Short abstract
The government is committed to improved access to psychological therapy. How big an expansion is necessary to meet the NICE guidelines on depression and anxiety, and how should it be organised?
If you have schizophrenia or bipolar depression in Britain, you will generally get specialist help from the NHS.1 But only about 1% of the British population have these terrible conditions. Many more (some 15% of us) have unipolar depression or anxiety disorders, yet if you have one of these, often crippling, conditions you are unlikely to get any specialist help at all. You can see your general practitioner, but he or she is unlikely to prescribe any treatment other than drugs.
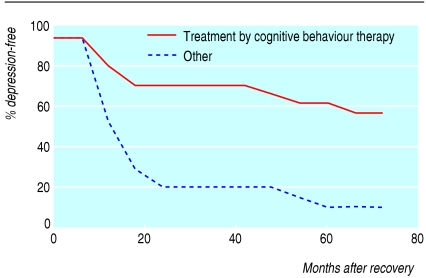
Figure 1.
Risk of relapse after recovery from depression
This pattern of prescribing is completely at variance with the guidelines from the National Institute for Health and Clinical Excellence (NICE) on treating depression and anxiety disorders.2-4 These guidelines recommend that cognitive behaviour therapy should be available as an option for all but the mildest or most recent forms of depression and anxiety. The guidelines also recommend other forms of psychological therapy for selected conditions. The guidelines are, of course, based on hundreds of randomised clinical trials. These show clearly that cognitive behaviour therapy is as effective as drugs for treating depression and anxiety in the short term, and tends to have more durable effects.2-6 Moreover, psychological help is what thousands or even millions of patients want.7
At present it is simply impossible for general practitioners to implement the NICE guidelines because the therapists are not available. Thus mentally ill people are denied specialist help, whereas it would automatically be supplied for equally disabling cases of physical illness. If the NICE guidelines were implemented many more people would receive help, and massive suffering would be avoided. And the cost of implementing the guidelines would be matched by savings to the government in reduced claims for incapacity benefits.
In what follows I shall discuss the scale of need, and show that the overall benefits of meeting it exceed the costs. I shall then show why the expanded provision should be provided through psychological treatment centres.
The cost of depression and anxiety
According to the World Health Organization, half of all people with ill health in Western Europe have mental illness.8-10 It accounts for as much suffering as all physical illnesses put together. And the bulk of these mental illnesses are depression and anxiety.
There is also a huge economic cost, because depression and anxiety make it much more difficult, or impossible, to do a job. And those capable of working are likely to have high rates of sickness absence.1 The resulting loss of output can be calculated as £17bn (€24bn, $30bn), or 1.5% of UK gross domestic product.11 Much of this cost falls on the Exchequer, which loses in consequence roughly £9bn in benefit payments to mentally ill people and in reduced tax receipts. There are now more than one million mentally ill people receiving incapacity benefits—more than the total number of unemployed people receiving unemployment benefits. So in Britain mental illness has now taken over from unemployment as our greatest social problem.
Cost effective treatments
Fortunately, much of this suffering and economic waste can be prevented by new treatments developed in the past 50 years. The new drug treatments are now available to all, but the psychological therapies are not: only 4% of all those with depression and anxiety disorders have received such therapy in the past year.1 Yet, according to NICE, psychological therapies are at least as effective as drugs. Many patients do not want to take drugs but would like “therapy.” This is one of many reasons why only a quarter of all those who are mentally ill are receiving any form of treatment (including drugs).1 If we are to tackle our mental health problems effectively, we need to deploy the evidence based psychological therapies on a large scale.
These therapies are quite different from traditional psychoanalysis. They are forward looking and practical, and they typically involve no more than 16 sessions. The best developed, and most studied, is cognitive behaviour therapy, in which patients are taught to challenge their negative thoughts and to pursue positive strategies to build on their strengths. A typical finding for depression (in double blind clinical trials) is that either drugs or weekly therapy will lift about half of the treated patients out of depression within four months. After successful treatment the risk of relapse is greater for those treated with drugs, unless they keep on taking them (figure).13-15 Thus the cost effectiveness of the two approaches is similar, but many people refuse drugs because of side effects and because they want to feel more in control of their emotions.
Recovery rates after therapy for anxiety disorders are similar to those for depression (when weighted by the types of disorder),2-4 but the benefits are greater because spontaneous recovery rates are lower. So the case for wider access to therapy is even more compelling.
Should the Treasury support psychological therapy? The cost of therapy would be about £750 for each patient who embarked on treatment.16 In the next two years the likely effect, compared with no treatment, would be about 12 extra months free of illness and at least one extra month in work, after allowing for natural recovery that could otherwise occur. In terms of extra output, the extra time in work is equivalent to more than £1880, which more than repays the £750 cost of treatment, without including the benefits of reduced suffering. To value the reduced suffering in money terms is not easy, but if we assume that a year free of illness is worth 0.2 QALYs (quality adjusted life years),17 the extra year without illness is worth about £6000 (assuming a QALY is “worth” £30 000, in line with values used by NICE).
