Abstract
Background
Trochanteric pain is the second most important diagnosis of hip problems presenting in primary care, but its incidence and prognosis in this context is largely unknown.
Aim
To determine the 1- and 5-year prognoses of trochanteric pain and the predictive variables for consistent complaints.
Design of the study
Retrospective cohort study.
Setting
One hundred and sixty-four patients (mean age = 55 years, 80% female) with incidental trochanteric pain in the years 1996 or 2000 were asked in 2001 for past and present symptoms of trochanteric pain. Therapeutic interventions, demographic factors and comorbidity were also investigated.
Method
The databases of 39 GPs were screened in order to identify all incident cases with a suspicion of trochanteric pain in the years 1996 or 2000. These cases were sent a questionnaire.
Results
The incidence of trochanteric pain in primary care is 1.8 patients per 1000 per year. After 1 year at least 36% still suffered from trochanteric pain, and after |5 years this was 29%. Patients with osteoarthritis (OA) in the lower limbs had a 4.8-fold risk of persistent symptoms after 1 year, as compared to patients without OA. Patients who had received a corticosteroid injection had a 2.7-fold chance of recovery after |5 years, as compared with patients who had not received an injection.
Conclusion
Trochanteric pain is shown to be a chronic disease in a substantial number of patients. The disorder is associated with much impairment when conducting daily activities.
Keywords: bursitis, cohort studies, osteoarthritis, primary care, trochanter, trochanteric pain
INTRODUCTION
Trochanteric pain, also known as trochanteric bursitis or pseudotrochanteric bursitis, is a frequently occurring problem. The pain experienced by 10–20% of all patients with hip problems presenting in primary care can be attributed to trochanteric pain.1
In 1979, Little described trochanteric pain as pain at the lateral side of the upper thigh, often with radiation to the knee.2 Although it has been attributed to trochanteric bursitis and/or tendinitis, one study reported that sonographic effusion of the bursa was seldom found; effusion around the trochanteric tendons, however, was more often present than in other patients with hip pain.3
Trochanteric pain has been described as a solitary syndrome that can occur as a result of trauma or as a comorbid condition in patients with lower back pain or osteoarthritis (OA) of the hip.4-11 Some authors have even described trochanteric pain as one of the first symptoms in developing hip OA.7,8
In order to gain more insight into trochanteric pain, we performed a retrospective cohort study in general practice, focusing on the 1- and 5-year prognosis.
In this article we aimed to address the following questions:
What is the incidence of trochanteric pain in general practice?
What is the impact of trochanteric pain on daily activities?
What therapy is given?
What is the prognosis of trochanteric pain after 1 and 5 years?
What variables might predict the prognosis?
METHOD
Sample identification and selection
GPs using electronic medical databases were approached in 2001 for participation in the study. Patients aged 18 years and older who presented to their GP in 1996 or 2000 with pain at the region of the greater trochanter were identified. The identification of these patients was done in a sensitive search in the electronic medical databases using the keywords ‘troch*’ or ‘pain*’ and ‘hip*’. The medical records of these patients were read, and they were identified as possible incident cases if they had consulted their GP for the first time in 2 years with this symptom. Only patients who confirmed by questionnaire that they had suffered from pain at the lateral side of the upper leg were considered incident cases with trochanteric pain.
The patients with trochanteric pain in 1996 were asked for the present condition of their symptoms. These data were used for the prognosis after |5 years. The data from patients with trochanteric pain in 2000 were used for the 1 year follow-up, subdivided into four groups: those presenting from January to March 2000 for the 16-month follow-up, those from April to June for the 13-month follow-up, from July to September for the 10-month follow-up, and finally, those from October to December 2000 for the 7-month follow-up.
How this fits in
Trochanteric pain is a common problem in general practice. The incidence of trochanteric pain in primary care is 1.8 per 1000 patients per year. In the majority of cases it is a prolonged, chronic disease, and causes substantial impairment of daily activities.
