Abstract
Objective:
Because of rising costs and shrinking reimbursements, hospitals must continually find ways to improve efficiency and productivity. This study attempts to increase caseloads in ambulatory surgery operating rooms while maintaining patient satisfaction and safety.
Summary Background Data:
In most hospitals, patients move through their operative day in a linear fashion, starting at registration and finishing in the recovery room. Given this pattern, only 1 patient may occupy the efforts of the operating room team at a time. By processing patients in a parallel fashion, operating room efficiency and patient throughput are increased while costs remain stable.
Methods:
Patients undergoing hernia repairs under local anesthesia with intravenous sedation were divided into a control group and an experimental group. Patients in the control group received their local anesthesia in the operating room at the start of the surgery. The experimental group patients received their local anesthesia in the induction room by the surgeon while the operating room was being cleaned and set up.
Results:
While operative time for the control group and the experimental group were nearly identical, the turnover time and the induction time were significantly shorter for the experimental group. The cumulative reduction in time during the operative day was sufficient to allow the addition of new operative cases.
Conclusions:
This study demonstrates a system of increasing operating room efficiency by changing patient flow rather than simply working to streamline existing steps. This increase in efficiency is not associated with the expansion of hospital budgets or a decrease in patient safety or satisfaction.
Hospitals are constantly struggling to improve operating room efficiency. By redesigning the process of patient flow through an operating room using parallel processing, we generated meaningful improvements in operating room efficiency.
To maintain prosperity and success in the current medical climate, hospitals must continually balance the forces of shrinking insurance reimbursements, advancements in medical technology, and the logistics of running an operationally complex and successful facility. In addition, the end result, namely, safe and high-quality health care for patients, cannot be compromised. When examined closely, the operating rooms serve as a scaled-down model for the challenges that face the entire hospital.
There are a number of studies in the literature aimed at increasing operating room efficiency and controlling operating room costs while striving to provide high-quality, technologically advanced surgical services. Often the focus is on streamlining the existing steps that are involved with patient care preoperatively, intraoperatively, and postoperatively. These studies, for example, have investigated: 1) how to better increase operating room ergonomics and organization, 2) how to identify and eliminate delays in the operating rooms as a whole, and 3) whether shortening a given variable in the operating room could actually make a meaningful impact on increasing case volume.3 The common aspect to these, and most other studies on enhancing operating room efficiency, is that the linear structure of patients moving one by one through the operative day remains unchanged. The creators of these studies adhere to this common linear principle because they believe that moving patients through the operating day in parallel rather than linearly would require a second team, which creates higher costs, without clear benefits.
In this study, we aimed to change this paradigm in a manner that has not been published in the literature to date. In our ambulatory surgery suites, most hernia repairs, including inguinal, umbilical, and ventral, are performed using local anesthesia and intravenous sedation. The historical routine is that the patient is brought into the operating room, intravenous sedation is administered, the surgeon shaves the patient, and the local anesthesia is injected. For this study, we examined the effects of the operating surgeon shaving and administering local anesthesia to the patient in the induction room while the prior patient was transported to the recovery room and the operating room was being turned over. Our belief was that parallel processing of patients would shorten the total time spent on each patient without impacting operative time. In addition, we thought that the patients would not be negatively impacted by this change in protocol and that they would remain highly satisfied with their care.
METHODS
This study was created based upon 4 central factors: a similar type of procedure for all involved patients, a single surgeon being involved in the study, accurate timing of specific intervals throughout the operative day, and a well-defined routine for all members of the operative team.
Procedure Type
We included only patients undergoing hernia surgery with a combination of local anesthesia and intravenous sedation as the anesthetic plan. The types of hernias included in this study were: inguinal hernias, both unilateral and bilateral, umbilical hernias, and small ventral hernias. The exclusion criteria for this study included patients who required general anesthesia secondary to the extensive or complex nature of their hernia, as judged by the operating surgeon, or patients who required a more aggressive anesthetic plan as determined by a preoperative anesthesia consultation. By including only hernia surgery, we were able to assess any variations in actual operative time between the study group and the control groups.
