Abstract
Since the signing of the Oslo Peace Accords and the establishment of the Palestinian Authority in 1994, reform activities have targeted various spheres, including the health sector. Several international aid and UN organizations have been involved, as well as local and international non-governmental organizations, with considerable financial and technical investments. Although important achievements have been made, it is not evident that the quality of care has improved or that the most pressing health needs have been addressed, even before the second Palestinian Uprising that began in September 2000. The crisis of the Israeli re-invasion of Palestinian-controlled towns and villages since April 2002 and the attendant collapse of state structures and services have raised the problems to critical levels. This paper attempts to analyze some of the obstacles that have faced reform efforts. In our assessment, those include: ongoing conflict, frail Palestinian quasi-state structures and institutions, multiple and at times inappropriate donor policies and practices in the health sector, and a policy vacuum characterized by the absence of internal Palestinian debate on the type and direction of reform the country needs to take. In the face of all these considerations, it is important that reform efforts be flexible and consider realistically the political and economic contexts of the health system, rather than focus on mere narrow technical, managerial and financial solutions imported from the outside.
Keywords: health sector reform, conflict, Occupied Palestinian Territories
Introduction
While the movement to reform health care is not new, the understanding of the health of a population, its determinants and ways to improve it has become far more sophisticated in recent times. Approaches to reform efforts have had to take into account the broader definition of health as a social construct as well as the economic, political and social contexts in which health services are provided.
For decades now, and in response to various pressures, developed and developing countries alike have been taking steps to change the policies and practices of their health systems (Sen and Koivusal 1998). In its modern sense, health sector reform (HSR) has featured prominently on the international health policy agenda since the late 1980s. What characterizes this contemporary version of HSR – and perhaps sets it apart from previous types of reform – is its association with ‘a particular set of policy prescriptions’ aiming at institutional and financial reform, principally introducing increasing market mechanisms in health care provision (Standing 1999). In the developing world, such reform has been largely, though not solely, donor-sponsored, with the World Bank assuming a leading role.
To date, there have been numerous examples of World Bank-supported HSR initiatives worldwide, driven by similar initial definitions and conceptual tenets. However, reform remains a highly context-dependent process. Even when dealing with the same political and financial driving forces, reform options and the realities of implementation diverge. This is partly due to conditions, which vary from country to country, such as the relative presence of political interest, will and capacity to implement reform (Standing 1999). Existing models seem to take as given certain pre-conditions, such as the presence of at least a general consensus regarding the ways in which society should proceed on its path to development, strong state institutions and structures, a relatively open and active economy, a vibrant civil society, rational action in policy-making, and the availability of minimum household and national resources. In fact these pre-conditions may not all be present in a particular setting. The structural conditions within which health systems develop and the constraints imposed by a particular setting must have an impact on the way in which reform can or cannot proceed. Such realities call for flexibility in approaching reform in differing contexts and for the exercise of great care regarding universal policies adopted by international aid agencies for implementation in sometimes very differing settings.
In the Occupied Palestinian Territories (OPT), as in other contexts, the structure, function and capacity of the health system has been shaped largely by the country’s complex political history. Since the signing of the Oslo Peace Accords and the establishment of the Palestinian Authority (PA) in 1994, reform activities have been taking place in the health sector with the involvement of several international aid and United Nations (UN) agencies as well as local and international non-governmental organizations (NGOs). This paper will take a critical look at recent developments in the health sector in the OPT, with the aim of contributing to the debate on whether the current approach to reforming the health care system can be effective in fulfilling people’s health needs. Specifically, the paper attempts to analyze the defects of the current approaches to reform by showing that, in the Palestinian case, the assumptions of the pre-conditions described above are simply and fundamentally flawed. Indeed, the Palestinian case of HSR demonstrates the inter-relatedness of health and politics and the importance of an analysis of health needs within a systemic context. Basing that analysis solely on biological and medical indicators, divorced from the social and environmental determinants, may lead investors in reform to the illusion that narrow technical and administrative solutions can solve complex health problems. In the Palestinian case, this microcosmic rather than systemic focus has led to investments in unworkable strategies. In this article, we will attempt to unravel where HSR, intended to engender a sustainable process (Berman 1995), has missed the forest for the trees, thus resulting in wasted resources and frustrated expectations. A description is necessary first of the geopolitical context and historical evolution of the Palestinian health system, in order to understand the root causes of its current difficulties. The paper will then analyze what have been, in our assessment, the major obstacles undermining reform approaches.
Perhaps it is important to point out that this paper does not attempt to evaluate the impact of reform initiatives implemented so far. In our opinion, such an evaluation is not possible at this time, both because of the ongoing state of conflict and destabilization of Palestinian Authority systems, including the health system, and because of the relatively short amount of time that has elapsed since the beginning of the reform initiatives (in this case, since the signing of the Oslo Peace Accords and the establishment of the Palestinian Ministry of Health). However, with evidence of systemic collapse even before the renewal of the second Palestinian Uprising (Intifada), it seemed important to reflect on and question the approach to reform that has been taken so far.