Questionnaire
The questionnaire covered patient characteristics (demographic data, daily activities and comorbidity), and various characteristics of the trochanteric pain (past and present symptoms, localisation, pain severity [Visual Analogue Scale {VAS}, 0–100] and type of therapy).
The present quality of life was assessed with the EuroQol (0 = worst possible quality of life, 1 = best possible quality of life).12 The present functional disability due to the trochanteric pain was assessed with the WOMAC (Western Ontario and McMaster) osteoarthritis index.13 This index is used to assess disability due to arthritis of the hip or knee. It has three discrete domains – pain (five questions, possible subscale score 0–20), stiffness (two questions, 0–8) and physical functioning (17 questions, 0–68) – and has a minimum score of 0 (best score) and a maximum score of 96 (worst score).
Data analysis
We investigated the percentage of patients who still had symptoms of trochanteric pain in 2001 (observed values). In a sensitivity analysis we assessed whether these figures would change due to potential selective non-response (expected values). In the first analysis we assumed that all non-responders did have trochanteric pain at baseline and were free of trochanteric pain at the time of investigation (best case scenario). In the second analysis we assumed them to still suffer from trochanteric pain at the end of the follow-up (worst case scenario).
Left and right censoring
There were only two time measurements for each patient: time of diagnosis and that of the follow-up investigation. This implies that the data of a specified time are based only on that particular subgroup of patients. For example, for patients with a follow-up of 13 months there is no data on their situation at 7, 10, 16 or 60 months, so if someone has recovered by 13 months, she/he could already have recovered by the 7- or 10-month stage; likewise, if not recovered at that time, she/he could have been recovered at 16 or 60 months. This ‘left and right censoring’ we corrected by analysing our data with the SAS program PROC LIFE REG (version 6.12).
Predictive variables
Variables that might have predicted improvement such as sex, duration of symptoms, body mass index (BMI) and co-morbidity were evaluated using the binary logistic regression mode in SPSS. Variables with a P-value of 0.20 or less in the univariate analysis were considered in the backward stepwise multivariate model. Variables with a P-value of 0.10 or less in the multivariate model were left in the model.
RESULTS
Incidence
Forty-one GPs in the southwest region of the Netherlands were approached, and 39 were willing to participate. A total of 95 297 persons were registered with these GPs.
Three hundred and forty-five patients with a suspicion of trochanteric pain were identified and sent a questionnaire, of whom 187 (54%) replied. Of these responders, 164 (88%) met our criteria of trochanteric pain – that is, patients ≥18 years of age with pain in the region of the greater trochanter (cases). The remaining 23 patients reported pain symptoms in the lower back, groin, buttocks or knees and not in the region of the greater trochanter. Figure 1 shows the flowchart of the patients and responders.
Figure 1.
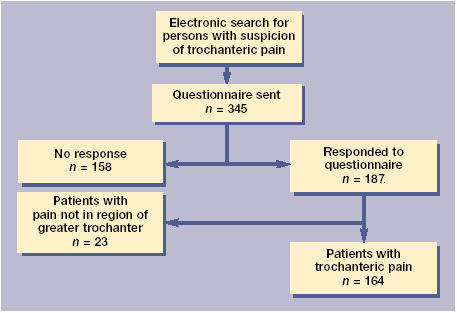
Flow-chart of patients and responders
There were no statistically significant differences between sex and age between the non-responders, responders and cases. Also, no statistical differences were found for comorbidity between the responders and the cases (Table 1).
Table 1.
Characteristics of all identified patients.
| Identified patients | Non responders | Responders | Cases | |
|---|---|---|---|---|
| Number | 345 | 158 | 187 | 164 |
| Mean age in years (SD) | 55.3 (15.4) | 54.4 (17.4) | 56.0 (13.5) | 55.4 (13.5) |
| Females (%) | 75 | 69 | 79.9 | 79.9 |
| Arthrosis on lower limbs, or lower back pain (%) | 48 | 58 |
SD = standard deviation.
The incidence of trochanteric pain registered by the GPs in this population is 1.8 per 1000 patients per year.
