Abstract
Objective:
To compare the efficacy of endoscopic retrograde cholangiopancreatography ± endoscopic sphincterotomy (ERCP ± ES) versus traditional conservative management in early gallstone pancreatitis with persistent ampullary obstruction (GSP + AO).
Summary Background Data:
The effectiveness of early ERCP ± ES in this setting is controversial.
Methods:
Sixty-one consecutive patients with GSP + AO within 48 hours from the onset of symptoms were randomized to receive either conservative treatment and selective ERCP ± ES after 48 hours (control group, 31 patients) or initial conservative treatment and systematic ERCP ± ES within 48 hours if obstruction persisted 24 hours or longer (study group, 30 patients). Patient outcome was compared in relation to treatment groups and to duration of obstruction.
Results:
In the control group, 22 patients disobstructed spontaneously within 48 hours; 3 of the remaining 9 patients underwent ERCP ± ES and none had impacted stones. In the study group, 16 patients disobstructed spontaneously and 14 underwent ERCP within 48 hours from the onset of symptoms; impacted stones were found and extracted by ES in 79% (11 of 14) of these.
Patients:
There were no deaths in either group. Patients in the study group showed a shorter period of obstruction (P = 0.016) and a lower rate of immediate complications (P = 0.026) than controls. Patients with obstruction lasting ≤48 hours regardless of the treatment group had fewer immediate complications than those whose obstruction persisted longer (P < 0.001).
Conclusions:
This study shows that in patients with GSP + AO limiting the duration of obstruction to not longer than 48 hours by ERCP + ES decreased morbidity.
The efficacy of early endoscopic retrograde cholangiopancreatography ± endoscopic sphincterotomy was compared with conservative management in gallstone pancreatitis with persistent ampullary obstruction. Sixty-one prospectively randomized patients within 48 hours from the onset of symptoms showed that shortening the duration of obstruction by endoscopic sphincterotomy reduces significantly the morbidity of early gallstone pancreatitis.
The first evidence of the role of gallstone obstruction in the genesis of gallstone pancreatitis (GSP) was provided in 1901, when Opie reported finding a gallstone impacted at the ampulla of Vater in a patient dying from acute pancreatitis.1 In 1974, we showed that gallstone impaction causing pancreatitis is usually a transient rather than a persistent phenomenon since most of the offending stones migrate rapidly and can be found in feces.2
Currently, most authors agree that transient obstruction by a migrating gallstone initiates the pancreatitis, but there is no consensus on the events that follow stone impaction and its effect on the course of pancreatitis. A number of experimental3,4 and clinical5–8 investigations have showed that the presence of common duct stones impacts the outcome of pancreatitis. Wilson et al reported finding common duct stones in 59% of 39 patients with fatal GSP,9 and Corfield et al found impacted stones in 56% of 25 patients who died from GSP.10 We showed that severe pancreatic lesions developed in 10.6% of 97 patients with GSP when gallstone obstruction resolved within 48 hours, but in 84.6% if obstruction persisted longer.11 Nevertheless, other investigators questioned the relationship between duration of obstruction and severity of pancreatitis as they observed hemorrhagic pancreatitis with the same frequency during early or delayed surgery and regardless of the presence of impacted stones.12,13
As the referenced findings are not mutually exclusive, the benefit of early interventional disobstruction in patients with GSP remains controversial. Four randomized trials comparing conservative treatment with early ERCP ± ES have come to contradictory conclusions.14–17 The inclusion of patients with non-biliary pancreatitis, the exclusion of patients with both obvious and not apparent obstruction (bilirubin level >5 mg/dL and <2.4 mg/dL, respectively) and the uncertainty of the term “early” as a result of measuring the time from admission in some of these reports, preclude an accurate assessment of the therapeutic value of ERCP. Meanwhile, GSP remains a common acute abdominal condition with a mortality rate of approximately 6% as reported from the placebo arm of treatment studies.18
Based on the results of our previous investigation, we hypothesized that duration of ampullary obstruction is an important determinant in the outcome of GSP; therefore, shortening the period of obstruction by ES might reduce the severity of GSP. To address these issues, we undertook a prospective randomized study narrowing the scope of investigation to those patients with GSP and documented concomitant ductal obstruction presenting within 48 hours from the onset of symptoms. The efficacy of ES on patients' outcome within such period was compared with that of conservative treatment.
MATERIALS AND METHODS
Study Design
All patients with GSP admitted to the Emergency Surgery Service of the Los Angeles County and University of Southern California Medical Center were evaluated for study eligibility. The criteria for enrollment are listed in Table 1. All patients received initially supportive treatment, including broad-spectrum antibiotics, analgesics, nasogastric tube aspiration, and routine right upper quadrant ultrasonography. Admission right upper quadrant ultrasound (US) was performed in 56 (92%) of the 61 patients: control group (n = 27) and study group (n = 29). The median time interval between admission US and onset of symptoms was 28.5 hours (range, 8–120 hours). US failed to evaluate the pancreas in 3 patients. Enhanced CT scan and magnetic resonance cholangiography (MRC) were used at the attending surgeon's discretion, particularly as initial procedure when US was not performed or the pancreas not visualized. These methods were also used in addition to US in the patients with suspicion of complications. CT scan was performed in 7 patients: control group (n = 4) and study group (n = 3) with median time interval of 4 days from admission. MRC was performed in 8 patients (control group, n = 7; and study group, n = 1) with a median interval of 4.2 days after admission.
