Abstract
Background
The use of primary care services in the UK is traditionally high in deprived areas. There has been little research into the effect of deprivation on the uptake of NHS Direct, a national nurse-led health helpline.
Aim
To explore the impact of deprivation, age and sex on call rates to two NHS Direct sites.
Design of study
Ecological study.
Setting
West Yorkshire and West Midlands NHS Direct sites.
Method
Details of NHS Direct calls between July 2001 and January 2002 were linked to electoral wards and the Indices of Multiple Deprivation for 2000. Age-standardised call rates were calculated for five deprivation levels. Using a negative binomial regression model, West Yorkshire call rates were analysed by age group, sex, deprivation level and geographical location. Rates were mapped by ward for West Yorkshire NHS Direct.
Results
Six-monthly call rates were highest for children under 5 years of age (130 per 1000 population). The ratio of female to male calls (all ages) was 1.30 (95% confidence interval [CI] = 1.27 to 1.33), this ratio being highest for the 15–44 year age group (P<0.001). For both West Yorkshire and West Midlands NHS Direct, call rates (all ages combined) were highest in areas within the middle of the range of deprivation. West Yorkshire call rates about those under 5 years of age were lower in the most deprived areas than in the least deprived areas (<1 year, P = 0.06; 1–4 years, P = 0.03). For adults aged 15–64 years, call rates were significantly higher in the most deprived areas (P<0.001).
Conclusion
This work supports previous research and shows that overall demand for NHS Direct is highest in areas where deprivation is at or just above the national average. Additionally, this study suggests that the effect of extreme deprivation appears to raise adult call rates but reduce rates of calls about children.
Keywords: access to health care, age groups, socioeconomic factors, telephone hotlines
INTRODUCTION
NHS Direct is a national 24-hour health initiative that began operating in 1998.1 Since 1999, call data derived from NHS Direct have been used for the surveillance of symptoms that may be indicative of infection.2-3 These call data indicate that, although there is national coverage by NHS Direct, call rates are still a fraction (approximately 1/30th) of GP consultation rates.4-6 NHS Direct calls may therefore not be representative of the population of England and Wales.
Questionnaire studies have indicated low awareness7 and low usage8 of NHS Direct among more deprived social groups. However, low awareness does not necessarily indicate low usage, which for other primary care services tends to be high in deprived areas.4,9-11 A single, published, study, using a large sample of NHS Direct's own call data, has examined the relationship between deprivation and the use of NHS Direct,12 and challenged previous assumptions that NHS Direct is underused in deprived areas.13 Work at other NHS Direct sites has found that the distribution of NHS Direct calls by age and sex is similar to that for GP services.14-15 We aimed to build on previous work by conducting an ecological analysis of call rates at two NHS Direct sites, to assess the effect of deprivation on call rates and to additionally explore the impact of age and sex.
How this fits in
The use of primary care services in the UK is traditionally high in deprived areas. At one NHS Direct site, call rates were shown to rise with increasing deprivation before declining at severe deprivation levels. This study supports previous findings that NHS Direct call rates (all ages combined) are highest in areas with deprivation levels at, or just above, the national average. It additionally suggests that the effect of extreme deprivation appears to raise adult call rates but reduces call rates relating to children.
METHOD
The age, sex and full postcode of residence of all people making NHS Direct triage calls (calls relating to symptoms) were collected from West Yorkshire NHS Direct and West Midlands NHS Direct for the period July 2001 to January 2002. Records were excluded if the age or postcode were incomplete or missing.
To help manage demand, NHS Direct sites often redirect calls to NHS Direct sites elsewhere in the country. Calls may therefore not originate from the catchment area (based on area dialling codes) of the site that handled the call. For the purposes of our study, proxy NHS Direct catchment areas were aggregated from 1998 health authority boundaries. Calls were categorised as networked calls, and excluded from the study, if the postcode was located outside the site catchment area.