Patient characteristics and impact of trochanteric pain
Of the 164 cases 80% were female and the mean age at diagnosis was 55.4 years (range = 21–87 years). Table 2 details other patient characteristics.
Table 2.
Characteristics of patients with trochanteric pain (n = 164).
| Baseline | Follow-up | |
|---|---|---|
| Mean age in years(SD) | 55.4 (13.5) | |
| Females (%) | 79.9 | 79.9 |
| Localisation | ||
| Right (%) | 40 | 40 |
| Bilateral (%) | 23 | 23 |
| Body Mass Index | ||
| Overweight (BMI 25–30) (%) | a | 35 |
| Obese (BMI >30) (%) | a | 15 |
| Hip osteoarthritis (%) | a | 24 |
| Knee osteoarthritis (%) | a | 16 |
| Lower back pain (%) | a | 14 |
Due to study design, reliable data at baseline for BMI and co-morbidity is unavailable. SD = standard deviation.
Of those working, about 34% were ‘very much troubled’ during work-related activities, and about a quarter of them had a history of sick leave due to the trochanteric pain. Roughly 40% of the patients were disturbed during sleep. Of the 60% of patients who participated in sport, 54% were ‘greatly impaired’ during their sporting activities.
The mean VAS score for hip pain in patients still suffering from trochanteric pain at follow-up was 46.0 and their mean total WOMAC score was 36.5. The mean total WOMAC score for those recovered was 11.2.
The mean EuroQol score for those with prolonged symptoms was 0.97 and for those recovered 0.99. The state of health assessed with the VAS was 68.5 for those with symptoms at follow-up, and 78.6 for those recovered (Table 3).
Table 3.
Pain and quality-of-life scores at follow-up for those with greater trochanteric pain symptoms (n = 116) and those without (n = 48).
| With symptoms at follow-up | Without symptoms at follow-up | (P-value) | |
|---|---|---|---|
| Pain (VAS 0–100) | 46.0 | 4.4 | <0.0001 |
| WOMAC pain (0–20) | 8.6 | 2.3 | <0.0001 |
| WOMAC function (0–68) | 25.0 | 7.6 | <0.0001 |
| WOMAC stiffness (0–8) | 3.1 | 1.3 | <0.0001 |
| WOMAC total (0–96) | 36.5 | 11.2 | <0.0001 |
| EuroQol | 0.970 | 0.992 | 0.024 |
| State of health (VAS 0–100) | 68.5 | 78.6 | 0.008 |
WOMAC = Western Ontario and McMaster osteoarthritis index. VAS = Visual Analogue Scale.
Therapy
Fifty-five per cent of patients were treated by their GP or specialist with medication (paracetamol, non-steroidal anti-inflammatory drugs [NSAIDs] and 52% of these patients mentioned a temporary improvement. Of the cases, 37% were injected in the region of the greater trochanter with corticosteroids (66% with improvement).
A third (35%) of the patients were only treated by their GP. Of these, 53% received paracetamol or NSAIDs (48% with improvement) and 34% were injected (60% with improvement).
Half (52%) of the patients in the study received physiotherapy (two-thirds of whom mentioned improvement). A third (36%) of the cases attended hospital, where therapy consisted of administration of paracetamol or NSAIDs (36%), or a local corticosteroid injection (34%). Three out of the five patients who received an operative treatment reported a reduction in pain.
Prognosis
At the 1-year follow-up stage, 76% of the responders still suffered from trochanteric pain; at 5 years this figure stood at 63%.
In the best-case scenario (all non-responders were cured at the time of investigation) at 1-year follow-up, 36% still had trochanteric pain and at 5 years, 29% did.
In the worst-case scenario (all non-responders were not cured at the time of investigation), these percentages changed to 84% and 83% respectively.
In the best-fitted analysis (PROC LIFE REG SAS), 78% of the responders had symptoms at 1-year follow-up and 60% at 5-year follow-up. Observed and expected values are shown in Figure 2.
Figure 2.
