Abstract
Objectives. We estimated the effect of community and school district resources on the identification of children with autistic disorder.
Methods. Latent growth curve regression models were applied to school district–level data from one large state.
Results. The rate of identification of autistic disorder increased on average by 1.0 child per 10000 per year (P<.001), with statistically significant district variation. After adjustment for district and community characteristics, each increase in decile of school revenue was associated with an increase of 0.16 per 10000 children identified with autistic disorder. The proportion of economically disadvantaged children per district was inversely associated with autistic disorder cases.
Conclusions. District revenue was associated with higher proportions of children identified with autistic disorder at baseline and increasing rates of identification when measured longitudinally. Economically disadvantaged communities may need assistance to identify children with autistic spectrum disorders and other developmental delays that require attention.
Autistic spectrum disorders (ASDs) are a disabling continuum of disorders affecting 2 to 4 of every 1000 live births.1,2 The core set of defining features includes deficits in verbal and nonverbal communication and restricted and repetitive patterns of behavior.3,4 The prevalence of ASD appears to be greater than previously thought, at least in part owing to improved ascertainment.5
The etiology of ASDs is uncertain. As yet, the disorders can be defined only by a set of specific behaviors.6 Twin studies have provided evidence of a strong genetic component, and multiple genetic loci have been identified, but no association with specific phenotypes has been established.7 Specific environmental factors, such as maternal rubella, also have been associated with ASDs.8 Other potential causes of ASDs, such as diet,9–11 gastrointestinal pathology,12 chemical imbalance,13 and vaccines,14–19 have been posited but remain controversial. Evidence for a dysfunction of the neuroimmune complex is mounting, but it requires more investigation into specific mechanisms.20–24 The association between ASDs and parenting practices25 has been completely discredited, and the association with socioeconomic status26–30 is largely viewed as spurious.
Successful behavioral interventions have been developed that improve language and socialization skills and decrease stereotyped and self-injurious behavior among children with ASDs.31 In part to ensure that they receive these services, but primarily to ensure that they receive the “free, appropriate education” to which they are entitled, children with ASDs are eligible for special education services through the Individuals With Disabilities Education Act.32 ASDs were identified as a separate disabling condition qualifying children for special education in 1990.33 Special education services, available for children from birth to age 21, can include participation in specialized classrooms, one-on-one instruction, and intensive behavioral interventions.3,34–36
Despite the fact that ASDs can be identified in children as young as 18 months,37 a large majority of these children are not identified until they are of school age.38–40 Unless parents exhibit distress or proactively discuss their concerns with pediatricians, physicians are often slow to recognize disorders in children or miss them altogether, even when signs and symptoms are apparent.41–44 Even when parents do express concern, recognition and referral are often delayed. For example, Howlin and Moore found that although the average age of diagnosis was 6 years, parents generally expressed concern about related problems much earlier.39 Glascoe found that the identification of developmental disorders is usually delayed to the point that the school system—as opposed to the health system—identifies 70% of children with developmental delays.38 Palfrey and colleagues found that when identification of more polymorphous phenotypes such as ASDs was delayed, the proportion identified by the school system was closer to 80%.43 In their large-scale prevalence study of ASDs, Yeargin-Allsopp and colleagues found that more than 75% of children with ASDs were identified through the school system.2
Clearly, schools play an important role in identifying children with developmental disorders such as ASDs; however, their methods of identification are suboptimal. For example, Yeargin-Allsopp found that in one metropolitan area, 18% of children who qualified for a diagnosis of ASDs according to study criteria were receiving special education services but had not been recognized as having ASDs by the school.2 There is little research, however, on the characteristics of schools and school systems that are associated with timely recognition and provision of services for children with ASDs. In their study of all 50 states, Lester and Kelman found that state policies were highly predictive of rates of identified learning disabilities, whereas state sociodemographic characteristics were not.45 They acknowledged, however, that it is difficult to summarize the sociodemographic characteristics of an entire state, a factor that may have influenced their results. They also pointed to the need for more fine-grained analysis.
One possibility is that school districts with greater resources are more effective at identifying and providing services to children with ASDs. Services for children with ASDs are often costly and can represent a considerable drain on related resources.46,47 The US Department of Education reports that there are considerable inequities in both revenues and special education spending by district across the United States.48 To our knowledge, there is no research that examines how these district characteristics influence the recognition of and provision of services to children with special needs.