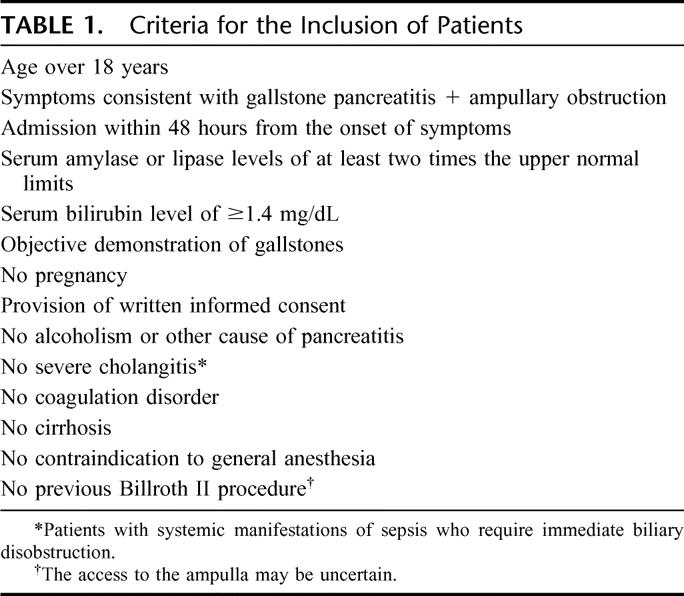
TABLE 1. Criteria for the Inclusion of Patients
Ampullary patency was monitored from admission as previously described by Acosta et al.19 The presence of the triad: severe and continuous epigastric pain, bile-free gastric aspirate, and elevated serum bilirubin level (determined every 6 hours), indicated obstruction, while relief of pain, falling bilirubin level, and appearance of bile in the gastric aspirate, defined spontaneous disobstruction. The condition of the ampulla was defined as “obstructed” or “patent” based on clinical, biochemical, and imaging criteria. ERCP ± ES and intraoperative cholangiography (IOC) were used as gold standard in all the patients with a positive diagnosis of obstruction, and also in those with a negative diagnosis when these procedures were performed to rule out mobile common duct stones within the first week of admission.
Total duration of obstruction (defined as the time elapsed from the onset of symptoms until spontaneous or operative disobstruction) was determined and recorded in all cases.
The severity of pancreatitis was assessed at admission and before treatment according to the Ranson20 and Acosta et al19 criteria. Comorbidity was assessed by a score index proposed by Charlson et al.21
Randomization
Eligible patients were randomized by a computer-generated list and sealed envelopes, to one of the 2 treatment groups: control group (conservative treatment ± selective ERCP ± ES after 48 hours) or study group (initial conservative treatment and ERCP ± ES within 48 hours if obstruction persisted for 24 hours or longer). All qualified patients provided written consent prior to randomization.
Therapeutic Approach
The management algorithm is represented in Figure 1. In the control group, supportive measures were maintained until a favorable clinical and laboratory response was obtained. ERCP ± ES was selectively performed after 48 hours from the onset of symptoms at the treating physician's discretion in patients with associated persistent jaundice or cholangitis. In the study group, patients experiencing spontaneous disobstruction within 48 hours continued with supportive measures until the resolution of pancreatitis. Those who remained obstructed underwent ERCP between 24 and 48 hours from the onset of symptoms complemented with ES if obstruction was confirmed. Elective cholecystectomy was carried out during the initial hospitalization and once the pancreatitis has subsided in most patients of both groups.
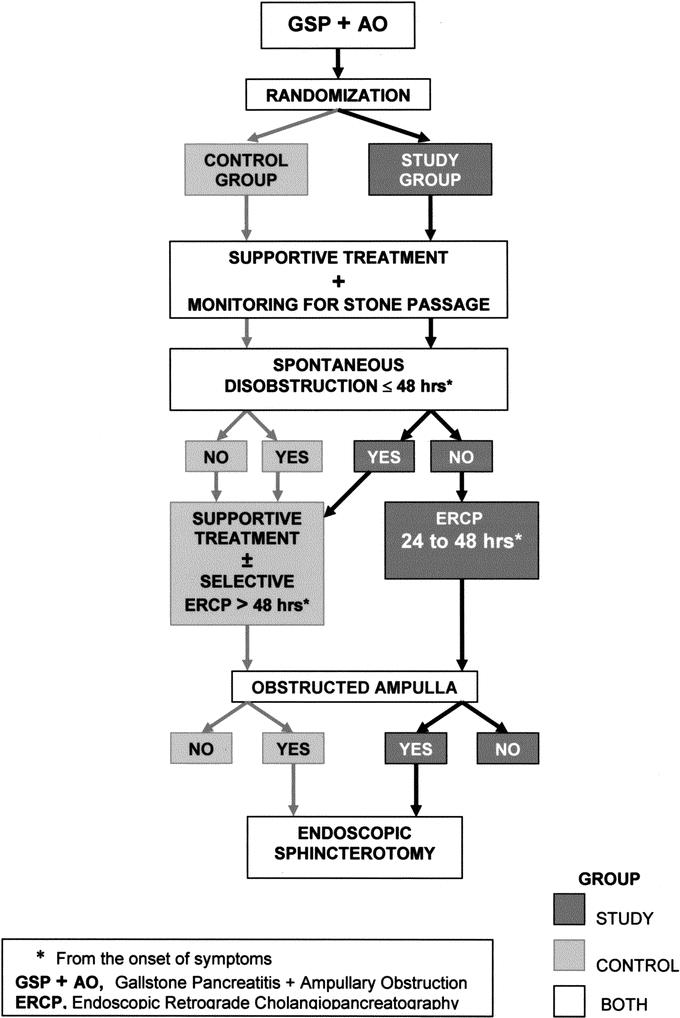
FIGURE 1. Gallstone pancreatitis with ampullary obstruction. Management algorithm.
