 and an increasing trend toward specialization has been listed as a key factor contributing to such inequitable distributions.8 Because they are taught in institutions dominated by specialists, physicians are subject to the pressures of specialization throughout their medical training, and often specialty medicine can be supported only in densely populated areas.9,10 The exception to this trend is among family practitioners (Table 1 ▶). The concentration of specialists in urban areas and a roughly equal geographic distribution of generalists translates to a ratio of physicians to population in the most urban counties 5 times that of the smallest, rural counties. Overall, the ratio of physicians to population in urban counties is 136% higher than that in rural counties. Likewise, the ratio of dentists to urban population is 150% of the rural ratio, and the ratio of hospital-based registered nurses to urban population is 130% of the rural ratio.7
TABLE 1—
Numbers of Physicians per 100 000 Population, by County Type and Specialty
| Specialty | Large Metropolitan (>1 million) | Small Metropolitan (<1 million) | Large Rural City (>10 000) | Small Rural City (<10 000) |
| Family/general practice | 26 | 32 | 30 | 31 |
| General internal medicine | 43 | 29 | 18 | 11 |
| General pediatric medicine | 22 | 15 | 9 | 4 |
| General obstetrics/gynecology | 15 | 12 | 9 | 3 |
| General surgery | 14 | 12 | 10 | 6 |
| All others | 147 | 123 | 69 | 27 |
Note. Data were derived from the Bureau of Health Professions.6
Statistical trends show growth among almost all classes of health professionals practicing in US nonmetropolitan counties. However, this statistic hides a pattern of increases in some communities and attrition of professionals in others. Between 1990 and 2000, 24.7% of non-metropolitan counties lost primary care physicians, compared with 7% of metropolitan counties. Number of physicians per population decreased in 37% of nonmetropolitan counties and in 14.7% of metropolitan counties. There is also substantial variation in the urban–rural distribution of physicians across states; in Nevada, New Hampshire, Montana, and Utah, the ratios of generalists to population are approximately the same in urban and rural areas. In contrast, in Illinois, Louisiana, and New York the ratio of generalists to population in rural counties is only 63% of the urban ratio.7
Primary care practitioners are arguably the key health professionals in most small communities. The federal government identifies areas with shortages, such as these small communities, through its health professional shortage area (HPSA) designation process. A variety of programs and benefits, including placing practitioners via the National Health Services Corps (NHSC), allowing foreign physicians to practice in selected areas by waiving restrictions on entry, and providing Medicare bonus payments, are dependent on HPSA designations.
To be designated for benefits, a community or locality that represents a “rational service area” in regard to primary care must have a ratio of number of citizens to number of active, practicing primary care physicians of greater than 3500:1. Certain “high need” communities that exhibit very high infant mortality rates and slightly lower ratios are also eligible for designation, along with areas where there is restricted access to primary care services as a result of language or cultural barriers. The latter include areas where private practitioners do not accept Medicaid patients and areas with high proportions of Native American residents or other population groups with demonstrated lack of access.
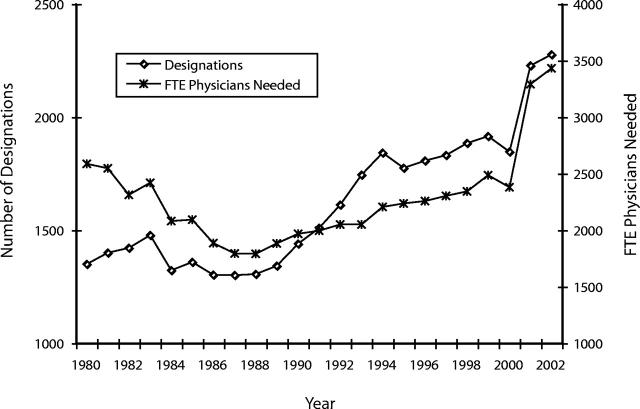
Over the past 20 years, the number of rural areas designated as HPSAs has increased, despite growth in the ratio of practitioners to population in these areas. Figure 2 ▶ traces changes in designations that have taken place since 1980 and the number of full-time-equivalent primary care physicians required to eliminate these designations.11 The changes observed are attributable to increases in the number of areas qualifying in regard to factors other than practitioner ratios and efforts by the federal government to provide technical assistance to communities through the designation process.5 Recent increases are also a function of higher NHSC appropriations and the current administration’s goal of increasing the number of federally qualified health centers supported by Congress through increased appropriations.
