Abstract
RNA viruses are notorious for their genetic plasticity and propensity to exploit new host-range opportunities, which can lead to the emergence of human disease epidemics such as severe acute respiratory syndrome, AIDS, dengue, and influenza. However, the mechanisms of host-range change involved in most of these viral emergences, particularly the genetic mechanisms of adaptation to new hosts, remain poorly understood. We studied the emergence of Venezuelan equine encephalitis virus (VEEV), an alphavirus pathogen of people and equines that has had severe health and economic effects in the Americas since the early 20th century. Between epidemics, VEE disappears for periods up to decades, and the viral source of outbreaks has remained enigmatic. Combined with phylogenetic analyses to predict mutations associated with a 1992–1993 epidemic, we used reverse genetic studies to identify an envelope glycoprotein gene mutation that mediated emergence. This mutation allowed an enzootic, equine-avirulent VEEV strain, which circulates among rodents in nearby forests to adapt for equine amplification. RNA viruses including alphaviruses exhibit high mutation frequencies. Therefore, ecological and epidemiological factors probably constrain the frequency of VEE epidemics more than the generation, via mutation, of amplification-competent (high equine viremia) virus strains. These results underscore the ability of RNA viruses to alter their host range, virulence, and epidemic potential via minor genetic changes. VEE also demonstrates the unpredictable risks to human health of anthropogenic changes such as the introduction of equines and humans into habitats that harbor zoonotic RNA viruses.
Keywords: alphavirus, arbovirus, equine, evolution
Many emerging infectious diseases such as severe acute respiratory syndrome (1, 2), hantavirus pulmonary syndrome (3), and Ebola (4) are caused by zoonotic RNA viruses that normally infect wild animals but occasionally infect humans. Other RNA viruses have been transferred more permanently across host species to use humans as their reservoir and/or amplification hosts, resulting in widespread diseases like AIDS (5), influenza (6), and dengue (7, 8). Their genetic plasticity and ability to adapt quickly to new host opportunities facilitate emergence of these RNA viruses (9, 10). However, the mechanisms of host-range change remain poorly understood.
Most arthropod-borne viruses (arboviruses) such as West Nile virus infect people via incidental “spillover,” when mosquitoes that bite reservoir hosts occasionally refeed on humans. However, a few arboviruses exploit domestic animals as secondary amplification hosts to increase spillover (11). Venezuelan equine encephalitis virus (VEEV; Togaviridae; Alphavirus) causes severe, sometimes fatal, disease in people and equines (horses, mules, and donkeys) during explosive epidemics that have affected hundreds of thousands of people in the Americas for nearly a century (12). The last major outbreak in 1995 affected northern Venezuela and Colombia, infecting an estimated 70,000–100,000 humans and an unknown but probably similar number of equines (13). Other outbreaks have been even more widespread, affecting Central America, Mexico, and Texas from 1969–1971 (14).
The VEEV contains a single-stranded RNA genome, ≈11,400 nt in length, with positive or messenger sense polarity (15). Entry of alphaviruses into cells involves interactions of the E2 envelope glycoprotein with cellular receptors that remain poorly characterized. The VEEV apparently uses the high-affinity laminin receptor (16), and recent studies indicate that C-type lectins such as DC-SIGN and L-SIGN can function as receptors for alphavirus infection of dendritic cells (17). Artificial passages also adapt VEEV to bind to heparan sulfate on the surface of vertebrate cells (18). However, the use of highly conserved and widely distributed receptors cannot explain the specificity of many VEEV-host interactions, suggesting the use of a coreceptor or some other processing step. After disassembly of the virion after acidification and fusion with the endosomal membrane, the genome is translated to produce the nonstructural proteins, which participate in genome replication and polyprotein processing (19–21). The structural genes, which encode the capsid as well as the E1 and E2 envelope glycoproteins, are translated from a subgenomic message. Virion maturation occurs when nucleocapsids form in the cytoplasm from 240 copies of the capsid protein and a genomic RNA molecule and interact with E2/E1 heterodimers embedded in the plasma membrane to initiate budding. The mature virion contains spikes on its surface that are primarily composed of the E2 protein.
The equine-virulent VEEV strains in serotypes IAB and IC, which are responsible for major outbreaks, are transmitted by mosquitoes that become infected after biting a viremic equine (22). People who live in agricultural settings become infected via spillover; thus, the ability to amplify efficiently in equines by generating high viremia levels leads to large numbers of human infections. Because equines have relatively long life spans, epidemics are self-limited due to both immunity in survivors and to mortality. Although an effective VEEV vaccine strain, TC-83, protects equines against disease and eliminates their role in amplification, vaccination programs usually wane several years after an outbreak. Therefore, epidemics have historically occurred every 10–20 years, when population turnover lowers herd immunity and vaccination efforts decrease.