While it is recognized that the situation of this developing country is a complex one, where rapid changes and political instability make it difficult to plan for the future, it is a key moment to take a critical look at health sector reform, as governmental systems are being established and policies are being formulated. Investigating the context in which changes in the health sector have taken place might contribute to a clearer vision of what is needed and what might be realizable in the future. Furthermore, in its broader framework, the Palestinian experience may also assist in improving our understanding of reform efforts in other countries of the world that endure endemic conflict and instability.
The geopolitical context of the Palestinian health care system
The modern geography of the OPT can only be understood in the context of its political history.1 Today, the OPT, a combined area of 6000 km2, are divided into two geographically distinct territorial units, the West Bank and the Gaza Strip separated by the State of Israel (World Bank 1998). The West Bank and Gaza, differing in their natural landscape, population distribution and legal systems, are inhabited by about 2.9 million individuals (including Arab East Jerusalem), of whom 65% reside in the West Bank (Palestinian Central Bureau of Statistics 1999: 39). The latter has a low population density (230 inhabitants per km2) with about one-fifth of the population consisting of refugees, whereas Gaza is ‘one of the most densely populated areas of the world’, with 2100 inhabitants per km2, of whom 65% are refugees (Khawaja 2000).
Approximately 47% of the Palestinian population is below 15 years of age (Palestinian Central Bureau of Statistics 1999: 49). Certain health and development indicators show important disparities between the two regions. For example, the total fertility rate (TFR) in the West Bank is 5.44 compared with 7.41 in the Gaza Strip, and the infant mortality rate (IMR) is 25.5 and 30.2 per 1000 live births in the West Bank and Gaza Strip, respectively (Palestinian Central Bureau of Statistics 1998a). In 1998, the West Bank and Gaza had a GNP per capita of US$1800 and as such were categorized as a lower-middle income economy by the World Bank. However, since the year 2000, per capita incomes have drastically decreased with the collapse of the Palestinian economy, due primarily to restrictions on movement of people and goods. It was estimated that by the beginning of 2002 not less than 45–50% of the Palestinian population were living below the poverty line (of US$2 per person per day) (World Bank 2002: iv).
It is noteworthy that the geographical divisions aggravated by the political conditions of the past several years have produced two separate de facto government health systems, one for Gaza and the other for the West Bank. This point seems to be missed by donors and current reform policies. The situation on the ground has led to the near impossibility of unifying and standardizing the two geographically isolated health sectors, creating redundancy in positions and bureaucracy and widening the already existing gap between the two regions. All these developments are antithetical to the goal of efficient health sector reform.
The evolution of the Palestinian health care system
Historical events during the past century have had a profound influence on the characteristics of the health system emerging today. Years of colonization and military occupation have shaped the capacity of the health system and defined its main actors. The evolution of the Palestinian health care system will be described in four eras: the British Mandate period (1920–48), the Jordanian and Egyptian rule (1948–67), Israeli Administration (1967–94) and the Palestinian Authority (1994–2000). The start of the second Palestinian Uprising in September 2000 marked a new reality, which changed living conditions in the country as a whole and necessarily radically influenced the functioning of the health system. The events since 2000 will also be considered in this paper.
Services during the British Mandate Period, 1920–48, and Jordanian and Egyptian Rule, 1948–67
Following World War I, with Palestine under the British Mandate, health services were provided by the Government Department of Health under the British Civil Administration between 1920–48. While some government hospitals and health clinics were provided for the Arab population, British colonial policy aimed to limit investments in the social services in the region, and thus the rural areas of the country, where most of the poor Palestinian population resided, had very limited access to medical services. Many city dwellers were able to utilize the Christian Mission hospitals and the government hospitals in the major Palestinian cities.
The 1948 Arab–Israeli War brought about the creation of the State of Israel and the displacement of the Palestinian population, whereby approximately 750 000 Palestinians became refugees (Sanbar 1984: 202). Immediately after the war, while Jordan ruled the West Bank and Egypt administered the Gaza Strip, two separate health systems began to emerge. Furthermore, the United Nations Relief and Works Agency for Palestine Refugees (UNRWA) was established by the United Nations General Assembly in 1949 and began operations in 1950, with the mandate to ‘carry out direct relief and works programmes for Palestine refugees’.2 Thus, as of the late 1950s, modern medical services began to become available to refugees and to the rural areas, as basic health and education infrastructures reached the countryside. However, those health services were mainly curative and rudimentary (Giacaman 1994).
The Palestinian health system under Israeli Administration: 1967–94
On the eve of the 1967 occupation of the West Bank and Gaza by Israel, there were three systems for health service provision operating in the area. The governments of Jordan and Egypt supervised the public system in the West Bank and the Gaza Strip, respectively, while UNRWA provided health services for refugees. The private sector included charitable organizations operating major hospitals and diagnostic centres or primary care centres. Following the occupation, the Israeli Civil Administration (under the Ministry of Defense and not the Ministry of Health) took over the governmental health care system and proceeded to administer it in a manner that kept it stunted and underdeveloped, with severe budget restrictions, referral to Israeli hospitals for tertiary care, and restrictions on licenses for new medical and health care projects, thus creating a total dependence on the Israeli health system (Giacaman 1994). In addition, health service delivery in that era was characterized by the disempowerment of the Palestinians in decision-making and top-level management. Although the actual service providers were all Palestinians, institutions were not developed to meet the changing needs and growth of the Palestinian population, nor were they strengthened so that they could function autonomously.