The ward level Index of Multiple Deprivation (IMD) 2000 score was used as a measure of deprivation.16 All wards in England were ranked according to their IMD score and divided into five deprivation quintiles, each quintile comprising 20% of the population of England. A higher IMD score or deprivation quintile indicates increasing deprivation. A Geographical Information System (ArcView GIS) was used to link each NHS Direct call record to a ward and hence a deprivation quintile. The 1998 mid-term population estimates for wards in England were obtained.17 For both the NHS Direct sites, 6-monthly age-standardised call rates per 1000 population (all ages) were calculated for each deprivation quintile. We also calculated the female to male call ratio for all ages (age standardised) for West Yorkshire NHS Direct.
To explore the impact of age, sex and deprivation on West Yorkshire call rates we used a negative binomial regression model, which can account for overdispersal of call rates. The numbers of calls for each ward were calculated for the following age groups: <1, 1–4, 5–14, 15–44, 45–64 and ≥65 years (males and females separately). The ward population of each age–sex category was calculated using 1991 Census population data,17 adjusted using 1998 mid-term population estimates for wards.18 Due to the imprecise nature of the West Yorkshire NHS Direct boundary, which was constructed from the boundaries of health authorities, we felt that call rates around the periphery of our catchment area could be low due to cross-boundary flows of calls. To account for this, the GIS was used to categorise each West Yorkshire ward into either an ‘edge ward’ (adjacent to the boundary, n = 24) or an ‘inner ward’ (enclosed within the edge wards, n = 102). The outcome variable for our model was call rate, with independent variables being sex, age group, deprivation quintile and edge ward. Interactions between variables were tested for significance. The negative binomial regression model was not used for West Midlands call data as the sex of the caller was missing from a substantial number of records.
Six-monthly call rates per 1000 population were mapped by ward for West Yorkshire NHS Direct.
RESULTS
There were 57 662 calls to West Yorkshire NHS Direct and 52 446 to West Midlands NHS Direct, of which 40 345 (70%) for West Yorkshire and 45 156 (86%) for West Midlands were included in the study. The majority of excluded calls were networked calls. After exclusions full postcodes were available for more than 98% of call records at both sites. The 6-monthly call rates to West Yorkshire and West Midlands NHS Direct, after exclusions, were 19.1 and 19.8 calls per 1000 population respectively.
Deprivation
Neither the West Yorkshire (population 2.2 million) nor the West Midlands NHS Direct (population 2.4 million) catchment areas conform to the national deprivation profile. These two sites have 35% and 45% of their catchment population within the most deprived 20% of the population of England (Table 1).
Table 1.
Ranges of index of multiple deprivation scores.a
| Range of scores | Deprivation quintile | Population (%) | Ratio | 95% CI |
|---|---|---|---|---|
| West Yorkshire NHS Direct | ||||
| 1.16–10.16 | 1 | 6 | 1.00 | – |
| 10.16–16.82 | 2 | 21 | 1.27 | 1.20 to 1.33 |
| 16.82–26.06 | 3 | 20 | 1.45 | 1.38 to 1.53 |
| 26.06–39.92 | 4 | 18 | 1.50 | 1.43 to 1.58 |
| 39.97–83.77 | 5 | 35 | 1.31 | 1.25 to 1.38 |
| West Midlands NHS Direct | ||||
| 1.16–10.16 | 1 | 9 | 1.00 | – |
| 10.16–16.82 | 2 | 10 | 1.31 | 1.25 to 1.37 |
| 16.82–26.06 | 3 | 13 | 1.41 | 1.36 to 1.47 |
| 26.06–39.92 | 4 | 23 | 1.40 | 1.35 to 1.45 |
| 39.97–83.77 | 5 | 45 | 1.22 | 1.18 to 1.27 |
Percentage of the population in each deprivation quintile, and call rate ratio by deprivation quintile (all ages [age standardised]). The baseline quintile is 1 (least deprived).