The viral source required to reinitiate epidemic VEEV circulation has remained enigmatic for nearly a century. Some outbreaks between 1938 and 1973 were probably caused by the use of incompletely inactivated vaccines (23, 24). One hypothesis for the origins of all serotype IAB and IC epidemic strains involves enzootic strains, which circulate among rodents in forest or swamp habitats, are avirulent for equines, and are incapable of generating sufficient equine viremia for amplification. These strains could mutate to alter their serotype and to acquire amplification potential via induction of high-titer equine viremia (25). Evidence supporting this hypothesis first came from antigenic and RNA fingerprinting studies (26, 27). Later, phylogenetic studies using VEEV sequences suggested that the IAB and IC epidemic serotypes evolved convergently from an enzootic ID lineage (28).
As a further test of the hypothesis of an enzootic origin for epidemic strains, we extended phylogenetic studies to examine relationships among strains and serotypes in the VEE complex of alphaviruses. To identify mutations with the potential to transform the enzootic, equine-amplification-incompetent phenotype to the epidemic phenotype, we used reverse genetics to place phylogenetically predicted mutations into the genome of an enzootic strain closely related to the predicted progenitor of a 1992–1993 VEE outbreak. A single mutation, encoding a Thr-to-Lys change at amino acid position 213 of the E2 protein, generated high-titer equine viremia, as well as the IC epidemic serotype.
Results
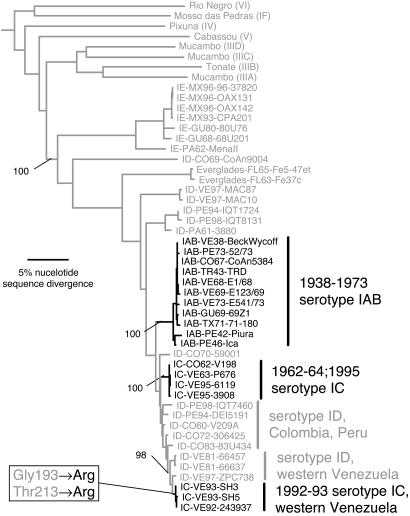
To extend previous phylogenetic studies designed to determine relationships among enzootic and epidemic VEEV strains, we sequenced the pE2 envelope glycoprotein precursor gene (1,677 nt including a portion of the E3 and 6K protein genes) for VEEV strains and related VEE complex alphaviruses. Phylogenetic trees constructed by using maximum parsimony, neighbor joining, and Bayesian methods all placed the enzootic variants in basal positions with the epidemic IAB and IC strains within three distal or derived groups (Fig. 1): (i) the IAB strains that probably emerged in the 1920s and reemerged later from incompletely inactivated vaccines (23); (ii) the IC serotype that emerged in 1962 and reemerged in 1995; and (iii) a third IC clade that emerged in western Venezuela in 1992 (29). The genetic (<0.7% nucleotide, ≤0.4% amino acid sequence divergence) and geographic relatedness of isolates from the 1992–1993 outbreak to sympatric, enzootic ID isolates from western Venezuela supported its local emergence (Fig. 1).
Fig. 1.
Phylogenetic tree of representatives of all VEE complex alphaviruses and all serotypes of VEEV generated by using the neighbor-joining program implemented in paup* 4.0 software. Homologous sequences of eastern equine encephalitis virus, the sister to the VEE complex, were used as an outgroup. Bayesian and maximum parsimony analyses produced trees with identical topologies except for the order of divergence of Pixuna and Cabassou viruses. Virus strains are designated by virus name (subtype in the VEE complex in parentheses) or VEEV serotype, followed by abbreviated country and year of isolation and strain name. Enzootic strains isolated from mosquitoes, humans, or sentinel animals infected in sylvatic habitats are gray; epidemic strains isolated from mosquitoes, humans, or horses during major VEE epidemics are black. Numbers indicate neighbor-joining bootstrap values for groups to the right. Branches are colored to minimize phenotypic changes, and transitions from gray to black indicate hypothetical phenotypic changes from enzootic to epidemic leading to VEE outbreaks. Maximum parsimony analyses were used to assign each amino acid substitution to each branch in the tree, and the box shows the two substitutions in the E2 envelope glycoprotein represented in the branch with the predicted enzootic-to-epidemic transition in 1992.
Serotype ID strain ZPC738, the closest relative to the 1992–1993 epidemic isolates (Fig. 1), is equine avirulent, whereas two isolates from the outbreak cause encephalitis and high-titer viremia (30). Identification of closely related enzootic and epidemic VEEV strains with typical equine virulence and amplification phenotypes allowed us to use reverse genetics to reproduce the hypothetical emergence of the 1992–1993 epidemic. Compared to epidemic serotype IC strain SH3, there are 15 deduced amino acid differences in the viral proteins (Table 1). Two differences were in the E2 envelope protein, a component of the viral spikes (31) and indicated by studies using chimeric enzootic/epidemic VEEV strains as the major determinant of equine virulence and amplification potential (32). Both amino acid differences were predicted by phylogenetic analyses (Fig. 1) to be associated with the 1992 epidemic emergence and to reflect replacement of uncharged, ancestral residues (Gly-193 and Thr-213) by Arg residues. Because these Arg substitutions both lie within an immunodominant region (33), we also suspected their involvement in the serotype change from ID to IC (Fig. 1). Residue 213 was identified as having responded to positive selection (34), possibly reflecting adaptation for equine replication. Furthermore, both E2 mutations involved replacements of uncharged (Gly-193 and Thr-213) amino acids by Arg residues, and E2-positive charge mutations have accompanied all epidemic emergences (34). We, therefore, hypothesized that one or both E2 mutations were responsible for the 1992 epidemic.