Even for the Treasury's own book-keeping, the therapy repays its £750 costs through savings on incapacity benefits and higher taxes of around £850 within two years of treatment. On top of this, there would be considerable savings to the rest of the NHS. Fewer people would become so mentally ill that they needed hospitalisation or outpatient treatment. (In one study, when cognitive behaviour therapy was made available to depressed patients via computer, their general practitioners referred 80% fewer people to secondary services.18) In addition, fewer people would keep attending their general practitioners or be sent for counselling. And fewer people would be referred for supposed physical illnesses (in London a half of referrals to acute hospitals failed to reveal a “medically explicable” physical condition).19
From the available evidence, NICE recommends cognitive behaviour therapy for every type of disorder, and various other treatments (such as family therapy and interpersonal therapy) for a limited range of disorders. While further research will probably show the wider value of other types of treatment, it seems sensible to base any proposed expansion of psychological therapy at this stage predominantly on cognitive behaviour therapy. This does not mean that the alternatives should disappear, but a major expansion, requiring large expenditure, has to be guaranteed to succeed and must therefore rely on the evidence available so far. These ideas have received general support with the British Psychological Society (personal communication, Graham Turpin, chair of the Division of Clinical Psychology, British Psychological Society; see also Roth and Stirling20).
More therapists
So what scale of expansion is needed? It is important for the government to begin by envisaging what kind of provision is necessary and justified, and only after that to consider how fast it could be established. About 2.75 million people go to their general practitioner with a mental problem during a year. Of these patients, roughly a third would probably opt for psychological therapy if it were available (and more would be encouraged to visit their doctor). Therefore, about 800 000 patients a year would require (mostly) cognitive behaviour therapy.
If we assume there is one therapist for every 80 patients treated in a year, we need an extra 10 000 therapists. There are two possible sources—clinical psychologists or a new type of “psychological therapist.” At present we produce 550 new clinical psychologists a year; this number should rise sharply, and most should go into providing therapy—say 5000 extra by 2013. The other 5000 therapists should be newly trained “psychological therapists” drawn from mainly older people with experience of mentally ill people—nurses, occupational therapists, social workers, and counsellors. They should be given rigorous training in (mostly) cognitive behaviour therapy while in employment. The “off the job” training would be part time, and there would be a one year qualification in cognitive behaviour therapy for a limited range of conditions and a two year qualification for a wider range of conditions, including some that are more complex.
Treatment centres
The final issue is how the work of these therapists should be organised in order to guarantee its effectiveness. The answer is: in as similar a way as possible to the clinical trials that showed it to be effective. This means that the therapists should work in teams, where junior therapists can be properly supervised, motivated, supported, and trained by senior therapists. Cognitive behaviour therapy is not like a drug, which is the same whoever administers it; it is much more effective when it is more professionally administered.21 So general practitioners should welcome the opportunity to refer patients to such teams rather than trying to organise the therapists themselves. These teams would operate on a “hub and spoke” basis, with the senior therapists being based in one building, but the bulk of therapy being delivered in general practices, job centres, workplaces, voluntary organisations, etc.
Summary points
NICE guidelines say that most patients with depression and anxiety disorders should be offered evidence based psychological therapies
Such treatments yield economic benefits that exceed the cost. There is no net cost to the government because of savings on incapacity benefits and other NHS costs
To implement the guidelines requires some 10 000 more therapists. Training this number is feasible over a seven year period
The extra therapists should work in teams with a central building, but much of the therapy should be given at “satellite” sites such as general practices and in job centres. Some 250 of these psychological treatment centres should be set up over the next seven years
The team structure makes it possible for the senior therapists to make the initial diagnosis and assign the patient to an appropriate therapist. All therapists would use a standard one page questionnaire to measure patient progress, which makes effective monitoring possible—and, if used nationally, makes it possible to compare the effectiveness of different teams. The team structure also allows for more flexible appointments and for individual therapists to develop particular areas of expertise. And a central building provides a location for case conferences, consulting rooms when these are not otherwise available, and a place to which patients can self refer when they do not wish to go through their general practitioner.
The name for these teams should make clear their connection with the central building, and they might be called psychological treatment centres (or therapy centres, if the phrase appeals). The idea of psychological treatment centres has received widespread support. A suitable objective for, say, 2013 would be one treatment centre for every 250 000 people: the centres would therefore have much longer spokes in rural than in urban areas. This would mean roughly 250 centres altogether in the UK. In rolling out such a system, it is vital to maintain quality throughout. A sensible objective could be to roll out 40 new centres each year, with each centre providing a training ground for future centres.
The alternative is a more decentralised and locally varied approach, in which it could be much more difficult to ensure quality and patient safety: bad therapy can easily do harm. To achieve a sufficient volume and quality of therapy will require in the initial phases a strong lead from the Department of Health.
