Abstract
For the past several years, diverse and often confused concepts of stigma have been invoked in discussions on AIDS. Many have argued compellingly that AIDS-related stigma acts as a barrier to voluntary counseling and testing. Less compelling are observations regarding the source of stigma or its role in decreasing interest in HIV care.
We reviewed these claims as well as literature from anthropology, sociology, and public health. Preliminary data from research in rural Haiti suggest that the introduction of quality HIV care can lead to a rapid reduction in stigma, with resulting increased uptake of testing. Rather than stigma, logistic and economic barriers determine who will access such services. Implications for scale-up of integrated AIDS prevention and care are explored.
Most of those involved in the movement to slow the spread of AIDS and to improve the quality of life of those living with HIV view stigma and discrimination as human rights violations requiring redress. Both organizations and individuals have taken various actions to address stigma; however, these actions often have not been grounded in a broad biosocial understanding of stigma and AIDS-related discrimination. The Joint United Nations Programme on HIV/AIDS (UNAIDS) often refers to the need to fight stigma in order to combat HIV/AIDS,1 but the definition of stigma remains unclear.
Stigma undoubtedly poses several challenges, but the mechanisms by which it is at the heart of the AIDS pandemic need to be explored. Stigma and discrimination are part of complex systems of beliefs about illness and disease that are often grounded in social inequalities. Indeed, stigma is often just the tip of the iceberg; because it is visible and generally accepted in public health discourse without further qualification, the term has frequently served as a means of giving short shrift to powerful social inequalities (for example, in Valdiserri2) that are much harder to identify and conceptualize.
In addition, the tendency to use “rapid” methodologies has generated a wealth of information regarding people’s knowledge and attitudes about AIDS-related stigma in different situations, but this information is often “desocialized”—decontextualized from larger social processes that are both historically rooted and linked to persons and processes that are not visible to the survey researcher. Such desocialized and disparate approaches have hindered the advancement of a theoretically sound understanding of AIDS-related stigma and have slowed effective actions to counter stigma.
Similar confusion surrounds debate over stigma as a barrier to introducing antiretrovirals to poor countries or to making voluntary HIV tests accessible. Again, such comments are insufficiently grounded in broader social analyses. The AIDS literature is rife with surveys that offer completely discrepant views on how stigma is related to events and processes as varied as sexual comportment, care-seeking behavior, and adherence to antibiotic regimens.3–5 Without reference to any particular experience in delivering AIDS care in the world’s poorest nations, 1 recent review claimed that
in many countries hardest hit by HIV, the stigma of this disease is at least as powerful, if not more so, than in wealthy nations. Although the prospect of access to treatment may encourage individuals to determine their HIV status, the linkage of treatment to directly observed HIV therapy may paradoxically lower the use of counseling and testing services due to confidentiality concerns.6(p1385)
Elsewhere, we have termed those assertions “immodest claims of causality,”7 since they are advanced authoritatively but may be readily countered by contrary claims.
Our concer n in this review is to question the understanding of AIDS-related stigma and to assess its relationships to integrated HIV prevention and care. That AIDS-related stigma exists and needs redress is not debated. But where is the evidence that stigma stands as a ranking obstacle to treatment in poor countries when less than 5% of people with advanced AIDS in these countries have access to highly active antiretroviral therapy (HAART)?8 Instead, some recent studies conducted in Botswana,9 Senegal,10 and Côte d’Ivoire11 showed that the cost of medications borne by patients is the main stated reason for lack of adherence to therapy.
Still, “stigma” has become, in the popular press, one more argument used to walk a slow walk to fight the pandemic. A study conducted in Zambia claims that “despite increasing access to prevention of mother-to-child transmission initiatives, including antiretroviral drugs, the perceived disincentives of HIV testing, particularly for women, largely outweigh the potential gains from available treatments.”12(p347) A closer look at the study shows that the use of antiretrovirals was limited to the prevention of mother-to-child transmission of HIV and did not include HAART to treat women (or any other adults) outside of pregnancy. What conclusions might be reached if proper therapy and a more equitable distribution of that therapy were introduced? A study conducted in Kenya showed that lack of access to drugs is the main factor compromising medical residents’ ability to provide care to AIDS patients.13
On a more hopeful note, the evaluation of a mother-to-child transmission program in the Dominican Republic suggested that implementation of effective therapy for mothers has helped diminish the stigmatization of patients, in part because health professionals focused on pregnant women as potential conduits of antiretrovirals destined to prevent transmission to unborn children.14 An AIDS program in rural Haiti also reported a sharp decline in AIDS-related stigma since the introduction of HAART.15
THEORETICAL FRAMEWORK
Our theoretical framework for the understanding of AIDS-related stigma has been developed over a decade of ethnographic research in rural Haiti. Our interpretations of the relevant literature are informed by more recent experience providing clinical services in rural Haiti.15 Although the first references to the association between stigma and health in the social science literature date back to the 1880s,16 sociologist Erving Goffman, beginning with his work in psychiatric hospitals in the late 1950s, developed what has become the benchmark social theory of the association between stigma and disease.17,18 Goffman defined stigma as the identification that a social group creates of a person (or group of people) based on some physical, behavioral, or social trait perceived as being divergent from group norms. This socially constructed identification lays the groundwork for subsequent disqualification of membership from a group in which that person was originally included. Although Goffman emphasized the importance of analyzing stigma in terms of relationships rather than individual traits or attributes,18 many subsequent interpretations of stigma have focused on individual attributes and are divorced from broader social processes, especially from relations of power.