Table 1.
Deduced amino acid differences between enzootic subtype ID strain ZPC738 and epidemic subtype IC strain SH3
| Protein | Amino acid position* | ZPC738 | SH3 |
|---|---|---|---|
| nsP1 | 106 | Gly | Glu |
| 176 | Asn | Asp | |
| 528* | Leu | Phe | |
| nsP3 | 212* | His | Tyr |
| 360* | Thr | Met | |
| 461 | Leu | Pro | |
| 481 | Gly | Arg | |
| nsP4 | 2 | Ile | Thr |
| 176 | Ala | Ser | |
| Capsid | 76* | Gly | Arg |
| 86 | Pro | Gln | |
| E2 | 193* | Gly | Arg |
| 213* | Thr | Arg | |
| E1 | 384 | Lys | Arg |
| 416 | Arg | Gly |
*Amino acid changes located in the branch representing the 1992 VEE emergence, as described in the legend to Fig. 1.
To test this hypothesis, we used an infectious cDNA clone derived from enzootic ID strain ZPC738, predicted to be almost identical in sequence to the ancestor of the 1992–1993 IC strains (Fig. 1). This clone produces VEEV that is phenotypically indistinguishable from its parent virus (35). We used site-directed mutagenesis to introduce both Arg residues (E2 positions 193 and 213) individually or in combination into the enzootic genome. Viruses rescued from the mutated clones replicated at comparable levels in mosquito and vertebrate cell cultures and exhibited murine virulence comparable with that of the parent virus (data not shown).
To test the hypothesis that one or both Arg mutations mediated the ID→IC antigenic change, we used mAbs (36) to serotype the mutants; enzootic (ID, IE)-specific mAb 1A1B-9 reacted against strain ZPC738 as expected, whereas epidemic (IAB, IC)-specific mAb 1A3A-5 reacted with the 1992–1993 epidemic strains as shown in ref. 29. The Gly-193→Arg mutation alone had no effect on mAb reactivity (Table 2). The Thr-213→Arg substitution altered the antigenicity from enzootic (mAb 1A1B-9-reactive) to epidemic (1A3A-5-reactive), and the combination of both Arg substitutions also produced the epidemic phenotype. These results demonstrated that Arg-213 substitution transforms the enzootic ID serotype to epidemic IC.
Table 2.
Plaque sizes and reactivity of parent and mutant strains of Venezuelan equine encephalitis virus with serotype-specific monoclonal antibodies
| Virus strain | Plaque size, mm |
Monoclonal antibody number (serotype specificity) |
|||
|---|---|---|---|---|---|
| Mean | SD | 1A4D-1 (all VEEV) | 1A1B-9(enzootic, serotype ID/IE) | 1A3A-5(epidemic, serotype IAB/IC) | |
| ZPC738 | 4.05* | 0.39 | Positive | Positive | Negative |
| ZPC738/R193 | 3.60* | 0.33 | Positive | Positive | Negative |
| ZPC738/R213 | 3.81* | 0.33 | Positive | Negative | Positive |
| ZPC738/R193/R213 | 1.94† | 0.26 | Positive | Negative | Positive |
| SH3 | 1.74† | 0.29 | Positive | Negative | Positive |
Reactivity with a 1:400 dilution of each antibody as described by Roehrig et al. (36).
*Significantly different mean plaque size (ANOVA; P < 0.05) from epidemic, serotype IC strain SH3.
†Significantly different mean plaque size (ANOVA; P < 0.05) from enzootic, serotype ID strain ZPC738.
To determine whether either Arg substitution affects equine virulence and viremia, hallmarks of epidemic strains, we began by testing plaque sizes, markers of these phenotypes (37, 38). Epidemic IAB and IC strains produce small plaques on Vero cells, whereas enzootic strains including serotype ID produce larger plaques (30, 37). Virus from the ZPC738 clone produced large plaques (mean diameter, 4.05 mm; see Table 3, which is published as supporting information on the PNAS web site), as reported in ref. 38. The individual Arg substitutions had little or no effect on plaque size, whereas the combination of both mutations transformed the large enzootic plaque phenotype to the small-size characteristic of epidemic strains (Table 3).