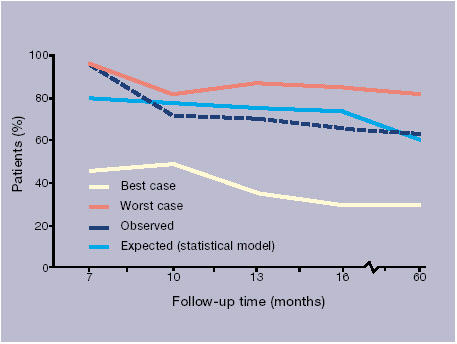
Percentage of patients with symptoms of trochanteric pain at follow-up (%).
Predictive variables
For the prognosis at 1 year, there were two variables that predicted sustained symptoms of trochanteric pain; duration of symptoms before the patient visited the GP (more versus less than 1 week) (odds ratio [OR] = 4.9, 90% confidence interval [CI] = 1.8 to 13.2) and the presence of OA in the lower limb(s) at follow-up (OR = 4.8 [CI = 1.2 to 18.5]). In this model, age and sex were considered as confounders (Table 4).
Table 4.
Possible determinants for prolonged complaints of trochanteric pain (univariate and multivariate analyses)
| 1-year follow-up | 5-year follow-up | |||
|---|---|---|---|---|
| Variables | Univariate OR (P-value) | Multivariate OR (90% CI) | Univariate OR (P-value) | Multivariate OR (90% CI) |
| Age (continuous) | 1.02 (0.30) | 1.01 (0.97 to 1.04) | 1.00 (0.95) | 1.00 (0.96 to 1.04) |
| Sex (male/female) | 1.75 (0.41) | 1.39 (0.41 to 4.77) | 1.23 (0.74) | 0.78 (0.25 to 2.38) |
| Bilateral symptoms (−/+) | 1.03 (0.96) | 2.32 (0.19) | 2.35 (0.66 to 8.35) | |
| BMI | ||||
| Normal (<25) | 0.55 (0.21) | a | ||
| Overweight (25–30) | 2.32 (0.13) | 2.38 (0.81 to 6.98) | a | |
| Obese (>30) | 0.83 (0.77) | a | ||
| Level of education | ||||
| Low (primary school) | 2.98 (0.07) | 1.73 (0.31) | ||
| Normal (secondary school) | 0.32 (0.03) | 0.96 (0.94) | ||
| High (higher education) | 1.33 (0.68) | 0.42 (0.19) | 0.38 (0.11 to 1.33) | |
| Duration of symptomsb | 5.53 (0.003) | 4.88 (1.81 to 13.16) | 4.50 (0.10) | 5.29 (1.05 to 26.57) |
| Analgesics (−/+) | 1.68 (0.27) | 0.63 (0.37) | ||
| Corticosteroid injection (−/+) | 1.24 (0.66) | 0.45 (0.15) | 0.37 (0.13 to 1.00) | |
| Arthrosis lower extremities (−/+) | 4.26 (0.03) | 4.77 (1.23 to 18.50) | a | |
| Lower back symptoms (−/+) | 4.19 (0.18) | 2.70 (0.42 to 17.52) | a | |
Data collected at the 5-year follow-up is likely to have changed over time and cannot be used as a determinant.
Before visit to the GP (less than 1 week/1 week or more). OR = odds ratio.
Patients developing OA did not receive corticosteroid injections more or less often when compared to patients not developing the disease (χ2 = 1.43, P = 0.71). No statistically significant differences were found in specific symptoms at first presentation, such as pain located only at the greater trochanter, or occurrence of the pain by applying pressure (χ2= 1.43 and 0.18 respectively, P = 0.71 and 0.33, respectively). In this model, age, sex, BMI, use of analgesics, or consultancy of physiotherapy all showed no significant relationship with the prognosis of trochanteric pain. For the long-term prognosis at 5 years there were two variables that predicted sustained symptoms of trochanteric pain: duration of symptoms before the patient visited the GP (more versus less than 1 week) (OR = 5.3 [CI = 1.1 to 26.6]); and having had a corticosteroid injection (OR = 0.4 [CI = 0.1 to 1.0]). In this model, age and sex were considered confounders.
