Abstract
Background:
The techniques of right hepatic trisectionectomy are now standardized in patients with hepatocellular or metastatic carcinoma, but not in those with hilar cholangiocarcinoma.
Methods:
Under preoperative diagnosis of hilar cholangiocarcinoma, 8 patients underwent “anatomic” right hepatic trisectionectomy with en bloc resection of the caudate lobe and the extrahepatic bile duct, in which the bile ducts of the left lateral section were divided at the left side of the umbilical fissure following complete dissection of the umbilical plate.
Results:
Liver resection was successfully performed, and all patients were discharged from the hospital in good condition, giving a mortality of 0%. All patients were histologically diagnosed as having cholangiocarcinoma. The proximal resection margins were cancer-negative in 7 patients and cancer-positive in 1 patient. Four patients with multiple lymph node metastases died of cancer recurrence within 3 years after hepatectomy. One patient died of liver failure without recurrence 42 months after hepatectomy. The remaining 3 patients without lymph node metastasis are now alive after more than 5 years.
Conclusions:
Anatomic right hepatic trisectionectomy with caudate lobectomy can produce a longer proximal resection margin and can offer a better chance of long-term survival in some selected patients with advanced hilar cholangiocarcinoma.
We introduced a new procedure of right hepatic trisectionectomy with en bloc resection of the caudate lobe for advanced hilar cholangiocarcinoma, in which the bile ducts of the left lateral section were divided at the left side of the umbilical fissure following complete dissection of the umbilical plate. This right trisectionectomy can produce a longer proximal resection margin on the left hepatic duct and offer a better chance of long-term survival.
An increasing number of hilar cholangiocarcinomas are being treated with liver resection.1–7 Based on preoperative accurate staging of cancer8 and in-depth knowledge of the surgical anatomy of the liver,9 various types of hepatobiliary resection have been developed,2 and combined resection of the caudate lobe has become a common prerequisite for curative resection in most patients with this disease.2,4,6 Right hepatic trisectionectomy with caudate lobectomy, resection of Couinaud's hepatic segments 1, 4, 5, 6, 7, and 8,9,10 is one surgical option, usually indicated for advanced hilar cholangiocarcinoma, which involves mainly the right intrahepatic bile ducts in continuity with the left medial sectional bile duct. The relative volume to be resected in this hepatectomy averages 81% of the liver,11 which indicates that this liver resection is very extensive.
Right hepatic trisectionectomy10 was previously named as right hepatic trisegmentectomy in the United States, while the term extended right hepatectomy or right hepatic lobectomy9 was used in European countries. Since this extended resection was first reported by Lortat-Jacob et al in 1952,12,13 the techniques have been standardized. In 1975, Starzl et al described in detail some important technical features of right hepatic trisectionectomy.14 Thereafter, many surgeons have reported modifications,15–19 mainly in an effort to avoid injury to the left hepatic duct. All of these previous techniques were applicable to hepatocellular carcinoma, liver metastasis, and benign hepatic diseases. In case of hilar cholangiocarcinoma, some novel procedures are required to obtain negative resection margins on the intrahepatic bile ducts.
In this contribution, we introduced practical techniques of “anatomic” right hepatic trisectionectomy with caudate lobectomy for hilar cholangiocarcinoma, in which the bile ducts of the left lateral section were divided at the left side of the umbilical fissure following complete dissection of the umbilical plate.9
METHODS
Patients
Eight patients with advanced hilar cholangiocarcinoma underwent anatomic right hepatic trisectionectomy with en bloc resection of the caudate lobe and the extrahepatic bile duct according to the surgical procedure detailed below (Fig. 1). All patients were jaundiced on admission with a mean serum total bilirubin concentration of 5.7 mg/dL (range, 2.1–11.7 mg/dL) and underwent percutaneous transhepatic biliary drainage before surgery.20,21 Embolization of the right portal vein plus the left medial portal branch11,22,23 was performed, approximately 2 or 3 weeks prior to liver resection, to increase the safety of surgery. The liver volume was estimated before and after embolization as the method reported previously.24 The extent of liver resection decreased by 10% on the average after portal vein embolization (Table 1).