FIGURE 2—
Nonmetropolitan primary care health professional shortage area designations, 1980–2001. Note. FTE = full-time equivalent. Data were derived from the Bureau of Health Professions.6
Use of physician assistants to staff rural clinics or provide independent primary care services in rural communities is often mentioned as a way to expand access.12,13 Of 39 000 active physician assistants practicing in the United States in 2000, approximately 18% were located in rural communities, a percentage slightly smaller than that for the overall US population. Selected studies have shown that physician assistants are more likely to practice in areas in which there are shortages of health professionals14 but that recent graduates of physician assistant programs indicate they are less likely to locate in rural communities than their predecessors.7
NURSES
A different set of forces drives markets and policies in the area of nursing. Cyclical changes in the balance of supply and demand for nurses have been tempered by market solutions,15 but the current shortage has been described as more resistant to economic responses and focused on fundamental problems involving the roles of nursing.16 However, any such shortages will be potentially more severe in rural areas; for example, in 2000 there were 213 full-time, active hospital-based nurses per 100 000 rural residents and 281 per 100 000 urban residents.11
Nurse practitioners are nurses with advanced training who are licensed to provide independent primary care. They have long been viewed as a means of increasing access in rural areas because of the lower fees they charge (relative to physicians), their demonstrated effectiveness, and the shorter time between their entry into training and their initiation of practice.12 As a result of variations in state practice laws and reporting requirements, the number of nurse practitioners providing a full scope of primary or advanced nursing care can only be estimated; however, there are probably more than 30 000 nurse practitioners providing primary care. Approximately 20% are located in rural communities, roughly equivalent to the population distribution.
It is difficult to summarize the effective urban–rural distribution of these practitioners; some states restrict the practice of nurse practitioners much more than others. In selected rural states, their contribution to the total volume of primary care is substantial; for example, a study conducted in Washington State showed that 10.3% of all outpatient rural generalist care is provided by nurse practitioners.17
DENTISTS
There is growing acceptance that there is a relative shortage of dentists in rural areas, as well as an emerging general shortage serving certain population groups, especially low-income individuals and those eligible for Medicaid benefits.18 Rural communities have long had shortages, and this situation is likely to worsen given that the total number of practicing dentists is predicted to decline in the coming decades.19 In 1998, rural counties had 29 dentists per 100000 population, as compared with 43 per 100000 in urban counties.7 In the same year, 247 counties did not have a single dentist.
At the end of 2002, there were 2041 dental HPSAs (i.e., areas eligible for placement of NHSC dentists and other program benefits); more than half of these areas were classified as rural. Programs designed to redistribute dentists are less prominent than those for physicians and nurses, but their effectiveness has been shown in the NHSC and in state loan repayment programs.20
PHARMACISTS
Data on the relative distribution of pharmacists in the United States are insufficient,21 but there is evidence of a widespread and growing national shortage of pharmacists.22 As a result of the rapid growth in the number and efficacy of prescription drugs, combined with Medicare drug benefit reforms, access to pharmacists is an important policy issue. Between 1990 and 1999, the number of prescriptions dispensed in ambulatory settings increased by 44%, from 1.9 billion to 2.8 billion. The relatively older age range of rural populations makes them more likely to require prescription drug therapies, while their lower overall incomes and rates of insurance coverage make it more difficult for them to purchase drugs.23 However, a 3-state study of access showed that rurality was less of a factor than socioeconomic status.24
MENTAL HEALTH PROFESSIONALS
In 1997, slightly less than 80% of all nonmetropolitan counties had any type of mental health professional, and 76% of designated mental HPSAs were rural counties.25 Substantial portions of rural mental and behavioral health services are paid for by Medicaid, and tendencies toward more intensive case management in order to contain costs tend to reduce the viability of rural mental health practices.26 The effects of this distributional pattern can be seen in the greater levels of untreated disease in these areas and the subsequent higher use of somatic curative services as well as more intensive psychiatric care.25,27–29
PUBLIC HEALTH PROFESSIONALS
Access to public health services is uneven in rural communities; in rural areas where there are local health departments, these departments are likely to be small, with a median of 12 full-time-equivalent staff, compared with 18 in suburban local public health agencies and 31 in metropolitan areas.30 Rural public health agencies have been shown to report budgets that are less than half those of urban departments or agencies, and a large majority (73%) of rural agencies (compared with 37% of suburban and 26% of urban local public health authorities) serve populations of less than 25 000. Hajat and colleagues30 found that access to training and continuing education were the biggest challenges facing rural public health professionals and suggested that regionalization is 1 way to overcome the inherent obstacles to coverage and staffing in rural communities.