UNRWA was able to develop its own system of basic services, including health, education, relief and social services, for the refugees relatively independently. However, with the highly centralized administration in Vienna, the bureaucratic structure did not foster Palestinian capacity building and leadership at the top echelon. As for the private sector, operating small hospitals and basic medical clinics owned and run by individual physicians on a fee-for-service basis, it attempted to provide an independent alternative in health service provision, but was subject to Israeli military rules and licensing restrictions that prohibited any serious development. In defiance and in response to the acute needs of the population, grassroots popular health committees, affiliated with Palestinian political movements, emerged in the late 1970s. Although small, they were determined to fill the gaps left by the Israelis in health service provision. These active and activist NGOs based their approach on reaching out to underserved areas with volunteer health providers and promoting preventive care, health education activities, popular participation in addressing health issues and grassroots mobilization in addition to basic curative services (Barghouthi and Giacaman 1990).
The health system under the Palestinian Authority: 1994–2000
In 1993, Israel and the Palestine Liberation Organization (PLO) signed an historic Declaration of Principles followed by a 1994 Agreement on the Gaza Strip and Jericho Area, which set the stage for the creation of the Palestinian Authority (PA) later that year. A subsequent series of negotiations and agreements resulted in further phased-out transfer of powers and responsibilities to the PA, including overall responsibility for health care provision. The Palestinian Ministry of Health (MoH) was established in 1994. In the current context, the Ministry of Health is the primary provider of health services to the population, with about 40% of primary health care visits taking place at government facilities, 31% at UNRWA and 29% at private and NGO facilities (Policy Research Incorporated 1999: 6).
The enormous task of rebuilding the ailing system has been aided by substantial donor assistance. Between 1994 and mid-1999, donors committed some US$353 million to the health sector and disbursed approximately half of that amount in actual assistance (Government of Japan and World Bank 2000: 43). HSR projects in the past years have focused on upgrading and expanding infrastructure, institution building within the Ministry and human resource development. Accomplishments have been considerable in constructing new hospitals in the West Bank and Gaza and in increasing the number of government primary health care clinics from 207 to 365 between 1994 and 1998,3 as well as gradually integrating family planning services initially into about 100 of these clinics. The ministerial structure was set up; a national health information system was developed; a government health insurance scheme was promoted; a plan for human resource development was developed and training carried out in certain areas such as women’s health; and participatory planning with the four categories of service providers (government, UNRWA, NGO and private) in developing policies and protocols in maternal and child health was undertaken.
Expanded coverage of government health insurance has also been one of the priorities of the Ministry of Health, which succeeded in increasing the number of adherents between 1994 and 1998 from 25% of households to 48% (Policy Research Incorporated 1999: 6), but with considerable mandatory coverage for the employees of the state in addition to police and security personnel. However, the financial crisis of the Ministry of Health beginning in the second half of 1997, when the Ministry of Finance failed to allocate it the expected budget, led to a deterioration of government services including a lack of essential drugs and supplies. This in turn resulted in a decline in public participation in the governmental health insurance programme (Economic Policy Research Institute 2000). Direct out-of-pocket household expenditure on medical care has come to account for 40% of total health expenditure in the West Bank and Gaza Strip (Policy Research Incorporated 1999: 4), raising concerns about equity in health care, particularly given rising poverty and the needs of the thousands injured by the Israeli army, who require long-term care.
Faced with the new situation on the ground, the role of nongovernmental health organizations began to change in several respects. Certain NGOs have had to downsize their operations, while others remain significant providers of essential services, such as primary care services, community-based rehabilitation, mental health schemes and health education, and they constitute a vital platform for debate on issues of health policy and planning, centralization/decentralization, coordination and information-sharing. While the private sector has expanded rapidly in the past few years (Barghouthi and Lennock 1997: 22–3), with phenomena such as group practices and private health insurance schemes beginning to develop, the extent to which its practices are monitored and regulated as well as the implications for the public sector of its rapid growth remain unclear.
Major obstacles to HSR initiatives
The following section outlines what, in our view, have been the major obstacles to reforming the health sector. Basically, it analyzes the faulty underlying assumptions of the presence of certain pre-conditions in the Palestinian context that are necessary for genuine and effective reform. Those include a stable, peaceful political environment with an active economy, strong state institutions and structures, internal political and popular will to implement reform, and the presence of a policy dialogue on what types of reforms the country should invest in.