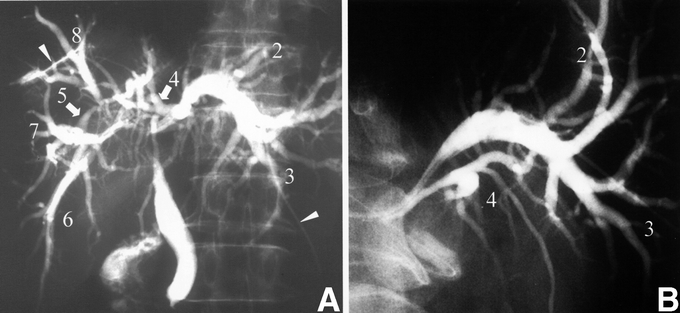
FIGURE 1. Cholangiograms through percutaneous transhepatic drainage catheter (case 2). A, Anteroposterior projection: the progression of cancer is predominant in the right anterior and posterior bile ducts. B, Right anterior oblique + cranial oblique projection: the left medial and lateral branches are also involved. The number indicates the segmental bile duct according to Couinaud's hepatic segment. Arrowheads indicate 2 biliary drainage catheters.
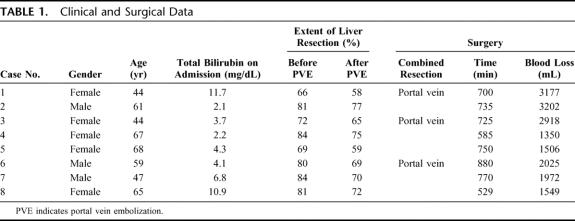
TABLE 1. Clinical and Surgical Data
Surgical Procedure
The first case (case 1 in Tables 1–3) was operated on January 13, 1993 (operator, Y.N.). A laparotomy was performed through an upper midline incision with bilateral subcostal extensions. The distal bile duct was divided in the pancreas. Skeletonization resection of the hepatoduodenal ligament, including dissection of the regional lymph nodes, was performed from the duodenum to the liver. The right hepatic artery was divided. Then, at a more superior level, the right portal vein was divided, and the defect was closed with a continuous suture. In 3 patients, the portal bifurcation adhered to and could not be freed from the tumor during skeletonization resection of the hepatoduodenal ligament. Thus, we performed portal vein resection and reconstruction by end-to-end anastomosis after complete dissection of the transverse portion of the left portal vein.25
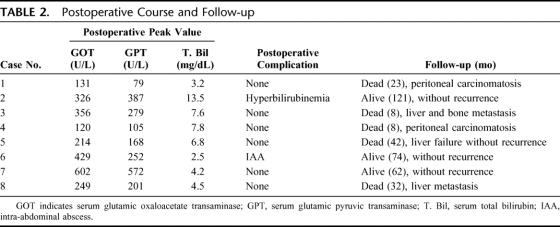
TABLE 2. Postoperative Course and Follow-up
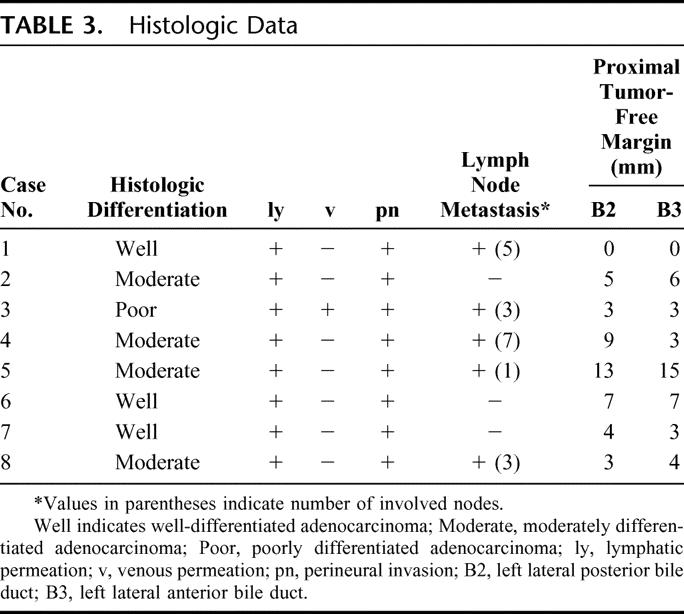
TABLE 3. Histologic Data
After mobilization of the right liver, a number of short hepatic veins were ligated and divided from the caudal to cranial direction as the right lobe was retracted anteriorly and to the left. The right hepatic vein was encircled extrahepatically by cautious dissection, clamped with vascular clamps, divided, and sewn with a continuous suture. All vena caval tributaries except the middle and left hepatic veins were ligated and divided because the caudate lobe was to be totally resected.