Assessment of Outcome Measures
Outcome measures were mortality and morbidity related to pancreatitis and to ERCP ± ES during hospitalization and within 30 days after discharge. Morbidity related to pancreatitis was classified according to a modified Atlanta criteria.22 We added “pancreatic phlegmon,” which, according to several authors including us, is not adequately defined by the Atlanta criteria. A diagnosis of pancreatic phlegmon was based upon the presence of typical clinical futures such as severe and persistent epigastric pain and tenderness (or palpable mass), nausea or vomiting with protracted or episodic elevation of amylase and bilirubin levels. Imaging studies confirmed the clinical diagnosis when revealing the presence of a solid pancreatic mass with increased echogenicity, normal pancreatic enhancement, and signs of peripancreatitis. Evidence of pancreatic phlegmon by surgical exploration included a pancreatic inflammatory mass, peripancreatic fluid, and fat necrosis. Minor radiologic changes such as “pancreatic enlargement or thickness,” “mild peripancreatitis,” or “tiny ascitis” without consistent symptomatology and laboratory values or a positive abdominal exploration did not sustain the diagnosis of pancreatic phlegmon.
Complications were categorized as immediate (occurring after treatment and during hospitalization) or delayed (occurring within 30 days after patient's discharge). Complications were considered as major if ICU admission and/or urgent invasive procedures were required or if radiologic evidence of pancreatic necrosis and/or systemic complications were detected; minor complications were those that did not qualify as major.
To assess the severity of immediate complications, the following variables were examined and compared with that of the patients with uncomplicated crisis of pancreatitis: radiologic evidence of pancreatitis, time to WBC normalization, time to resume oral feeding, time to undergo elective cholecystectomy, and length of hospitalization.
Patient outcome was determined by the house-staff members and attending physicians in charge of the patients. They were assisted by skilled radiologists and endoscopists for imaging interpretation who provided written and signed reports. All of them were blinded to the randomization.
Statistical Analysis
The trial was designed to have 80% power when comparing an assumed mortality of 6% in the conservative treatment group18 and of 1% in those receiving ERCP ± ES within 48 hours from the onset of symptoms, as previously reported.19 Initial estimation was 204 patients per arm.23,24
The Institutional Review Board (IRB) of the USC Keck School of Medicine approved the study protocol. As required by the IRB, an annual interim analysis was performed using the O'Brien-Fleming criteria.25 Data were analyzed on an intent-to-treat basis and also according to duration of obstruction within or beyond 48 hours (a cutoff time identified previously9). The Fisher exact test was used to compare categorical variables;26 the 2-sample t test was used for continuous variables; 95% confidence intervals were calculated by the Blyth and Still methods.27 The Kaplan-Meier curves28 and the log-rank test29 were used to compare the variables used to assess the severity of immediate complications. Statistical significance was considered at a P level of 0.05.
With 61 of 408 (15%) patients enrolled, no patient had died in either group. However, there was a significantly lower complication rate in the study group (P = 0.026), moreover, in the patients with obstruction no longer than 48 hours regardless of their treatment group (P < 0.001) This precluded the continuation of the trial as the efficacy of shortening the period of obstruction by early ERCP ± ES was thought to be of enough magnitude as to render continuing the trial unjustifiable.
RESULTS
From May 21, 2001 to May 20, 2002, 192 patients with GSP were admitted to our service. A total of 131 of them were excluded from the study because they did not meet the enrollment criteria. The remaining 61 patients (mean age, 40 years; female, 75%; Hispanic, 82%) qualified for the study and were enrolled. Six (10%) patients (3 in each treatment group) presented severe pancreatitis at admission by the Ranson (n =3), Acosta (n = 2), or both criteria (n = 1).
Forty-nine of the 61 patients underwent cholecystectomy, including 43 procedures performed laparoscopically, 2 planned open, and 4 requiring conversion from laparoscopic to an open technique. Cholecystectomy was performed during the initial hospitalization and once the pancreatitis has subsided in 44 patients. In another patient, cholecystectomy was carried out (open) for associated acute cholecystitis. Four patients underwent interval elective cholecystectomy (range, 26–60 days after initial discharge). IOC was performed in 14 patients.
Cholelithiasis was diagnosed by radiologic procedures and confirmed at cholecystectomy (n = 49), ERCP ± ES (n = 5), or surgical exploration (n = 1). In the remaining 6 patients, the radiologic diagnosis of cholelithiasis was not operatively confirmed in our institution.
Common bile duct (CBD) stones were detected in 18 (30%) of the 61 patients all confirmed by urgent or elective ERCP (n = 15), IOC (n = 2), or surgical exploration (n = 1). CBD stones impacted at the ampulla were detected in 11 (37%) patients, all in the study group (isolated, n = 4; and associated to mobile stones, n = 7). Mobile CBD stones without impaction were found in the remaining 7 patients. CBD stones were not detected in the remaining 43 patients, as confirmed by ERCP (n = 8), IOC (n = 12), surgical exploration (n =1), or clinical course (n = 22).
Monitoring ampullary patency predicted ampullary obstruction in 17 patients being accurate in 15, all of whom (100%) had ampullary obstruction confirmed by ERCP; the remaining 2 patients were not obstructed at the time of ERCP (false positives). The test used to predict ampullary patency was accurate in all 44 patients as confirmed by ERCP (n = 6), IOC (n = 12), or clinical course (n = 26).