The current study used data from one large state to examine differences in the proportion of children identified with autistic disorder and the rate at which they were identified, as a function of school district resources. We focused on autistic disorder rather than the spectrum of disorders because autistic disorder represents the most severe and phenotypically distinct end of the spectrum,49 and is therefore the most reliably and validly diagnosed.50,51
METHODS
Data Source and Sample
Administrative data from the Texas Education Agency (TEA) for school years 1994/1995 to 2000/2001 were analyzed. Data and data description are available at the TEA Web site (http://198.214.99.202). In compliance with the Texas Education Code, the Public Education Information Management System contains data necessary for the legislature and the TEA to perform their legally authorized functions in overseeing public education. The database consists of student demographics, student academic records, and school personnel, financial, and organizational information. Numbers of autistic disorder cases per district were obtained by special request from the TEA. Data were from all 1040 school districts that were in existence for the total study period. These districts represented approximately 4 million children enrolled in grades kindergarten through 12.
Measures
Diagnosis of autistic disorder was abstracted from the school record for each year of the study period. Diagnoses were made by qualified special education psychologists employed by the TEA or by psychologists or medical doctors outside the TEA system. While diagnoses were not standardized, there is considerable evidence that diagnoses of autistic disorder are made with good reliability and specificity in the field.50–52 Autism rates for each district were obtained by calculating the ratio of the total number of autistic children to the total enrolled in that district for a specific school year.
District and population resources, as described in each of the variables listed below (in italics), were calculated as of the 1994/1995 school year. In response to concerns that resources may have shifted over the course of the study period, comparisons were made for each year of the study period. Results suggest that 70% of districts remained within the same decile of resources over the course of the study. An additional 28.4% varied by ±1 decile, suggesting relative stability over the course of the study.
District revenue included budgeted revenue from all local, state, and federal sources, except for receipts from the sale of bonds and other revenues budgeted in the capital projects fund. When capital projects are excluded, this amount includes only funds budgeted to be spent on students. Deciles of revenue were calculated from these data. This variable is intentionally unadjusted for the number of students per district to avoid the assumption that amounts spent on students in large districts are comparable to those spent on smaller districts. We appropriately adjusted for district wealth and student population in the multivariate analysis.
Average teacher salary was calculated as the total salary of teachers divided by the number of full-time-equivalent teachers. The total salary amount was base pay only; any supplements were excluded.
District population wealth was calculated as the district’s total taxable property value in 1994 as determined by the Comptroller’s Property Tax Division (CPTD), divided by the total number of students in the district in 1994/1995. Property value was determined by the CPTD as part of its annual study, which attempts to present uniformly appraised property valuations statewide. The CPTD value is calculated by applying ratios created from uniform independent appraisals to the district’s assessed valuations.
Racial composition was accounted for by the proportion of White children enrolled in schools within each district.
Total number of students was calculated as all enrolled students as of October 28, 1994, in grades prekindergarten through 12, who attended at least 1 day of school for that school year. Statewide, 6975 students, or 0.2% of all students, were enrolled in but never attended school.
Proportion of economically disadvantaged students was calculated as the percentage of students who were eligible for free meals under the National School Lunch and Child Nutrition Program, reduced-price meals under the National School Lunch and Child Nutrition Program, or other public assistance.
Proportion of students enrolled in special education was calculated as the number of students enrolled in special education divided by the total number of students enrolled in each district.
Number of teachers per student was calculated as the total number of students divided by the total number of full-time-equivalent teachers.