The transverse portion of the left portal vein usually gives off several branches to the caudate lobe. These small ramifications were ligated and divided, so that this portion was dissected free from the hilar plate. Next, the umbilical portion of the left portal vein was exposed by dissecting the serosa of the umbilical fissure. When the umbilical fissure was concealed by fusion of the inferior lips of the medial and the lateral sections of the left liver, this liver bridge was divided.
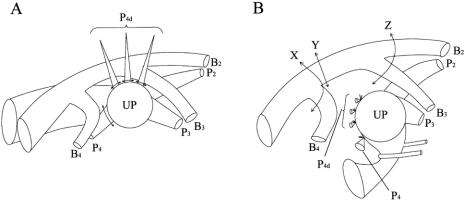
The portal branch of segment 4 (P4) was ligated and divided at its origin. Seven of the 9 patients had 2 P4s: the inferior (P4a) and the superior (P4b) branches arose from the umbilical portion of the left portal vein independently without formation of the common trunk.26 Two or 3 other small ramifications feeding the caudal part of segment 4 also were ligated and divided. Next, the umbilical plate was exposed behind the umbilical portion of the left portal vein as the round ligament was pulled down caudally and to the left. All of the small portal branches (P4d)26 arising from the cranial side of the umbilical portion were carefully ligated and divided (Fig. 2A). The proximal side of the ligamentum venosum also was ligated and divided at the cranial side of the elbow of the left portal vein. Thus, the cranial side of the umbilical portion of the left portal vein was completely detached from the umbilical plate (Fig. 2B). This dissection produced a demarcation along the “left” side, not the right side, of the falciform ligament. This demarcation is usually encountered after pedicle occlusion of the segments 2 and 3 in left lateral sectionectomy.
FIGURE 2. Schematic illustrations (anteroposterior view) of complete dissection of the umbilical plate. A, All of the small portal branches arising from the cranial side of the umbilical portion (P4 days) are divided. B, The umbilical portion (UP) of the left portal vein is isolated from the umbilical plate. Three lines indicate resection line of left-side bile ducts in right hepatectomy (arrow X), conventional right hepatic trisectionectomy (arrow Y), and anatomic right hepatic trisectionectomy (line Z). The number indicates the segmental bile duct (B) and portal branch (P) according to Couinaud's hepatic segment.
Normally, the left hepatic artery originates from the proper hepatic artery, reaches caudally to the base of the umbilical portion of the left portal vein, and enters the base of the umbilical fissure to the left of the umbilical portion. In 1 patient (case 1), however, the left hepatic artery passed to the right, then to the cranial side of the umbilical portion. This anomalous distribution of the left hepatic artery created a technical problem since its presence compromised the detachment of the artery from the left hepatic duct. Albeit with difficulty, the dissection was possible in this particular patient.
The liver dissection was carried out along the demarcation (the left side of the falciform ligament), thereby transecting the middle hepatic vein at the confluence of the left hepatic vein (Fig. 3). Next, as the umbilical portion of the left portal vein was retracted to the left, the bile ducts of the left lateral section were divided at the left side of the umbilical portion of the left portal vein (Fig. 3), proximally to the confluence of the bile ducts from segments 2 and 3 after carefully detaching these bile ducts from the left lateral sectional branches (P2 and P3) of the left portal vein.