For both West Yorkshire and West Midlands NHS Direct, call rates (all ages combined) rose with increasing deprivation before falling in the most deprived areas (Table 1). The highest call rates were in quintiles 3 and 4 for both sites (those areas with deprivation equal or just above the national average). Call rates were significantly lower in the least deprived wards (quintile 1) than any other areas (quintiles 2 to 5).
Regression model
There were significant interactions within the model between age group and deprivation (P<0.001) and between age group and sex (P<0.001) (see below). Edge ward was not associated with these interactions and does not bias the results of this study.
Age and sex
The highest 6-monthly call rates to West Yorkshire NHS Direct were for children aged <1 year (130 calls per 1000) and between 1 and 4 years (58 per 1000) (Table 2). The ratio of female to male calls (all ages) was 1.30 (95% confidence interval [CI] = 1.27 to 1.33). Call rates about boys were higher than about girls, although this difference was not statistically significant (Table 2). Rates of calls were higher about women than for men, this difference being most pronounced for 15–44 year olds (P<0.001).
Table 2.
Proportions of calls to West Yorkshire NHS Direct.
| Age band in years | Calls (%) | 6-monthly call rate per 1000 population | Female:male (95% CI) | P-value |
|---|---|---|---|---|
| <1 | 6.6 | 130.3 | 0.93 (0.85 to 1.03) | 0.16 |
| 1–4 | 17.3 | 58.4 | 0.93 (0.86 to 1.02) | 0.10 |
| 5–14 | 11.7 | 17.3 | 0.98 (0.89 to 1.07) | 0.60 |
| 15–44 | 42.6 | 18.7 | 1.99 (1.84 to 2.15) | <0.001 |
| 45–64 | 11.8 | 10.7 | 1.57 (1.43 to 1.72) | <0.001 |
| 65 | 6.9 | 8.5 | 1.15 (1.03 to 1.28) | 0.01 |
Deprivation, age and sex
For West Yorkshire NHS Direct, call rates for the <1 year and 1–4 year age groups were lowest in the most deprived wards (<1 year, P = 0.06; 1–4 years, P = 0.03), significantly so for the 1–4 year age group (Table 3). For adults of working age (15–64 years), call rates rose with increasing deprivation and were significantly higher in the most deprived areas (quintiles 3 to 5) than in the least deprived. There was no significant variation in call rates for older people (≥65 years). The relationship between call rates and deprivation was the same for males and females as it was for both sexes combined, that is, this relationship did not differ significantly between men and women (data not shown).
Table 3.
Call rate ratios for West Yorkshire NHS Direct by age-group and deprivation quintile.a
| Quintile | Call rate ratio | 95% CI | P-value |
|---|---|---|---|
| Age group <1 years | |||
| 1 | 1.00 | ||
| 2 | 1.02 | 0.8 to 1.3 | 0.88 |
| 3 | 1.16 | 0.91 to 1.48 | 0.22 |
| 4 | 1.09 | 0.85 to 1.39 | 0.48 |
| 5 | 0.80 | 0.63 to 1.01 | 0.06 |
| Age group 1–4 years | |||
| 1 | 1.00 | ||
| 2 | 1.06 | 0.85 to 1.32 | 0.61 |
| 3 | 1.28 | 1.03 to 1.59 | 0.03 |
| 4 | 1.10 | 0.87 to 1.37 | 0.38 |
| 5 | 0.80 | 0.65 to 0.99 | 0.03 |
| Age group 5–14 years | |||
| 1 | 1.00 | ||
| 2 | 1.24 | 0.98 to 1.59 | 0.7 |
| 3 | 1.63 | 1.29 to 2.08 | <0.0001 |
| 4 | 1.61 | 1.27 to 2.06 | <0.0001 |
| 5 | 1.32 | 1.05 to 1.67 | 0.02 |
| Age group 15–44 years | |||
| 1 | 1.00 | ||
| 2 | 1.26 | 1.03 to 1.54 | 0.02 |
| 3 | 1.40 | 1.15 to 1.71 | <0.001 |
| 4 | 1.61 | 1.31 to 1.97 | <0.0001 |
| 5 | 1.56 | 1.29 to 1.89 | <0.0001 |
| Age group 45–64 years | |||
| 1 | 1.00 | ||
| 2 | 1.28 | 1.02 to 1.62 | 0.03 |
| 3 | 1.49 | 1.19 to 1.89 | <0.001 |
| 4 | 1.43 | 1.13 to 1.81 | 0.003 |
| 5 | 1.48 | 1.18 to 1.85 | <0.001 |
| Age group ≥65 years | |||
| 1 | 1.00 | ||
| 2 | 1.07 | 0.83 to 1.37 | 0.60 |
| 3 | 1.12 | 0.87 to 1.43 | 0.38 |
| 4 | 1.16 | 0.91 to 1.5 | 0.23 |
| 5 | 0.97 | 0.76 to 1.23 | 0.78 |
The baseline quintile is quintile 1 (least deprived).
