Abstract
Intratracheal delivery of aerosolized monoclonal antibodies with specificity for Yersinia pestis LcrV and F1 antigens protected mice in a model of pneumonic plague. These data support the utility of inhaled antibodies as a fast-acting postexposure treatment for plague.
Yersinia pestis is a gram-negative bacterium that causes bubonic, septicemic, and pneumonic plagues. The natural hosts of Y. pestis are small mammals, with the occasional spread to humans from animal reservoirs via the bite of an infected flea causing bubonic plague. Bubonic plague can develop into the more deadly pneumonic form of plague which can then spread bacteria from person to person via airborne droplets, with the potential for rapid spread of the disease. The ability of Y. pestis to infect via the airborne route also makes it a potential bioterrorist weapon. Efforts to control plague outbreaks rely on effective health surveillance monitoring and medical treatments to prevent epidemic spread of the disease (16).
New plague vaccines based on the F1 and V antigen (LcrV) proteins provide a high degree of protection but must be administered several weeks before exposure to prevent plague (2, 10, 13, 17, 21, 22, 25). Although strategies to reduce the time to immunity have shown promise (23), it is unlikely that vaccines will provide postexposure protection against plague. Antibiotics are used for prophylactic treatment to control the spread of the disease and as a therapy (16). However, plasmid-borne antibiotic resistance has been reported previously (8, 9). Furthermore, compliance issues and side effects associated with continued antibiotic administration following the 2001 anthrax attack in the United States highlights the need for treatments that are free from side effects (20).
As an alternative to antibiotics, antibody treatment has been demonstrated to be effective against a number of infectious diseases (4, 26, 27), including plague (1, 12). We showed recently that intraperitoneal injection of monoclonal antibodies (MAbs) that target the F1 and LcrV proteins (MAb F1-04-A-G1 and MAb 7.3, respectively) protected mice in a synergistic manner as a pretreatment or as a postexposure therapy (11).
Ideally, a therapy to mitigate against disease following the deliberate release of a bioterrorist weapon should be compatible with self-administration by a minimally invasive route and provide long-term protection. It is known that compounds of various molecular sizes, including antibodies, can be delivered via the lung to treat a range of respiratory and nonrespiratory diseases (5, 14, 15, 18). The lung has many perceived benefits for administration of therapeutics to treat infections caused by inhaled microorganisms (5, 18, 19). Inhalational delivery of aerosolized antibodies could be used to rapidly generate a high concentration of antibody in the lung milieu, the most likely portal of entry to the body for Y. pestis and other airborne pathogens. Perhaps most importantly, inhaled therapies have the potential for self-administration. In this study we evaluated the therapeutic properties of antibodies administered as an aerosol in a model of pneumonic plague.
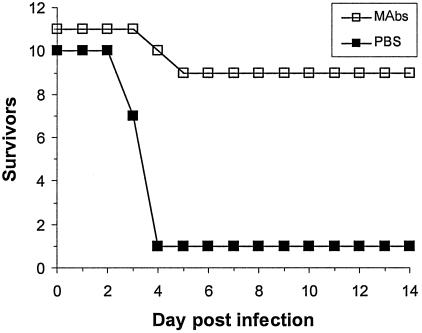
All experiments were conducted in accordance with the United Kingdom Animals (Scientific Procedures) Act 1986. Six- to eight-week-old female BALB/c mice (Charles Rivers, Margate, United Kingdom) were exposed to 2,700 CFU aerosolized Y. pestis strain GB as described previously (24). Strain GB has a minimal lethal dose of approximately 100 CFU following aerosol challenge in our model (17, 23, 24). Two hours following challenge, mice were anesthetized by intraperitoneal injection of 100 μl saline containing 0.6 mg medetomidine (Pfizer, Kent, United Kingdom) and 1.65 mg ketamine (Fort Dodge Animal Heath, Southampton, United Kingdom). A PenCentuary (PenCentuary, Inc., PA) intratracheal microsprayer device was used to deliver MAbs 7.3 and F1-04-A-G1 in a 50-μl volume of phosphate-buffered saline (PBS) (3). Protective plague MAbs F1-04-A-G1 (1) and 7.3 (12) were affinity purified from tissue culture cell supernatants as described previously (11). Each mouse was dosed with 77.5 μg of each antibody. Immediately following intratracheal dosing, animals were revived by subcutaneous injection of 0.1 mg atipamezole hydrochloride (Pfizer, Kent, United Kingdom). Mice treated postexposure with MAbs were protected from infection with aerosolized Y. pestis (GB), whereas mice dosed with PBS were not (P < 0.01; log rank test) (Fig. 1).
FIG. 1.
Lung delivery of antibody protects mice against pneumonic plague. Mice received 77.5 μg of MAb 7.3 and 77.5 μg of MAb F1-04-A-G1 in 50 μl of PBS via the intratracheal route 2 h after infection with 27 minimal lethal doses of Y. pestis. MAb 7.3 offered statistically significant protection compared with results for PBS-treated mice (P = 0.003; log rank test).