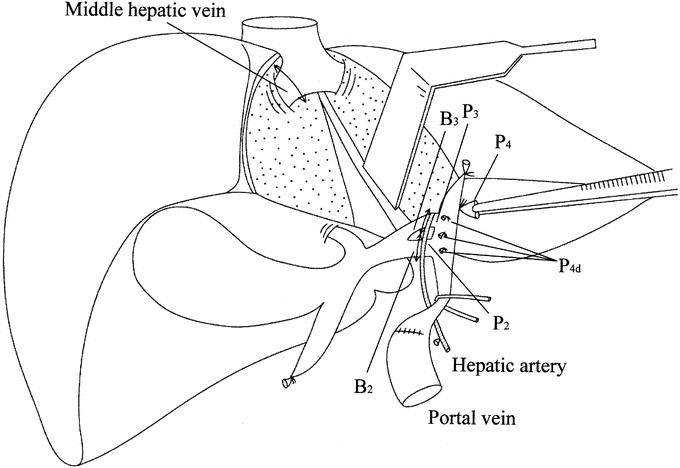
FIGURE 3. Schematic illustration of anatomic right hepatic trisectionectomy with caudate lobectomy. After transecting the middle hepatic vein, the bile ducts of the left lateral section are divided at the left side of the umbilical portion of the left portal vein. The number indicates the segmental bile duct (B) and portal branch (P) according to Couinaud's hepatic segment.
Bilioenteric continuity was reestablished by Roux-en-Y hepaticojejunostomy. The jejunal limb was brought to the hepatic ducts via the retrocolic-anteduodenal (n = 1) or the retrocolic-retrogastric route (n = 7) as reported previously.27 All anastomoses were performed with mucosa-to-mucosa alignment, by interrupted sutures using 5–0 polydioxanone (PDS, Ethicon, Tokyo, Japan), and drained externally by a 6-Fr polyvinyl chloride tube (PTBD tube, Hakko, Chikuma, Japan) introduced via transhepatic or transjejunal route. The tubes were usually removed 3 weeks after hepatectomy.
RESULTS
Liver resection was performed safely without any intraoperative complications. The operative time ranged from 529 minutes to 880 minutes and the blood loss was from 1506 mL to 3202 mL (Table 1). Serum glutamic oxaloacetic transaminase and glutamic pyruvic transaminase levels were moderately (<500 IU/L) elevated after hepatectomy, followed by a return to normal range within 1 week. Insufficiency of hepaticojejunostomy did not occur in any patients. In 6 patients, postoperative recovery was uneventful without any major complications. One patient developed intra-abdominal abscess that required percutaneous drainage. The remaining one patient (case 2) had postoperative hyperbilirubinemia with a peak serum total bilirubin concentration of 13.5 mg/dL. The patient's condition was well, and his bilirubin concentration gradually decreased without any particular therapy. All patients were discharged from the hospital in good condition (Table 2).
Histologically, all patients were diagnosed as having invasive type cholangiocarcinoma with lymphatic permeation and perineural invasion. The length of proximal tumor-free resection margin ranged from 0 mm to 15 mm (Table 3; Fig. 4). Thus, proximal resection margin, despite this extended resection, was positive in 1 patient, whereas negative margin was achieved in the remaining 7 patients. As to long-term follow-up, the patient with positive proximal margin (case 1) did not develop local recurrence around the hepaticojejunostomy but died of peritoneal carcinomatosis. Four patients with multiple lymph node metastases (case 1, 3, 4, and 8) died of cancer recurrence. One other patient (case 5) died of unknown liver failure without recurrence (proved by autopsy) 42 months after hepatectomy. The remaining 3 patients (case numbers 2, 6, and 7) have been well without recurrence for 62, 74, and 121 months after surgery (Table 2).