Ongoing conflict and the assumption of transition to peace-building
Reform initiatives in the OPT have taken a path similar to those in other post-conflict situations in the sense that they were based on the assumption that the country was entering a period of peace-building and political transition following prolonged conflict.4 In fact, however, the Oslo period proved to yield a contrary reality that consistently undermined HSR initiatives. Despite the apparent progress in state building that began with the Oslo peace process, the situation on the ground remained highly problematic. By 1998, it had become clear that a final and peaceful solution to the long conflict between Israelis and Palestinians was not materializing, and old problems were deepening as the post-Oslo period was marked by severe economic deprivation, a seemingly permanent bantustanization and isolation of villages and towns (Figure 1), restrictions on the movement of the Palestinian population, and increasing expropriation of land and natural resources for settlement expansion or bypass roads. In short, the process had come to be perceived by Palestinians as entailing a string of negative economic, social, political and human consequences. The area had undergone continuous crises after the signing of the Accords (Giacaman and Lonning 1998: ix–x), and in September 2000, despite the massive international aid that had been poured into the country to buffer the deteriorating situation on the ground, the political interim solution exploded with the second Palestinian Uprising (Intifada), leading to a very serious undermining of already fragile public institutions and services.
Figure 1.
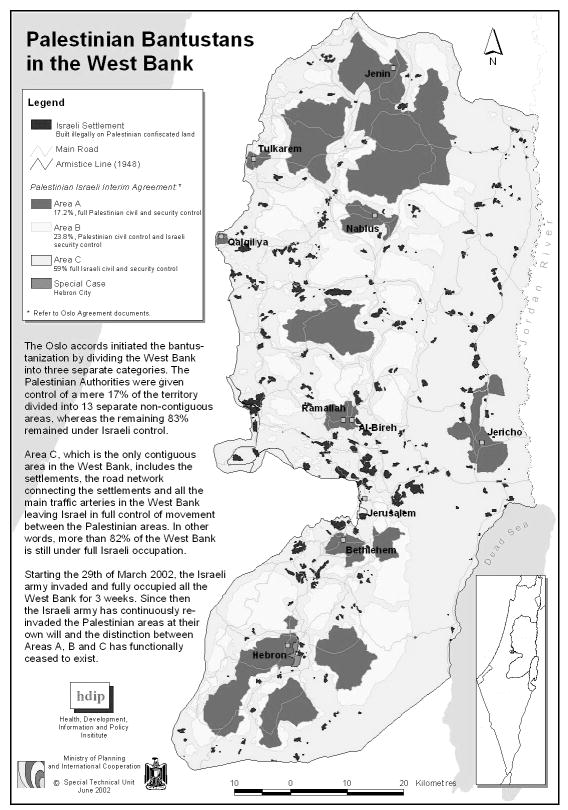
Palestinian Bantustans in the West Bank
Overnight, these events drove the OPT into an unprecedented economic crisis with at least half of the population living under the poverty line by the beginning of 2002 (World Bank 2002). In addition, the death of over a thousand Palestinians, the injury of thousands more, and the substantial destruction of property and infrastructure including roads, as well as the shelling and occasional ramsacking of hospitals, all contributed further to the precipitation of a health system crisis, undoing to a considerable extent donor-led attempts at reform. The situation since the re-invasion of Palestinian-controlled areas beginning on 29 March 2002 has become even more critical.
Endeavours to build capacity within the Ministry of Health and within health institutions were foiled by the overwhelming need to meet the emergency situation. This focus on emergency needs, however, has led to the abandonment of the goal of system-building. Reform attempts turned once again to relief, dwarfing, for instance, years of work in developing an essential drug list and a rational drug use programme, and interrupting the debate on how to finance government health services, such as introducing user fees. In response to the national emergency, the Ministry of Health began, quite rightly, to provide free services to the insured and un-insured alike and to receive drug donations from international donors that undermined the use of its essential drug list, undoing its attempts at rehabilitating prescription patterns and along the way, further weakening the local drug industry.
Thus the ongoing national liberation struggle and conflict with Israel is not only proving to be protracted and seemingly never-ending, but also making current reform efforts seem impossible to achieve. This means that, although one should not give up on attempts at reform, assumptions pertaining to a post-conflict setting in the OPT must be modified to suit the harsh reality of ongoing strife. Policies need to be guided by the principle of mixing selected possible and realizable reform measures with relief and emergency operations, rehabilitation and reconstruction. Otherwise, reform operations are likely to be frustrated by events.
Weakened Palestinian state structures and institutions
The nature and functioning of PA structures: dependence and authoritarianism
In order to understand the political system and policy environment in which reform has been attempted in the OPT, and consequently assess the feasibility and the potential for success of reform schemes, one needs first to examine the nature of the Palestinian regime that emerged in the post Oslo period. The policy environment is characterized by dependence: political dependence as defined by the Oslo Accords and economic dependence on the Israeli market and international assistance. Within this context, the state-like structure has emerged. As early as 1997, various analysts began to note that what appears to be a process of modern state building was not necessarily characteristic of the reality on the ground. The use of customary law and the promotion of extended families and kinship groups by the PA were beginning to be questioned as perhaps part of a ‘broad strategy for de-politicizing society and centralizing power by weakening modern groups and strengthening tradition’ (Frisch 1997: 342).