Single Surgeon
We had a single surgeon involved in the study. The study surgeon performed hernia repairs on Wednesdays and on Thursday afternoons. Prior to the study, he typically sequentially performed 5 or 6 inguinal hernia repairs on Wednesdays, and between 2 and 4 hernia repairs on Thursdays. By involving only one surgeon, any significant interpersonal variability secondary to operative style and plan, local anesthesia administration, and time lapsed during preparation and draping of the patient was erased. In addition, the single surgeon was able to synthesize the new style of processing patients and incorporate that style efficiently into his operative day.
Accurate Timing of Intervals
We then defined and measured comparable time intervals for data accuracy. While creating the study, 3 specific time periods were identified. The first period involved 3 activities: initiating intravenous sedation as the patient's anesthetic, injecting local anesthetic as a preoperative block, and preparing the patient for surgery by shaving the operative site, applying topical cleansers, and sterile draping. This period was designated as the “sedation, block, and prep” time and begins as the patient enters the room. The next time interval is the actual operative time. This period includes the time period between finishing patient preparation and finishing the operation. The third time period includes the turnover time for the room. During this time, the room is cleaned, and the instruments and anesthesia machine are cleaned and arranged for the next patient.
Well-Defined Team Roles
We then created defined roles for each operative team member. This part of the project was crucial to redesigning the flow of patients through the operating room. The standard personnel for an inguinal hernia repair under intravenous sedation include a surgeon with an assisting surgical resident, a surgical scrub technician, a nurse circulator, and a nurse providing intravenous sedation. Prior to this study, both nurses remained in the operating room during the turnover period or attended to their other duties while the surgeon and surgical resident attended to nonoperative work. In addition, prior to the study, nurses and surgical scrub technicians were freely substituted during the operative day. Essentially, there was not any strict team cohesiveness or team order. In this study, switches were only performed at the conclusion of a case.
During the study, the team became a well-defined unit. At the beginning of the operative day, the team was constructed and remained together for the entire day. The roles for the team were broken down for each of the 3 measured time periods. During the turnover time period, one nurse and the surgical scrub remained in the operating room to prepare for the upcoming case. The second nurse and the surgeon went to the preoperative holding area to start the sedation and block. In the preoperative holding area, a specific slot was designated for hernia patients that contained the supplies necessary to begin the sedation, block, and prep time. These supplies included a cardiac monitor, intravenous medications, local anesthetics, and razors. When the operating room was ready, the surgeon and nurse transported the sedated and blocked patient into the operating room where the prep took place. The next step was the operation, at which all members of the team were present. At the end of the operation, one nurse and the surgical resident transported the patient to the recovery room, while the surgeon went to the preop area to begin with the next patient. This methodology essentially outlines a strategy where a significant portion of the sedation, block, and prep time overlaps with the turnover time.
Study Logistics
The study surgeon performed herniorrhaphies all day Wednesday and Thursday afternoons. Careful time measurements were made of all time intervals during the Wednesday and Thursday cases for approximately 2 months prior to beginning the actual study. This group served as the historical control. At the time of study initiation, Wednesday was designated as a study day, while Thursday was designated as a control day. During the study days, the above-mentioned 4 key factors were strictly followed. On the control days, the normal prestudy flow of patients and team members occurred. The patients were blindly assigned to Wednesday or Thursday based exclusively on the preoperative scheduling availability and the patient's own availability/schedule. On Wednesday, the first case of the day was treated and recorded as a control case because there was no preceding case.
Patient Satisfaction Survey
Patients that were treated during the study days were provided with a survey to analyze their degree of satisfaction with their operative day. The survey was created by the study designers and addressed a number of the key factors to the operative day, including surgeon expectations, pain control, operative team interaction, and overall feelings regarding their operative experience at the hospital. The patients were assured that their answers would remain anonymous.
Study Statistics
Data were summarized using mean ± SD. Analysis of variance techniques were used to compare the 3 study groups. Since the turnover time was not normally distributed, the analysis of this interval was done on the log-transformed scale. Statistical significance was set with a 2-sided P value ≤ 0.05.