Analyses
A structural modeling approach employing latent growth curve modeling (LGCM) was used to determine the rate of change in autistic disorder over the 7-year period. This rate of change was then regressed onto independent variables of interest. LGCM is a well-documented strategy for modeling change over time.53 In contrast to standard autoregressive models, which estimate the intradistrict change between each year of the study, LGCM estimates the full trajectory of change across each district’s measurement points.54 The parameters of interest are the intercept, which provides an estimate of the proportion of children diagnosed with autistic disorder at baseline, and the slope, which provides an estimate of the trajectory of change in that proportion over time. The variances of the intercept and slope are also of interest because they indicate whether there is heterogeneity among the slopes across districts. Variation in the intercept or slope indicates the extent to which there are differences among districts. We estimated the model by using maximum likelihood methods with AMOS software.55
In addition to the χ2 test,56 we used 2 common test statistics to assess LGCM goodness of fit: the root mean square error of approximation and the comparative fit index. A root mean square error of approximation of 0.05 or less indicates a close fit to the data.57,58 A comparative fit index below 0.95 suggests model misspecification, while values from 0.95 to 1.0 indicate adequate to excellent fit.59
RESULTS
Table 1 ▶ provides summary statistics of the variables used in the analysis. There was considerable variation in most variables. A comparison of the medians, means, and ranges suggests that with regard to district revenue and wealth, as well as number of students, schools, and students per teacher, there were a few outlying districts with large values that skewed the distribution of these variables. For example, the mean district revenue was $17.4 million, with a range of $100 000 to $966.7 million.
TABLE 1—
Baseline Descriptive Statistics for School Districts (n = 1040): Texas, 1994/1995 School Year
| Variable | Median | Mean | SD | Minimum | Maximum |
| District revenue, $ millions | 4.56 | 17.4 | 52.2 | 0.1 | 966.7 |
| No. of students | 856 | 3535 | 10 753 | 13 | 202 363 |
| White students, % | 72 | 65.6 | 26.25 | 0 | 100 |
| Economically disadvantaged students, % | 44.6 | 45.4 | 18.42 | 0 | 100 |
| No. of schools | 3.0 | 6.2 | 14.32 | 1 | 263 |
| Schools receiving special education, % | 13.0 | 13.7 | 4.53 | 0 | 37 |
| Teacher salary, $ | 27 063 | 27 271 | 2294 | 19 580 | 35 515 |
| No. of students per teacher | 13.6 | 13.39 | 2.89 | 4.3 | 57.54 |
| District wealth, $ | 134 102 | 219 606 | 364 870 | 0 | 6 130 479 |
Note. For an explanation of how the variables were calculated, see Methods section.
Results of the LGCM demonstrate that in school year 1994/1995, the average proportion of children identified with autistic disorder was 2.5 per 10 000 (P < .001). The rate of identification of autistic disorder increased on average by 1.0 child per 10 000 per year (P < .001). The LGCM also showed that there was significant variability associated with both the baseline and rates of change over time (P < .001 and P < .01, respectively), indicating that the rates of autism at baseline and the change over time differed significantly across counties. The latent growth model demonstrated an adequate fit to the data, with a comparative fit index of 0.99 and a root mean square error of approximation of 0.06.
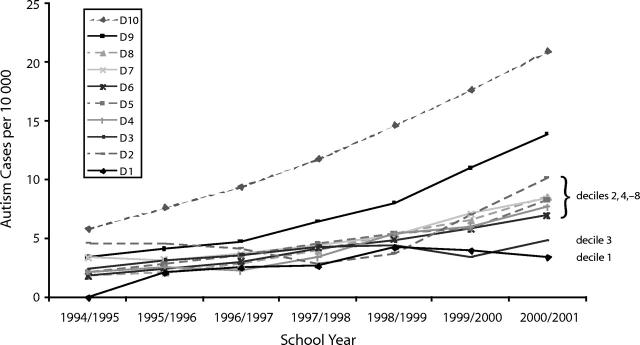
Figure 1 ▶ depicts the rate of identified cases of autistic disorder over the course of the study period, as a function of decile of district revenue. Over the course of the study, those districts within the highest (10) and second highest (9) revenue deciles experienced more than a 300% increase in rates of identification. Rates of change among deciles 4 through 8 were relatively indistinguishable. Deciles 1 and 3 experienced almost no change in the rate of identification of autistic disorder, whereas decile 2 experienced a doubling in the rate of identification. By the end of the study period, deciles 9 and 10 had rates of identification that were far greater than those of districts in the lower deciles of revenue. The statistical difference between the slope trajectories across deciles was tested by a χ2 difference test. The slopes of deciles 9 and 10 were significantly different from each other (P< .0001) and from those of the other deciles. While deciles 1 and 3 were not significantly different from each other, they were statistically different from the other deciles (P< .001). There were no significant differences between deciles 2, 4, 5, 6, 7, and 8.