Key anthropological and sociological contributions to our understanding of AIDS have introduced new components to Goffman’s definition of stigma and offer the promise of novel conceptual frameworks.19–22 Others have used a similar approach to understanding stigma associated with diseases such as hookworm, tuberculosis, cancer, polio, and sexually transmitted infections and the association of these diseases with racist ideology in the United States23,24 or with cholera-related stigma in Venezuela.25 Further contributions of anthropological work to the understanding of AIDS stigma have been obtained through research conducted in Zambia,26 South Africa,27 the Philippines,28 Haiti,29 and Puerto Rico and the United States.30
The field of social psychology has clarified the cognitive processes that lead to labeling and stereotyping. However, most psychological research focuses more on individualistic perceptions and attitudes than on the broader social context in which such perceptions are grounded. Most of these studies discuss the implications of these beliefs—in terms of misunderstandings, misinformation, and negative attitudes—as far as efforts to change the perceptions of the stigmatizers are concerned. Examples from Jamaica31 and Mexico32 are illustrative. Such approaches seek to improve HIV/AIDS education and to enhance sensitivity and empathy training or tolerance through personal contact with people living with HIV.4,33–35 However, these laudable efforts have placed little emphasis on the larger economic and political processes in which stigma is grounded.
More recently, some anthropologists20,36–39 have challenged approaches that emphasize cognitivist explanations of stigma rather than the structural violence that generates the social inequalities in which stigma is invariably rooted. According to Parker and Aggleton, the desocialization of stigma is not
drawn directly from Goffman, who, on the contrary, was very much concerned with issues of social change. . . . Yet the fact that Goffman’s framework has been appropriated in much research on stigma (whether in relation to HIV/AIDS or other issues), as though stigma were a static attitude rather than a constantly changing (and often resisted) social process has seriously limited the ways in which stigmatization and discrimination have been approached in relation to HIV and AIDS.20(p14)
These authors proposed that stigma be analyzed within frameworks drawing on concepts of power, dominance, hegemony, and oppression.40,41 They further proposed interventions that have deeper social, political, and economic roots, because “stigma is deployed by concrete and identifiable social actors seeking to legitimize their own dominant status within existing structures of social inequality.”20(p18) This resocialized view of stigma defines discrimination, one of the consequences of stigma, as “when, in the absence of objective justification, a distinction is made against a person that results in that person’s being treated unfairly and unjustly on the basis of belonging or being perceived to belong, to a particular group.”42 Other anthropologists have been scrupulous in ensuring that their interpretations of stigma are informed by the lived experience of those who suffer from it.22,29,43–47
A useful definition of AIDS-related stigma comes from the field of sociology:
In our conceptualization, stigma exists when the following interrelated components converge. In the first component, people distinguish and label human differences. In the second, dominant cultural beliefs link labeled persons to undesirable characteristics—to negative stereotypes. In the third, labeled persons are placed in distinct categories so as to accomplish some degree of separation of “us” from “them.” In the fourth, labeled persons experience status loss and discrimination that lead to unequal outcomes. Finally, stigmatization is entirely contingent on access to social, economic, and political power that allows the identification of differentness, the construction of stereotypes, the separation of labeled persons into distinct categories, and the full execution of disapproval, rejection, exclusion, and discrimination.48(p367)
These authors noted that stigma is a “persistent predicament” and sought to understand “why the negative consequences of stigma are so difficult to eradicate.”48,49(p379) The fundamental causes of stigma need to be addressed, they argued, by targeting multiple mechanisms to bring about change. Yet these authors limited the depth of required transformations to changing “deeply held attitudes and beliefs of powerful groups” and confining “the power of such groups to make their cognitions the dominant ones.”48(p381) In acknowledging the centrality of social, economic, and political power differentials—emphasizing that cognitive processes are necessary but not sufficient causes for the production of stigma—they concluded that a better understanding of stigma requires an understanding of how these power differentials, along with issues of constraint and resistance, exert their impact on stigma.48
We propose structural violence as a conceptual framework for understanding AIDS-related stigma. Every society is shaped by large-scale social forces that together define structural violence. These forces include racism, sexism, political violence, poverty, and other social inequalities that are rooted in historical and economic processes that sculpt the distribution and outcome of HIV/AIDS. Structural violence predisposes the human body to pathogenic vulnerability by shaping risk of infection and also rate of disease progression.7,50–53 Structural violence also determines who has access to counseling, diagnostics, and effective therapy for HIV disease. Finally, structural violence determines, in large part, who suffers from AIDS-related stigma and discrimination.