Others also began to note the emergence of an authoritarian regime, increasingly constraining the development and expansion of civil society, which cannot develop or last without the protection afforded by democratic structures. Soon, analysts began to conclude that the emerging government is taking the one-party state form, yet functioning as a neo-patrimonial bureaucratic regime with monopoly of political power (Hilal 1998a, b). These internal strains, increasing over time, converged with Palestinian perceptions that the Oslo agreements are unjust and detrimental to the national interests, as the agreement did not satisfy the legitimate demands of an occupied people for independent statehood, nor did it inhibit the continuing Israeli colonialist expansion in Palestinian areas, undermining even the meagre possibilities of creating peace. The Palestinian Authority came to be perceived as incapable of transforming itself into a democracy as long as it remained confined to the Oslo framework. The relationship between the population and the PA thus became increasingly conflict-ridden (Giacaman 1998).
In a critical expose of the workings of the PA, Palestinian Legislative Council (PLC) Member Azmi Shu’aybi revealed facts and processes that could only undermine most attempts at health sector reform (Shu’aybi and Shikaki 2000: 90). He raises questions that are important for the present argument, namely, the relationship between political processes and the absence of genuine reform. For instance, he notes that the civil service, which numbered around 20 000 when taken over by the PA from the Israeli military government, was inflated to 70 000–75 000 in a period of only 5 years. According to Shu’aybi, salaries in this sector account for 60 to 70% of public expenditure, resulting from unnecessary appointments in compensation for revolutionary heroism, current political support or both, and constituting a major drain on the national budget. He notes that the cabinet hardly ever meets, leading to an absence of collective decision-making, integrated planning and the adoption of general policy lines. Thus, he claims, the Planning Minister formulates the PA development plan, but other ministers, as a result of this solo performance, become unwilling to work in accordance with this plan that they did not help formulate. Overall, the picture that he paints is not only chaotic, but also tragic in terms of the absence of potential for reform.
In the health sector, the ramifications of such a system of rule can be far-reaching, as the need to coordinate at the intersectoral level with other ministries, such as education, housing, environment, agriculture and food supplies is paramount. In addition, the limitations of the Oslo accords for a public health approach are evident, in particular the virtual absence of control by the PA over water, land, the environment and the movement of people and goods (Sayigh and Shikaki 1999: 25), Israel having maintained its control in these areas. While one can argue that some reform projects can still succeed in the context of this particular policy environment, the fact remains that such attempts are likely to be limited to the domain of medical care and not to public health care. For example, water projects became a high priority for donor countries, as the amounts of water available to the Palestinian population do not meet the UN standards for the minimum requirement per capita, while ‘per capita supplies to Israeli settlers in the West Bank and Gaza are roughly four times higher than the amount supplied to the Palestinian population’ (World Bank and UNSCO 1999: 17). However, many of these projects aimed at expanding the water supply have been delayed or abandoned due to the difficulty of receiving permits from the Israeli government for their implementation.
The limited capacity of Palestinian health institutions to implement reforms
To its credit, the health system in the post-Oslo period has registered many achievements despite the occupation’s legacy of neglect and underdevelopment. However, despite those accomplishments in the government sector, the rapid increase in MoH employees from 2000 to 7000 persons (Sayigh and Shikaki 1999: 93) and numerous training courses, it is not evident that the quality of care has improved, even prior to the destruction attendant upon the Intifada that began in September 2000. This may be partially attributed to the difficulty in strengthening weak institutions in times of instability, where crisis management has become the routine. Institution building, based on an inexperienced administration that is externally financed by multiple donors in a context of rapid political and economic change, is complex and frustrating. Israeli control over many aspects of development in OPT adds to the complexity of the process. The limited regulatory role of the Ministry of Health as well as the Palestinian people’s growing disillusionment with the lack of transparency, accountability and participatory approach of the PA in general (Government of Japan and World Bank 2000: xvii) have affected public institutions. The government sector with its low pay scale, aggravated by the depreciation of the Israeli currency, has made it difficult to attract the most qualified health providers and technicians (Sayigh and Shikaki 1999: 96), and many public sector physicians supplement their salaries with a private practice. Political pressures have influenced how human resources are utilized in the health sector, not always in the most rational or effective manner. Thus physicians are carrying out some tasks that might be better accomplished by other types of health providers, creating concerns of sustainability for the health system, in addition to the acceptability of services, as in the case of women who prefer health care from female providers while the large majority of physicians are male. The issue of the effectiveness of extensive training courses offered to certain health providers has also been raised, where the criteria for selection of participants, the training methods utilized (primarily in the classroom rather than on-the-job), and the supervision and follow-up in the field require further consideration.
Donor policies and practices
Overall donor aid for the Palestinians has been described as ‘one of the largest ever undertaken by the international community, in both absolute and per capita terms’ (Sayigh and Shikaki 1999: 28), amounting to US$175 per person (World Bank Group 2001: 1). Of total donor aid, 8% was allocated to the health sector, nearly half of this financial support coming from Japan (33%) and Spain (15%) (World Bank and UNSCO 1999: 26–7). According to the World Bank, one of the numerous challenges facing development in the OPT is the involvement of ‘more than forty donors, over two dozen multilateral organizations and UN agencies, and hundreds of local and international NGOs in the development effort’ (Government of Japan and World Bank 2000: ix). In many cases, external assistance has mobilized excessive human resources and created more fragmentation than cooperation. The efforts of many professional cadres in the health sector are often directed towards acquiring and maintaining donor funds, keeping them out of their fields of practice, where they are most needed to maintain continuity in the implementation of projects. In some cases, donor preferences for funding rather than the actual needs determined in a perspective of sustainable development have defined the very nature of the projects themselves. Technical assistance, amounting to 23% of donor disbursement to the health sector (World Bank and UNSCO 1999: 28), is frequently linked to assistance from donor nationals, who often have limited time in the field and are not familiar with the culture or the language. Palestinian Authority officials and Palestinian researchers report, respectively, that 70 and 90% of technical assistance funds are spent on donor personnel or in donor countries, totalling almost one-fifth of all donor aid (amounting to over US$450 million between 1993–99) (Government of Japan and World Bank 2000: 107). Monitoring and reporting procedures vary with each donor, creating excessive paper work in a context of limited resources.