DISCUSSION
Summary of main findings
The incidence of trochanteric pain in primary care is 1.8 patients per 1000 per year. In this study, after 1 year 76% of the responders still suffered from trochanteric pain, and after 5 years approximately 63% did. Due to possible selection bias, these figures would probably be lower in reality, but not lower than 36% and 29%, respectively.
Predictors associated with improvement within 1 year were duration of symptoms at the first visit to the GP and the absence of osteoarthritis in the lower limbs. Again, the duration of symptoms before the first visit to the GP, as well as having had a corticosteroid injection, were predictive for improvement within 5 years.
The strengths and limitations of this study
This study is vulnerable to different biases. The first is selection bias. This may be a result of the high number of non-responders (46%), and it is probable that patients with sustained symptoms were more likely to return the questionnaire. We were able to correct for this kind of bias in the calculation of the prognosis of trochanteric pain (best/worst-case scenario). Likewise, it could be that patients without symptoms at the time of the investigation did not return the questionnaire. Therefore, we expect that the real percentage with sustained symptoms is lower than observed, and will approximate those from the best-case scenario.
For the calculation of the incidence of trochanteric pain, however, the data are likely to be influenced by this selection bias. That is why we chose not extrapolate the 12% of patients who were inaccurately selected with pain located elsewhere to the non-responders group, but instead to calculate the incidence directly from the patients with trochanteric pain as reported by the GP.
The impact of trochanteric pain seems to be substantial; about 30–40% of the patients were impaired in their daily activities. However, these data are also prone to selection bias, because it is probable that the patients with sustained symptoms were more likely to return the questionnaire. Moreover, these data are also prone to a second type of bias introduced; the so-called recall bias (historical information reported by the participants is known to be inaccurate).
The third type of bias in this study is the bias by indication. An important finding of this study is that patients who received a corticosteroid injection in the region of the greater trochanter showed a better prognosis of their hip problems after 5 years. There might have been bias by indication; perhaps only patients with a lot of pain received an injection. Due to the retrospective character of this study, we were not able to correct for this potential confounder. However, assuming that the more severe cases have a worse prognosis, but also receive an injection earlier, this study gives an indication that corticosteroid injections are more effective than other treatments in trochanteric pain.
To look for other potential biases by indication, we analysed whether there were variables that might influence the GP to chose to give an injection. The only two variables found were pain elicited when the patient lay on the affected side, and the development of lower back pain at the time of follow-up. However, these variables do not significantly influence the model.
Finally, our results suggest that patients with OA had a higher risk of persistent symptoms after 1 year, compared to patients without OA. This finding may be biased because the greater trochanter is one of the sites to which hip or knee OA can refer to.14
As we only had information from the questionnaire, we did not have objective information about the condition of the patients. The data on OA were collected at the end of the follow-up period, and not when the symptoms of trochanteric pain began, therefore confusion between cause and consequence is possible. Nonetheless, we think that data on OA would not have changed much and would be fairly stable over a period of 1 year. Hence, we used these data in the model for the 1-year follow-up, but not for the 5-year follow-up.
Comparison with existing literature
Prognosis
This is the first study on the long-term prognosis of trochanteric pain. There are only a few case series available of patients receiving one type of intervention, but the longest follow-up time reported was 2 years. In that study a recovery rate of about 90% was reported.5 A different study reported on a follow-up after surgery of a maximum period of 60 months.15 These highly selected patients in secondary care are not comparable with our population in primary care.
Therapy
In our study population, 37% of patient received corticosteroid injection(s), and about 66% reported an improvement. This is comparable with the outcome of a case series in which about 61% of the patients had improved 6 months after local injection of corticosteroid and lidocaine.16
The improvement found in our study, however, differs from earlier case series in which all patients reported improvement after local corticosteroid injection(s).5,17 This discrepancy may be due to pre-selection of the patients (outpatient clinic) or the previously mentioned selection bias.