In societies marked by profound racism, it is expected that people of color with AIDS will be more stigmatized than in societies where racism is more attenuated. Similarly, gender inequality determines the extent to which sexism will mark the course of HIV disease. In highly sexist settings, the disclosure of HIV infection is more likely to provoke stigma and threat of domestic violence than in environments where women enjoy gender equity. Class often trumps both racism and sexism. The poor almost invariably experience violations of their social and economic rights. We can therefore conclude that poverty, already representing an almost universal stigma, will be the primary reason that poor people living with HIV suffer from greater AIDS-related stigma. Racism, sexism, and poverty exacerbate one another, especially where political violence and social inequalities are added to the equation. Together, social forces determine not only risk of HIV infection but also risk of AIDS-related stigma.
To improve our understanding of AIDS-related stigma, it is necessary to focus on a series of variables readily discernible across different societies; these include the experience of people living with HIV, public perceptions of AIDS, local experiences of stigma and discrimination and their influence in care-seeking activities, varied degrees of stigma over the course of HIV disease, impact of stigma on quality of life, and structural sources of stigma and discrimination (B. J. Good, written communication, May 2003). The understanding of these experiences and the analysis of these processes permit a better understanding of how different strategies, ranging from legal recourse to the introduction of HAART, can alter the course of AIDS-related stigma.
RESULTS
Public health experts prescribing health policies for poor countries believe that stigma, the high cost of treatment, the lack of infrastructure, and poor patient adherence to treatment constitute insurmountable barriers to effective AIDS control. From our experience providing health and social services in rural Haiti, this is not the case.15,52,54,55 Haiti is by far the most impoverished country in Latin America and, not coincidentally, the hemisphere’s most HIV-affected country, with an adult prevalence of around 5.6%.56 To illustrate how structural violence is embodied and generates stigma, we explored the history of one of our patients in rural Haiti. Because the “texture” of dire affliction is better felt in the gritty details of biography, and since any example begs the question of its relevance, we argue that the story of our patient is anything but anecdotal. In the eyes of the epidemiologist as well as the political analyst, Samuel has suffered in exemplary fashion.
In 2001, Samuel Morin was dying of AIDS. Until then, Samuel, 40 years old, had farmed a small plot of land and had a tiny shop—which sold everything from matches to soap—in a town in central Haiti. He considered himself poor but was able to send his 4 children to school. Samuel was an active member of his church and sometimes used his meager earnings to help neighboring families in crisis, providing food if their crops failed, or helping with school fees. He also supported his sister and her 3 children after his brother-in-law died of AIDS.
When Samuel became ill in the mid-1990s, his wife had to assume all responsibility for the farming, although he could still sit and mind the shop. But after a while, Samuel recalled, “the disease transformed me. I looked like a stick.” He continued to lose weight and then developed visible skin infections and thrush; he had difficulty swallowing food and began to cough. It was at this time, he felt, that people stopped coming to his shop. His children had to leave school because they were needed to help in the fields and because Samuel and his wife could no longer afford the school fees. Eventually, the shop failed completely. His wife left him and returned to her parents’ home in Portau-Prince.
In July 2001, when Samuel weighed only 80 pounds (Figure 1a ▶), he decided to use his last 10 Haitian dollars to pay for a truck ride to the Clinique Bon Sauveur in Cange, a 6-hour walk from his home. Since then, Samuel has been receiving HAART under the supervision of an accompagnateur (community health worker), free of charge. In almost 3 years of therapy, Samuel stated, he has not missed a dose; he has responded clinically—he has gained 30 pounds, has normal skin color, and feels “great”—and has an undetectable viral load (Figure 1b ▶ shows Samuel a year after initiation of therapy). Moreover, his family has returned to him, his children are back in school, and he has reopened his shop. He also volunteers with the local Partners In Health team in HIV-prevention efforts. Of his recovery, Samuel said, “I was a walking skeleton before I began therapy. I was afraid to go out of my house and no one would buy things from my shop. But now I am fine again. My wife has returned to me and now my children are not ashamed to be seen with me. I can work again.”
FIGURE 1—

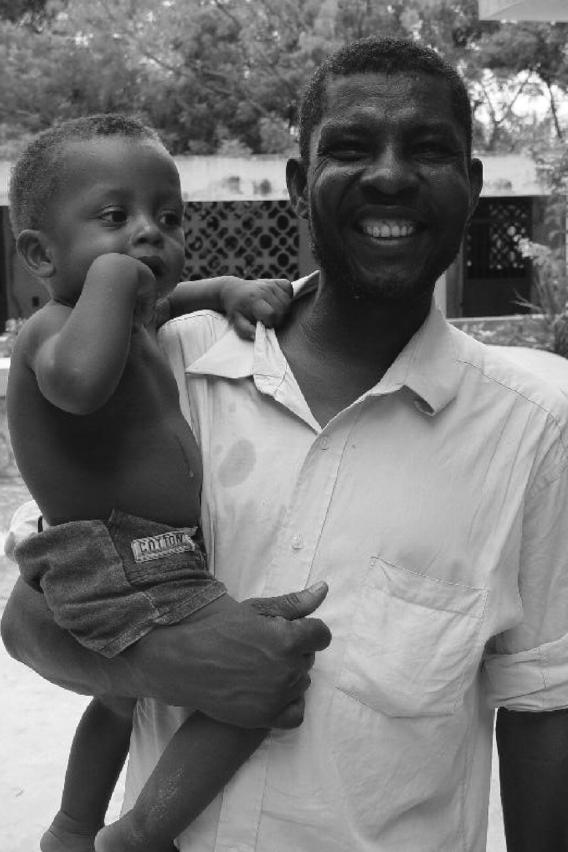
Samuel Morin, (a) in July 2001 before receiving HAART and (b) 1 year later, after a year of therapy.