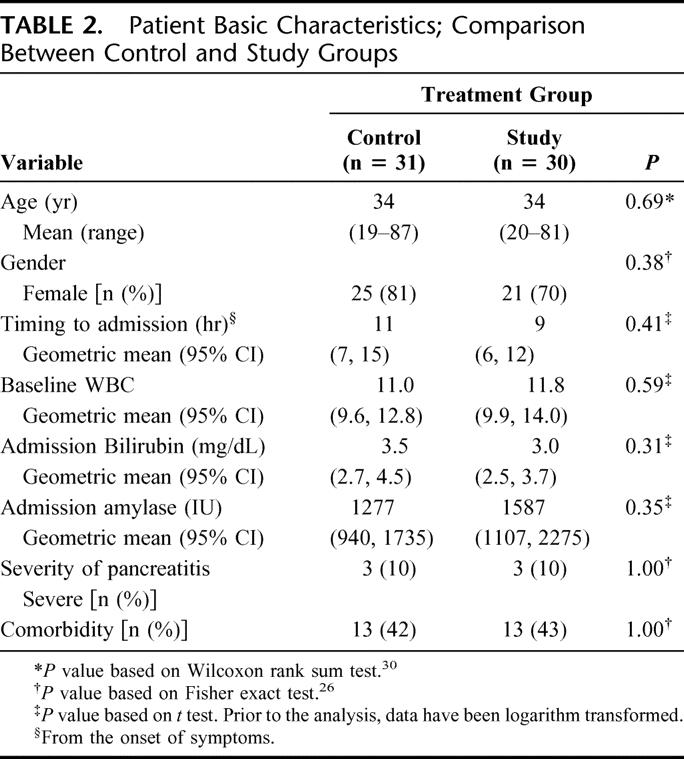
The 2 treatment groups were similar with regard to their basic characteristics (Table 2).
TABLE 2. Patient Basic Characteristics; Comparison Between Control and Study Groups
Outcome in 31 Patients Assigned to Conservative Treatment
There were 22 patients who disobstructed spontaneously within 48 hours from the onset of symptoms and 9 patients in whom obstruction persisted longer. Three of these 9 patients underwent ERCP at 53, 59, and 62 hours from the onset of symptoms; none of them had gallstones impacted, but 2 had ampullary obstruction (edema and sludge, respectively) based on the absence of bile in the duodenum, difficult duct cannulation, and a gush of dark bile coming from the common duct after ES. The third patient who also had papillary edema without signs of obstruction did not undergo ES. Twenty-one of the 22 patients who disobstructed spontaneously within 48 hours experienced a rapid resolution of their pancreatitis; the remaining patient developed a pancreatic phlegmon, which subsided uneventfully with conservative measures only. Two of the 9 patients with obstruction over 48 hours also experienced a rapid resolution of their pancreatitis; the remaining 7 patients developed immediate complications (Table 3); 6 of them had minor complications and recovered with conservative treatment. The remaining patient who had had ES and sludge extraction 53 hours after onset of symptoms developed a pancreatic phlegmon, acute cholecystitis, and bile peritonitis, which required urgent exploration (cholecystectomy and drainage) and ICU admission for 4 days. This patient also recovered uneventfully. No patient died. The duration of obstruction and outcome in this group are reported in Table 3. Twenty-two patients underwent elective cholecystectomy averaging 8 days from admission. Six patients required elective ERCP + ES for choledocholithiasis averaging 7 days from admission (prior to cholecystectomy, 3; after cholecystectomy, 1; and as a unique procedure, 2). Hospitalization averaged 10 days.
TABLE 3. Duration of Obstruction and Outcome According to Treatment Groups
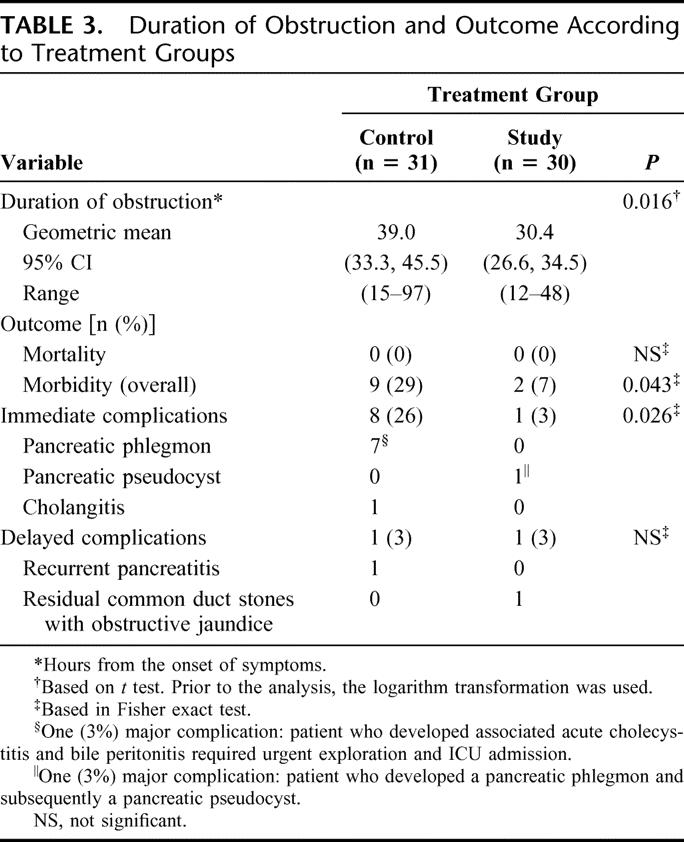
Outcome in 30 Patients Assigned to ERCP ± ES ≤48 Hours
Sixteen patients disobstructed spontaneously within 48 hours from the onset of symptoms, and 14 remained obstructed for 24 hours or longer. All these 14 patients underwent ERCP averaging 34 hours (range, 24–48 hours) from the onset of symptoms. Ampullary obstruction was confirmed in 13 patients: a stone impacted at the ampulla, 11 patients; and papillary edema, 2 patients. All 13 patients underwent ES. The remaining patient who was clinically obstructed had choledocholithiasis without stone impaction or other sign of obstruction; CBD stones were removed through the ampulla avoiding sphincterotomy. Twenty-nine patients (16 treated conservatively and 13 who underwent ERCP ± ES) experienced a complete and rapid resolution of their pancreatitis. The remaining patient (ERCP + ES and impacted stone extraction) developed a pancreatic phlegmon and, subsequently, a 6-cm pancreatic pseudocyst, which regressed after 50 days of outpatient therapy. No patient died. The duration of obstruction and outcome in this group are reported in Table 3. Twenty-two patients had cholecystectomy averaging 6 days after admission. Three of the16 patients treated conservatively underwent elective ERCP ± ES to rule out choledocholithiasis (as a first procedure, 2; and after cholecystectomy, 1). Hospitalization averaged 9 days.