The fundamental case for expansion is the evidence that therapy works. This evidence comes from trials conducted in psychological treatment centres. The expansion should therefore be provided through teams based in centres but reaching out to people near their homes. If this is well done, it could transform the lives of millions, at no net cost to the Exchequer.
Contributor and sources: RL directs the Well-being Programme in the Centre for Economic Performance at the London School of Economics. In January 2005 he was invited by the prime minister's strategy unit to present the paper “Mental health: Britain's biggest social problem?.” Discussions after this led to a Labour Party Manifesto commitment to expand psychological therapy in the NHS. The Department of Health now has a programme on improved access to psychological therapy, to design and promote the necessary expansion. Two pilots will begin shortly. RL and other members of the Mental Health Policy Group, which meets at the Centre for Economic Performance, have written a preliminary cost-benefit analysis for the expansion.
Competing interests: None declared.
Editorial by Scott and p 1027
References
- 1.Office for National Statistics, Psychiatric morbidity survey. London: ONS, 2000.
- 2.National Institute for Clinical Excellence. Depression: management of depression in primary and secondary care. London: NICE, 2004. (Clinical guideline 23.)
- 3.National Institute for Clinical Excellence. Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care. London: NICE, 2004. (Clinical guideline 22.) [PubMed]
- 4.National Institute for Clinical Excellence. Post-traumatic stress disorder (PTSD): the management of PTSD in adults and children in primary and secondary care. London: NICE, 2005. (Clinical guideline 26.)
- 5.Clark DM, Ehlers A, McManus F, Hackmann A, Fennell M, Campbell H, et al. Cognitive therapy versus fluoxetine in generalized social phobia: a randomized placebo-controlled trial. J Consult Clin Psychol 2003;71: 1058-67. [DOI] [PubMed] [Google Scholar]
- 6.Liebowitz MR, Heimberg RG, Schneier FR, Hope DA, Davies S, Holt CS, et al. Cognitive-behavioral group therapy versus phenelzine in social phobia: long-term outcome. Depress Anxiety 1999;10: 89-98. [PubMed] [Google Scholar]
- 7.Levenson R, Greatly A, Robinson J. London's state of mind. London: King's Fund, 2003: 86.
- 8.WHO International Consortium in Psychiatric Epidemiology. Cross-national comparisons of the prevalences and correlates of mental disorders. Bull World Health Organ 2000:78: 413-26. [PMC free article] [PubMed] [Google Scholar]
- 9.Layard R. Happiness: lessons from a new science. London: Penguin Books, 2005.
- 10.Layard R. Sainsbury Centre lecture: Therapy for all on the NHS. http://www.scmh.org.uk/80256FBD004F3555/vWeb/flKHAL6H3D4F/$File/Layard%20Lecture%20SCMH%20120905.doc (accessed 30 Mar 2006).
- 11.Layard R. Mental health: Britain's biggest social problem? Available at http://cep.lse.ac.uk/layard/ (accessed 7 Apr 2006).
- 12.Fava GA, Ruini C, Rafanelli C, Finos L, Conti S, Grandi S. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry 2004;161: 1872-6. [DOI] [PubMed] [Google Scholar]
- 13.Craighead W, Hart A, Craighead L, Ilardi S. Psychosocial treatments for major depressive disorder. In: Nathan P, Gorman J, eds. A guide to treatments that work. Oxford: Oxford University Press, 2002: 245-61.
- 14.Hollon S, Beck A. Cognitive and cognitive behavioural therapies. In: Lambert M, ed. Handbook of psychotherapy and behavior change. 5th ed. New York: John Wiley, 2004.
- 15.Department of Health and Human Services. Mental health, a report of the surgeon general. Rockville, MD: DHHS, 1999.
- 16.Layard R, Clark D, Knapp M, Mayraz G. Implementing the NICE guidelines for depression and anxiety. A cost-benefit analysis. Available at http://cep.lse.ac.uk/layard/ (accessed 7 Apr 2006).
- 17.Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord 1998;48: 25-36. [DOI] [PubMed] [Google Scholar]
- 18.Marks I, Mataix-Cols D, Kenwright M, Cameron R, Hirsch S, Gega L. Pragmatic evaluation of computer-aided self-help for anxiety and depression. Br J Psychiatry 2003;183: 57-65. (With further information from Marks.) [DOI] [PubMed] [Google Scholar]
- 19.Nimnuan C, Hotopf M, Wessely S. Medically unexplained symptoms: an epidemiological study in seven specialities. J Psychosom Res 2001;51: 361-7. [DOI] [PubMed] [Google Scholar]
- 20.Roth T, Stirling P. Expanding the availability of psychological therapy: Lord Layard's inaugural Sainsbury Centre for Mental Health lecture. Clinical Psychology Forum 2005;Nov(155): 47-50.
- 21.Roy-Byrne PP, Craske MG, Stein MB, Sullivan G, Bystritsky A, Katon W, et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry 2005;62: 290-8. [DOI] [PMC free article] [PubMed] [Google Scholar]