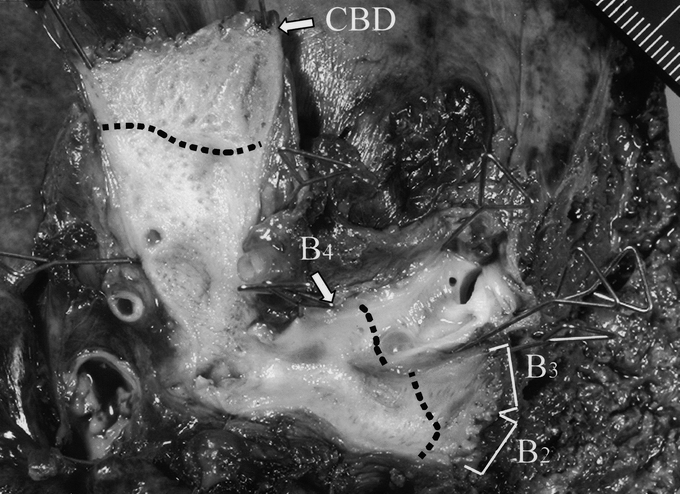
FIGURE 4. The resected specimen (case 2). The extrahepatic bile duct is opened longitudinally, from the distal resection margin (CBD) up to the proximal margin (B2, B3). The left medial bile duct (B4) also is opened. Dotted line indicates the extension of carcinoma.
DISCUSSION
Important matters in liver resection for hepatocellular carcinoma or metastatic liver cancer are division of the feeding arteries and draining portal vein branches of the liver tumor, and obtaining sufficient resection margins around the tumor. Little consideration is given to dividing the bile ducts, so long as the bile duct to be preserved is not injured. In contrast, where the intrahepatic bile duct is divided is critical in the treatment of hilar cholangiocarcinoma, since this tumor originates from and extends along the bile duct intramurally28 or superficially.28,29 Hepatobiliary surgeons, therefore, must understand the differences in resection techniques for hepatocellular or metastatic carcinoma and hilar cholangiocarcinoma.
Starzl et al14 have reported that the blood supply and duct drainage of segment 4 originate within the umbilical fissure and feed back toward the right side buried in liver substance. They have emphasized that in right trisectionectomy these structures should be ligated and divided within the liver substance just to the right of the falciform ligament without entering the umbilical fissure, avoiding injury to the blood supply and duct drainage of the left lateral section. This method is applicable only to right hepatic trisectionectomy for hepatocellular or metastatic carcinoma, in which the left hepatic duct is to be preserved in continuity with the common bile duct. In addition, the proximal portions of segment 4 bile duct are divided along the raw surface of the liver; therefore, this procedure should not be used for cholangiocarcinoma.
It has been proposed that the small part of the liver, which is supplied by small portal branches arising from the cranial side of the umbilical portion of the left portal vein, belongs to segment 4. Takayasu et al26 have reported that a group of these small portal branches appear like a “crest” on the anteroposterior view portogram and are located in the dorsocranial area of the left medial subsegmental territory. Therefore, resection using our methodology would not be “extended” but would be a true “anatomic” right trisectionectomy, whereas that according to Lortat-Jacob et al12 and Starzl et al14,15 would be “subtotal” trisectionectomy.
Right trisectionectomy with caudate lobectomy is indicated for advanced hilar cholangiocarcinoma, which extends to the left hepatic duct near the umbilical fissure with extensive involvement of the intrahepatic bile ducts of the right lobe. In such difficult cases, if the left hepatic duct is divided at the right side of the umbilical fissure, a possibility exists that the resected margin of the left hepatic duct would be cancer-positive. This cut edge of the left hepatic duct is achievable even in right hepatectomy with caudate lobectomy, in which most of the left medial section is preserved. Therefore, only when the bile duct is divided at the left side of the umbilical fissure, right hepatic trisectionectomy for hilar cholangiocarcinoma may be of significance from the viewpoint of achieving cancer-negative margins. If this right hepatic trisectionectomy were not applied, the proximal resection margins of the bile ducts would have been cancer-positive in most of our cases.
