Abstract
Background
Motivational Interviewing is a well-known, scientifically tested method of counselling clients developed by Miller and Rollnick and viewed as a useful intervention strategy in the treatment of lifestyle problems and disease.
Aim
To evaluate the effectiveness of motivational interviewing in different areas of disease and to identify factors shaping outcomes.
Design of study
A systematic review and meta-analysis of randomised controlled trials using motivational interviewing as the intervention.
Method
After selection criteria a systematic literature search in 16 databases produced 72 randomised controlled trials the first of which was published in 1991. A quality assessment was made with a validated scale. A meta-analysis was performed as a generic inverse variance meta-analysis.
Results
Meta-analysis showed a significant effect (95% confidence interval) for motivational interviewing for combined effect estimates for body mass index, total blood cholesterol, systolic blood pressure, blood alcohol concentration and standard ethanol content, while combined effect estimates for cigarettes per day and for HbA1c were not significant. Motivational interviewing had a significant and clinically relevant effect in approximately three out of four studies, with an equal effect on physiological (72%) and psychological (75%) diseases. Psychologists and physicians obtained an effect in approximately 80% of the studies, while other healthcare providers obtained an effect in 46% of the studies. When using motivational interviewing in brief encounters of 15 minutes, 64% of the studies showed an effect. More than one encounter with the patient ensures the effectiveness of motivational interviewing.
Conclusion
Motivational interviewing in a scientific setting outperforms traditional advice giving in the treatment of a broad range of behavioural problems and diseases. Large-scale studies are now needed to prove that motivational interviewing can be implemented into daily clinical work in primary and secondary health care.
Keywords: body mass index; interview, psychological; meta-analysis; motivation; randomised controlled trials; review, systematic
INTRODUCTION
The concept of motivational interviewing evolved from the experience of treating alcoholism, and was first described by Miller in 1983.1 This basic experience was developed into a coherent theory, and a detailed description of the clinical procedure was provided by Miller and Rollnick,2 who defined motivational interviewing as a ‘directive, client-centred counselling style for eliciting behaviour change by helping clients to explore and resolve ambivalence’. Miller and Rollnick's theory also draws inspiration from Carl Rogers' work on non-directive counselling, described in 1953.3 The examination and resolution of ambivalence is the central purpose of non-directive counselling, and the counsellor is intentionally directive in pursuing this goal. Motivational interviewing is a particular way of helping clients recognise and do something about their current or potential problems. It is viewed as being particularly useful for clients who are reluctant to change or who are ambivalent about changing their behaviour. The strategies of motivational interviewing are more persuasive than coercive, more supportive than argumentative, and the overall goal is to increase the client's intrinsic motivation so that change arises from within rather than being imposed from without.4 The spirit of motivational interviewing is captured in the key points Box 1 (Supplementary Box 1 is an extended version of this box).
Box 1. Characteristics of the motivational interviewing.2.
-
▸
‘Motivational interviewing’ relies upon identifying and mobilising the client's intrinsic values and goals to stimulate behaviour change.
-
▸
Motivation to change is elicited from the client and not imposed from without.
-
▸
Motivational interviewing is designed to elicit, clarify, and resolve ambivalence and to perceive benefits and costs associated with it.
-
▸
Readiness to change is not a client trait, but a fluctuating product of interpersonal interaction.
-
▸
Resistance and ‘denial’ is often a signal to modify motivational strategies.
-
▸
Eliciting and reinforcing the client's belief in ability to carry out and succeed in achieving a specific goal is essential.
-
▸
The therapeutic relationship is a partnership with respect of client autonomy.
-
▸
Motivational interviewing is both a set of techniques and counselling style.
-
▸
Motivational interviewing is directive and client-centred counselling understanding and eliciting behaviour change.
Motivational interviewing is broadly applicable in the management of diseases that to some extent are associated with behaviour.5-77 It has been used and evaluated in relation to alcohol abuse, drug addiction, smoking cessation, weight loss, adherence to treatment and follow-up, increasing physical activity, and in the treatment of asthma and diabetes. Motivational interviewing has been used by various healthcare providers, including, psychologists, doctors, nurses and midwives. This aim of this review is to provide an overview of the areas in which motivational interviewing has been applied, to evaluate its effectiveness as an intervention tool in randomised controlled clinical trials and to identify factors shaping outcomes in the areas reviewed.