In reflecting on Samuel’s experience, it is possible to argue that AIDS treatment can spark a “virtuous social cycle.” Access to comprehensive AIDS care57 saved Samuel’s life; returning to work and securing school fees for his children has allowed him to surmount some of the miserable conditions faced by the majority of Haitians. It is also possible to discern direct links between access to care and stigma. There are the links mentioned by Samuel: proper HIV care can transform a disfiguring and consumptive disease into a manageable condition that is invisible to one’s consociates. Integrating people living with HIV into the workforce of a community health program—around 5% of our current staff are persons living with HIV—permits them to receive comprehensive care, send their children to school, and earn steady wages. Further, the demonstrably favorable response of Samuel and others to HAART has sparked interest in voluntary counseling and testing. Together, these processes have contributed to lessening the impact of the AIDS stigma.
Years ago, before the advent of effective therapy for AIDS, anthropologists noted that the introduction of such therapy may alter profoundly the social interpretations of the disease.43,58 Other social scientists have shown that stigma is aggravated by an undefined etiology and the lack of an effective treatment.59 AIDS has afforded ample possibilities to study the social construction of stigma. Exposure to a new disease, as occurred with AIDS in Haiti in the 1980s, generates new cultural models of the etiology and expected course of disease.29,60,61 These models change with time because diseases have a social course—that is, pathology is embedded in social experience.42,60 The social experience of AIDS is affected profoundly by the advent of effective therapy.
The Haiti project already demonstrates that individuals who can access effective care are the most likely to get an HIV test,15 which supports social theories on the social course of illness. The introduction of antiretrovirals has had a profound and positive impact on the demand for voluntary counseling and testing. It is possible to chart the rise in demand for testing and counseling in rural Haiti by following laboratory registers and daily reports. Since 1998, when we introduced the first free and comprehensive AIDS program in rural Haiti at the Clinique Bon Sauveur,15 demand for such services has more than quintupled.
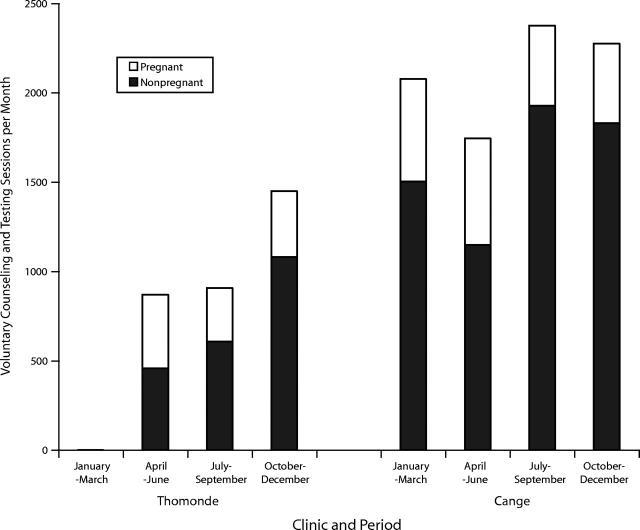
Samuel Morin was diagnosed and treated initially in Cange. But looking at his home-town of Thomonde, where community-based AIDS care was introduced only in 2003, is instructive. Figure 2 ▶ shows how rapidly voluntary counseling and testing may increase when comprehensive prevention and care are introduced. In Thomonde, voluntary counseling and testing sessions per month have skyrocketed from 0 to an average of 869 in the second quarter and up to 1450 in the fourth quarter; at the Clinique Bon Sauveur in Cange, the number of voluntary counseling and testing sessions are stable, averaging 2118 per month.
FIGURE 2—
Average monthly uptake of voluntary counseling and testing in a new (Thomonde) and an ongoing (Cange) AIDS clinic: rural Haiti, 2003.
As so many of our patients have noted, what is the motivation for learning one’s serostatus when there is no possibility of being treated for opportunistic infections or of access to prevention of mother-to-child transmission during pregnancy, much less of being treated with antiretrovirals when needed? Can we blame these public health failures on stigma alone?
DISCUSSION
The Haiti experience suggests that improving clinical services can raise the quality of prevention efforts, boost staff morale, and reduce AIDS-related stigma. As 1 of the first donor-supported treatment projects in a very poor country, our team’s experience suggests that the full participation of community health workers will be required if HIV prevention and care are to reach the poorest and most vulnerable communities. Adjuvant social services must also be part of a comprehensive project, as must attention to tuberculosis and primary health care needs. Only a biosocial framework drawing on both qualitative and quantitative methods can hope to assess the epidemiological, social, and economic impact of both the epidemic and responses to it.
The last 2 decades have taught us a great deal about failure and how it is best measured; new HIV infections and AIDS deaths are the grim yardsticks. A lack of decent medical care and effective prevention strategies (including the absence of a vaccine and inadequate women-controlled barrier methods) frustrates public health efforts. However, a broad range of other events and processes are markers for failure: AIDS-related stigma and discrimination, unsafe blood transfusions, unattended childbirths, unclean water, and a lack of social services for HIV-affected individuals and families would figure high on this list of indirect markers.