Noie et al30 reported performance of anatomic right hepatic trisectionectomy in only 1 patient with hilar cholangiocarcinoma who died of peritoneal dissemination 14 months after surgery. The detailed pathologic data of the patient were not described in their report. In our series, 4 patients with multiple lymph node metastases died of cancer recurrence within 3 years after hepatectomy. The remaining 4 patients survived or are now alive more than 3 years: 3 patients had no lymph node metastasis and 1 patient had only one involved node. These observations suggest that anatomic right hepatic trisectionectomy offers a long-term survival at least in patients without multiple lymph node metastases.
CONCLUSION
We have demonstrated that anatomic right hepatic trisectionectomy with caudate lobectomy, in which the bile ducts of the left lateral section are divided at the left side of the umbilical fissure, can be performed safely even in patients with obstructive jaundice. However, we again stress that in this procedure the greatest care is required to avoid injury of vascular structure to segments 2 and 3. Performance of R0 resection is essential for long-term survival. For this sake, anatomic right hepatic trisectionectomy, in comparison to a right hepatectomy or conventional right hepatic trisectionectomy, can produce a longer resection margin of the left hepatic duct, and this procedure can offer a better chance of long-term survival in some selected patients with advanced hilar cholangiocarcinoma.
Footnotes
Reprints: Masato Nagino, MD, Division of Surgical Oncology, Department of Surgery, Nagoya University Graduate School of Medicine, 65 Tsurumai-cho, Showa-ku, Nagoya 466-8550, Japan. E-mail nagino@med.nagoya-u.ac.jp.
REFERENCES
- 1.Hadjis NS, Blenkharn JI, Alexander N, et al. Outcome of radical surgery in hilar cholangiocarcinoma. Surgery. 1990;107:597–604. [PubMed] [Google Scholar]
- 2.Nimura Y, Hayakawa N, Kamiya J, et al. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535–544. [DOI] [PubMed] [Google Scholar]
- 3.Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogura Y, Mizumoto R, Tabata M, et al. Surgical treatment of carcinoma of the hepatic duct confluence. World J Surg. 1993;17:85–93. [DOI] [PubMed] [Google Scholar]
- 5.Nagorney DM, Donohue JH, Farnell MB, et al. Outcomes after curative resections of cholangiocarcinoma. Arch Surg. 1993;128:871–878. [DOI] [PubMed] [Google Scholar]
- 6.Sugiura Y, Nakamura S, Iida S, et al. Extensive resection of the bile ducts combined with liver resection for cancer of the main hepatic duct junction: a cooperative study of the Keio bile duct cancer group. Surgery. 1994;115:445–451. [PubMed] [Google Scholar]
- 7.Miyagawa S, Makuuchi M, Kawasaki S. Outcome of extended right hepatectomy after biliary drainage in hilar bile duct cancer. Arch Surg. 1995;130:759–763. [DOI] [PubMed] [Google Scholar]
- 8.Nimura Y. Staging of bile duct carcinoma: cholangiography and cholangioscopy. Endoscopy. 1993;25:76–80. [DOI] [PubMed] [Google Scholar]
- 9.Couinaud C. Surgical Anatomy of the Liver Revisited. Paris, 1989. [Google Scholar]
- 10.Strasberg S, Belghiti J, Clavien PA, et al. The Brisbane 2000 terminology of liver anatomy and resections. HPB. 2000;2:333–339. [Google Scholar]
- 11.Nagino M, Nimura Y, Kamiya Y, et al. Right or left trisegment portal vein embolization before hepatic trisegmentectomy for hilar bile duct carcinoma. Surgery. 1995;117:677–681. [DOI] [PubMed] [Google Scholar]