How this fits in
Motivational interviewing is a well known, scientifically tested method of counselling clients and is viewed as a useful intervention strategy in the treatment of lifestyle problems and disease. A systematic review and meta-analysis of randomised controlled trials shows that motivational interviewing in a scientific setting outperforms traditional advice giving in the treatment of a broad range of behavioural problems and diseases. Large-scale studies are now needed to prove that it can be implemented into daily clinical work in primary and secondary health care.
METHOD
Search strategy
The following electronic libraries were searched according to the Cochrane Collaboration's search strategy for randomised controlled trials for each database: the Cochrane Central Register of Controlled Trials on the Cochrane Library (issue 4, 2002); Medline (1966 to January 2004); EMBASE (January 1974 to January 2004); and PsycINFO, including PsychLIT (1967 to January 2004), CancerLit (1966 to January 2004), ScienceDirect/ISI, including SciSearch and Social SciSearch (1972 to January 2004), Sociological Abstracts (1963 to January 2004), Social Services Abstracts (1980 to January 2004), Ebsco research databases (1980 to January 2004), CSA/EconLit index (1969 to January 2004), CSA Biological Sciences (1982 to January 2004), Biological Abstracts (1969 to January 2004), AIDS & Cancer Research Abstracts (1982 to January 2004), AskERIC (1966 to January 2004), BIOSIS Previews (1969 to January 2004), ABI-INFORM (1971 to January 2004). The following search terms were used for Medline and adapted for all of the other databases: ‘motivational interviewing’, ‘motivational behaviour’, ‘behaviour/motivational interviewing’, ‘behaviour change’, ‘motivational change’ and ‘behaviour change/motivational interviewing’. The proceedings of conferences during 1997 to 2004 on diabetes held by the American Diabetes Association, Diabetes UK (formerly British Diabetic Association), the European Association for the Study of Diabetes, and the International Diabetes Federation were searched under psychological, educational, or behavioural headings for reports of any trials using motivational interviewing. The reference lists of included studies and reviews were searched for additional studies. If an included trial did not supply sufficient data needed for the meta-analysis, we tried to obtain data by approaching the authors and at the same time asking for data from unpublished trials. Figure 1 shows the progress of randomised controlled trials through the review.
Figure 1.
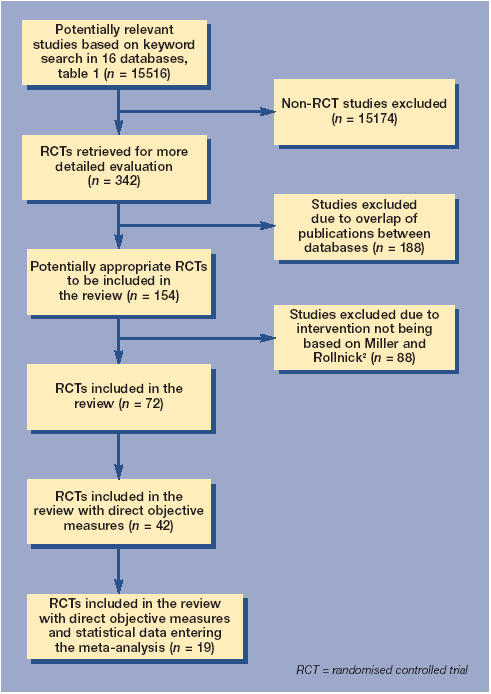
Flowchart of progress of randomised controlled trials through the review.
Selection
Figure 2 shows a funnel plot (for more information on funnel plots see reference 78). Randomised controlled trials included in the review were those using motivational interviewing as defined according to Miller and Rollnick as an intervention,4 regardless of the context of client counselling. Those randomised controlled trials in which there was no or minimal description of the methods of motivational interviewing and the modes of delivery were excluded. Studies were only included where traditional advice giving was used to help and advise clients and served as a control. ‘Traditional advice giving’ is used as an expression for a GP-centred approach: that is, the GP defines the patients' problem from a biomedical perspective and does not include the patient perspective on the matter, thus giving advice accordingly.