FACTORS IMPEDING AND ENHANCING RURAL PRACTICE
The concentration of training in urban environments is probably the most important factor that drives practitioners away from rural areas.31 The concentration of technology, peers, family, and employment opportunities tends to draw geographically mobile, rural-oriented professionals to urban centers. Their professional careers are subsequently defined by their training experiences in urban locales.32
The structures that encourage and support rural practice are complex and spread across many programs and systems. Thus, health professionals are more vulnerable to urban influences in that no single element can focus their attention on rural needs. Using primary care medicine as an example, the “pipeline” from early education to a rural career passes through a supportive science education environment to a medical school that supports primary care and, finally, to a placement program that matches health professionals to a rural community that must be linked to a system of continuing education and support.
POLICIES AFFECTING GEOGRAPHIC DISTRIBUTIONS
Many government and professional policies have sought to influence health care professionals to practice in rural areas. Indirect policies have attempted to increase the demand for services through social insurance or direct support for caregivers; Medicare and Medicaid are examples of indirect forces acting to redistribute the supply of health professionals. Grants for federally qualified health centers also indirectly influence work-force distributions by generating demand for services. The present focus is on programs that directly influence choice of practice locations independent of demand. These programs can be classified as coercive, normative, or utilitarian in nature. This typology was proposed by Etzioni33 and interpreted in a similar classification of programs intended to recruit and retain physicians (for details, see Crandall et al.34).
In many countries of the world, individuals who undergo medical or health professional training are often required to practice in a less desirable part of their national health system early in their practice.35 This requirement can be viewed as a form of “coercion” or indenture. Programs that exchange required practice in an underserved area for tuition support or loan forgiveness fall into this category. This type of support from the federal government was originally applied to nursing and subsequently became the standard recruiting mechanism for physicians into the NHSC. Selected states had used these incentive mechanisms even earlier.36
The passage of the Emergency Health Personnel Act of 1970, which created the NHSC, signaled a broader federal commitment to support the redistribution of practitioners toward rural and other underserved areas. The NHSC was viewed as both a policy and a practical success, making use of a stimulus that tipped more altruistic practitioners toward rural practice or co-opted physicians with less choice into rural communities. The enthusiasm of the early volunteers and scholarship recipients in the program was tempered by the bureaucratic structure of the NHSC, in which care was not always taken to match practitioners to communities. This top-down approach was at odds with what most often resulted in successful placements: a local, marketlike choice process driven by altruism or economic considerations.37
The NHSC responded with administrative reforms and has been able to demonstrate its effectiveness to Congress and the current administration to the extent that its authorizing legislation has been renewed, and President Bush requested a 32% increase in appropriations in his 2003 budget in order to add 1800 new placements in the coming years.38 The success of these coercive programs in increasing the supply of rural practitioners has been uneven,39 with fairly clear indications that scholarship programs are less effective than loan repayment programs.40
Support for international medical graduates may be seen as another direct and essentially coercive mechanism to influence the supply of rural practitioners. Programs that allow international medical graduates to practice in underserved areas have been in place for decades, and there have been specific rural-focused pathways through which these individuals can receive visas allowing them to enter the United States and practice medicine. Examples are the “Conrad State-20” program and various programs sponsored by the Appalachian Regional Commission and the Delta Regional Authority. The Conrad program was expanded in 2003 to allow 30 foreign-born practitioners per state to practice. In the wake of September 11, 2001, this and other visa waiver placement programs were centralized within the Department of Health and Human Services, removing them from agencies, such as the Department of Agriculture and the Appalachian Regional Commission, with more connections to rural communities.41 The latter change may not disproportionately affect the supply of rural physicians; international medical graduates now represent 24% of all practicing physicians, but their distribution does not significantly favor under-served rural areas.42 Normative programs attempt to match the inclinations and backgrounds of potential, and sometimes practicing, health care professionals with the communities and populations they are being encouraged to serve. These incentives are found in federal support offered to state offices of rural health, health career opportunity programs, area health education centers, rural interdisciplinary team training programs, and health education and training centers. These programs often attempt to influence individuals who are either in the “pipeline” (training for a career as a health professional) or entering the workforce to enter a generalist field and to complete part of their training in rural communities, which will familiarize them with the realities of rural life and practice.43,44
Often, programs attempt to recruit individuals with rural backgrounds.32,45 For example, the Quentin Burdick Rural Interdisciplinary Team Training Program represents a unique combination of place-based familiarization and work-structure-focused training. This grant program requires individuals from a combination of health professions to work together as they train to practice in rural, under-served areas.46,47 The advantages of this approach have been promoted in various policy initiatives, but beneficial effects on either recruitment and retention or outcomes have not been clearly demonstrated.