FIGURE 1—
Rates of child autism in Texas school districts from 1994 to 2001, by unadjusted decile of district resources.
Table 2 ▶ shows the results of the LGCM. Three separate models are presented. In the first, the rate of change was regressed onto district revenue. In the second, it was regressed onto revenue and community characteristics, and in the third, other school characteristics were added as well. Model 1 shows the positive direct effect of district revenue on the rate of change in autistic disorder. District revenue accounted for 9% of the variance in the rate of change. Model 2 shows the additional contribution of community characteristics, which accounted for another 5.5% of the variance in the rate of change. In this model, the percentage of economically disadvantaged children was inversely related to the increase in the proportion of children identified with autistic disorder, and the predictive value of district revenue remained relatively unchanged. In model 3, both associations remained significant after adjustment for other school district characteristics (average teacher salary, total number of students, percentage in special education, and student/teacher ratio). Among the school characteristics entered into the model, only the total number of students in the district was directly associated with the rate of change in autistic disorder.
TABLE 2—
Regression Models (Coefficient andPValue) Predicting Rate of Change in Autism Among Children in Texas School Districts
| Revenue Only | Revenue and District Community Characteristics | Revenue, District Community, and Other District Characteristics | ||||
| District revenue, deciles | 0.164 | <.001 | 0.165 | <.001 | 0.151 | <.001 |
| District wealth | . . . | . . . | 0.000 | .612 | 0.000 | .310 |
| % of economically disadvantaged students | . . . | . . . | −0.018 | <.001 | −0.018 | <.001 |
| % of White students | . . . | . . . | −0.002 | .620 | −0.001 | .851 |
| Teacher salary, $ thousands | . . . | . . . | . . . | . . . | −0.001 | .860 |
| Total no. of students, hundreds | . . . | . . . | . . . | . . . | 0.002 | <.001 |
| % of students in special education | . . . | . . . | . . . | . . . | −0.005 | .932 |
| No. of students per teacher | . . . | . . . | . . . | . . . | −0.049 | .074 |
| Proportion of high schools in district | −0.862 | .008 | ||||
| Variance (R2 ), % | 9.0 | 14.5 | 18.2 | |||
Note. Boldface indicates that the regression coefficient is a significant predictor.
To address the concern that smaller districts had a greater proportion of schools that were high schools, we adjusted the multivariate analysis to include this proportion as a covariate. The coefficient between revenue and the rate of change in ASDs was unaffected (β = .151, SE = .03, P < .001). There was a significant inverse association between the proportion of schools in a district that were high schools and rate of autistic disorder.
DISCUSSION
The results of this study suggest that the increase in the identification of children with autistic disorder in Texas closely paralleled nationwide trends.60,61 Our findings also suggest that school district resources, as measured by district revenue, are associated with an increased rate of identifying children with autistic disorder. This association remained after adjustment for a variety of school district factors. Districts with more students also had a higher rate of identification of children with autistic disorder on average, while those with a higher proportion of economically disadvantaged students had lower rates of identification on average.
By the end of the study period, there was considerable variability in the prevalence of children with recognized autistic disorder across districts. Among districts in the top decile of revenue, 21 children per 10000 were diagnosed with autistic disorder, while among districts in the lowest decile, the diagnosis rate was 3.5 children per 10000.
Limitations
At least 4 study limitations should be considered. Perhaps most important, the true community district-level prevalence of autistic disorder—as opposed to the treated prevalence—is not certain. Small area variation in this prevalence would quite probably affect the proportion of children in each district identified with autistic disorder. Recent epidemiological studies suggest no difference in the prevalence of autistic disorder across a variety of factors, including race, ethnicity, and socioeconomic status.2 It is possible, however, that parents of children with this disorder may move into districts with greater resources, inflating the prevalence for those districts. This in and of itself would be an important finding, since it suggests that districts with less revenue are not meeting the needs of these families.
A second limitation is that district and population resources measured in 1994 may have changed over time, affecting the observed association of resources and rise in diagnosed autism. The potential effect of this limitation is ameliorated, however, by the fact that the overwhelming majority of districts either remained within the same decile level of resources or changed by only one decile level.