Figure 2.
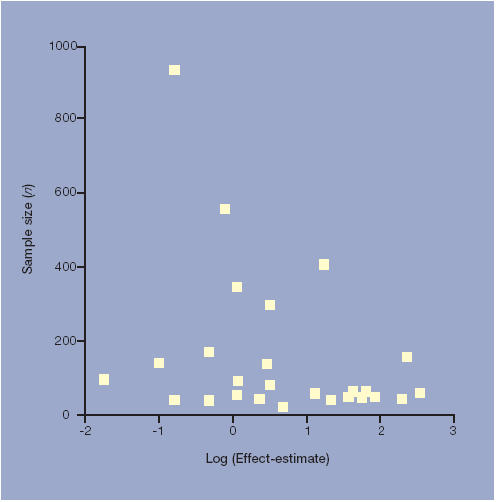
Funnel plot of randomised controlled trials using motivational interviewing as intervention.
Qualitative data synthesis
Quality assessment of each of the resulting 72 randomised controlled trials was carried out with a validated scale79,80 and individual components known to affect estimates of intervention efficacy.81 The scale consisted of three items pertaining to description of randomisation, masking, dropouts and withdrawals in the reporting of a randomised controlled trial, and ranged from 0 to 5, with higher scores indicating better reporting. The individual components assessed the adequacy of reporting of randomisation, allocation concealment and double blinding. High-quality trials scored a minimum of 2 out of 5.81
Validity assessment and data extraction
The abstracts of studies identified by electronic searches were assessed by one author and extracted onto a data extraction form. Confirmation of outcome measures and clinically relevant goals was assessed by all the authors. All studies were examined to assess the clinical relevance of their goals and outcome measures to client treatment; for example, HbA1c as an outcome measure and the study goal as a 1% reduction in HbA1c. Supplementary Table 1 shows objective outcome measures, together with assessment of clinical relevance and statistically significant effects in the studies. Furthermore, for a study to be classified as showing an effect, the recorded effect had to be statistically significant. When a study is classified as demonstrating an effect, it therefore has both a statistically significant effect and a clinically relevant effect to client treatment.
Quantitative data synthesis
Statistical data analysis was conducted using SPSS version 11.0 software. The information extracted from the included trials was described and summarised. The meta-analysis was carried out using Excell 2003 and STATA version 8 software. The meta-analysis conforms to the Cochrane Reviewers' Handbook.78 The meta-analysis was performed as a generic inverse variance meta-analysis, in which we assumed homogeneity between study estimates. The assumption of homogeneity is based on the confidence intervals for the study estimates having large overlaps, which indicates homogeneity.78 The meta-analysis calculates combined estimates of effect with standard error and 95% confidence intervals. The meta-analysis is based on the randomised controlled trials that included objective measures and submitted statistical data.
Study characteristics
The variables extracted for analysis are shown in Box 2.
Box 2. Variables extracted for analysis.
Characteristics of the intervention
-
▸
Ways of delivery (general practice, outpatient clinic, home and telephone)
-
▸
Duration of intervention (time used in one counsellor–client encounter)
-
▸
Number of intervention encounters (counselling encounter)
-
▸
Practising counsellor (psychologist, doctor, nurse or midwife)
Design of study (study group and follow-up)
-
▸
Number of participants
-
▸
Follow-up period
-
▸
Inclusion criteria (population and selection)
Area of intervention
-
▸
Adherence to treatment of diseases
-
▸
Adherence to life style changes
Outcome measures
-
▸
Direct indicators (health outcome; for example, blood glucose, blood cholesterol; utilisation of healthcare services; for example, length of hospital stay)
-
▸
Indirect indicators (subjective report, self-assessment, questionnaires)
RESULTS
Trial flow
Details of the systematic review of randomised controlled trials are shown in Figure 1.
Quantitative data synthesis
A systematic literature search produced 72 randomised controlled studies assessing the effectiveness of motivational interviewing in client counselling, the first published in 1991. A summary of the results is shown in Table 1. Publication bias is non-significant (Figure 2).78
Table 1.
