Abstract
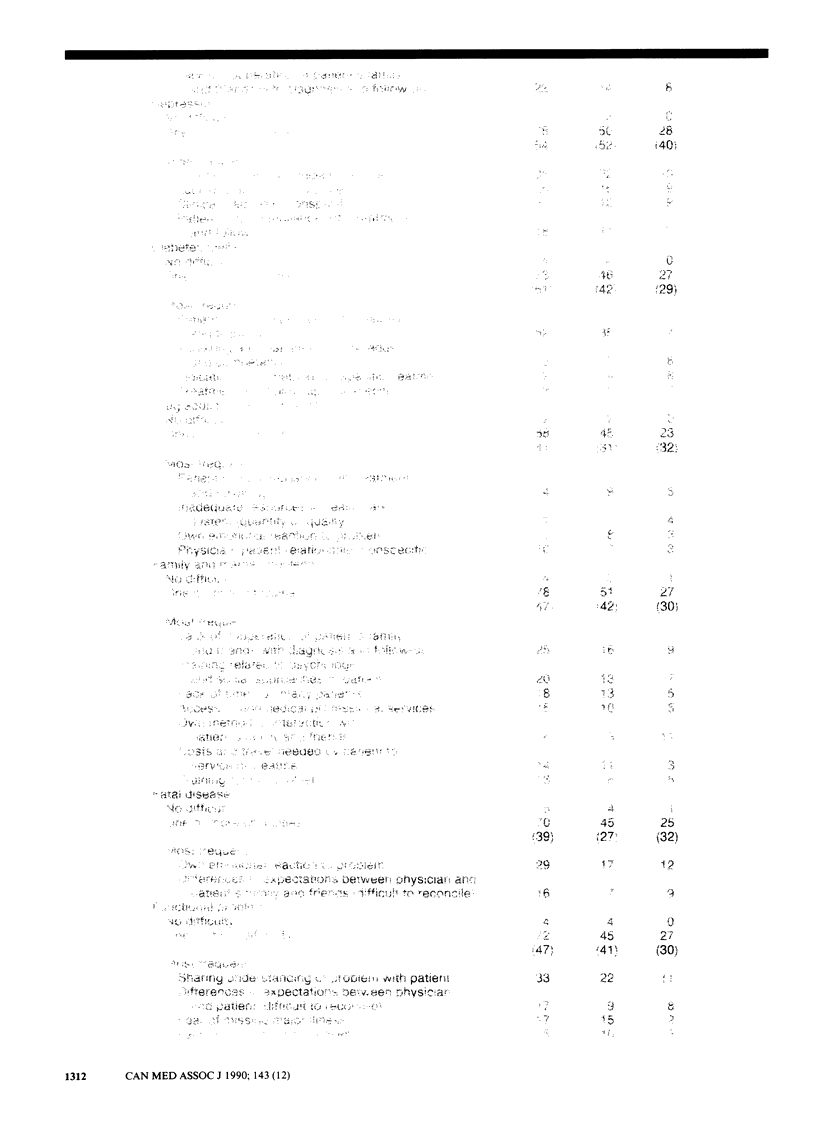
This study was conducted to describe the difficulties perceived by general practitioners concerning 24 common clinical problems and to compare their perceptions with those of faculty members in family medicine. A random sample of 467 general practitioners and all 182 faculty members in family medicine in Quebec were sent one of four open-ended questionnaires, each of which dealt with six clinical problems; 214 general practitioners and 114 faculty members participated. A total of 5111 difficulties were reported; the number reported by each subject varied from 0 to 13 (mean 2.6 [standard deviation 2.09]) per problem. The problems that generated the most difficulties were depression, confusion in the elderly, chronic back pain, loss of autonomy in the elderly and sexually transmitted disease. The most frequent difficulties were with the patient's noncompliance with treatment, clinical diagnosis, failure of a specific treatment, inadequate health care resources and the physician's own emotional reactions. The difficulties for each problem were the same in the two groups 70% of the time. Physician's perceptions of their difficulties can be useful in the planning of initial training and continuing medical education.
Full text
PDF








Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barham P. M., Benseman J. Determining continuing medical education curricula for general practitioners--a survey of self-perceived needs. N Z Med J. 1983 May 25;96(732):395–397. [PubMed] [Google Scholar]
- Curry L., Putnam R. W. Continuing medical education in Maritime Canada: the methods physicians use, would prefer and find most effective. Can Med Assoc J. 1981 Mar 1;124(5):563–566. [PMC free article] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–174. [PubMed] [Google Scholar]
- Schneeweiss R., Rosenblatt R. A., Cherkin D. C., Kirkwood C. R., Hart G. Diagnosis clusters: a new tool for analyzing the content of ambulatory medical care. Med Care. 1983 Jan;21(1):105–122. doi: 10.1097/00005650-198301000-00008. [DOI] [PubMed] [Google Scholar]
- Sibley J. C., Sackett D. L., Neufeld V., Gerrard B., Rudnick K. V., Fraser W. A randomized trial of continuing medical education. N Engl J Med. 1982 Mar 4;306(9):511–515. doi: 10.1056/NEJM198203043060904. [DOI] [PubMed] [Google Scholar]