Utilitarian models are those that support practice elements or the conditions of practice for practitioners within particular market structures. The largest program of this type is Area Health Education Centers (AHEC), which supports state or regional community-based training and continuing education systems for practitioners in rural and underserved communities. In reality, the AHEC program conducts activities reaching well beyond utilitarian education, including providing science education support and orientation for minority students, offering a normative program intended to reduce inequities in the workforce, and supporting NHSC and other indentured practitioners.
AHEC directly funds 46 programs linking health sciences schools with community-based centers and projects. Each year the program contributes to the training of more than 17 000 medical students and residents and 15 000 students in other areas of health care. More than 330 000 individuals receive continuing education either in an AHEC or via some form of distance learning. This extension of the academic health center into the community, along with the melding of the multiple types of programs, perhaps represents a model for how health professional education should be organized; yet, federal appropriations for AHECs have been eliminated by the George W. Bush administration in the past 3 budgets.
Utilitarian approaches also include forms of expert support for rural practitioners often provided by state offices of rural health, all of which have federal grant support. These offices actively identify rural practice locations and recruit practitioners from all disciplines. Some of these offices include the services of experts who provide financial advice, planners who assist in the development of new or expanded practices, and even architects who help design and build new facilities.
POLICY EFFECTS
The activism of workforce policymakers during the past decade is reflected in the multiple programs intended to improve the supply, distribution, and diversity of the health care workforce. One central symbol around which much of this policy activity is focused—primary care—is slowly losing its power as a policy force.48,49 In addition, despite some specific examples of success in recruiting and retaining practitioners in areas where they were formerly absent,46 there is no overall sense that distributional problems have been solved. Federal policy in support of the training and redistribution of health professionals has, over time, been ambivalent.50 Current policy reflects this ambivalence.
The George W. Bush administration, in its budgets submitted to Congress, has either severely reduced the budgets of or recommended elimination of many programs that would affect the distribution of health professionals. For example, in its Program Assessment Rating Tool review of federal agencies, the Office of Management and Budget labeled the health profession programs within the Department of Health and Human Services as “ineffective.”51 At the same time, the NHSC was rated as “moderately effective,” and the administration has asked for expansion of its budget and scope.
The arguments of economists have been used to support the negative federal assessments of health profession training programs intended to promote practice in underserved areas. Conservatives consider supporting the preparation of professionals who will be high earners (e.g., physicians) a distortion of the market,52 but liberals consider it a necessary element of improving overall equity in the system.53 Nevertheless, federal support of workforce programs has persisted since the late 1960s, and these programs have emphasized training practitioners to care for underserved populations. Encouragement of rural practice has been a consistent theme within these programs and has become a formal, specific focus of federal workforce policy.
More recently, emphasis has been placed on programs designed to develop a more diverse health workforce, and this will help rural areas in selected regions of the United States.54 AHEC is the closest version of a comprehensive coordinated support system, but its funding has been threatened in recent years, and it depends on many other federal, state, and community programs to maintain a “pipeline” to rural and under-served practices.55
ADAPTATION IN THE FIELD, MARKETS, AND ALTRUISM
The market forces that drive professionals into urban centers might be too strong to reverse without equally strong policy initiatives to counter them. Health care professionals are now tightly wedded to technology that is capital intensive and subject to forces that require centralization. Strengthening the bargaining power of rural populations is 1 way to counter this situation, potentially via favorable payment policies offered through Medicare and Medicaid. Piecemeal supplements tied to small portions of practice income via Medicare bonus payments apparently are not effective as economic stimulants in terms of selecting a practice location56; only the overall enhancement of practitioners’ earning potential seems likely to influence their decisions regarding where to practice. Any rural workforce program must overcome this dominating economic condition if it is to be successful. Economic forces are less often considered in normative–coercive solutions such as the NHSC. A lasting solution to geographic imbalance in the health care workforce will address some of the macro-level forces built around the core structures of medicine and medical training.