Study data (n = 72).
| Effect | ||
|---|---|---|
| Ways of delivery and duration of encounter in minutes (n = 70)a | Yes | No |
| Individual interview, 10–20 | 7 | 4 |
| Individual interview, 30–45 | 12 | 5 |
| Individual interview, 60 | 26 | 6 |
| Individual interview, 60–120 | 4 | 2 |
| Group interviewb | 3 | 0 |
| Telephone interviewb | 0 | 1 |
| Number of encounters (n = 71)c | Yes | No |
| 1 | 10 | 15 |
| 2 | 12 | 0 |
| 3 | 5 | 1 |
| 4 | 8 | 2 |
| 5 | 3 | 0 |
| >5 | 13 | 2 |
| Counsellor profession (n = 76)d | Yes | No |
| Psychologist | 33 | 9 |
| Doctor | 19 | 4 |
| Other health care provider (nurse, midwife, dietician) | 5 | 6 |
| Intervention period in months (n = 71)e | Yes | No |
| <3 | 4 | 11 |
| 3–5 | 8 | 3 |
| 6–11 | 10 | 3 |
| 12 | 16 | 3 |
| 12–24 | 5 | 3 |
| >24 | 5 | 0 |
| Measuring method (n = 116)f | Yes | No |
| Direct biological/clinical measures (e.g. HbA1c) | 25 | 8 |
| Direct utilisation of healthcare services (e.g. number of encounters) | 8 | 3 |
| Indirect measures (e.g. questionnaire) | 53 | 19 |
| Area of intervention (n = 72) | Yes | No |
| Diabetes/asthma | 2 | 1 |
| Smoking cessation | 8 | 4 |
| Weight-loss/physical activity | 8 | 2 |
| Alcohol abuse | 23 | 5 |
| Psychiatrics/addiction | 12 | 7 |
Two studies only described the intervention as an individual interview without describing an accurate length of the interview.
The length of the group and telephone interviews was not described in the articles.
One study only described the intervention as an individual interview without describing the number of counselling encounters.
Five studies involved encounters with several counsellors of different educational background, which is why the total number exceeds the total number of studies.
Study did not describe the follow-up period.
In some studies both direct and indirect measures were used, which is why the total number exceeds the total number of studies.
The meta-analysis shows a significant effect (95% CI) of motivational interviewing for combined effect estimates for body mass index, total blood cholesterol, systolic blood pressure, blood alcohol concentration and standard ethanol content (as opposed to concentration), while combined effect estimates for cigarettes per day and for HbA1c are non-significant (Table 2 [Supplementary Table 2 is an extended version of this table]).
Table 2.
Meta-analysis, the motivational interviewing effect.
| Effect measure | n | Combined effect estimate | P-value (95% CI) |
|---|---|---|---|
| Body mass index | 1140 | 0.72 | 0.0001 (0.33 to 1.11) |
| HbA1c (%GHb) | 243 | 0.43 | 0.155 (−0.16 to 1.01) |
| Total blood cholesterol (mmol/l) | 1358 | 0.27 | 0.0001 (0.20 to 0.34) |
| Systolic blood pressure (mmHg) | 316 | 4.22 | 0.038 (0.23 to 8.99) |
| Number of cigarettes/day | 190 | 1.32 | 0.099 (−0.25 to 2.88) |
| Blood alcohol content (mg%) | 278 | 72.92 | 0.0001 (46.80 to 99.04) |
| Standard ethanol content (units) | 648 | 14.64 | 0.0001 (13.73 to 15.55) |
Qualitative data synthesis
Quality assessment was made with a validated scale ranging from 0 to 5 and high-quality trials scored a minimum of 2 out of a maximum possible score of 5. Out of 72 randomised controlled trials, 50 were assessed at 3 points, 21 at 2 points and one at 1 point.