Donor approaches, procedures and mechanisms lack flexibility and are often not adapted to the reality on the ground. For example, the issue of the high Palestinian fertility rate was addressed by a donor-supported move to increase access to family planning services. Statistics show that lack of knowledge and cost are not prohibitive factors (Palestinian Central Bureau of Statistics 1998b: 90). The approach, in itself, was limited, given that the determinants of high fertility are far more complex than the mere availability of modern contraception,5 and because other means of dealing with the social and economic injustice inherent in the problem were not debated. Furthermore, the project design of broadening the content and range of maternal health services by integrating family planning into the existing services at the primary health care clinics did not pay sufficient consideration to the time and effort needed to improve the quality of care in weak and overburdened institutions. Time limits and the frequent donor requirements of rapidly measurable results lead to the illusion of ‘quick fixes’, whereas the implementation of sustainable health projects focused on quality are arduous tasks often involving structural and behavioural changes, and requiring repetition, supervision and on-going support.
The limited political analysis on the part of the donors in relation to the major obstacles to health and well-being, and their proven incapacity to influence change in the political arena as a prerequisite to reforming the health system, have often resulted in the non-sustainability and ineffectiveness of projects. In contrast to this tunnel-vision approach to the health of the population that limits its scope to increased physical access, service efficiency and technical and managerial improvements, the Palestinian experience highlights the importance of a primary and public health approach to health and health care delivery. Preventing illness and promoting health is a challenge that goes far beyond the provision of services, and a health-sustaining environment is an essential component (McMichael and Beaglehole 2000). In the case at hand, it appears that ideas for change in the health sector focused exclusively on the physical access to health services, rather than on the promotion of a healthy environment. The fact of the matter is, however, that the two are inextricably linked, and that the former, if deprived of the latter, cannot be effective.
The policy vacuum
The OPT still lacks a general development policy, and within the context of this vacuum the World Bank is of growing influence, especially in economic projects, but also in health and other social sectors. Its policy is directed towards a free-market economy, emphasizing the private sector (which is minimally regulated) within the framework of structural adjustment (Hilal 1998b: 124). But the OPT as a nation has neither agreed to structural adjustment as the way forward, nor to the economy being directed towards the free market, although in the longer term, it has been argued, this may indeed be the path to Palestinian development, a position that is rather clearly stated in the Palestinian Development Plan. On the other hand, it has also been argued that ‘the philosophy of economic liberalization advocated by international organizations, the United States and the European Union, given the de-developed condition of the Palestinian economy inherited by the PA after three decades of Israeli occupation, could only widen socio-economic and class inequalities’ (Hilal 1998b: 124). This could undermine the equity principle that is so important for reform to which international aid usually pays lip service while proceeding instead in the direction of economic efficiency and cost-effectiveness.
In its Medium Term Development Strategy for the Health Sector, the World Bank emphasizes that, in cooperation with the PA’s Ministry of Health, it will assess the health sector in terms of the efficiency and the quality of its service, the sustainability of present financial arrangements and equity and accessibility to services (World Bank 1998: 1). The intentions expressed are admirable. However, the document then proceeds to delineate the path to reform in almost entirely economic terms, where access and equity appear to be conflated, and where access is elaborated in terms of ‘affordability of premiums’, ‘ability to pay’ and focusing on physical/distance access. Other definitions, including equity in quality and social access, were not given due consideration, even when acknowledging political and economic trends such as high unemployment, declining wages and the existence of a large informal sector.
Moreover, the World Bank also realizes that to achieve its objectives in the health sector, changes in the nature and processes of decision making and budgetary allocations are crucial for efficiency and cost-effectiveness (particularly in relation to the appointment system with its implications for the health budget, the necessity for decentralization in the decision making and managerial structures, and in budgetary allocation and transparency). Yet, as the World Bank also notes, aid ‘is a fundamentally political process’, and in the Palestinian case, the primary function of international aid is to sell the fragile and flawed peace process to the Palestinian people, by showing tangible results in their daily lives. Its apparent lack of consideration for long-term development needs and sustainability seem to contradict its very discourse. Indeed, the World Bank recognizes the challenge that long-term development and peace building efforts (the need to show rapid tangible results) may not always be compatible. Time has shown that it is difficult to sell a basically unjust peace process with aid money, not only because the ‘peace dividends’ have never materialized, but also because freedom is still an issue for people who are struggling for self-determination. Serious attempts at health sector reform require a just resolution to the Palestinian-Israeli conflict that the population, and not only the PA, is willing to accept.