And there’s the analytic rub: we don’t know how best to analyze such a diverse set of inextricably related problems. What evaluative framework might guide us as we attempt to measure phenomena as varied as HIV incidence and AIDS-related stigma and discrimination? How might we assess the impact of new projects? How do we address poverty and gender inequality in AIDS prevention and care, if they are so manifestly related to HIV transmission and outcomes? The best framework for analysis and evaluation would need to be robustly biosocial, since the phenomena it attempts to describe are nothing if not both biological and social. The framework would draw on conventional epidemiology, certainly, but also on complementary resocializing disciplines in which patients’ voices and experiences are heard and documented. Anthropology and sociology are among these disciplines, as is the sociology of science. Unfortunately, ethnographic inquiry and community health worker reports are not often regarded, within public health, as reliable sources of information.
Could this evaluative framework be anything other than biosocial? It must not only assess the impact of stigma on morbidity and mortality but also address questions of stigma and equity; it must offer a resocialized understanding of how inequalities come to take their toll through disparities of risk for infection, radically different courses of disease, and disparities of access to proven therapies. Some of the indicators that we suggest be used include the number of patients with access to effective care, serosurveys in sentinel populations (e.g., prenatal clinics), HIV prevention checklists (sex education, condom distribution), number of person-hours of prevention through information and education campaigns, number of sites offering prevention of mother-to-child transmission of HIV, number of community health workers supervising therapy, reinforcement of public health infrastructures, creation of coalitions to expand and “harmonize” prevention and care services, transparent reporting of expenditures, and avoidance of drug stock depletions. We need, now, a novel synthesis of complementary methodologies, both quantitative and qualitative. We need to value the input of community groups, including community health workers and others who deliver services directly to those in greatest need.
The transformation of AIDS from an inevitably fatal disease to a chronic and manageable one has decreased stigma dramatically in Haiti, as Samuel’s story shows. Our own experience in Haiti suggests that it is clear that the impact of a “low-tech” HIV prevention-and-care project could be measured without importing a new and costly “evaluation infrastructure.” Table 1 ▶ lists some indirect indices of positive impact and the potential sources of data that might be made available in even the poorest communities. The most daunting challenges for which scale-up projects must be prepared are those having to do with the poverty of patients.
TABLE 1—
Assessing the Impact of a Comprehensive AIDS Program: Possible Data Points
| Indicators | Sources of Information Needed to Evaluate Indicators |
| Impact on patient outcomes | Patient charts, weight, activities of daily living |
| Impact on burden of disease | Prenatal screening |
| Response to local calls for equity | Community forums, focus groups |
| Reduced mortality | Chart review, community health workers’ reports |
| Reduced rates of hospitalization | Daily reports, chart review |
| Reduced stigma | Ethnographic inquiry, case histories |
| Improved staff morale | Staff meetings, ethnographic study |
| Increased demand for voluntary counseling and testing | Laboratory registers, daily reports |
| Meeting public health goals | External Ministry of Health evaluation |
AIDS, stigma, and blame have been intertwined since the start of the epidemic. One of the characteristics of AIDS stigma is that, from the onset, this disease has been associated with lifestyles that society attributes, with little evidence, to being shaped by “voluntary acts.” In America and Europe, where in the 1980s the epidemic ravaged groups of homosexuals and heroin addicts, there was very little solidarity with infected people because they were blamed for having “opted” for sexual practices or for addiction and reproached by society as immoral. The stigma that already existed toward these groups was amplified by AIDS.62 This type of social discrimination was extended to poor countries where cases of HIV infection began to be diagnosed29 and to other groups of vulnerable people, including poor women.
Some of these prejudices were reflected within universities, international organizations, foundations, bilateral organizations, governments, financing institutions, and pharmaceutical companies—institutions key to effective responses to the pandemic. A general hostility to people living with HIV is suggested by the fact that, until recently, AIDS prevention, not treatment, was the leitmotiv of international AIDS work; treatment was the privilege of those able to pay for it. These are powerful fora, and their position set the agenda for both funding and action. Freire might say that such positions are “sectarized”: “Sectarization . . . transforms reality into something false that, thus, cannot be transformed.”63(p30) By ignoring or giving short shrift to visible evidence of structural violence in the transmission of HIV and in the stigma that it generates, these “fora of knowledge” may perpetuate, sometimes by inaction, both stigma and discrimination.