Altruism is an important and often overlooked force that drives a substantial portion of the health care workforce and cannot be discounted as a mechanism to promote rural practice.57 However, centralization and “utilitarian” approaches can blunt the expression of altruism. Increased local autonomy can help in the matching of willing, caring professionals to needy or welcoming rural communities, but this alone will not carry the total burden of resisting strong market forces.
General health workforce policies must have normative goals given the persisting inequitable distribution that represents, at best, a problem of distributional equity and, at worst, a problem regarding the quality of care available to rural communities. However, the larger forces that drive resource allocation in a market-dominated system cannot be overcome by coercion or fiat; there must be accommodation. The lessons taken from utilitarian policies is that they can adapt to meet normative policy ends.
Acknowledgments
The use of the terminology developed by Etzioni was suggested by Thomas R. Konrad, who has done extensive work in the area of physicians’ career choices; he and Donald Pathman provided support and advice during the development of the article. The Journal editor and the editor of the special issue on rural health, Charles Phillips, provided useful suggestions for focus and reorganizing early versions of the article. One anonymous reviewer strongly supported the inclusion and strengthening of the interpretive characterization of federal programs and deserves credit for this emphasis.
Peer Reviewed
References
- 1.Newhouse JP, Williams AP, Bennett BW, Schwartz WB. The Geographic Distribution of Physicians: Is the Conventional Wisdom Correct? Santa Monica, Calif: Rand Corp; 1982.
- 2.Newhouse JP. Geographic access to physician services. Annu Rev Public Health. 1990;11:207–230. [DOI] [PubMed] [Google Scholar]
- 3.Newhouse JP, Williams AP, Bennett BW, Schwartz WB. Does the geographical distribution of physicians reflect market failure? Bell J Economics. 1982; 13:493–505. [Google Scholar]
- 4.Rosenblatt RA, Hart LG. Physicians and rural America. In: Ricketts TC, ed. Rural Health in the United States. New York, NY: Oxford University Press Inc; 1999:38–51.
- 5.Council on Graduate Medical Education. Tenth Report: Physician Distribution and Health Care Challenges in Rural and Inner-City Areas. Rockville, Md: Health Resources and Services Administration; 1998.
- 6.Bureau of Health Professions. Area Resource Files. Rockville, Md: Health Resources and Services Administration; 2002.
- 7.Larson EH, Johnson KE, Norris TE, Lishner DM, Rosenblatt RA, Hart LG. State of the Health Workforce in Rural America: Profiles and Comparisons. Seattle, Wash: WWAMI Rural Health Research Center; 2003.
- 8.Rosenblatt RA, Moscovice IS. Rural Health Care. New York, NY: John Wiley & Sons Inc; 1982.
- 9.Rosenblatt RA, Cherkin DC, Schneeweiss R, et al. The structure and content of family practice: current status and future trends. J Fam Pract. 1982;15: 681–722. [PubMed] [Google Scholar]
- 10.Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290: 1173–1178. [DOI] [PubMed] [Google Scholar]
- 11.Larson EH, Hart LG, Goodwin MK, Geller J, Andrilla C. Dimensions of retention: a national study of the locational histories of physician assistants. J Rural Health. 1999;15:391–402. [DOI] [PubMed] [Google Scholar]
- 12.Baer LD, Smith LM. Nonphysician professionals and rural America. In: Ricketts TC, ed. Rural Health in the United States. New York, NY: Oxford University Press Inc; 1999:52–60.
- 13.Hooker R, Cawley JF. Physician Assistants in American Medicine. 2nd ed. Philadelphia, Pa: WB Saunders; 2002.