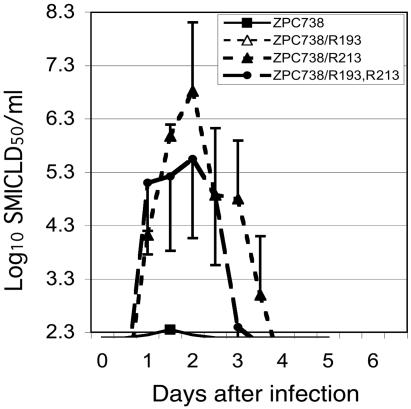
No small animal VEE models have been identified that predict equine virulence and viremia phenotypes, and the parent enzootic ID and epidemic IC strains we used all produce fatal encephalitis in 100% of mice infected s.c. (30). Therefore, to determine whether Arg mutations can generate a VEEV strain capable of epidemic amplification, we infected horses with the mutants. Studies have shown that the ZPC738 parent strain is avirulent for horses, producing little or no viremia, whereas IC strains 243937 and SH3 from the 1992–1993 epidemic are virulent and generate high viremia titers (30). Virus from the ZPC738 clone had a low viremia phenotype consistent with its parent strain [viremia was detected in one of four horses (Fig. 2)]. Virus with the Arg-193 substitution failed to produce detectable viremia in any of the four horses infected, and no apparent disease was seen. In contrast, the Arg-213 had a dramatic effect on both virulence and viremia, producing neurologic disease and significantly (P < 0.001) increasing the mean peak viremia titer to a level comparable with that of the epidemic strains SH3 and 243937 (30). The combination of both Arg mutations also generated a virulent VEEV strain with significantly higher peak viremia than that of the enzootic strain (P < 0.001) and consistent with the epidemic, equine amplification-competent phenotype. Compared with the single Arg-213 mutant, the double-Arg mutant produced slightly higher viremia 24 h after infection but lower viremia 36–48 h after infection; these differences were not significant (P > 0.05). A possible minor effect on early viremia of the Arg-193 mutation, suggested by its requirement for the small, epizootic plaque phenotype, deserves further study.
Fig. 2.
Mean viremia titers expressed in suckling mouse intracranial lethal dose 50% units for four horses infected s.c. with 2,000 plaque-forming units of VEEV rescued from the enzootic infectious clone (ZPC738), as well four horses infected with mutants with Arg residues at E2 positions 193 and 213, and five horses infected with a double-mutant containing both Arg residues. Bars indicate SEM.
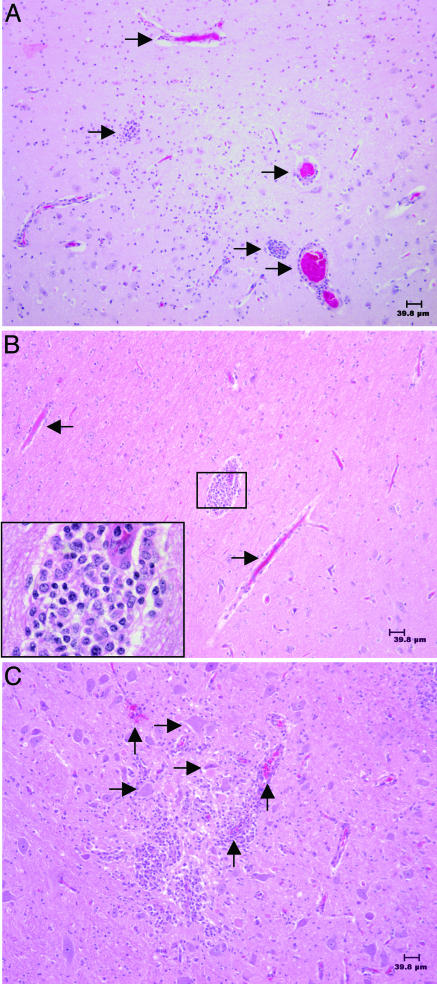
The virulent phenotype observed in all horses inoculated with ZPC738/R213 or ZPC738/R193/R213 viruses consisted of high biphasic fever beginning 1–2 days postinoculation, followed by a decrease in feed consumption, depression, reluctance to move, and neurological signs such as ataxia or stumbling. Horses with severe disease had a nonsuppurative meningoencephalitis typical of VEE, characterized by widespread perivascular infiltration of mononuclear cells, formation of glial nodules, neuronal cell death, and microhemorrhages throughout the brain (Fig. 3).
Fig. 3.
Histopathological analyses of brain samples from animals infected with VEEV strains, as described in Materials and Methods, showing representative lesions. (A) Strain ZPC738 containing the Arg residue at E2 position 193, day 7 postinfection. Congestion and vascular and perivascular (Virchow–Robin space) infiltration by mononuclear cells (arrows) in the brainstem. (B) Strain ZPC738 containing the Arg residue at E2 position 213, day 7 postinfection. Congestion and vascular and perivascular (Virchow–Robin space) infiltration by mononuclear cells (arrows) in the brainstem; Inset shows higher magnification of an area of extensive infiltration. (C) Strain ZPC738 containing the Arg residues at E2 positions 193 and 213, day 7 postinfection. Congestion and vascular and perivascular (Virchow–Robin space) infiltration by mononuclear cells (vertical arrows), as well as neuronal cell death characterized by angulation of hypereosinophilic neurons and microhemorrhage (horizontal arrows) in the brainstem.