Since the 1980s, blaming the victim has been a powerful current in the social experience of AIDS. Victim blaming helps to explain the lack of solidarity in providing appropriate care to people living with HIV; discrimination in the arenas of housing, employment, and education has been documented in the Caribbean64–68 and in other parts of the world. The only people not often blamed for their own misfortune are those deemed infected by mechanisms considered unrelated to “personal choices in lifestyles.” These exceptions include health professionals who, by occupational accident, are exposed to HIV-infected blood and hemophiliacs and other recipients of blood products infected by medical and political negligence, as occurred in France in 1985.69 Additionally, children who contract HIV in utero or during birth or breastfeeding are also often exempt from blame (as noted in Puerto Rico70). These same children may face, as they grow older, discrimination when attending school (as in Mexico71). Even women infected through rape are often blamed or the violence of which they are victims.53
Exemptions from blame may be reflected at the national level within systems of social security or of private insurance that cover antiretroviral therapy for exempted groups but not for others. In the international arena, the division of people living with HIV into “blameworthy” and “blameless” categories reinforces the lack of will on the part of rich countries to finance AIDS treatment in poor countries. The funding gap, which reflects social inequalities between and among countries, is itself a reflection and source of structural violence contributing to AIDS-related stigma. Stigma and human-rights violations deriving from it are often the only visible part of deep-rooted social inequality. Addressing the root causes of stigma will require addressing structural violence, including the symbolic violence perpetuated by shallow theories about AIDS-related stigma. These theories may lead to inaction. To assess AIDS-related stigma and declare it a cause rather than both cause and consequence of inequality will probably weaken efforts to address AIDS among those with heightened risk of HIV because of poverty, racism, and gender inequality.
Acknowledgments
We acknowledge the Wilbur Marvin Fund of the David Rockefeller Center for Latin American Studies at Harvard University for the award of a 2003 Faculty Grant to the authors to work on the project “HIV/AIDS in the Caribbean: The Impact of Effective Therapy on Stigma.” The scale-up of AIDS care in central Haiti has been made possible by the Global Fund to Fight AIDS, Tuberculosis and Malaria.
We are grateful to Yasmin Khawja, Haun Saussy, Joan Paluzzi, Alice Yang, and Rob Stavert for their contributions. We are most indebted to the Haitian clinical team, led by Dr Fernet Léandre, for its efforts to implement integrated AIDS prevention and care under very difficult circumstances.
Human Participant Protection No protocol approval was needed for this study.
Contributors Both authors conceptualized the article, interpreted findings, and wrote the article.
Peer Reviewed
References
- 1.Piot P. From planning to implementation: success against AIDS in the region. Opening speech at: 2nd Latin American Forum on HIV/AIDS and STIs; April 8, 2003; Havana, Cuba.
- 2.Valdiserri RO. HIV/AIDS stigma: an impediment to public health. Am J Public Health. 2002;92: 341–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fortenberry JD, McFarlane M, Bleakley A, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92:378–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am J Public Health. 2002;92:371–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Egger M, Pauw J, Lopatatzidis A, et al. Promotion of condom use in a high-risk setting in Nicaragua: a randomised controlled trial. Lancet. 2000;355: 2101–2105. [DOI] [PubMed] [Google Scholar]
- 6.Liechty C, Bangsberg D. Doubts about DOT: antiretroviral therapy for resource-poor countries. AIDS. 2003;17:1383–1387. [DOI] [PubMed] [Google Scholar]
- 7.Farmer P. Infections and Inequalities: The Modern Plagues. Berkeley: University of California Press; 1999.
- 8.Scaling Up Antiretroviral Therapy in Resource-Limited Settings. Geneva, Switzerland: World Health Organization; 2002.
- 9.Weiser S, Wolfe W, Bangsberg D, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 2003;34(3):281–288. [DOI] [PubMed] [Google Scholar]
- 10.I Lanièce, Ciss M, Desclaux A, et al. Adherence to HAART and its principal determinants in a cohort of Senegalese adults. AIDS. 2003;17(suppl 3): S103–S108. [DOI] [PubMed] [Google Scholar]
- 11.Delaunay K, Vidal L, Msellati P, Moatti J-P. La mise sous traitement antirétroviral dans l’Initiative: l’explicite et l’implicite d’un processus de sélection. In: Msellati P, Vidal L, Moatti J-P, eds. L’accès aux traitements du VIH/sida en Côte d’Ivoire. Aspects économiques, sociaux et comportementaux. Paris, France: Agence Nationale de Recherches sur le Sida; 2001:87–113.
- 12.Bond V, Chase E, Aggleton P. Stigma, HIV/AIDS and prevention of mother-to-child transmission in Zambia. Eval Program Plann. 2002;25:347–356. [Google Scholar]
- 13.Raviola G, Machoki MI, Mwaikambo E, Good MJD. HIV, disease plague, demoralization and “burnout”: resident experience of the medical profession in Nairobi, Kenya. Cult Med Psychiatry. 2002;26: 55–86. [DOI] [PubMed] [Google Scholar]
- 14.Cáceres Ureña FI, Duarte I, Moya EA, Pérez-Then E, Hasbún MJ, Tapia M. Análisis de la situación y la respuesta al VIH/SIDA en República Dominicana. Santo Domingo, Dominican Republic: Instituto de Estudios de Población y Desarrollos (IEPD) and Asociación Dominicana Pro-Bienestar de la Familia (PROFAMILIA); 1998.
- 15.Farmer P, Léandre F, Mukherjee J, et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet. 2001;358:404–409. [DOI] [PubMed] [Google Scholar]
- 16.Tuke DH. The Cagots. J Anthropol Instit Great Britain Ireland. 1880;9:376–385. [Google Scholar]
- 17.Goffman E. Asylums: Essays on the Social Situation of Mental Patients and Other Inmates. Garden City, NY: Anchor Books; 1961.