RESULTS
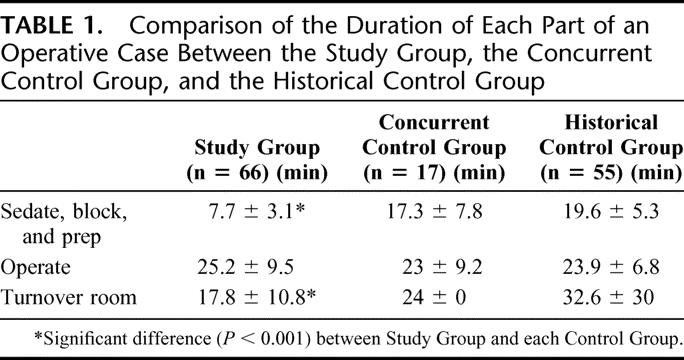
The first step in evaluating the results is to compare the 3 measured time intervals between the historical controls, the study population, and the concurrent study control group. The 3 time intervals were as follows: 1) sedate, block, and prep time, 2) operative time, and 3) turnover time. For the prestudy control group, 55 cases were measured. The means of the 3 time intervals were 19.6 ± 5.3 minutes, 23.9 ± 6.8 minutes, and 32.6 ± 30 minutes, respectively. For the concurrent control group, 17 cases were measured. The 3 time intervals were 17.3 ± 7.8 minutes, 23 ± 9.2 minutes, and 24 ± 0 minutes, respectively. For the study group, 66 cases were measured. The time intervals were 7.7 ± 3.1 minutes, 25.2 ± 9.5 minutes, and 17.8 ± 10.8 minutes, respectively (Table 1). There were no statistically significant differences between the time intervals measured for the historical control group and the concurrent control group. The study group, however, had statistically significant differences when compared with each group for the sedate, block, and prep interval as well as the turnover time interval (P < 0.001). Importantly, there were no statistically significant differences between the operative times for all 3 groups after this interval was statistically adjusted to account for different operations. This consistent operative time between all 3 groups indicates that there was no difference in operative strategy as well as no imposed pressures to increase operative speed for study purposes.
TABLE 1. Comparison of the Duration of Each Part of an Operative Case Between the Study Group, the Concurrent Control Group, and the Historical Control Group
From a standpoint of the operating room system as a whole, this increased rate of patient flow did not cause any delays downstream. In the Post-Anesthesia Care Unit, there was no significant difference between the mean times spent by patients from all 3 groups after surgery. The mean time was 85.3 ± 55.3 minutes for the historical control group, 124.3 ± 140.8 minutes for the concurrent control group, and 82.4 ± 38.5 minutes for the study group.
In regards to the operating room time blocked out for the study surgeon's cases, there was at least a 33% reduction in time used each day for the study days versus the control days. This reduction in block time usage was approximately consistent across the entire study period of 12 weeks. This decrease in usage allowed the surgeon to stop using his Thursday afternoon block time altogether and shift his total caseload to Wednesday (without reducing the total number of cases performed). The surgeon's caseload was very consistent during the study averaging 8 to 10 hernias per week. The surgeon's caseload over the 2003 and 2004 years was also consistent (338 versus 329 hernia cases). This freed up additional operating room capacity for other surgeons’ cases and led to fewer cases in the concurrent control arm. The surgeon now uses Thursday afternoon for administrative endeavors or to perform general anesthesia cases.
Finally, it is important to gauge the satisfaction with the new system from the standpoint of the patients. The purpose of the patient satisfaction survey was not to compare between the study group and the control group to assess for differences. Rather, it was to identify an empirical level of satisfaction with a number of aspects that make up the patient's overall experience. As seen in Figure 1, the patients had an overall positive attitude toward their hospital experience, with at least 90% of patients agreeing in the affirmative with questions regarding their surgeon, their nurses, and the overall hospital experience. Also, it is important to note that the response rate for this survey was approximately 60%, rather than the average response rate in the hospital for other surveys of 38%. The results reinforce that the changes made to the operative day were not perceived in a negative way.