Discussion
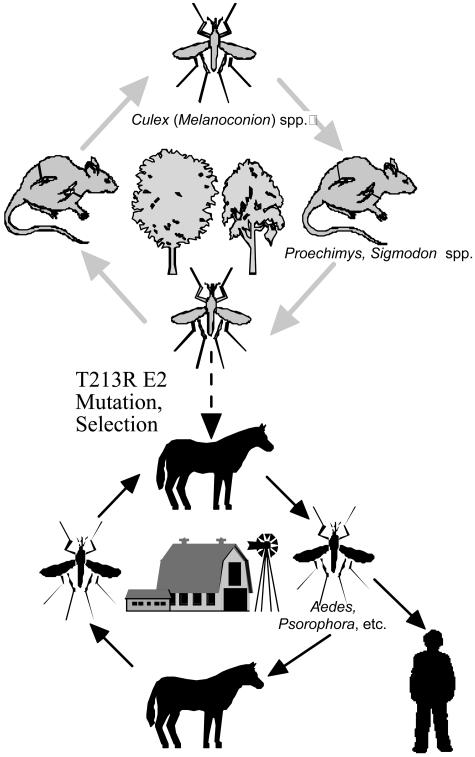
Our findings support the hypothesis that epidemic, serotype IC VEEV can arise via a single mutation in enzootic serotype ID strains that circulate in western Venezuela (Fig. 4). A Thr→Arg mutation at residue 213, in an immunodominant region of the E2 envelope glycoprotein, transformed the enzootic equine-avirulent, and amplification-incompetent phenotypes into the epidemic, virulent, and amplification-competent phenotype. This laboratory experiment recapitulated the evolutionary history of the serotype IC epidemic strains isolated during the 1992–1993 outbreak as deduced by using phylogenetics (Fig. 1). Determining the effects of this mutation on equine pathogenesis will require additional studies focusing on early steps in infection and replication. A possible role of the Gly-193→Arg mutation in the emergence process, either in enhancement of the early viremia or possibly as a compensatory mutation for the Arg-213 mutation, deserves further study. The lack of mutations of the residue at position 193 in other VEE emergence events depicted in Fig. 1 (in contrast to position 213, which changes during each epidemic emergence), along with the efficient viremia induction of the Arg-213 mutant alone, argue against a compensatory effect. However, the combination of two positive-charge E2 mutations in the other, major IAB and 1962/1995 IC emergences (34) suggests a role for the Arg-193 mutation in the 1992 outbreak.
Fig. 4.
Cartoon showing the emergence process for epidemic VEEV strains supported by this study. Enzootic, sylvatic VEEV strains in serotype ID (gray) are transmitted continuously among rodent reservoir hosts such as spiny rats (Proechimys spp.) and cotton rats (Sigmodon spp.) by mosquito vectors in the subgenus Culex (Melanoconion). Mutations in the E2 envelope glycoprotein, such as the Thr-213→Arg identified in this study, are selected by equines because they generate high-titer viremia sufficient for amplification. The resultant epidemic strains (black) in serotypes IAB and IC are transmitted by abundant floodwater mosquitoes such as Aedes and Psorophora spp., which have wide host ranges including equines and humans. Spillover to humans who live in proximity to infected equines results in epidemics involving up to hundreds of thousands of people before equine mortality and immunity exhaust the supply of amplification hosts or vector populations decline.
Our results have important implications for understanding VEE ecology and epidemiology. Most RNA viruses, including alphavirus populations, exhibit high mutant frequencies on the order of 10−4 mutants/nucleotide (39). Therefore, the Arg-213 mutant that is capable of initiating epidemic amplification might be produced whenever VEEV populations reach ≈104. Additional selective forces on the RNA genome sequence related to genomic or subgenomic RNA replication, secondary structure, and/or packaging could complicate the selection of such mutations in nature and should be studied further. A population size of 104 is exceeded in infected mosquitoes, which generally develop titers of ≈106 infectious units, including ≤104 in the saliva (40, 41) and in reservoir hosts such as spiny rats (42, 43) and cotton rats (42, 44), which develop peak viremia titers exceeding 104 infectious units/ml. This finding suggests that ecological factors including transport of nascent epidemic strains to locations conducive to equine amplification, as well as epidemiologic and ecologic factors including equine herd immunity and mosquito densities, constrain the frequency of VEE epidemics rather than the generation of amplification-competent mutants. Envelope glycoprotein mutations that facilitate transmission by Aedes (Ochlerotatus) taeniorhynchus, an important mosquito vector, could also be involved in some epidemics (45, 46). However, there is no evidence of enhanced vector infection by the 1992–1993 IC strains compared with the putative ID progenitors, such as strain ZPC738 (47).
Our findings suggest that VEE epidemics can arise wherever an appropriate E2 protein gene mutation occurs coincident with susceptible equine populations and abundant floodwater vectors such as Aedes and Psorophora spp. Constant vigilance, including equine vaccination and surveillance for epidemic emergence, are therefore needed, especially in Venezuela and Colombia where enzootic, strain ZPC738-like VEEV strains circulate continuously. Whether other enzootic VEEV strains or lineages in serotype ID, or even in serotypes IE or II (Everglades virus) can become epizootic, equine-amplification-competent via the same or similar mutations in the E2 protein is an important question that needs to be answered. The strain that we tested (ZPC738) represents one of six major VEEV lineages (Fig. 1) that has been isolated only in western Venezuela, Colombia, and northern Peru. Other lineages occur in various locations from coastal Ecuador to Florida (Everglades virus falls within the VEEV clade). The lack of association between these lineages and subtype IAB or IC emergences (Fig. 1) suggest that either: (i) genetic differences between these enzootic strains and the ID lineage we tested (represented by strain ZPC738) prevent the former from adapting easily for equine replication; or (ii) ecological differences in the regions where the other enzootic lineages circulate are less conducive to epizootic transmission. A history of VEE outbreaks in Central America, where serotype IE strains are found, as well as locations of South America and Panama where many of the other ID lineages occur, argue for the first hypothesis. Reverse genetic studies placing the T213R E2 mutation into cDNA clones derived from other enzootic lineages, a further test of this hypothesis, are needed.