- 14.Grumbach K, Hart LG, Mertz E, Coffman J, Palazzon L. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003;1:97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buerhaus PI, Staiger DO. Trouble in the nurse labor market? Recent trends and future outlook. Health Aff. 1999;18:214–222. [DOI] [PubMed] [Google Scholar]
- 16.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–1993. [DOI] [PubMed] [Google Scholar]
- 17.Larson EH, Palazzo L, Berkowitz B, Pirani M, Hart LG. The contribution of nurse practitioners and physician assistants to generalist care in Washington State. Health Serv Res. 2003;38: 1033–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oral Health in America: A Report of the Surgeon General. Rockville, Md: National Institute of Dental and Craniofacial Research; 2000. NIH publication 00-4713.
- 19.Milgrom PM, Tichendorf D. Dental care. In: Geyman JP, Norris TE, Hart LG, eds. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001: 195–202.
- 20.Mofidi M, Konrad TR, Porterfield DS, Niska R, Wells B. Provision of care to the underserved populations by National Health Service Corps alumni dentists. J Public Health Dent. 2002;62: 102–108. [DOI] [PubMed] [Google Scholar]
- 21.Stratton TP. The economic realities of rural pharmacy practice. J Rural Health. 2001;17:77–81. [DOI] [PubMed] [Google Scholar]
- 22.Bureau of Health Professions. Report to Congress. The Pharmacist Work-force: A Study of the Supply and Demand for Pharmacists. Rockville, Md: Health Resources and Services Administration; 2000.
- 23.Straub L, Tripp C. Pharmacy services in rural Illinois: current issues. South Ill University Rural Res Rep. 2000; 11:2. [Google Scholar]
- 24.Caset MM, Klinger J, Moscovice I. Pharmacy services in rural areas: is the problem geographic access or financial access? J Rural Health. 2002;18: 467–477. [DOI] [PubMed] [Google Scholar]
- 25.Hartley D, Bird DC, Dempsey P. Rural mental health and substance abuse. In: Ricketts TC, ed. Rural Health in the United States. New York, NY: Oxford University Press Inc; 1999: 159–178.
- 26.Lambert D, Gale J, Bird D, Hartley D. Medicaid managed behavioral health in rural areas. J Rural Health. 2003;19: 22–32. [DOI] [PubMed] [Google Scholar]
- 27.Lambert D, Hartley D. Linking primary care and rural psychiatry: where have we been and where are we going? Psychiatr Serv. 1998;49:965–967. [DOI] [PubMed] [Google Scholar]
- 28.Rost K, Fortney J, Fischer E, Smith J. Use, quality, and outcomes of care for mental health: the rural perspective. Med Care Res Rev. 2002;59:231–265. [DOI] [PubMed] [Google Scholar]
- 29.Hartley D, Britain C, Sulzbacher S. Behavioral health: setting the rural health research agenda. J Rural Health. 2002;18(suppl):242–255. [DOI] [PubMed] [Google Scholar]
- 30.Hajat A, Stewart K, Hayes KL. The local public health workforce in rural communities. J Public Health Manage Pract. 2003;9:481–488. [DOI] [PubMed] [Google Scholar]
- 31.Pathman DE, Riggins TA. Promoting medical careers in underserved areas through training. Fam Med. 1996; 28:508–510. [PubMed] [Google Scholar]
- 32.Rabinowitz HK, Diamond JJ, Vekoski JJ, Gayle JA. The impact of multiple predictors on generalist physicians’ care of underserved populations. Am J Public Health. 2000;90:1125–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Etzioni A. A Comparative Analysis of Complex Organizations. New York, NY: Free Press; 1961.
- 34.Crandall LA, Dwyer JW, Duncan RP. Recruitment and retention of rural physicians: issues for the 1990s. J Rural Health. 1990;6:19–38. [DOI] [PubMed] [Google Scholar]
- 35.Reinhardt UE. Dreaming the American dream: once more around on physician workforce supply. Health Aff. 2002;21:28–32. [DOI] [PubMed] [Google Scholar]
- 36.Lewis CE, Fein R, Mechanic D. A Right to Health: The Problem of Access to Primary Health Care. New York, NY: John Wiley & Sons Inc; 1976.
- 37.Pathman DE, Konrad TR, Ricketts TC III. The National Health Service Corps experience for rural physicians in the late 1980s. JAMA. 1994;272: 1341–1348. [PubMed] [Google Scholar]
- 38.Kaiser Family Foundation. HHS announces $89M in scholarships, loan repayments for care providers working in rural areas, inner cities. Available at: http://www.kaisernetwork.org/daily_reports/rep_index.cfm?hint=3&DR_ID=9779. Accessed January 19, 2004.