Third, it should be emphasized that this is an ecological study that precludes interpretation at the individual level. We have used aggregate units (e.g., district-level data) in this analysis to investigate differential rates of change in autism at the district level. It follows that individual data are required to make a better case for the suggested conclusion that resource-poor districts inadequately address a valid demand for ASD services. Further study of ASDs and service inequalities would require collecting additional data about family, child, and specific school characteristics. This research suggests the need to incorporate multilevel modeling strategies to better understand variation at all levels of analysis, both at the individual and the district level.
Finally, these results are from one state and therefore may not be generalizable to other parts of the country, especially given that regulations regarding funding for autism-related services may vary from state to state.
Implications
Despite these limitations, there are important implications related to these findings. It is likely that district revenue is an accurate proxy for funds spent on students. Because these analyses adjusted for the number of students in the district, revenues reflected per-pupil spending. Districts with higher rates of per-pupil spending had prevalence rates of diagnosed autistic disorder that approached the known community prevalence rates. The rate of increase in diagnosis in these districts suggests that the proportion will continue to rise.
On the other hand, districts that spent the least amount per student were serving very low proportions of children diagnosed with autistic disorder, with rates of change that did not appear to be approaching the known community prevalence any time in the near future. The fact that this finding was not altered by the inclusion of the total number of children receiving special education services suggests that in districts with greater revenue, children with autistic disorder are diagnosed and enter the special education system differently than other children with special needs. Because the effect of district revenue on the rates of diagnosed autistic disorder did not vary as a function of measures of community economic status, it is likely that the schools and school policies play a specific role in identifying these children, regardless of the resources of the families whose children are enrolled.
There are also implications related to the fact that the proportion of economically disadvantaged students in a district had an independent effect on the rates of diagnosed autistic disorder. Although rigorous studies have found no association between higher socioeconomic status and ASDs, researchers have noted that families with greater economic resources are more likely to obtain treatment and other services for their children.26–30 Families with fewer economic resources may interpret their children’s behavior in a way that does not lead to medical intervention. For example, Bussing and colleagues found that families’ willingness to apply a medical label to their children’s attention deficit/hyperactivity symptoms varied as a function of socioeconomic factors.62
Even when families are aware of their children’s disorder, they may lack the resources to advocate with schools for appropriate services. Wildin and Barnett pointed specifically to the morass of organizational and legal actions in Texas that must occur for children with special needs to receive appropriate educational services.63 Other researchers have also pointed out the complexity of laws governing special education and the difficulties in interpreting rights and responsibilities.64
Districts with more students had on average greater rates of children diagnosed with autistic disorder. Student population may be a proxy for urbanicity and access to academic health settings where there is a greater familiarity with developmental delays. It may also be that a critical mass of students is required for standardized service provision to be put into place. For example, schools may not initiate a classroom specifically devoted to the needs of children with ASDs unless they have identified enough children with the disorder. Such resources, once they are available, may in turn facilitate more identification.
A final implication relates to the finding that districts with a higher proportion of schools that were high schools had lower rates of children diagnosed with autistic disorder. It may be that even when children are diagnosed with and receive services for ASDs in elementary and middle school, those services are not continued into the high school years. Although further study with school-level data is required to test this hypothesis, the potential lack of services for adolescents with ASDs has important implications for service planning.
Further research is needed to determine which revenue and spending patterns are associated with improved ascertainment. In the meantime, it is important to consider providing resources to poorer districts and economically disadvantaged communities to help them identify children with ASDs and other developmental delays that require attention.
Acknowledgments
This work was supported by the Department of Family and Community Medicine at the University of Texas Health Science Center San Antonio.
Human Participant Protection No institutional review board approval was required for this study.
Contributors R. F. Palmer, S. Blanchard, and D. S. Mandell jointly participated in the conception and design of the article. With the other authors, C. R. Jean offered critical interpretation of the results and contributed important intellectual content. R. F. Palmer and S. Blachard acquired and analyzed the data. D. S. Mandell had primary responsibility for drafting the article.