To investigate MAb biodistribution following pulmonary delivery, a cohort of mice were anesthetized and dosed intratracheally with MAb F1-04-A-G1 and MAb 7.3 using the PenCentuary (PenCentuary, Inc., PA) intratracheal microsprayer device as described previously (3). Mice were dosed with either 15.5 or 77.5 mg of each antibody. Two hours following intratracheal dosing, blood samples were taken by cardiac puncture of terminally anesthetized mice prior to humane killing by cervical dislocation. Blood was stored overnight at 4°C and centrifuged at 12,000 × g, and the serum component was removed by aspiration and stored at −20°C prior to analysis. Bronchoalveolar lavage wash samples were collected by gently injecting 5 ml of ice-cold lavage medium (0.9% [wt/vol] NaCl, 0.05% [wt/vol] Tween 20, 0.1% [wt/vol] NaN3, and 1 mM phenylmethylsulfonyl fluoride) (Sigma, Dorset, United Kingdom) into the trachea to inflate the lungs, by means of an intravenous cannula (Abbott Laboratories, Ireland); antibody solutions were stored at −20°C prior to analysis. Titration of specific antibody in serum or bronchoalveolar lavage samples was achieved with an indirect enzyme-linked immunosorbent assay as described previously (7). Anti-LcrV and anti-F1 MAbs were detected in the serum samples of all treated mice (Table 1), indicating that Y. pestis-specific antibodies access the systemic compartment following intratracheal aerosol delivery. There is likely to be significant mucociliary clearance following bronchopulmonary delivery of antibodies (14, 15). The inability to detect anti-LcrV and anti-F1 MAbs in lung wash samples 2 hours after intratracheal administration in all but two of the treated animals is consistent with the thesis that MAbs are either rapidly cleared or absorbed into the blood and lymph (6, 18).
TABLE 1.
Analysis of serum and lung wash samples following intratracheal administration of MAbs 7.3 and F1-04-A-G1
| Mouse | Treatmenta | Amt of MAb (ng ml−1)b
|
|||
|---|---|---|---|---|---|
| 7.3
|
F1-04-A-G1
|
||||
| Serum | Lung wash | Serum | Lung wash | ||
| 1 | PBS | ND | ND | ND | ND |
| 2 | PBS | ND | ND | ND | ND |
| 3 | 15.5 μg MAb | 1,631 | ND | 882 | ND |
| 4 | 15.5 μg MAb | 18 | 5 | 77 | 20 |
| 5 | 15.5 μg MAb | 5 | 10 | 43 | 30 |
| 6 | 15.5 μg MAb | 284 | ND | 377 | ND |
| 7 | 77.5 μg MAb | 586 | ND | 872 | ND |
| 8 | 77.5 μg MAb | 671 | ND | 634 | ND |
MAb 7.3 (15.5 or 77.5 μg in 50 μl PBS) and MAb F1-04-A-G1 (15.5 or 77.5 μg in 50 μl PBS) or PBS was delivered as a spray to the lungs of anesthetized mice by means of the PenCentuary device.
Amount of MAb 7.3 or MAb F1-04-A-G1 in mouse serum and lung wash samples 2 h posttreatment. ND, none detected.
In summary, these data demonstrate that mice can be protected from aerosol-initiated infection by intratracheal administration of aerosolized Y. pestis-specific antibodies. These data support the development of self-administrable antibody-based drugs for plague treatment, to be used in the event of a bioterrorist attack.
Acknowledgments
We acknowledge the support of Amanda Gates, Wendy Butcher, Tony Stagg, and Steve Lever, DSTL, Porton Down, United Kingdom, and Robert Bull, NMRC, Bethesda, MD, for MAb F1-04-A-G1.