- 39.Pathman DE, Konrad TR, Ricketts TC. The comparative retention of National Health Service Corps and other rural physicians: results of a 9-year follow-up study. JAMA. 1992;268: 1552–1558. [PubMed] [Google Scholar]
- 40.Pathman DE, Taylor DH Jr, Konrad TR, et al. State scholarship, loan forgiveness, and related programs: the unheralded safety net. JAMA. 2000;284: 2084–2092. [DOI] [PubMed] [Google Scholar]
- 41.Hagopian A, Thompson MJ, Kaltenbach E, Hart LG. Health departments’ use of international medical graduates in physician shortage areas. Health Aff. 2003;22:241–249. [DOI] [PubMed] [Google Scholar]
- 42.Mick SS, Lee SY, Wodchis WP. Variations in geographical distribution of foreign and domestically trained physicians in the United States: ‘safety nets’ or ‘surplus exacerbation’? Soc Sci Med. 2000;50:185–202. [DOI] [PubMed] [Google Scholar]
- 43.Geyman JP. Graduate education for rural practice. In: Geyman JP, Norris TE, Hart LG, eds. Textbook of Rural Medicine. New York, NY: McGraw-Hill; 2001:369–380.
- 44.Geyman JP, Hart LG, Norris TE, Coombs JB, Lishner DM. Educating generalist physicians for rural practice: how are we doing? J Rural Health. 2000; 16:56–80. [DOI] [PubMed] [Google Scholar]
- 45.Rabinowitz H. Recruitment and retention of rural physicians: how much progress have we made? J Am Board Fam Pract. 1995;8:496–499. [PubMed] [Google Scholar]
- 46.Mareck DG. Minnesota’s rural health school: interdisciplinary community education. Fam Med. 2003;35(2): 86–88. [PubMed] [Google Scholar]
- 47.DePoy E, Wood C, Miller M. Educating rural allied health professionals: an interdisciplinary effort. J Allied Health. 1997;26(3):127–132. [PubMed] [Google Scholar]
- 48.Mullan F. Primary care: an endangered species. AHEC Natl Area Health Educ Centers Bull. 2000;17(2):1–9. [Google Scholar]
- 49.Moore GT. Primary care in crisis. In: Showstack J, Rothman AA, Hassmiller SB, eds. The Future of Primary Care. San Francisco, Calif: Jossey-Bass; 2004:3–16.
- 50.Fox DM. From piety to platitudes to pork: the changing politics of health workforce policy. J Health Polit Policy Law. 1996;21:825–844. [PubMed] [Google Scholar]
- 51.Office of Management and Budget. Budget of the United States Government Fiscal Year 2005. Washington, DC: Executive Office of the President; 2004. Available at: http://www.whitehouse.gov/omb/budget/fy2005/pma/hhs.pdf. Accessed December 7, 2004.
- 52.Rosenthal MB, Zaslavsky AM, Newhouse JP. The geographic distribution of physicians revisited. Available at: http://rwj.harvard.edu/core. Accessed April 5, 2004. [DOI] [PMC free article] [PubMed]
- 53.K Grumbach. Fighting hand to hand over physician workforce policy. Health Aff. 2002;21:13–27. [DOI] [PubMed] [Google Scholar]
- 54.Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff. 2002;21:90–102. [DOI] [PubMed] [Google Scholar]
- 55.Ricketts TC, Fraher EP, Roussel A, Fruhbeis M, Weiner BJ, Schwalberg R. An Evaluative Study of the Area Health Education Centers Program: A Final Report to the Health Resources and Services Administration. Chapel Hill, NC: Cecil G. Sheps Center for Health Services Research; 2002.
- 56.Shugarman LR, Farley DO. Shortcomings in Medicare bonus payments for physicians in underserved areas. Health Aff. 2003;22:173–178. [DOI] [PubMed] [Google Scholar]
- 57.Fell and LE, Lesser CS, Staiti AB, Katz A, Lichiello P. The resilience of the health care safety net, 1996–2001. Health Serv Res. 2003;38:489–502. [DOI] [PMC free article] [PubMed] [Google Scholar]