Peer Reviewed
References
- 1.Bryson S. Epidemiology of autism—brief report. J Autism Dev Disord. 1996;26:165–167. [DOI] [PubMed] [Google Scholar]
- 2.Yeargin-Allsopp M, Rice C, Karapurkar T, Doernberg N, Boyle C, Murphy C. Prevalence of autism in a US metropolitan area. JAMA. 2003;289(1):49–55. [DOI] [PubMed] [Google Scholar]
- 3.Volkmar F, Cook E, Pomeroy J, Realmuto G, Tanguay P. Practice parameters for the assessment and treatment of children, adolescents and adults with autism and other pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry. 1999;38(12 suppl): 32S–54S. [DOI] [PubMed] [Google Scholar]
- 4.Filipek P, Accardo P, Ashwal S, et al. Practice parameter: screening and diagnosis of autism. Neurology. 2000;55:468–479. [DOI] [PubMed] [Google Scholar]
- 5.Wing L. The definition and prevalence of autism: a review. Eur Child Adolesc Psychiatry. 1993;2:61–74. [DOI] [PubMed] [Google Scholar]
- 6.Wing L. The autistic spectrum. Lancet. 1997;350: 1761–1766. [DOI] [PubMed] [Google Scholar]
- 7.Folstein S, Rosen-Sheidley B. Genetics of autism: complex aetiology for a heterogeneous disorder. Nat Rev Genet. 2001;2(12):943–955. [DOI] [PubMed] [Google Scholar]
- 8.Dykens E, Volkmar F. Medical conditions associated with autism. In: Cohen D, Volkmar F, eds. Handbook of Autism and Pervasive Developmental Disorders. 2nd ed. New York, NY: Wiley; 1997:388–407.
- 9.Brudnak M. Application of genomeceuticals to the molecular and immunological aspects of autism. Med Hypotheses. 2001;57(2):186–191. [DOI] [PubMed] [Google Scholar]
- 10.Garvey J. Diet in autism and associated disorders. J Fam Health Care. 2002;12(2):34–38. [PubMed] [Google Scholar]
- 11.Knivsber A, Reichelt K, Nodland M. Reports on dietary intervention in autistic disorders. Nutr Neurosci. 2001;4(1):25–37. [DOI] [PubMed] [Google Scholar]
- 12.Wakefield A, Puleston J, Montgomery J, Anthony A, O’Leary J, Murch S. The concept of enterocolonic encephalopathy, autism and opioid receptor ligands. Aliment Pharmacol Ther. 2002;16(4):663–674. [DOI] [PubMed] [Google Scholar]
- 13.Levy S, Hyman S. Alternative/complementary approaches to treatment of children with autistic spectrum disorders. Infants Young Child. 2002;14(3): 33–42. [Google Scholar]
- 14.DeStefano F, Chen R. Autism and measles, mumps, and rubella vaccine: no epidemiological evidence for a causal association. J Pediatr. 2000;136(1): 125–126. [PubMed] [Google Scholar]
- 15.DeStefano F, Chen R. Autism and measles-mumps-rubella vaccination: controversy laid to rest? CNS Drugs. 2001;15(11):831–837. [DOI] [PubMed] [Google Scholar]
- 16.Fombonne E, Chakrabarti S. No evidence for a new variant of measles-mumps-rubella-induced autism. Pediatrics. 2001;108(4):E58. [DOI] [PubMed] [Google Scholar]
- 17.Taylor B, Miller E, Farrington C, et al. Autism and measles, mumps, and rubella vaccine: no epidemiological evidence for a causal association. Lancet. 1999; 353:2026–2029. [DOI] [PubMed] [Google Scholar]
- 18.Geier M, Geier D. Thimerisol in childhood vaccines, neurodevelopmental disorders and heart disease in the United States. J Am Physicians Surg. 2003;8(1): 6–11. [Google Scholar]
- 19.Singh V, Lin S, Newell E, Nelson C. Abnormal measles-mumps-rubella antibodies and CNS autoimmunity in children with autism. J Biomed Sci. 2002;9(4): 359–364. [DOI] [PubMed] [Google Scholar]
- 20.Licinio J, Alvarado I, Wong M-L. Autoimmunity in autism. Mol Psychiatry. 2002;7(4):329. [DOI] [PubMed] [Google Scholar]
- 21.Singh V. Plasma increase of interleukin-12 and interferon-gamma. Pathological significance in autism. J Neuroimmunology. 1996;66(1–2):143–145. [DOI] [PubMed] [Google Scholar]