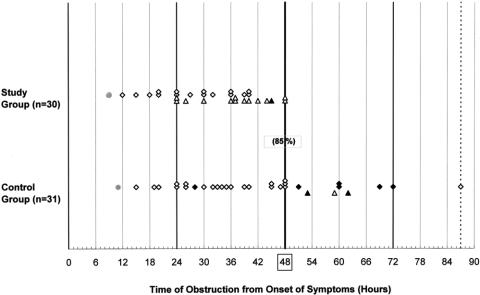
Analysis and Comparison of Outcome Measures
There were no deaths in either group and no complications from ERCP or ES. The overall rate of complications was 18%, and the rate of immediate complications was 15%. The 2 treatment groups differed regarding the duration of obstruction, which was significantly shorter in the study group (Table 3). In the study group, the overall rate of complications and the rate of immediate complications were significantly lower than in the control group. However, the 2 groups did not significantly differ regarding the timing of elective cholecystectomy and the length of hospitalization. When patient outcome was assessed in relation to the duration of ampullary obstruction (≤ and >48 hours) irrespective of their treatment group assignment, these 2 groups were equally matched with regard to their basic characteristics; they differed only for the bilirubin level at admission, which was higher in the >48 hours group: mean, 6.0 mg/dL (95% confidence interval [CI], 4.1, 8.8) versus 2.9 mg/dL (95% CI, 2.5, 3.4). The incidence of immediate complications in relation to the time of obstruction in both treatment groups is represented in Figure 2. Eighty-five percent (52 of 61) of the patients in both groups disobstructed within 48 hours, spontaneously (n = 38) or operatively (n = 14). The rate of immediate complications in this group was 4% (2 of 52). The remaining 9 (15%) patients (all in the control group) disobstructed beyond 48 hours, spontaneously (n = 6) or by ERCP ± ES (n = 3). The rate of immediate complications in the latter group was 78% (7 of 9) significantly higher than that in the ≤48 hours group (Table 4). In the first group (≤48 hours obstruction), the rate of complications did not differ between the 2 treatment groups: control, 4.5% (1 of 22) versus study, 3% (1 of 30), and also between the patients with spontaneous, 2.6% (1 of 38) and operative 7% (1 of 14) disobstruction.
FIGURE 2. Incidence of immediate complications in relation to the time of obstruction in both treatment groups. The rate of patients disobstructed within 48 hours is between brackets. The time of admission (mean) is represented by a filled circle, the patients with spontaneous disobstruction by diamond shapes, and those who underwent ERCP ± ES by triangle shapes. The empty shapes (diamonds and triangles) represent the patients without immediate complications and the filled shapes, those with complications.
TABLE 4. Patients' Outcome According to Duration of Obstruction
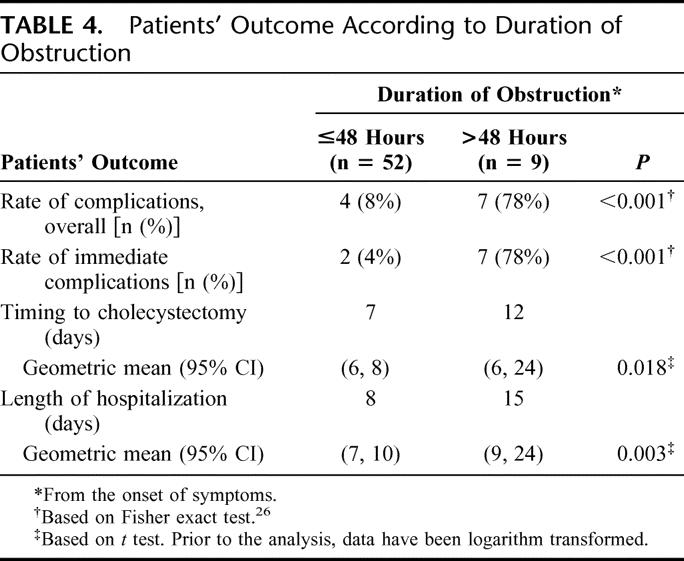
The group with ≤48 hours obstruction showed as well a statistically significant shorter time for elective cholecystectomy and a shorter hospital stay than that with longer obstruction (Table 4).