Location
Call rates for edge wards (the periphery of the West Yorkshire catchment area) were 5.1% lower than for inner wards, but this difference was not significant (ratio of edge to inner wards = 0.95, 95% CI = 0.90 to 1.00). Six-monthly call rates for West Yorkshire wards varied between 11.3 and 42.4 per 1000 population (median = 24) and were highest in and around the Halifax and Huddersfield urban areas and south of Leeds (Figure 1).
Figure 1.
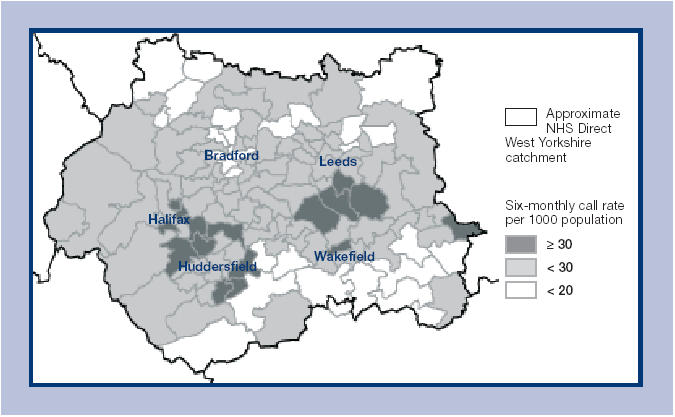
Map of 6-monthly call rates per 1000 population by ward for West Yorkshire NHS Direct.
DISCUSSION
Summary of main findings
The impact of deprivation on NHS Direct call rates in West Yorkshire differs between age groups. The effect of extreme deprivation appears to raise adult call rates but reduce rates of calls about children. When considering total demand for the service (all ages), call rates to West Midlands and West Yorkshire NHS Direct were highest in areas with deprivation levels at or just above the national average. The relationship between call rates and deprivation was the same for males, females and both sexes combined.
Strengths and limitations of this study
This study has used adjusted population data to calculate call rates. Population data and deprivation indices generated from the 2001 Census will improve the accuracy of this type of study in the future. Some bias may have occurred as a result of not including calls made within our two NHS Direct site catchment areas but networked elsewhere in England. This bias is considered minimal, as calls are not networked on the basis of age or relative location within a site boundary. The use of a national call database, from which calls can be extracted by postcode, could resolve this problem. The non-inclusion of networked calls also means our analysis will show an underestimation of the true call rates. This study was able to eliminate any bias caused by the imprecise nature of our NHS Direct site boundary (‘edge effects’) by distinguishing between inner and edge wards. Finally, the local distribution of primary care services, other than NHS Direct, may explain some of the fourfold variation in call rates between wards in West Yorkshire. Although methodologically difficult, we recommend that proximity to other health services, as well as the ethnic composition of the catchment areas, should be taken into account when analysing call rates for further studies. This could help clarify how existing health services, as well as social factors, have influenced the relative uptake of NHS Direct.