- 22.Singh V, Warren R, Averett R, Ghaziuddin M. Circulating autoantibodies to neuronal and glial filament proteins in autism. Pediatr Neurol. 1997;17(1):88–90. [DOI] [PubMed] [Google Scholar]
- 23.Singh V, Warren R, Odell J, Warren W, Cole P. Antibodies to myelin basic protein in children with autistic behavior. Brain Behav Immun. 1993;7(1): 97–103. [DOI] [PubMed] [Google Scholar]
- 24.Stubbs E, Magenis R. HLA and autism. J Autism Dev Disord. 1980;10(1):15–19. [DOI] [PubMed] [Google Scholar]
- 25.DeMyer M, Pontius W, Norton J, Barton S, Allen J, Steele R. Parental practices and innate activity in normal, autistic and brain-damaged infants. J Autism Child Schizophr. 1972;2:49–66. [DOI] [PubMed] [Google Scholar]
- 26.Ritvo E, Freeman B, Pingree C, et al. The UCLA–University of Utah epidemiologic survey of autism: prevalence. Am J Psychiatry. 1989;146(2):194–199. [DOI] [PubMed] [Google Scholar]
- 27.Gillberg C, Schaumann H. Social class and infantile autism. J Autism Dev Disord. 1982;12(3):223–228. [DOI] [PubMed] [Google Scholar]
- 28.Wing L. Childhood autism and social class: a question of selection. Br J Psychiatry. 1980;137: 410–417. [DOI] [PubMed] [Google Scholar]
- 29.Tsai L, Stewart M, Faust M, Shook S. Social class distribution of fathers of children enrolled in the Iowa Autism Program. J Autism Dev Disord. 1982;12(3): 211–221. [DOI] [PubMed] [Google Scholar]
- 30.Steffenburg S, Gillberg C. Autism and autistic-like conditions in Swedish rural and urban areas: a population study. Br J Psychiatry. 1986;149:81–87. [DOI] [PubMed] [Google Scholar]
- 31.Matson J, Benavidez D, Compton L, Paclawskyj T, Baglio C. Behavioral treatment of autistic persons: a review of research from 1980 to the present. Res Dev Disabil. 1996;17(6):433–465. [DOI] [PubMed] [Google Scholar]
- 32.Individuals With Disabilities Education Act Amendments of 1997, Pub L No. 105–17, 111 Stat 38 (1997).
- 33.Pub L No. 94–142, 89 Stat 773, amended by Pub L No. 101–476, 104 Stat 1141 (1990) (codified at 20 USC §1400 et seq. [1994]).
- 34.Rapin I. Autistic children: diagnosis and clinical features. Pediatrics. 1991;87(2):751–760. [PubMed] [Google Scholar]
- 35.Campbell M, Schopler E, Cueva J, Hallin A. Treatment of autistic disorder. J Am Acad Child Adolesc Psychiatry. 1996;35(2):134–143. [DOI] [PubMed] [Google Scholar]
- 36.Committee on Children With Disabilities. Technical report: the pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics. 2001;107(5):E85. [DOI] [PubMed] [Google Scholar]
- 37.Baron-Cohen S, Wheelwright S, Cox A, et al. Early identification of autism by the Checklist for Autism in Toddlers (CHAT). J R Soc Med. 2000;93(10): 521–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Glascoe F. Evidence-based approach to developmental and behavioural surveillance using parents’ concerns. Child Care Health Dev. 2000;26(2):137–149. [DOI] [PubMed] [Google Scholar]
- 39.Howlin P, Moore A. Diagnosis of autism. A survey of over 1200 patients in the UK. Autism. 1997;1:135–162. [Google Scholar]
- 40.Mandell D, Listerud J, Levy S, Pinto-Martin J. Race differences in the age of diagnosis among Medicaid-eligible children with autism. J Am Acad Child Adolesc Psychiatry. 2002;41(12):1447–1453. [DOI] [PubMed] [Google Scholar]
- 41.Dulcan M, Costello E, Costello A, Edelbrock C, Brent D, Janiszewski S. The pediatrician as gatekeeper to mental healthcare for children: do parents’ concerns open the gate? J Am Acad Child Adolesc Psychiatry. 1990;29(3):453–458. [DOI] [PubMed] [Google Scholar]
- 42.Horwitz S, Leaf P, Leventhal J. Identification of psychosocial problems in pediatric primary care: do family attitudes make a difference? Arch Pediatr Adolesc Med. 1998;152(4):367–371. [DOI] [PubMed] [Google Scholar]