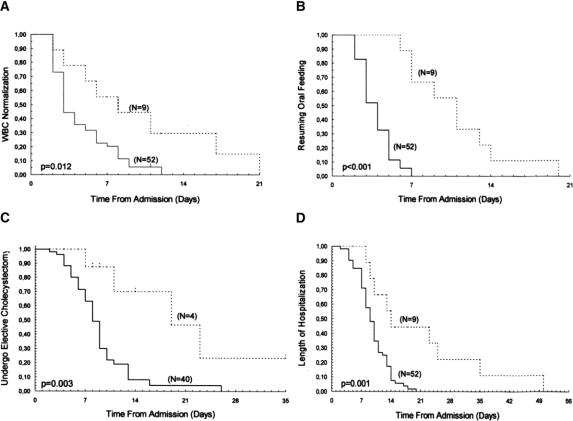
The duration of obstruction was significantly longer in the patients with complications than in those without (mean, 53.5 versus 33.0 hours; P < 0.001, t test). The patients with complications showed significantly longer periods for WBC normalization, resuming oral feeding, undergo elective cholecystectomy and hospitalization (Table 5; Fig. 3). The difference in the number of patients with radiologic signs of acute pancreatitis between the 2 groups (78%, 7 of 9 versus 14%, 7 of 49, respectively; P = 0.09631) did not reach statistical significance but still showed a definite trend toward the patients without complications (radiologic studies were not available in 3 patients). In addition, while all the 7 patients with pancreatic phlegmon showed radiologic changes consistent with this condition, the 7 patients without clinical and laboratory signs of complications presented only minor radiologic changes consistent with mild or moderate pancreatitis.
TABLE 5. Time to WBC Normalization, to Resuming Oral Feeding, to Undergo Elective Cholecystectomy, and Total Hospital Stay in 61 Patients With or Without Complications
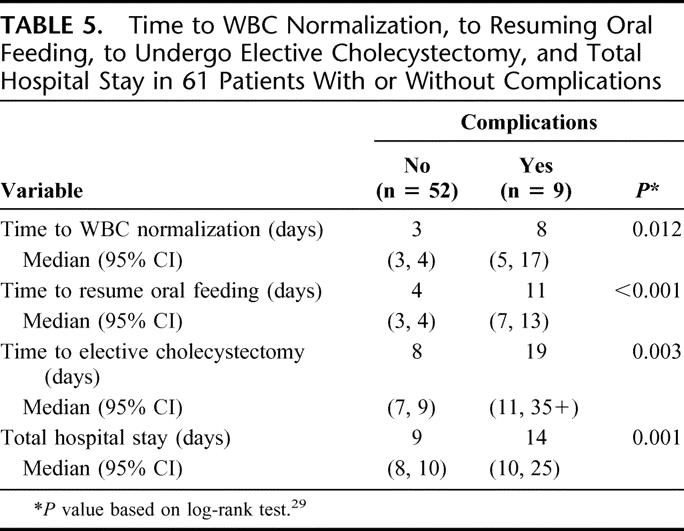
FIGURE 3. Kaplan-Meier curves28 for probability of (A) WBC normalization, (B) resuming oral feeding, (C) undergo elective cholecystectomy and (D) length of hospitalization, according to the time elapsed from admission. Patients with immediate complications (dotted line) and those without (solid line). P values were calculated using log-rank test.
DISCUSSION
The importance of early ERCP + ES to restore ampullary patency in patients with GSP has been addressed in several randomized prospective studies.14–17 However, the benefit of this approach remains controversial except for patients with associated cholangitis.17 A most confusing factor is that, in approximately 80% of these patients, the offending stone passes spontaneously within 48 hours, making emergency ERCP irrelevant. Nevertheless, a small but not negligible number of patients experience either a longer19 or permanent (∼5%)32 stone impaction, which may lead to severe pancreatitis or death.9,10
Unfortunately, there are no early reliable predictors to identify the patients at risk. Indeed, by including all patients with GSP, the majority of whom would be expected to disobstruct spontaneously, previous studies may have skewed the possibility of detecting the benefits of early ES.
Our single-center study differs substantially from prior prospective randomized trials14–17 in that our study only included patients with GSP + AO within 48 hours of evolution. According to our previous investigations, it is the only group in which progression of pancreatitis can be prevented. While this restricted our ability to recruit patients, it provided us with a very homogeneous group of patients. It allowed us a better assessment of the relationship between duration obstruction and severity of pancreatitis and of the effect of early disobstruction in this setting. Furthermore, by allowing 24 hours for the stones to pass spontaneously, we applied the more aggressive treatment only to those at greater risk of developing complications.
The diagnosis of persistent ampullary obstruction was confirmed by ERCP and relieved by ES in 15 of 17 patients. The assumption of spontaneous disobstruction was confirmed by the clinical course and laboratory response in all the remaining 44 patients. False negatives could not be assessed in these patients, many of whom obviously did not undergo unnecessary invasive procedures. The utility of MRC to identify common bile duct CBD stones has been advocated by several authors.33,34 In our opinion, this procedure should be routinely performed at admission if available.
The inclusion of “pancreatic phlegmon” in the list of possible pancreatic complications in our study may be questioned because it has been rejected by the Atlanta Symposium.22 However, several authors including ourselves consider that pancreatic phlegmon is a well-defined clinical entity, distinct from uncomplicated acute pancreatitis with an incidence between 8%35 and 18%.36 In addition, it has been shown that these patients have a higher incidence of severe pancreatitis associated with longer periods of fever, abdominal pain, hyperamylasemia, leukocytosis, and hospital stay than did controls patients with uncomplicated pancreatitis.37,38 Although most phlegmons resolve spontaneously, a significant number may progress to more severe complications35–43 with a reported mortality rate as high as 21%.37 The 2 major complications observed in our series (one in each treatment group) were preceded by pancreatic phlegmons. Finally, it is worth considering that during the early stages of GSP, where major complications are rare and death is almost nonexistent, pancreatic phlegmon may be the only available index to assess patients' prognosis and outcome.