Comparison with existing literature
These call data support previous work,15,19 in that the distribution of calls by age and sex is comparable to that for GP services,4-5,9-10 apart from the low call rate from those over 65 years. What is more interesting is how the effect of deprivation on NHS Direct call rates is different from its effect on the use of other primary care services. Previous work has demonstrated high GP consultation rates for adults4 and children from low social classes,9 and high demand for out-of-hours contact with doctors in deprived areas.10-11 Conversely, the pattern of NHS Direct call rates at three NHS Direct sites (West Midlands, West Yorkshire and southeast London in a previous study)12 indicates a drop in call rates between average and severely deprived areas. The analysis of West Yorkshire call data also shows that this drop does not occur for all age groups. Call rates about young children were lowest in deprived areas, whereas call rates about adults were generally highest in deprived areas. The distribution of local health services, behavioural factors, and some bias due to the ecological fallacy20 could explain this.
Implications for further research
The IMD score is an index that was produced recently and has been used as a proxy for deprivation on an individual level, as opposed to the more commonly used Jarman index21 and Townsend score,22 which are based on 1991 Census data. The IMD score is timely, as it comprises 1991 Census data as well as government socioeconomic data from the late 1990s. The use of national IMD quintiles in this study, rather than site specific quintiles, has helped to establish some baseline data for comparison with similar work at other NHS Direct sites.
In this study we analysed calls from people with symptoms, whereas one fifth of NHS Direct calls are from people who are not reporting symptoms but seeking health information. We are unsure how call rates for health information vary by age, sex and local deprivation. Two sites with predominantly urban populations were studied here and further research is required to examine whether NHS Direct has been successful in reaching rural communities. Provisional analysis of call data from one site (Midlands Shires NHS Direct) suggests call rates are significantly lower in rural areas than in urban areas (D Cooper, unpublished data, 2002).
NHS Direct call profiles, as presented here, will be most useful if regular updates are produced. They may then be of use to NHS Direct so that they can assess demand for the service and evaluate the success of promotional activities. Analysis of national call data should now be undertaken to determine whether call rates about children in deprived areas are also low in other parts of the country.
This work supports previous research by showing that NHS Direct call rates are highest in areas where deprivation levels are at, or just above, the national average.12 This study also suggests that the effect of extreme deprivation appears to raise adult call rates but reduce rates of calls about children. Work is needed to examine whether this relationship exists across the country and on an individual level. The significant local variations in call rates demonstrated here (by age, sex and deprivation) should be considered by NHS Direct when developing the service, and by public health staff when using call data for health protection and surveillance purposes.3
Acknowledgments
We thank West Midlands NHS Direct and West Yorkshire NHS Direct for contributing call data to this study. We thank Ralph Smith for his help with the GIS aspects of this work and Babatunde Olowokure and James Munro for their comments on earlier drafts of this paper.