Materials and Methods
Virus Strains.
Enzootic VEEV strain ZPC738 (ID), isolated from a sentinel hamster infected in a tropical lowland forest of Zulia State, Venezuela, in 1997 (38), was passaged once in BHK-21 cells to generate RNA for infectious cDNA cloning (35); epidemic strain SH3 (IC), isolated during the 1992–1993 western Venezuela epidemic (29), was passaged once in Vero monkey kidney cells and once in baby hamster kidney cells.
Plaque Assays.
Confluent Vero cells in six-well cell culture plates were infected with serial dilutions of VEEV and incubated for 1 h at 37°C; then 2 ml of MEM with 1.0% Noble agar was added to each well, and the cells were incubated at 37°C for 48 h. The cells were fixed with 10% formaldehyde for 30 min, then the agar plugs were removed, and the cells were stained with 20% methanol/0.25% crystal violet. The diameters of 20 plaques were measured for each strain; for irregularly shaped plaques, two measurements were made at right angles and averaged.
cDNA Clones.
The RNA isolation, RT-PCR, cloning, sequencing, and construction of the pM1-738 infectious cDNA clone from strain ZPC738 was described in ref. 35. Mutations to genome positions 9117 and 9178 were generated in a subcloned cDNA fragment 2,265 nt in length, flanked by restriction sites AflII (genome position 8031) and SnaBI (genome position 10296) by using the Stratagene QuikChange site-directed mutagenesis kit. The mutations were verified by sequencing and recloned back into the pM1-738 backbone.
Equine Infections.
Seventeen horses with undetectable levels of alphavirus-neutralizing antibodies (tested against Venezuelan, eastern and western equine encephalitis viruses) were used for experimental infections. The lack of an anamnestic neutralizing antibody response to the latter viruses after VEEV infection suggested that they had not been vaccinated before against alphaviruses. The horses were infected by s.c. inoculation in the shoulder region with 2,000 plaque-forming units (within the range inoculated by VEEV mosquito vectors; see ref. 40) of VEEV in 1 ml of MEM containing 10% alphavirus antibody-free horse serum. Rectal temperatures were recorded twice daily, and blood was collected twice daily from the jugular vein. Animals that developed clinical signs of encephalitis or prolonged anorexia were killed with an overdose of pentobarbital.
Phylogenetic Analysis.
Sequencing of the pE2 envelope glycoprotein no. 2 precursor gene was performed by amplification by using RT-PCR viral RNA. Nucleotide and deduced amino acid sequences were aligned with homologous VEEV sequences from the GenBank library by using the pileup program of the Genetics Computer Group (Madison, WI) (48) and analyzed by using maximum parsimony and neighbor-joining programs implemented in the paup* 4.0 software package (49) as well as Bayesian analysis by using mrbayes 3.0 (50) with one million generations, a general time-reversible model of nucleotide substitutions with empirically estimated base frequencies, and either codon position-specific rates or a gamma model for the distribution of substitution rates among nucleotide sites.
Statistics.
ANOVA (for normally distributed data) or the Kruskal–Wallis test (for data not normally distributed) with Dunn’s multiple comparisons test were used to evaluate mean plaque sizes and viremia titers. For serum samples negative for virus, one half the value representing the detection limit of the assay was used for calculation of means (1.1 suckling mouse LD50 units).
Supplementary Material
Acknowledgments
We thank Wenli Kang for excellent technical assistance and Diana Ortiz for excellent statistical assistance. This research was supported by National Institutes of Health (NIH) Grants AI39800 and AI48807. S.P. was supported by NIH K08 Grant AI059491. I.P.G. was supported by the Centers for Disease Control and Prevention Training Grant T01/CCT622892.
Abbreviations
- VEE
Venezuelan equine encephalitis
- VEEV
VEE virus.
Conflict of interest statement: No conflicts declared.
This paper was submitted directly (Track II) to the PNAS office.
See Commentary on page 4803.