- 18.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Garden City, NY: Anchor Books; 1963.
- 19.Weiss MG, Ramakrishna J. Stigma interventions and research for international health. Paper presented at: Stigma and Global Health: Developing a Research Agenda; September 5–7, 2001; Bethesda, Md.
- 20.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57:13–24. [DOI] [PubMed] [Google Scholar]
- 21.Das V. Stigma, contagion, defect: issues in the anthropology of public health. Paper presented at: Stigma and Global Health: Developing a Research Agenda; September 5–7, 2001; Bethesda, Md.
- 22.Alonzo AA, Reynolds NR. Stigma, HIV and AIDS: an exploration and elaboration of a stigma trajectory. Soc Sci Med. 1995;41(3):303–315. [DOI] [PubMed] [Google Scholar]
- 23.Wailoo K. Stigma, race, and disease in 20th century America: an historical overview. Paper presented at: Stigma and Global Health: Developing a Research Agenda; September 5–7, 2001; Bethesda, Md.
- 24.Brandt A. No Magic Bullet: A Social History of Venereal Disease in the United States Since 1880. Oxford, England: Oxford University Press; 1985.
- 25.Briggs C, Mantini-Briggs C. Stories in the Time of Cholera: Racial Profiling During a Medical Nightmare. Berkeley: University of California Press; 2003.
- 26.AIDS Gausset Q. and cultural practices in Africa: the case of the Tonga (Zambia). Soc Sci Med. 2001; 52(4):509–518. [DOI] [PubMed] [Google Scholar]
- 27.Wojcicki JM, Malala J. Condom use, power and HIV/AIDS risk: sex-workers bargain for survival in Hillbrow/Joubert Park/Berea, Johannesburg. Soc Sci Med. 2001;53(1):99–121. [DOI] [PubMed] [Google Scholar]
- 28.Simbulan NP, Aguilar AS, Flanigan T, Cu-Uvin S. High-risk behaviors and the prevalence of sexually transmitted diseases among women prisoners at the women state penitentiary in Metro Manila. Soc Sci Med. 2001;52(4):599–618. [DOI] [PubMed] [Google Scholar]
- 29.Farmer P. AIDS and Accusation: Haiti and the Geography of Blame. Berkeley: University of California Press; 1992.
- 30.Finlinson HA, Robles RR, Colón HM, et al. Puerto Rican drug users experiences of physical and sexual abuse: comparisons based on sexual identities. J Sex Res. 2003;40(3):277–285. [DOI] [PubMed] [Google Scholar]
- 31.Hue LE. Children’s [sic] involvement in HIV/AIDS support initiatives help reduce stigma and discrimination. Paper presented at: 14th International AIDS Conference; July 7, 2002; Barcelona, Spain.
- 32.McCauley A, Stewart H, Baker S, et al. HIV prevention programs can reduce stigma among students. Paper presented at: 14th International AIDS Conference; July 9, 2002; Barcelona, Spain.
- 33.Devine PG, Plant EA, Harrison K. The problem of “us” versus “them” and AIDS stigma. Am Behav Sci. 1999;42(7):1208–1224. [Google Scholar]
- 34.Herek GM. Illness, stigma, and AIDS. In: Costa P, Vanden GR, eds. Psychological Aspects of Serious Illness. Washington, DC: American Psychological Association; 1990:103–150.
- 35.Pryor JB, Reeder GD, Landau S. A social-psychological analysis of HIV-related stigma. Am Behav Sci. 1999;42(7):1189–1207. [Google Scholar]
- 36.Parker R, Camargo KR Jr. Pobreza e HIV/AIDS: aspectos antropológicos e sociológicos. Cad Saúde Pública. 2000;16(suppl 1):89–102. [PubMed] [Google Scholar]
- 37.Farmer P. Introducing ARVs in resource-poor settings. Plenary lecture. Paper presented at: 14th International AIDS Conference; July 10, 2002; Barcelona, Spain.
- 38.Castro A. Determinantes socio-políticos de la infección por VIH: violencia estructural y culpabilización de la víctima. Conferencia plenaria [Socio-political determinants of HIV: structural violence and the blaming of the victim. Plenary lecture]. Paper presented at: 2nd Latin American Forum on HIV/AIDS and STIs; April 10, 2003; Havana, Cuba.
- 39.Abadía-Barrero C. “I Have AIDS but I Am Happy”: Children’s Subjectivities, AIDS, and Social Responses in Brazil. Boston, Mass: Harvard School of Dental Medicine; 2002.
- 40.Foucault M. Histoire de la sexualité [The History of Sexuality]. Paris, France: Gallimard; 1976.
- 41.Bourdieu P. La distinction: Critique sociale du jugement [Distinction: A Social Critique of the Judgment of Taste]. Paris, France: Minuit; 1979.