Study characteristics
An effect of motivational interviewing was demonstrated in 74% (53/72) of the randomised controlled trials. None of the publications reported any adverse effects of motivational interviewing, nor did they explicitly aim to report this. No studies showed motivational interviewing to be harmful or to have any kind of adverse effects. A total of 94% (68/72) of the randomised controlled trials used individual interviews. Of the remaining four studies, three used group therapy and one study used a telephone interview, but these showed no effect. The median duration in all the studies of an individual counselling encounter was estimated to be 60 minutes (range = 10–120 minutes). Among the studies using encounters of 60 minutes, 81% (26/32) showed an effect. Out of 11 studies using less than 20 minutes per encounter 64% (7/11) showed an effect. The likelihood of an effect rose with the number of encounters. Therefore, an effect was demonstrated in 40% (10/25) of studies with one counselling session, but 87% (13/15) of studies with more than five encounters. The studies had an estimated median follow-up period of 12 months (range 2 months to 4 years). A prolonged follow-up period increased the percentage of studies showing an effect. Therefore, 36% (4/11) of studies with a 3-month follow-up period ascertained an effect compared with 81% (26/32) of studies allowing a 12-month or longer follow-up period.
Healthcare providers who acted as counsellors included: psychologists (55% [42/76]); medical doctors (30% [23/76]); and others such as nurses, midwives and dieticians (15% [1/76]. Medical doctors obtained an effect from motivational interviewing in 83% (19/23) of the studies, while psychologists obtained an effect in 79% (33/42) of the studies. Other healthcare providers obtained an effect in 46% (5/11) of the studies.
Intervention targeted alcohol abuse, psychiatric diagnoses, and different aspects of addiction in 47 out of the 72 studies, and motivational interviewing outperformed traditional advice giving in 75% (35/47) of these studies. Motivational interviewing targeted physiological problems, such as weight loss, lowering of lipid levels, increasing physical activity, diabetes, asthma and smoking cessation in 25 of 72 studies and had an effect in 72% (18/25) of them. Smoking cessation studies alone reported an effect in 67% (8/12) of the studies, whereas studies involving the treatment of diabetes, asthma, and weight-related problems reported an effect in 77% (10/13). All studies used indirect measures; for example, questionnaires. Forty-six per cent (33/72) also used direct effect measures: health outcome, direct/indirect indicators and utilisation of healthcare services. An effect of motivational interviewing was obtained in 75% of the studies elicited in terms of direct measures (33/44) and in 74% of the studies elicited in terms of indirect outcome measures (53/72).
DISCUSSION
Summary of main findings
This review documents that motivational interviewing in a scientific setting effectively helps clients change their behaviour and that it outperforms traditional advice giving in approximately 80% of the studies. No studies have reported motivational interviewing to be harmful or to have any kind of adverse effect; however, no study did explicitly aim to report this.
The meta-analysis shows significant effects of motivational interviewing for combined effect estimates of body mass index, total blood cholesterol, systolic blood pressure, blood alcohol concentration and standard ethanol content (Table 2). In particular, the magnitude of the decrease of body mass index, systolic blood pressure, blood alcohol concentration and standard ethanol content is of clinical relevance and implies that motivational interviewing can and should be used. The significant decrease for the combined effect estimate of total blood cholesterol is of less clinical importance. However, viewing an effect as clinically important or not, it is imperative to keep in mind that motivational interviewing is based on making the patients themselves aware of the potential for change in behaviour resulting in improved health parameters, which means that small changes may also be of interest if they mark the beginning of a changing process for the patient. The nature of changes in the patient is almost always related to both adherence to prescribed medication and to the type of changes the patient makes in their lifestyle. However, the effect of motivational interviewing in some problem areas; for example, weight loss and smoking cessation, is primarily brought about through a change in personal habits, whereas the effect on asthma primarily comes from adherence to prescribed medication. This meta-analysis provides evidence of the significant effect of motivational interviewing on many different areas of intervention.