References
- 1.Guan Y., Zheng B. J., He Y. Q., Liu X. L., Zhuang Z. X., Cheung C. L., Luo S. W., Li P. H., Zhang L. J., Guan Y. J., et al. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 2.Rota P. A., Oberste M. S., Monroe S. S., Nix W. A., Campagnoli R., Icenogle J. P., Penaranda S., Bankamp B., Maher K., Chen M. H., et al. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 3.Nichol S. T., Spiropoulou C. F., Morzunov S., Rollin P. E., Ksiazek T. G., Feldman H., Sanchez A., Childs J., Zaki S., Peters C. J. Science. 1993;262:914–917. doi: 10.1126/science.8235615. [DOI] [PubMed] [Google Scholar]
- 4.Feldmann H., Wahl-Jensen V., Jones S. M., Stroher U. Trends Microbiol. 2004;12:433–437. doi: 10.1016/j.tim.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 5.Gao F., Bailes E., Robertson D. L., Chen Y., Rodenburg C. M., Michael S. F., Cummins L. B., Arthur L. O., Peeters M., Shaw G. M., et al. Nature. 1999;397:436–441. doi: 10.1038/17130. [DOI] [PubMed] [Google Scholar]
- 6.Webster R. G., Hulse D. J. Rev. Sci. Tech. 2004;23:453–465. doi: 10.20506/rst.23.2.1493. [DOI] [PubMed] [Google Scholar]
- 7.Wang E., Ni H., Xu R., Barrett A. D., Watowich S. J., Gubler D. J., Weaver S. C. J. Virol. 2000;74:3227–3234. doi: 10.1128/jvi.74.7.3227-3234.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holmes E. C., Twiddy S. S. Infect. Genet. Evol. 2003;3:19–28. doi: 10.1016/s1567-1348(03)00004-2. [DOI] [PubMed] [Google Scholar]
- 9.Domingo E. Virology. 2000;270:251–253. doi: 10.1006/viro.2000.0320. [DOI] [PubMed] [Google Scholar]
- 10.Holland J., Domingo E. Virus Genes. 1998;16:13–21. doi: 10.1023/a:1007989407305. [DOI] [PubMed] [Google Scholar]
- 11.Weaver S. C., Barrett A. D. Nat. Rev. Microbiol. 2004;2:789–801. doi: 10.1038/nrmicro1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walton T. E., Grayson M. A. In: The Arboviruses: Epidemiology and Ecology. Monath T. P., editor. Vol. 4. Boca Raton, FL: CRC; 1988. pp. 203–231. [Google Scholar]
- 13.Weaver S. C., Salas R., Rico-Hesse R., Ludwig G. V., Oberste M. S., Boshell J., Tesh R. B. Lancet. 1996;348:436–440. doi: 10.1016/s0140-6736(96)02275-1. [DOI] [PubMed] [Google Scholar]
- 14.Lord R. D. Bull. Pan Am. Health Organ. 1974;8:100–110. [PubMed] [Google Scholar]
- 15.Kinney R. M., Johnson B. J., Welch J. B., Tsuchiya K. R., Trent D. W. Virology. 1989;170:19–30. doi: 10.1016/0042-6822(89)90347-4. [DOI] [PubMed] [Google Scholar]
- 16.Ludwig G. V., Kondig J. P., Smith J. F. J. Virol. 1996;70:5592–5599. doi: 10.1128/jvi.70.8.5592-5599.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klimstra W. B., Nangle E. M., Smith M. S., Yurochko A. D., Ryman K. D. J. Virol. 2003;77:12022–12032. doi: 10.1128/JVI.77.22.12022-12032.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernard K. A., Klimstra W. B., Johnston R. E. Virology. 2000;276:93–103. doi: 10.1006/viro.2000.0546. [DOI] [PubMed] [Google Scholar]
- 19.Strauss J. H., Strauss E. G. Microbiol. Rev. 1994;58:491–562. doi: 10.1128/mr.58.3.491-562.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schlesinger S., Schlesinger M. J. In: Fields’ Virology. 4th Ed. Knipe D. M., Howley P. M., editors. New York: Lippincott, Williams & Wilkins; 2001. pp. 895–916. [Google Scholar]
- 21.Griffin D. E. In: Fields’ Virology. 4th Ed. Knipe D. M., Howley P. M., editors. New York: Lippincott, Williams & Wilkins; 2001. pp. 917–962. [Google Scholar]
- 22.Weaver S. C., Ferro C., Barrera R., Boshell J., Navarro J. C. Annu. Rev. Entomol. 2004;49:141–174. doi: 10.1146/annurev.ento.49.061802.123422. [DOI] [PubMed] [Google Scholar]
- 23.Weaver S. C., Pfeffer M., Marriott K., Kang W., Kinney R. M. Am. J. Trop. Med. Hyg. 1999;60:441–448. doi: 10.4269/ajtmh.1999.60.441. [DOI] [PubMed] [Google Scholar]
- 24.Kinney R. M., Tsuchiya K. R., Sneider J. M., Trent D. W. J. Genet. Virol. 1992;73:3301–3305. doi: 10.1099/0022-1317-73-12-3301. [DOI] [PubMed] [Google Scholar]
- 25.Johnson K. M., Martin D. H. Adv. Vet. Sci. Comp. Med. 1974;18:79–116. [PubMed] [Google Scholar]
- 26.Young N. A., Johnson K. M. Am. J. Epidemiol. 1969;89:286–307. doi: 10.1093/oxfordjournals.aje.a120942. [DOI] [PubMed] [Google Scholar]