Ethics committee
West Midlands Multicentre Research Ethics Committee
Competing interests
None
REFERENCES
- 1.NHS Direct online. http://www.nhsdirect.nhs.uk/ (accessed 18 Feb 2005)
- 2.Cooper DL, Smith GE, Hollyoak VA, et al. Use of NHS Direct calls for the surveillance of influenza – a second year's experience. Commun Dis Public Health. 2002;5(2):127–131. [PubMed] [Google Scholar]
- 3.Baker M, Smith GE, Cooper DL, et al. Early warning and NHS Direct: a role in community surveillance? J Public Health Med. 2004;25:362–368. doi: 10.1093/pubmed/fdg096. [DOI] [PubMed] [Google Scholar]
- 4.Royal College of General Practitioners, Office of Population, Censuses and Surveys, and Department of Health. Morbidity statistics from general practice: fourth national study, 1991–1992. London: OPCS; 1995. http://www.statistics.gov.uk/downloads/theme_health/MB5No3.pdf (accessed 18 Feb 2005) [Google Scholar]
- 5.Rowlands S, Moser K. Consultation rates from the general practice research database. Br J Gen Pract. 2002;52:658–660. [PMC free article] [PubMed] [Google Scholar]
- 6.Directorate of Access and Choice. Developing NHS Direct: a strategy document for the next 3 years. London: Department of Health; 2003. http://www.publications.doh.gov.uk/developingnhsdirect/developingnhsdirect-apr03.pdf (accessed 18 Feb 2005) [Google Scholar]
- 7.The Comptroller and Auditor General. NHS Direct in England. London: National Audit Office; 2002. http://www.nao.org.uk/publications/nao_reports/01-02/0102505.pdf (accessed 18 Feb 2005) [Google Scholar]
- 8.Ring F, Jones M. NHS Direct usage in a GP population of children under 5 years: is NHS Direct used by people with the greatest health need? Br J Gen Pract. 2004;54:211–213. [PMC free article] [PubMed] [Google Scholar]
- 9.Saxena S, Majeed A, Jones M. Socioeconomic differences in childhood consultation rates in general practice in England and Wales: prospective cohort study. BMJ. 1999;318:642–646. doi: 10.1136/bmj.318.7184.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salisbury C, Trivella M, Bruster S. Demand for and supply of out of hours care from general practitioners in England and Scotland: observational study based on routinely collected data. BMJ. 2000;320:618–621. doi: 10.1136/bmj.320.7235.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carlisle R, Groom LM, Avery AJ, et al. Relation of out of hours activity by general practice and accident and emergency services with deprivation in Nottingham: longitudinal survey. BMJ. 1998;316:520–523. doi: 10.1136/bmj.316.7130.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burt J, Hooper R, Jessopp L. The relationship between the use of NHS Direct and deprivation in southeast London: an ecological analysis. J Public Health Med. 2003;25:174–176. doi: 10.1093/pubmed/fdg038. [DOI] [PubMed] [Google Scholar]
- 13.George S. NHS Direct audited. BMJ. 2002;324:558–559. doi: 10.1136/bmj.324.7337.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munro J, Nicholl JP, O'Cathain A, Knowles E. Evaluation of NHS Direct first wave sites: first interim report to the Department of Health. Sheffield: Medical Care Research Unit; 1999. [Google Scholar]
- 15.Munro J, Nicholl JP, O'Cathain A, Knowles E. Evaluation of NHS Direct first wave sites: second interim report to the Department of Health. Sheffield: Medical Care Research Unit; 2000. [Google Scholar]
- 16.Department of Environment, Transport and the Regions. London: DETR; 2000. ‘Indices of Deprivation.’ Regeneration Research Summary No. 37. http://www.casa.ucl.ac.uk/2003/imd2000.pdf (accessed 18 Feb 2005) [Google Scholar]
- 17.Census Dissemination Unit. The 1991 Census datasets. http://census.ac.uk/cdu/datasets (accessed 7 March 2005)
- 18.Penhale B, Noble M, Smith G, Wright G. Final consultation on ward level population estimates. Oxford: Social Disadvantage Research Group; 1999. http://www.odpm.gov.uk/stellent/groups/odpm_urbanpolicy/documents/page/odpm_urbpol_608095.pdf (accessed 18 Feb 2005) [Google Scholar]
- 19.Payne F, Jessopp L. NHS Direct: review of activity data for the first year of operation at one site. J Public Health Med. 2001;23:155–158. doi: 10.1093/pubmed/23.2.155. [DOI] [PubMed] [Google Scholar]
- 20.Robinson WR. Ecological correlations and the behaviour of individuals. American Sociological Review. 1950;15:351–557. [Google Scholar]
- 21.Jarman B. Identification of under-privileged areas. BMJ. 1983;286:1705–1709. doi: 10.1136/bmj.286.6379.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Townsend P. Poverty in the UK. London: Penguin; 1979. [Google Scholar]