- 42.Maluwa M, Aggleton P, Parker R. HIV- and AIDS-related stigma, discrimination, and human rights. Health Hum Rights. 2002;6(1):1–18. [Google Scholar]
- 43.Kleinman A, Wang W-Z, Li S-C, et al. The social course of epilepsy: chronic illness as social experience in interior China. Soc Sci Med. 1995;40(10): 1319–1330. [DOI] [PubMed] [Google Scholar]
- 44.Good BJ, Good M-JDV. In the subjunctive mode: epilepsy narratives in Turkey. Soc Sci Med. 1994;38(6): 835–842. [DOI] [PubMed] [Google Scholar]
- 45.Kleinman A, Kleinman J. Suffering and its professional transformation. Cult Med Psychiatry. 1991;15(3): 275–301. [DOI] [PubMed] [Google Scholar]
- 46.Farmer P, Kleinman A. AIDS as human suffering. Dædalus. 1989;118(2):135–160. [Google Scholar]
- 47.Whittaker AM. Living with HIV: resistance by positive people. Med Anthropol Q. 1992;6(4): 385–390. [Google Scholar]
- 48.Link B, Phelan J. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- 49.Link BG, Phelan J. On stigma and its public health implications. Paper presented at: Stigma and Global Health: Developing a Research Agenda; September 5–7, 2001; Bethesda, Md.
- 50.Castro A, Farmer P. Anthropologie de la violence: la culpabilisation des victimes. Notre Librairie: Revue des Littératures du Sud. 2002;148:102–108. [Google Scholar]
- 51.Farmer P. Pathologies of Power: Health, Human Rights, and the New War on the Poor. Berkeley: University of California Press; 2003.
- 52.Castro A, Farmer P. El sida y la violencia estructural: la culpabilización de la víctima. Cuadernos de Antropología Social. 2003;17:31–49. [Google Scholar]
- 53.Farmer P, Connors M, Simmons J, eds. Women, Poverty, and AIDS: Sex, Drugs, and Structural Violence. Monroe, Me: Common Courage Press; 1996.
- 54.Farmer P, Castro A. Un pilote en Haïti: de l’efficacité de la distribution d’antiviraux dans des pays pauvres, et des objections qui lui sont faites. Vacarme. 2002;19:17–22. [Google Scholar]
- 55.Castro A, Farmer P. Infectious disease in Haiti: HIV/AIDS, tuberculosis, and social inequalities. EMBO Rep. 2003;4(6 suppl):S20–S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Report on the HIV/AIDS Epidemic. Geneva, Switzerland: UNAIDS; 2004.
- 57.Castro A, Farmer P, Kim JY, et al., eds. Scaling Up Health Systems to Respond to the Challenge of HIV/AIDS in Latin America and the Caribbean. Washington, DC: Pan American Health Organization; 2003.
- 58.Lévi-Strauss C. Anthropologie structurale [Structural Anthropology]. Paris, France: Plon; 1958.
- 59.Sontag S. Illness as Metaphor. New York, NY: Farrar, Straus and Giroux; 1978.
- 60.sorcery Farmer P. Sending sickness:, politics, and changing concepts of AIDS in rural Haiti. Med Anthropol Q. 1990;4(1):6–27. [Google Scholar]
- 61.AIDS-talk Farmer P. and the constitution of cultural models. Soc Sci Med. 1994;38(6):801–809. [DOI] [PubMed] [Google Scholar]
- 62.Altman D. AIDS in the Mind of America. Garden City, NY: Doubleday; 1986.
- 63.Freire P. Pedagogía del oprimido [The Pedagogy of the Oppressed]. Madrid, Spain: Siglo XXI; 1970.
- 64.Bacchus R. Legal and ethical dimensions of HIV/AIDS. In: Howe G, Cobley A, eds. The Caribbean AIDS Epidemic. Kingston, Jamaica: University of the West Indies Press; 2000:151–185.
- 65.Walrond ER. Regional policies in relation to the HIV/AIDS epidemic in the Commonwealth Caribbean. In: Howe G, Cobley A, eds. The Caribbean AIDS Epidemic. Kingston, Jamaica: University of the West Indies Press; 2000:57–70.
- 66.Trotman L. HIV/AIDS in the workplace: the workers’ perspective. In: Howe G, Cobley A, eds. The Caribbean AIDS Epidemic. Kingston, Jamaica: University of the West Indies Press; 2000:139–150.
- 67.Francis CR. The psychological dynamics of the AIDS epidemic in the Caribbean. In: Howe G, Cobley A, eds. The Caribbean AIDS Epidemic. Kingston, Jamaica: University of the West Indies Press; 2000:186–201.
- 68.Royes H. A Cultural Approach to HIV/AIDS Prevention and Care: Jamaica’s Experience. Kingston, Jamaica: UNESCO, Cultural Policies for Development Unit; 1999. Studies and Reports, Special Series 8.
- 69.Sultan Y. Épidémiologie de l’infection par le virus LAV/HTLVIII chez les hémophiles polytransfusés en France. Résultats d’une enquête menée par 28 centres d’hémophiles. Nouv Rev Fr Hematol. 1986;28(5): 327–329. [PubMed] [Google Scholar]
- 70.Susser I, Kreniske J. Community organizing around HIV prevention in rural Puerto Rico. In: Bond GC, Kreniske J, Susser I, Vincent J, eds. AIDS in Africa and the Caribbean. Boulder, Colo: Westview Press; 1997:51–64.
- 71.Aggleton P, Parker R, Maluwa M. Stigma, Discrimination and HIV/AIDS in Latin America and the Caribbean. Washington, DC: Inter-American Development Bank; February 2003.