- 43.Palfrey J, Singer J, Walker D, Butler J. Early identification of children’s special needs: a study in five metropolitan communities. J Pediatr. 1987;111:651–659. [DOI] [PubMed] [Google Scholar]
- 44.Shevell M, Majnemer A, Rosenbaum P, Abrahamowicz M. Profile of referrals for early childhood developmental delay to ambulatory subspecialty clinics. J Child Neurol. 2001;16(9):645–650. [DOI] [PubMed] [Google Scholar]
- 45.Lester G, Kelman M. State disparities in the diagnosis and placement of pupils with learning disabilities. J Learn Disabil. 1997;30(6):599–607. [DOI] [PubMed] [Google Scholar]
- 46.Jarbrink K, Knapp M. The economic impact of autism in Britain. Autism. 2001;5(1):7–22. [DOI] [PubMed] [Google Scholar]
- 47.Jacobson J, Mulick J. System and cost research issues in treatments for people with autistic disorders. J Autism Dev Disord. 2000;30(6):585–593. [DOI] [PubMed] [Google Scholar]
- 48.Parrish T, Hikido C, Fowler W. Inequalities in Public School District Revenues. Washington, DC: US Dept of Education; 1998.
- 49.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
- 50.Eisenmajer R, Prior M, Leekam S, et al. Comparison of clinical symptoms in autism and Asperger’s disorder. J Am Acad Child Adolesc Psychiatry. 1996; 35(11):1523–1531. [DOI] [PubMed] [Google Scholar]
- 51.Hill A, Bolte S, Petrova G, Beltcheva D, Tacheva S, Poustka F. Stability and interpersonal agreement of the interview-based diagnosis of autism. Psychopathology. 2001;34(4):187–191. [DOI] [PubMed] [Google Scholar]
- 52.Mahoney W, Szatmari P, MacLean J, et al. Reliability and accuracy of differentiating pervasive developmental disorder subtypes. J Am Acad Child Adolesc Psychiatry. 1998;37(3):278–285. [DOI] [PubMed] [Google Scholar]
- 53.McArdle J. Dynamic but structural equation modeling of repeated measures data. In: Nesselroade J, Cattell R, eds. Handbook of Multivariate Experimental Psychology. New York, NY: Plenum; 1986:561–614.
- 54.Williet J, Sayer A. Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychol Bull. 1994;116:363–381. [Google Scholar]
- 55.Arbuckle J. Analysis of Moment Structures—AMOS [software]. Chicago, Ill: Small Waters Corporation; 1994.
- 56.Joreskog K. A general approach to confirmatory maximum likelihood factor analysis. Psychometrika. 1969;34:183–202. [Google Scholar]
- 57.Bollen K, Long J, eds. Testing Structural Equation Models. Newbury Park, Calif: Sage Publications; 1993.
- 58.Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, eds. Testing Structural Equation Models. Newbury Park, Calif: Sage Publications; 1993:136–162.
- 59.Bentler P. Comparative fit indexes in structural models. Psychol Bull. 1990;10:238–246. [DOI] [PubMed] [Google Scholar]
- 60.Dales L, Hammer S, Smith N. Time trends in autism and in MMR immunization coverage in California. JAMA. 2001;285(9):1183–1185. [DOI] [PubMed] [Google Scholar]
- 61.US Dept of Education. Twenty-Third Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act. Jessup, Md: Bureau of Special Education; 2001.
- 62.Bussing R, Schoenberg N, Perwien A. Knowledge and information about ADHD: evidence of cultural differences among African-American and white parents. Soc Sci Med. 1998;46(7):919–928. [DOI] [PubMed] [Google Scholar]
- 63.Wildin S, Barnett S. A guide to educational services and financial assistance for children with disabilities. Tex Med. 1996;92(11):57–63. [PubMed] [Google Scholar]
- 64.Dalton M. Education rights and the special needs child. Child Adolesc Psychiatr Clin North Am. 2002; 11(4):859–868. [DOI] [PubMed] [Google Scholar]