Implications for future research or clinical practice
These data show that trochanteric pain is a prolonged chronic disease in a substantial number of patients. The disorder is associated with great impairment in daily activities.
A trial comparing oral medication (analgesics) with corticosteroid injection is needed to investigate common and promising interventions in primary care for patients with trochanteric pain.
Acknowledgments
We thank Roos Bernsen for her clear advice on the statistical feasibility of this study design.
Funding body and reference number
This study was supported by a grant from the Revolving Fund, Erasmus Medical Centre, reference number 2000/164
Ethics committee and reference number
Reference number 194.008/2000/164
Competing interests
None
REFERENCES
- 1.Bierma-Zeinstra S, Bohnen A, Ginai A, et al. Validity of American College of Rheumatology criteria for diagnosing hip osteoarthritis in primary care research. J Rheumatol. 1999;26:1129–1133. [PubMed] [Google Scholar]
- 2.Little H. Trochanteric bursitis: a common cause of pelvic girdle pain. Can Med Assoc J. 1979;120:456–458. [PMC free article] [PubMed] [Google Scholar]
- 3.Bierma-Zeinstra SM, Bohnen AM, Bernsen RM, et al. Hip problems in older adults: classification by cluster analysis. J Clin Epidemiol. 2001;54:1139–1145. doi: 10.1016/s0895-4356(01)00398-5. [DOI] [PubMed] [Google Scholar]
- 4.Collee G, Dijkmans BA, Vandenbroucke JP, Cats A. Greater trochanteric pain syndrome (trochanteric bursitis) in low back pain. Scand J Rheumatol. 1991;20:262–266. doi: 10.3109/03009749109096798. [DOI] [PubMed] [Google Scholar]
- 5.Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehabil. 1986;67:815–817. [PubMed] [Google Scholar]
- 6.Traycoff RB. ‘Pseudotrochanteric bursitis’: the differential diagnosis of lateral hip pain. J Rheumatol. 1991;18:1810–1812. [PubMed] [Google Scholar]
- 7.Swezey RL. Pseudo-radiculopathy in subacute trochanteric bursitis of the subgluteus maximus bursa. Arch Phys Med Rehabil. 1976;57:387–390. [PubMed] [Google Scholar]
- 8.Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanter pain syndrome) Mayo Clin Proc. 1996;71:565–569. doi: 10.4065/71.6.565. [DOI] [PubMed] [Google Scholar]
- 9.Spear IM. Noninfectious trochanteric bursitis and peritendinitis. Surg Clin North Am. 1952;95:1217–1224. doi: 10.1016/s0039-6109(16)33703-3. [DOI] [PubMed] [Google Scholar]
- 10.Gordon EJ. Trochanteric bursitis and tendinitis. Clin Orthop. 1961;20:193–202. [PubMed] [Google Scholar]
- 11.Haller CC, Coleman PA, Estes NC, Grisolia A. Traumatic trochanteric bursitis. Kans Med. 1989;90:17–18, 22. [PubMed] [Google Scholar]
- 12.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 13.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 14.Creamer P, Lethbridge-Cejku M, Hochberg MC. Where does it hurt? Pain localization in osteoarthritis of the knee. Osteoarthritis Cartilage. 1998;6:318–323. doi: 10.1053/joca.1998.0130. [DOI] [PubMed] [Google Scholar]
- 15.Kagan AII. Rotator cuff tears of the hip. Clin Orthop. 1999;368:135–140. [PubMed] [Google Scholar]
- 16.Shbeeb MI, O'Duffy JD, Michet CJ, Jr, et al. Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol. 1996;23:2104–2106. [PubMed] [Google Scholar]
- 17.Ege Rasmussen KJ, Fano N. Trochanteric bursitis. Treatment by corticosteroid injection. Scand J Rheumatol. 1985;14:417–420. doi: 10.3109/03009748509102047. [DOI] [PubMed] [Google Scholar]