- 27.Rico-Hesse R., Roehrig J. T., Trent D. W., Dickerman R. W. Am. J. Trop. Med. Hyg. 1988;38:195–204. doi: 10.4269/ajtmh.1988.38.195. [DOI] [PubMed] [Google Scholar]
- 28.Powers A. M., Oberste M. S., Brault A. C., Rico-Hesse R., Schmura S. M., Smith J. F., Kang W., Sweeney W. P., Weaver S. C. J. Virol. 1997;71:6697–6705. doi: 10.1128/jvi.71.9.6697-6705.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rico-Hesse R., Weaver S. C., de Siger J., Medina G., Salas R. A. Proc. Natl. Acad. Sci. USA. 1995;92:5278–5281. doi: 10.1073/pnas.92.12.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang E., Bowen R. A., Medina G., Powers A. M., Kang W., Chandler L. M., Shope R. E., Weaver S. C. Am. J. Trop. Med. Hyg. 2001;65:64–69. doi: 10.4269/ajtmh.2001.65.64. [DOI] [PubMed] [Google Scholar]
- 31.Pletnev S. V., Zhang W., Mukhopadhyay S., Fisher B. R., Hernandez R., Brown D. T., Baker T. S., Rossmann M. G., Kuhn R. J. Cell. 2001;105:127–136. doi: 10.1016/s0092-8674(01)00302-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greene I. P., Paessler S., Austgen L., Anishchenko M., Brault A. C., Bowen R. A., Weaver S. C. J. Virol. 2005;79:9128–9133. doi: 10.1128/JVI.79.14.9128-9133.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson B. J., Brubaker J. R., Roehrig J. T., Trent D. W. Virology. 1990;177:676–683. doi: 10.1016/0042-6822(90)90533-w. [DOI] [PubMed] [Google Scholar]
- 34.Brault A. C., Powers A. M., Holmes E. C., Woelk C. H., Weaver S. C. J. Virol. 2002;76:1718–1730. doi: 10.1128/JVI.76.4.1718-1730.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anishchenko M., Paessler S., Greene I. P., Aguilar P. V., Carrara A. S., Weaver S. C. J. Virol. 2004;78:1–8. doi: 10.1128/JVI.78.1.1-8.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roehrig J. T., Bolin R. A. J. Clin. Microbiol. 1997;35:1887–1890. doi: 10.1128/jcm.35.7.1887-1890.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martin D. H., Dietz W. H., Alvaerez O., Jr., Johnson K. M. Am. J. Trop. Med. Hyg. 1982;31:561–568. doi: 10.4269/ajtmh.1982.31.561. [DOI] [PubMed] [Google Scholar]
- 38.Wang E., Barrera R., Boshell J., Ferro C., Freier J. E., Navarro J. C., Salas R., Vasquez C., Weaver S. C. J. Virol. 1999;73:4266–4271. doi: 10.1128/jvi.73.5.4266-4271.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weaver S. C., Bellew L. A., Gousset L., Repik P. M., Scott T. W., Holland J. J. Virology. 1993;195:700–709. doi: 10.1006/viro.1993.1421. [DOI] [PubMed] [Google Scholar]
- 40.Smith D. R., Carrara A. S., Aguilar P. V., Weaver S. C. Am. J. Trop. Med. Hyg. 2005;73:33–39. [PubMed] [Google Scholar]
- 41.Weaver S. C. In: Viral Pathogenesis. Nathanson N., editor. New York: Lippincott–Raven; 1997. pp. 329–352. [Google Scholar]
- 42.Young N. A., Johnson K. M., Gauld L. W. Am. J. Trop. Med. Hyg. 1969;18:290–296. [PubMed] [Google Scholar]
- 43.Carrara A., Gonzales M., Ferro C., Tamayo M., Aronson J., Paessler S., Anishchenko M., Boshell J., Weaver S. C. Emerg. Infect. Dis. 2005;11:663–669. doi: 10.3201/eid1105.041251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coffey L. L., Carrara A. S., Paessler S., Haynie M. L., Bradley R. D., Tesh R. B., Weaver S. C. Emerg. Infect. Dis. 2004;10:2182–2188. doi: 10.3201/eid1012.040442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brault A. C., Powers A. M., Weaver S. C. J. Virol. 2002;76:6387–6392. doi: 10.1128/JVI.76.12.6387-6392.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brault A. C., Powers A. M., Ortiz D., Estrada-Franco J. G., Navarro-Lopez R., Weaver S. C. Proc. Natl. Acad. Sci. USA. 2004;101:11344–11349. doi: 10.1073/pnas.0402905101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ortiz D. I., Weaver S. C. J. Med. Entomol. 2004;41:987–993. doi: 10.1603/0022-2585-41.5.987. [DOI] [PubMed] [Google Scholar]
- 48.Devereux J., Haeberli P., Smithies O. Nucleic Acids Res. 1984;12:387–395. doi: 10.1093/nar/12.1part1.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Swofford D. L. paup*: Phylogenetic Analysis Using Parsimony (*and Other Methods) Sunderland, Massachusetts: Sinauer Associates; 1998. Ver. 4. [Google Scholar]
- 50.Huelsenbeck J. P., Ronquist F. Bioinformatics. 2001;17:754–755. doi: 10.1093/bioinformatics/17.8.754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.