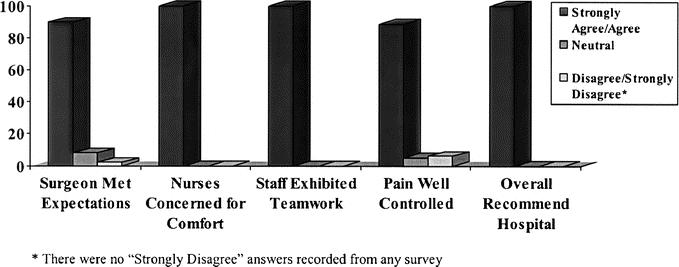
FIGURE 1. Patient satisfaction survey responses for specific key categories.
DISCUSSION
This study was conceived while assessing potential changes that would increase operating room efficiency. The necessity to increase operating room efficiency is born out of the current medical climate that creates financial and productivity pressures on hospitals, physicians, and staff. This problem is not new but rather has been addressed in a number of different ways over the past decade.
One previously described model is to adjust the ergonomics and simplify the nursing routines within the operating room. Methods outlined in this process involve removing excess equipment from the operating room that is not used regularly, rearranging equipment that is used regularly to make it readily accessible, and restructuring the operating room itself to make it more user friendly. By doing this, a moderate isolated decrease in turnover time was accomplished.1 This effort did not affect any other time period for each patient's operation.
A second model involves recording in great detail all the possible measurable time periods for each patient's operation.2 This would include breaking down our 3 time periods into many more blocks. After making the measurements, initiatives are created across the Surgery and Anesthesia departments, as well as with the operating room coordinators and staff, to decrease any and all intervals possible. The methods used to enforce the goals of this type of study include regular meetings among representatives from all groups, regularly distributed reports to all physicians involved, and consistent efforts to maintain any improvements in efficiency. This is a labor-intensive approach, and the time saved overall in a day for a given operating room was usually less than enough time to perform an extra case. To realize a benefit with this type of approach, there would need to be a very fluid operating room staff that could float between rooms or finish the working day on short notice and midshift.
Similarly, a third approach3 analyzes the potential benefits of shortening one measured time block, the time allotted for anesthesia work. By analyzing the amount of time that the anesthesia staff needed to safely perform their job, it was determined that they would have to reduce their actual working time by an impossible amount to create enough extra time to add even 1 short case per day. Thus, they determined that, by simply working to increase their efficiency in the current linear system of handling patients, they could not feasibly produce a significant time or money benefit.
The common thread that links these 3 and most other operating room efficiency studies is that they are working based on the standard linear structure of patient flow through the operating day. By adhering to this premise, they are inherently limited in their gains. In addition, these studies are applying their work toward a wide spectrum of operating rooms in which the actual operating time occupies a large percentage of the day.
In this study, we worked to provide a new approach to enhancing operating room efficiency. By parallel processing, the team, which includes the surgeon, nurses, and scrub technicians, effectively is able to work on 2 patients simultaneously. Although most surgeons and anesthesiologists are familiar with the fact that the anesthesia team begins their preparation of a patient while the room is being turned over from the last patient, this does not effectively reduce the amount of time necessary to actually provide anesthesia for the patient. By beginning the anesthesia process in the preoperative holding area, including intravenous sedation and local anesthesia administration, a significant decrease was realized in the amount of in-room time spent on this process. This was quantified in a significant decrease in the time period for sedate, block, and prep (Table 1). This was done without adding personnel or additional equipment to the process, thus reducing both fixed and variable costs per case. In some systems, patients have their general anesthesia induction performed, or a regional block set, in a separate holding area adjacent to the operating room. Although this would provide a similar decrease in the in-room sedate, block, and prep time period, this system usually requires a second team of a physician and nurse. The extra cost for this system will decrease the benefits of the increased operating room efficiency.
This study also highlights an important aspect of operating room efficiency: coherent team function. By maintaining a constant team throughout the entire day, members of the team can predict the requirements that their specific job entails. This was highlighted best in the significant reduction of time elapsed during room turnover (Table 1). The routine that is created among team members allowed for enhanced cooperation as well as an increased subjective feeling of team unity. This type of team unity spurs efficient work behavior and allows the day to flow smoothly. The turnover time in the room dropped 25% versus concurrent controls and approximately 50% versus historical controls. The size of this reduction was surprising but is clearly linked to a sense of team unity.