If one then links these considerations to the increasingly diminishing space for public discourse, the retreat of mass organizations and the threat against civil society institutions posed by the emerging regime, one can begin to see more clearly what is possible and what is not possible to achieve without reforming the political system itself first, instead of simply working to implement HSR projects imported from the outside.
Conclusion
Health sector reform processes in the developing world have been known to neglect crucial issues and be led by ‘naïve’ assumptions (Thomason 1997). In the case of the OPT, an unjust framework for peace resulting in ongoing conflict is a main impediment to reform, transforming it into relief and interrupting the build-up and consolidation of reform initiatives. The events beginning on 29 March 2002, leading to re-occupation of major towns and many villages, and the resulting destruction of most PA and NGO structures, as well as the collapse of the private sector and the economy, can only emphasize how faulty these assumptions have been. However, even in post-conflict situations, health development is ‘contingent upon overcoming major structural obstacles in these unstable and resource poor environments’ (Macrae et al. 1995: ix). In this situation, donors appear to operate in a manner similar to that in other ‘post-conflict’ areas, seeking unsustainable quick impact solutions to health system problems that took years to generate in a context heavily burdened with under-development. They operate in the absence of a comprehensive policy forum, neglecting policy dialogue, and focusing on plans derived from donor strategies instead. Although donor reports often mention the importance of Palestinian ownership of the development process, the reality is different. A World Bank report discussing who should take the lead in the aid coordination process in this country states ‘with so many vested historical, national, economic, commercial and political interests in this very high-profile hotspot, it is unrealistic to expect that donors will eventually cede the lead role solely to the Palestinians’ (Balaj and Wallich 1999: 3). At the local level, even the actual processes of consultation in relation to proposed plans are flawed, appearing to some to be more rhetoric than substance, precisely because of the defective nature of the community participation processes. This appearance of participation either takes the shape of ‘quick and dirty’ rapid appraisals that often miss out on the needs of the most vulnerable groups, such as women and children, or of ‘wish list’ workshops directed usually towards the same constituency, senior managers, some university personnel and a few NGOs, to legitimize continuing with the policies and strategies pre-determined by donors.
As is the case in other developing countries, the swiftness of development planning in OPT to suit donor agendas and budgetary deadlines ‘constitutes a major threat to appropriate policy development’ (Macrae et al. 1995: xi). The political motive of selling the peace process has only exacerbated the situation. With planning taking place at an inappropriate speed in relation to the requirements of the context, it becomes difficult, if not impossible, to address adequately the serious structural and systemic problems that come in the way of turning plans into successful realities. Increasing centralization, the absence of transparency, the weakening of civil society and the consequent diminishing space for demand-shaped reform and advocacy and the weak regulatory role of government, all work together to produce frustrating results. Frustrating because what we are witnessing is an emerging crisis in government policy, in public credibility, and in health financing, exacerbated by ill-conceived notions of sustainability in a non-sustainable environment dictated by war, instability and dependence. It is unrealistic to think that a real partnership can exist in the inherently unequal relationship of donor and beneficiary. Nevertheless, it is imperative to be aware of the specific agendas and the limitations of donor aid, to determine the priorities for health sector reform within a contextual analysis, and to promote public debate at all levels of the society. The Palestinians need a clear vision and comprehensive health policy, based on a conception that includes a health-promoting environment, and formulated in genuine consultation with the population. Such an approach might lead to a more sustainable process of health sector reform, including real negotiations with the donors on the priorities and the terms of international assistance.
In the face of all these considerations, the economic focus on reform, with its emphasis on managerial restructuring and cost containment in the health field, is potentially dangerous, as it distracts attention from the principal issues that need to be addressed in reform, and is not responsive to the population’s needs. After all, it is not efficiency or the reform process per se that is needed, but the construction of a health system that will promote the social right to health development for Palestinian citizens including the factors of quality and of equity.
Footnotes
Biographies
Rita Giacaman is Director of the Department of International Community Health at the Institute of Community and Public Health, Birzeit University, Occupied Palestinian Territories.
Hanan F Abdul-Rahim and Laura Wick are researchers at the Institute of Community and Public Health, Birzeit University, Occupied Palestinian Territories.
For details on the history of the Arab-Israeli conflict, which is beyond the scope of this paper, see the ‘Question of Palestine’ on the official UN site at [http://www.un.org/Depts/dpa/qpal/index. html]. This comprehensive site includes an historical overview of the conflict, as well as relevant maps, UN documents, resolutions, and other useful information.
Due to the decrease in NGO primary health care clinics during this same period, the overall number of clinics, particularly in the West Bank, has not changed significantly (Government of Japan and the World Bank 2000: 43).
For an interesting analysis of issues pertaining to international assistance to countries in transition from war to relative peace see Macrae et al. (1995).
For an analysis of this question, see Giacaman (1997) and Fargues (2000).
References
- Balaj B, Wallich C. 1999. Aid coordination and post-conflict reconstruction: the West Bank and Gaza Experience. Precis. Washington, DC: World Bank Operations Evaluation Department.