Our study showed that the 2 treatment groups differed significantly regarding the rate of complications confirming our hypothesis. However, the 2 groups did not differ regarding the rates of major and delayed complications, and the time to cholecystectomy and length of hospitalization.
The analysis of patients' outcome based upon the duration of obstruction irrespective of the treatment groups showed that the rate of immediate complications was significantly lower among patients whose obstruction lasted less than 48 hours, confirming the results of previous investigations.5,6,11,19 In addition, both the timing of elective cholecystectomy and the length of hospitalization were shorter than those of the patients with longer obstruction. The lack of statistical significance between these 2 variables in the treatment groups, therefore, may be related to the high incidence of spontaneous disobstruction within 48 hours in the control group (71%) that substantially reduced the duration of obstruction in this arm. However, the overall duration of obstruction was even shorter in the study group because of the systematic use of ERCP within 48 hours. It resulted in a significant reduction in the incidence of immediate complications, which still achieved statistical significance.
Our study shows that the duration of ductal obstruction is a critical factor in determining the severity of GSP and that the beneficial effect of early disobstruction within 48 hours occurred irrespective of whether it happened spontaneously or operatively. The occurrence of complications in 2 of our patients with less than 48 hours of obstruction suggests that the safe obstruction period to prevent progression of pancreatitis might be even shorter than the 48 hours assumed, or other factors besides duration of obstruction may play a role in determining the severity of pancreatitis. One among the latter is the absence of a distensible gallbladder (as a result of previous removal or sclerosis) capable of decreasing the abnormally high intraductal pressure resulting from stone impaction.44 The only patient who developed an immediate complication in study group had undergone cholecystectomy 5 years earlier.
CONCLUSION
This study shows that there is a short period of time not longer than 48 hours from the onset of symptoms (perhaps shorter) when either spontaneous or operative disobstruction may prevent the progression of pancreatitis. Furthermore, it shows that, in patients whose obstruction remains at 24 hours, ERCP and ES benefit the outcome of GSP and these patients can accurately be identified on the basis of simple clinical, biochemical, and radiologic criteria. Recognition and understanding of the role of duration of obstruction during the first 48 hours of GSP and the appropriate identification of patients with either persistent or transient obstruction during that period are useful tools to improve outcome in the management of these patients.
ACKNOWLEDGMENTS
The authors thank Frida Bergmann, PhD, Instituto de Investigaciones Médicas de Rosario, Rosario, Santa Fé, Argentina, for her critical and detailed review.
Footnotes
Reprints: Thomas V. Berne, MD, Department of Surgery, LAC + USC Medical Center, 1200 North State Street, Room 9900, Los Angeles, CA 90033. E-mail: berne@usc.edu.
REFERENCES
- 1.Opie EL. The etiology of acute hemorrhagic pancreatitis. Bull Johns Hopkins Hosp. 1901;12:182–188. [Google Scholar]
- 2.Acosta JM, Ledesma CL. Gallstone migration as a cause of acute pancreatitis. N Engl J Med. 1974;290:484–487. [DOI] [PubMed] [Google Scholar]
- 3.Senninger N, Moody FG, Coelho JCV, et al. The role of biliary obstruction in the pathogenesis of acute pancreatitis in the opossum. Surgery. 1986;99:688–693. [PubMed] [Google Scholar]
- 4.Rünzi M, Saluja S, Lerch MM, et al. Early ductal decompression prevents the progression of biliary pancreatitis: an experimental study in the opossum. Gastroenterology. 1993;105:157–164. [DOI] [PubMed] [Google Scholar]
- 5.Acosta JM, Rossi R, Rubio Galli OM, et al. Early surgery for acute gallstone pancreatitis: evaluation of a systematic approach. Surgery. 1978;83:367–370. [PubMed] [Google Scholar]
- 6.Acosta JM, Pellegrini CA, Skinner DB. Etiology and pathogenesis of acute biliary pancreatitis. Surgery. 1980;88:118–125. [PubMed] [Google Scholar]
- 7.Stone JP, Fabian TC, Dunlop WE. Gallstone pancreatitis: biliary tract pathology in relation to time of operation. Ann Surg. 1981;194:305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mercer LC, Salzstein EC, Peacock JB, et al. Early surgery for biliary pancreatitis. Am J Surg. 1984;148:749–753. [DOI] [PubMed] [Google Scholar]
- 9.Wilson C, Imrie CW, Carter DC. Fatal acute pancreatitis. Gut. 1988;29:782–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corfield AP, Cooper MJ, Williamson RCN. Acute pancreatitis: a lethal disease of increasing incidence. Gut. 1985;26:724–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Acosta JM, Rubio Galli OM, Rossi R, et al. Effect of duration of ampullary gallstone obstruction on severity of lesions of acute pancreatitis. J Am Coll Surg. 1997;184:499–505. [PubMed] [Google Scholar]