Editor: J. B. Bliska
REFERENCES
- 1.Anderson, G. W., P. L. Worsham, C. R. Bolt, G. P. Andrews, S. L. Welkos, A. M. Friedlander, and J. P. Burans. 1997. Protection of mice from fatal bubonic and pneumonic plague by passive immunization with monoclonal antibodies against the F1 protein of Yersinia pestis. Am. J. Trop. Med. Hyg. 56:471-473. [DOI] [PubMed] [Google Scholar]
- 2.Andrews, G. P., D. G. Heath, G. W. Anderson, S. L. Welkos, and A. M. Friedlander. 1996. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect. Immun. 64:2180-2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bivas-Benita, M., R. Zwier, H. E. Junginger, and G. Borchard. 2005. Non-invasive pulmonary aerosol delivery in mice by the endotracheal route. Eur. J. Pharm. Biopharm. 61:214-218. [DOI] [PubMed] [Google Scholar]
- 4.Casadevall, A. 2002. Passive antibody administration (immediate immunity) as a specific defense against biological weapons. Emerg. Infect. Dis. 8:833-841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cleland, J. L., A. Daugherty, and R. Mrsny. 2001. Emerging protein delivery methods. Curr. Opin. Biotechnol. 12:212-219. [DOI] [PubMed] [Google Scholar]
- 6.Davis, S. S. 1999. Delivery of peptide and non-peptide drugs through the respiratory tract. Pharm. Sci. Technol. Today 2:450-456. [DOI] [PubMed] [Google Scholar]
- 7.Eyles, J. E., G. J. E. Sharp, E. D. Williamson, I. D. Spiers, and H. O. Alpar. 1998. Intra nasal administration of poly-lactic acid microsphere co-encapsulated Yersinia pestis subunits confers protection from pneumonic plague in the mouse. Vaccine 16:698-707. [DOI] [PubMed] [Google Scholar]
- 8.Guiyoule, A., G. Gerbaud, C. Buchrieser, M. Galimand, L. Rahalison, S. Chanteau, P. Courvalin, and E. Carniel. 2001. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg. Infect. Dis. 7:43-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guiyoule, A., B. Rasoamanana, C. Buchrieser, P. Michel, S. Chanteau, and E. Carniel. 1997. Recent emergence of new variants of Yersinia pestis in Madagascar. J. Clin. Microbiol. 35:2826-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heath, D. G., G. W. Anderson, J. M. Mauro, S. L. Welkos, G. P. Andrews, J. Adamovicz, and A. M. Friedlander. 1998. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine 16:1131-1137. [DOI] [PubMed] [Google Scholar]
- 11.Hill, J., C. Copse, S. Leary, A. J. Stagg, E. D. Williamson, and R. W. Titball. 2003. Synergistic protection of mice against plague with monoclonal antibodies specific for the F1 and V antigens of Yersinia pestis. Infect. Immun. 71:2234-2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill, J., S. E. C. Leary, K. F. Griffin, E. D. Williamson, and R. W. Titball. 1997. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect. Immun. 65:4476-4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leary, S. E. C., E. D. Williamson, K. F. Griffin, P. Russell, S. M. Eley, and R. W. Titball. 1995. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect. Immun. 63:2854-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patton, J. S. 1996. Mechanisms of macromolecule absorption by the lungs. Adv. Drug Delivery Rev. 19:3-36. [Google Scholar]
- 15.Patton, J. S. 2000. Pulmonary delivery of drugs for bone disorders. Adv. Drug Delivery Rev. 42:239-248. [DOI] [PubMed] [Google Scholar]
- 16.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Russell, P., S. M. Eley, S. E. Hibbs, R. J. Manchee, A. J. Stagg, and R. W. Titball. 1995. A comparison of plague vaccine, Usp and Ev76 vaccine-induced protection against Yersinia pestis in a murine model. Vaccine 13:1551-1556. [DOI] [PubMed] [Google Scholar]
- 18.Sanjar, S., and J. Matthews. 2001. Treating systemic diseases via the lung. J. Aerosol Med. 14:S51-S58. [DOI] [PubMed] [Google Scholar]
- 19.Sayani, A. P., and Y. W. Chien. 1996. Systemic delivery of peptides and proteins across absorptive mucosae. Crit. Rev. Ther. Drug Carrier Syst. 13:85-184. [PubMed] [Google Scholar]
- 20.Shepard, C. W., M. Soriano-Gabarro, E. R. Zell, J. Hayslett, S. Lukacs, S. Goldstein, S. Factor, J. Jones, R. Ridzon, I. Williams, and N. Rosenstein. 2002. Antimicrobial postexposure prophylaxis for anthrax: adverse events and adherence. Emerg. Infect. Dis. 8:1124-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Titball, R. W., and E. D. Williamson. 2004. Yersinia pestis (plague) vaccines. Exp. Opin. Biol. Ther. 4:965-973. [DOI] [PubMed] [Google Scholar]
- 22.Williamson, E. D. 2001. Plague vaccine research and development. J. Appl. Microbiol. 91:606-608. [DOI] [PubMed] [Google Scholar]
- 23.Williamson, E. D., S. M. Eley, A. J. Stagg, M. Green, P. Russell, and R. W. Titball. 2000. A single dose sub-unit vaccine protects against pneumonic plague. Vaccine 19:566-571. [DOI] [PubMed] [Google Scholar]
- 24.Williamson, E. D., S. M. Eley, A. J. Stagg, M. Green, P. Russell, and R. W. Titball. 1997. A sub-unit vaccine elicits IgG in serum, spleen cell cultures and bronchial washings and protects immunized animals against pneumonic plague. Vaccine 15:1079-1084. [DOI] [PubMed] [Google Scholar]
- 25.Williamson, E. D., and R. W. Titball. 2002. Vaccines against dangerous pathogens. Br. Med. Bull. 62:163-173. [DOI] [PubMed] [Google Scholar]
- 26.Zeitlin, L., R. A. Cone, T. R. Moench, and K. J. Whaley. 2000. Preventing infectious disease with passive immunization. Microbes Infect. 2:701-708. [DOI] [PubMed] [Google Scholar]
- 27.Zeitlin, L., R. A. Cone, and K. J. Whaley. 1999. Using monoclonal antibodies to prevent mucosal transmission of epidemic infectious diseases. Emerg. Infect. Dis. 5:54-64. [DOI] [PMC free article] [PubMed] [Google Scholar]