To show a “real world” benefit for this study, it is important to note that the operating room time used by this surgeon was shortened by one third after the completion of the study even though his caseload remained unchanged. The remaining unused block time was reappropriated to other surgeons, who were able to perform additional operative cases. Whereas other studies have shown a numerically significant improvement in efficiency, they have often failed to show that more procedures could be performed during a given day in a single operating room. In this study, more cases were performed using the same room in the same day, without incurring costs for additional staff or resources. This provides a clear benefit for the surgeons and the hospital in terms of increased productivity and increased revenue, respectively.
The factors that hindered other studies were that they maintained a linear process for patients and they tried to apply their results to operating rooms with longer cases and general anesthesia cases. The key for the success of this study was that the system was applied to an operating room with a specific type of case in a parallel manner. It is important to state, however, that although this study was performed with a single surgeon performing a specific set of similar operations, the results are applicable to many other settings. The fundamental requirements to generate a benefit from this system include a surgeon who is performing a succession of short cases under local anesthesia/intravenous sedation. Thus, a plastic surgeon, orthopedic surgeon, or general surgeon who schedules multiple sequential procedures can easily apply this system. In a broader sense, this system can also be applied to physicians, such as gastroenterologists and general surgeons, who perform multiple endoscopies under intravenous sedation.
Finally, it is essential that the patients were satisfied with this system. By distributing a survey to those patients who underwent this pilot program, we were able to identify any potential shortcomings of the system as perceived from the patient's perspective. In Figure 1, the results of the patient survey show that the patients are pleased with both the overall operative day as well as the individual parts. Although the survey was dispersed to only study patients, it was simply meant to identify any perceived weaknesses of the new system, rather than create a comparison between the pilot group and the control group. The strongly positive responses, as well as the robust response rate, provided the positive feedback necessary to continue with this new operative flow poststudy.
Although the data from this study are statistically strong, there are some specific potential drawbacks. The first is that the study population and the control groups are relatively small. Despite being able to attain statistically significant data, it will be important to follow the trends as this type of operating room system is carried forward. In addition, this study required that a relatively consistent team be assembled and maintained together. In smaller hospitals, it may not be possible to earmark personnel for a specific team. Furthermore, although the patient survey relayed very positive feedback on the patient's experiences and perceptions of their hospital day, there was no comparison to a control group's responses. This is only a relative shortcoming, however, given that, even if there was a small difference in positive feedback, the answered surveys displayed empirically excellent feedback. Finally, this study required a surgeon who was both busy enough to schedule similar cases in succession as well as willing to entertain a new system. If another surgeon was not willing to adhere to the necessary changes, did not have a sufficient caseload to schedule multiple similar cases on a given day, or did not have the operating room facilities to accommodate the caseload in this manner, this type of organization would not be successful. We are currently identifying other surgeons with a consistent case volume and attempting to expand the use of this system. We are also attempting to mathematically model the operating suite to identify optimal configurations for general, regional, and longer case combinations.
As surgeons, anesthesiologists, and hospital administrators continue to struggle with ways to increase operating room efficiency and profitability in the face of decreasing reimbursements and increasing costs of equipment and technology, this study provides a new way to approach the problem. Whereas previous efforts have worked within the standard framework of patient flow, this parallel processing system may provide a new method to attack this growing problem.
Footnotes
Reprints: David L. Berger, MD, Massachusetts General Hospital, Wang Ambulatory Care Center, Suite 465, 15 Parkman Street, Boston, MA 02114. E-mail: dberger@partners.org.
REFERENCES
- 1.Mangum SR, Cutler K. Increased Efficiency through OR redesign and process simplification. AORN. 2002;76:1041–1046. [DOI] [PubMed] [Google Scholar]
- 2.Overdyk FJ, Harvey SC, Fishman RL, et al. Successful strategies for improving operating room efficiency at academic institutions. Anesth Analg. 1998;86:896–906. [DOI] [PubMed] [Google Scholar]
- 3.Dexter F, Coffin S, Tinker JH. Decreases in anesthesia-controlled time cannot permit one additional surgical operation to be reliably scheduled during the workday. Anesth Analg. 1995;81:1263–1268. [DOI] [PubMed] [Google Scholar]