- 12.Lortat-Jacob JL, Robert HG, Henry C. Hepatectomie lobaire droite reglee pour tumour maligne secondaire. Arch Mal Appareil Digestif. 1952;41:662–667. [PubMed] [Google Scholar]
- 13.Belghiti J. Milestones in liver disease: the first anatomical right resection announcing liver donation. J Hepatol. 2003;39:475–479. [DOI] [PubMed] [Google Scholar]
- 14.Starzl TE, Bell RH, Beart RW, et al. Hepatic trisegmentectomy and other liver resections. Surg Gynecol Obstet. 1975;141:429–438. [PMC free article] [PubMed] [Google Scholar]
- 15.Starzl TE, Koep LJ, Weil R, et al. Right trisegmentectomy for hepatic neoplasms. Surg Gynecol Obstet. 1980;150:208–214. [PMC free article] [PubMed] [Google Scholar]
- 16.Nagasue N, Hirose S. Hepatic trisegmentectomy using the Lin liver clamp. Surg Gynecol Obstet. 1983;156:302–304. [PubMed] [Google Scholar]
- 17.Carabasi RA, Messerschmidt WH, Jarrell BE, et al. A method for protection of the left hepatic duct during right hepatic trisegmentectomy. Surg Gynecol Obstet. 1986;162:189–190. [PubMed] [Google Scholar]
- 18.Brower ST, Miller C, McElhinney AJ. Avoidance of injury to the left hepatic duct during parenchymal dissection for hepatic trisegmentectomy. Surg Gynecol Obstet. 1989;168:457–458. [PubMed] [Google Scholar]
- 19.Yanaga K, Kawahara N, Taketomi A, et al. Retrograde right hepatic trisegmentectomy. Surgery. 1996;119:592–595. [DOI] [PubMed] [Google Scholar]
- 20.Nagino M, Hayakawa N, Nimura Y, et al. Percutaneous transhepatic biliary drainage in patients with malignant biliary obstruction of the hepatic confluence. Hepatogastroenterology. 1992;39:296–300. [PubMed] [Google Scholar]
- 21.Nimura Y, Kamiya J, Kondo S, et al. Technique of inserting multiple biliary drains and management. Hepatogastroenterology. 1995;42:323–331. [PubMed] [Google Scholar]
- 22.Nagino M, Nimura Y, Kamiya J, et al. Selective portal vein embolization in preparation for extensive liver resection: the ipsilateral approach. Radiology. 1996;200:559–563. [DOI] [PubMed] [Google Scholar]
- 23.Nagino M, Kamiya J, Uesaka K, et al. Right trisegment portal vein embolization for biliary tract carcinoma: technique and clinical utility. Surgery. 2000;127:155–160. [DOI] [PubMed] [Google Scholar]
- 24.Nagino M, Nimura Y, Kamiya J, et al. Changes in hepatic lobe volume after right portal vein embolization in biliary tract cancer patients. Hepatology. 1995;21:434–439. [PubMed] [Google Scholar]
- 25.Ebata T, Nagino M, Kamiya J, et al. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg. 2003;238:720–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takayasu K, Moriyama N, Muramatsu Y, et al. Intrahepatic portal vein branches studied by percutaneous transhepatic portography. Radiology. 1985;154:31–36. [DOI] [PubMed] [Google Scholar]
- 27.Nagino M, Kamiya J, Kanai M, et al. Hepaticojejunostomy using a Roux-en-Y jejunal limb via the retrocolic-retrogastric route. Langenbeck's Arch Surg. 2002;387:188–189. [DOI] [PubMed] [Google Scholar]
- 28.Sakamoto E, Nimura Y, Hayakawa N, et al. The pattern of infiltration at the proximal border of hilar bile duct carcinoma. Ann Surg. 1998;227:405–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhuiya MR, Nimura Y, Kamiya J, et al. Carcinoma of the hepatic hilus with superficial spreading to the intrahepatic segmental bile ducts. J Hepatobiliary Pancreat Surg. 1993;1:22–26. [Google Scholar]
- 30.Noie T, Bandai Y, Kubota K, et al. Extended right trisegmentectomy for hilar bile duct carcinoma. Hepatogastroenterology. 1997;44:998–1001. [PubMed] [Google Scholar]