- Barghouthi M, Lennock J. 1997. Health in OPT: Potential and challenges. Ramallah: OPT Economic Policy Research Institute (MAS).
- Barghouthi M, Giacaman R. 1990. The emergence of an infrastructure of resistance: the case of health. In: Nassar J, Heacock R (eds). Intifada, OPT at the Crossroads. NY: Praeger, pp. 73–87.
- Berman P (ed). 1995. Health sector reform in developing countries: making health development sustainable. Boston: Harvard University Press.
- Economic Policy Research Institute (MAS). 2000. Social Monitor 3, p. 13.
- Fargues P. Protracted national conflict and fertility change: Palestinians and Israelis in the twentieth century. Population and Development Review. 2000;26:463–9. doi: 10.1111/j.1728-4457.2000.00441.x. [DOI] [PubMed] [Google Scholar]
- Frisch H. Modern absolutist or neopatriarchal state building? Customary law, extended families, and the Palestinian Authority. International Journal of Middle East Studies. 1997;9:342. [Google Scholar]
- Giacaman R. 1994. Health conditions and services in the West Bank and Gaza Strip United Nations Conference on Trade and Development. UNCTAD/ECDC/SEU/3.
- Giacaman R. 1997. Population and fertility, Palestinian women: a status report. Birzeit, OPT: Women’s Studies Program, Birzeit University.
- Giacaman G. 1998. In the throes of Oslo: Palestinian society, civil society, and the future. In: Giacaman G, Lonning D (eds). After Oslo: new realities, old problems. London: Pluto Press, pp. 1–51.
- Giacaman G, Lonning D (eds). 1998. After Oslo: new realities, old problems. London: Pluto Press.
- Government of Japan and the World Bank. 2000. Aid effectiveness in the West Bank and Gaza. Jerusalem: The Secretariat of the Ad Hoc Liaison Committee.
- Hilal J. 1998a. The Palestinian political system after Oslo: a critical analytical study. Ramallah, OPT: Muwatin, The Palestinian Institute for the Study of Democracy (in Arabic).
- Hilal J. 1998b. The effects of the Oslo Agreement on the Palestinian political system. In: Giacaman G, Lonning D (eds). After Oslo: new realities, old problems. London: Pluto Press, pp. 121–45.
- Khawaja M. The recent rise in Palestinian fertility: permanent or transient? Population Studies. 2000;54:331. doi: 10.1080/713779091. [DOI] [PubMed] [Google Scholar]
- Macrae J, Zwi A, Birungi H, 1995, A healthy peace? Rehabilitation and development of the health sector in a post-conflict situation. London: Department of Public Health and Policy, London School of Hygiene and Tropical Medicine.
- McMichael A, Beaglehole R. The changing global context of public health. The Lancet. 2000;356:495–9. doi: 10.1016/s0140-6736(00)02564-2. [DOI] [PubMed] [Google Scholar]
- Palestinian Central Bureau of Statistics. Demographic statistics: main indicators. Accessed online at [ http://www.pcbs.org] Updated September. 1998a;13:1998. [Google Scholar]
- Palestinian Central Bureau of Statistics. 1998b. Women and men in OPT: trends and statistics. Ramallah: PCBS.
- Palestinian Central Bureau of Statistics. 1999. Population, Housing and Establishment Census-1997, Final Results – Population Report – Palestinian Territory First Part. Ramallah, OPT: PCBS.
- Policy Research Incorporated. 1999. Social impact assessment, West Bank and Gaza Strip Bethesda, Maryland: Health System Development Project.
- Sanbar E. 1984. OPT 1948, L’Expulsion. Washington DC: Les Livres de la Revue d’Etudes Palestiniennes.
- Sayigh Y, Shikaki K. 1999. Strengthening Palestinian public institutions New York: The Council on Foreign Relations.
- Sen K, Koivusal M. Health care reform and developing countries: a critical overview. International Journal of Health Planning and Management. 1998;13:199–215. doi: 10.1002/(SICI)1099-1751(1998070)13:3<199::AID-HPM518>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Shu’aybi A, Shikaki K. A window on the workings of the PA: an inside view. IPS Forum. Journal of OPT Studies. 2000;XXX:90. [Google Scholar]
- Standing H. 1999. Framework for understanding gender inequalities and health sector reform: an analysis and review of policy issues. Brighton: Institute of Development Studies.
- Thomason J. 1997. Health sector reform in developing countries: a reality check. [http://www.acithn.uq.edu.au/conf97/papers97/thomason.htm], Plenary paper from Australian Tropical Health and Nutrition Conference, 17–19 July 1997, pp. 6–78.
- World Bank. 1998. West Bank and Gaza: Medium-term development strategy for the health sector. Washington DC: The World Bank.
- World Bank. 2002. Fifteen Months, Intifada, Closures and Palestinian Economic Crisis. An Assessment. March. Washington DC: World Bank.
- World Bank Group. 2001. One Year of Intifada. West Bank and Gaza Update, November. Washington DC.
- World Bank and United Nations Office of the Special Coordinator in the Occupied Territories (UNSCO). 1999. Donor investment in Palestinian development 1994–1998. Jerusalem: World Bank and UNSCO.