- 12.Kelly TR, Wagner DS. Gallstone pancreatitis: a prospective randomized trial of the timing of surgery. Surgery. 1988;104:600–604. [PubMed] [Google Scholar]
- 13.Oria A, Alvarez J, Chiappetta L, et al. Choledocholithiasis in acute gallstone pancreatitis: incidence and clinical significance. Arch Surg. 1991;126:566–568. [DOI] [PubMed] [Google Scholar]
- 14.Neoptolemos JP, Carr-Locke DL, London NJ, et al. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988;2:979–983. [DOI] [PubMed] [Google Scholar]
- 15.Fan S-T, Lai ECS, Mok FPT, et al. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med. 1993;328:228–232. [DOI] [PubMed] [Google Scholar]
- 16.Nowak A, Nowakowska-Dulawa E, Marek TA, et al. Final results of the prospective, randomized controlled study on endoscopic sphincterotomy versus conventional management in acute biliary pancreatitis. Gastroenterology. 1995;108(suppl A):380. [Google Scholar]
- 17.Fölsch UR, Nitsche R, Luedke R, et al. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. N Engl J Med. 1997;336:237–342. [DOI] [PubMed] [Google Scholar]
- 18.SSAT, AGE, ASGE Consensus Panel. General Summary. Management of the biliary tract in acute necrotizing pancreatitis: SSAT, AGE, ASGE Consensus Panel. Society for Surgery of the Alimentary Tract, American Gastroenterological Association, American Society for Gastrointestinal Endoscopy. J Gastrointest Surg. 2000;5:221. [PubMed] [Google Scholar]
- 19.Acosta JM, Ronzano GD, Pellegrini CA. Ampullary obstruction monitoring in acute gallstone pancreatitis: a safe, accurate, and reliable method to detect pancreatic ductal obstruction. Am J Gastroenterol. 2000;95:122–127. [DOI] [PubMed] [Google Scholar]
- 20.Ranson JHC. Etiological and prognostic factors in human acute pancreatitis: a review. Am J Gastroenterol. 1982;77:633–638. [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 22.Bradley LE III. A clinically based classification system for acute pancreatitis: summary of the International Symposium on Acute Pancreatitis, Atlanta, GA, September 11–13, 1992. Arch Surg. 1993;128:586–590. [DOI] [PubMed] [Google Scholar]
- 23.Casagrande JT, Pike MC, Smith PG. An improved approximate formula for calculating sample size for comparing two binomial distributions. Biometrics. 1978;34:483–486. [PubMed] [Google Scholar]
- 24.Buckley J. Power User Manual. Pasadena, CA: Epicenter Software, 1986. [Google Scholar]
- 25.O'Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35:549–556. [PubMed] [Google Scholar]
- 26.Mehta CR, Patel NR. A network algorithm for performing Fisher's exact test in rXc contingency tables. JASA 1983 78:427–434. [Google Scholar]
- 27.Blyth CR, Still HA. Binomial confidence intervals. JASA. 1983;78:108–116. [Google Scholar]
- 28.Kaplan EL, Meier P. Nonparametric estimation form incomplete observations. JASA. 1958;53:457–481. [Google Scholar]
- 29.Miller RG Jr. Survival Analysis. New York: John Wiley & Sons, 1981:94–98. [Google Scholar]
- 30.Rosner B. Fundamental of Biostatistics. Boston: PWS-KENT, 1990:304–309. [Google Scholar]
- 31.Zar JH. McNemar Test: Biostatistical Analysis. Englewood Cliffs, NJ: 1974:127. [Google Scholar]
- 32.White TT. Pancreatitis. London: Edward Arnold, 1966:6. [Google Scholar]
- 33.Hochwald SN, Dobryansky M, Rofsky NM, et al. Magnetic resonance cholangio-pancreatography accurately predicts the presence or absence of choledocholithiasis: J Gastrointest Surg. 1998;2:573–579. [DOI] [PubMed] [Google Scholar]
- 34.Makary MA, Duncan MD, Harmon JW, et al. The role of magnetic resonance cholangio-graphy in the management of patients with gallstone pancreatitis. Ann Surg. 2005;241:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fan ST, Choi TK, Chan FL, et al. Pancreatic phlegmon: what is it? Am J Surg. 1989;157:544–547. [DOI] [PubMed] [Google Scholar]
- 36.Warshaw AL. Inflammatory masses following acute pancreatitis: phlegmon, pseudocyst, and abscess. Surg Clin North Am. 1974;54:621–636. [DOI] [PubMed] [Google Scholar]
- 37.Maroun MC, Uscanga L, Lara F, et al. Flemón pancreático: una forma potencialmente fatal de pancreatitis aguda. Rev Inv Clín. 1992;44:507–512. [PubMed] [Google Scholar]
- 38.Sostre CF, Flournoy JG, Bova JG, et al. Pancreatic phlegmon: clinical features and course. Dig Dis Sci. 1985;30:918–927. [DOI] [PubMed] [Google Scholar]
- 39.Hunter TB, Haber K, Pond GD. Phlegmon of the pancreas. Am J Gastroenterol. 1982;77:949–952. [PubMed] [Google Scholar]
- 40.Warshaw AL. Can pancreatic phlegmon be diagnosed? Hepatobiliary Pancreat Surg. 1990;2:300–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lawson DD, Daggett WM, Civetta JM. Surgical treatment of acute necrotizing pancreatitis. Ann Surg. 1970;172:605–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beger HG, Bittner PA, Block S, et al. Bacterial contamination of pancreatic necrosis: a prospective clinical study. Gastroenterology. 1986;91:433. [DOI] [PubMed] [Google Scholar]
- 43.Gerzof SG, Banks PA, Robbins AH, et al. Early diagnosis of pancreatic infection by computed tomography-guided aspiration. Gastroenterology. 1987;93:1315. [DOI] [PubMed] [Google Scholar]
- 44.Acosta JM. The role of the sphincter of Oddi in acute pancreatitis. Gastroenterol Clin Biol. 1988;12:533–536. [PubMed] [Google Scholar]