The review has shown that motivational interviewing can be effective even in brief encounters of only 15 minutes and that more than one encounter with a patient increases the likelihood of effect.5,6,14,16,36,37,41,42,45
This review sheds new light on the assumption that the effectiveness of motivational interviewing depends upon the counsellor's profession. The effect was not related to the counsellor's educational background as medical doctor or psychologist. Therefore, there was no statistically significant difference in the percentage of studies obtaining an effect from motivational interviewing, whether it was performed by psychologists, psychiatrists, physicians or GPs. Use of motivational interviewing probably depends on other aspects such as duration and number of client–counsellor encounters. However, it would be reasonable to speculate that aspects such as training and experience of motivational interviewing methods and client–counsellor relationships also influence the effectiveness, even if this cannot be shown in this review. Five studies involved other health workers as counsellors; for example, nurses, midwives and dieticians, and another six studies partly involved other health workers in the counselling encounter. Only five of these 11 studies found motivational interviewing to be effective.8,9,13,14,19,22,24,30,57,65,67 This may to some extent be explained by the design of these studies, as most of them reported on the effect of only one encounter, they had follow-up periods shorter than 3 months, and they began with difficult subjects such as HIV-positive drug misusers who were making changes to their lifestyle.
Strength and limitations of this study
Publication bias is a well-known problem. However, a funnel plot (Figure 2) of all the studies within the research area of motivational interviewing indicates publication bias to be non-significant. Furthermore, a methodological quality rating79-81 shows that, except for one study, all the randomised controlled trials in this review have a high methodological quality. All studies in the meta-analysis demonstrate a positive effect or tendency, although not all studies show a significant effect of motivational interviewing. However, the meta-analysis was only performed on the 19 studies (out of 42) that stated objective measures and statistical data needed for the meta-analysis in the article or delivered these data afterwards on request. Of the remaining 23 studies, 17 concluded that there was a significant effect of motivational interviewing and 6 showed a non-significant effect (Supplementary Table 1). These remaining studies did not deliver the statistical data needed for meta-analysis either in the article or afterwards. However, in view of the fact that a vast majority (33/42) of the randomised controlled trials with objective measures concluded that there was a significant effect of motivational interviewing, we believe a potential selection bias to be non-significant and the results of the meta-analysis to be valid.
Implications for future research
This review underscores the crucial importance of the motivational interviewing setting and study design for obtaining an effect. A follow-up period shorter than 3 months increases the risk of counselling failure, probably due to lack of intervention.13,19,20,24,26,32,60
Another important aspect was the use of indirect measures versus direct measures. This review showed that an effect of motivational interviewing can be demonstrated by indirect measures such as questionnaires, but also by direct objective measures such as blood pressure, blood glucose, weight and length of hospital stay. When it is possible to measure effect by epidemiological as well as clinical direct measures and to capture effect by clinical endpoints, this should be done to ensure the reliability of the results. The optimal design would match the specificity and reliability of direct measures with the in-depth qualitative perspective of indirect measures; for example, using questionnaires. Furthermore, in the optimal design it is imperative that an effort is made in future studies to describe precisely how motivational interviewing education is performed and how to use the methods in client counselling, allowing us all to learn more about how to increase and maximise its effect.
Implications for clinical practice
This review shows that motivational interviewing has been used in the treatment of various lifestyle problems and diseases, psychological as well as physiological. The review shows that approximately 75% of the studies do obtain an effect, regardless of whether the problems are psychological or physiological, which is supported by the meta-analysis. We can therefore argue that motivational interviewing is not limited in any way to counselling of a small group of selected clients, but can be used in the treatment of a broader area of diseases that to some extent are influenced by behaviour. When viewed in combination with the fact that there are no apparent harmful effects or adverse effects of motivational interviewing, it suggests that this is a method with an important potential effect, from which patients very well may benefit.
The review and meta-analysis leads to the conclusion that motivational interviewing in a scientific setting outperforms traditional advice giving in the treatment of a broad range of behavioural problems and diseases. However, evaluation of exact methods of motivational interviewing in a clinical setting is lacking. We now need large-scale studies of randomised controlled trials and qualitative studies on how to implement the methods of motivational interviewing to prove that it can be implemented into daily clinical work for healthcare providers and yield effects for the benefit of patients.
Supplementary Material
Acknowledgments
Thanks to Professor Carl Erik Mabeck for sharing his profound knowledge on the area of motivational interviewing and for all his support in writing this review. Thanks also Morten Frydenberg, Associate Professor at the Department of Biostatistics, Aarhus University, for his statistical advice.
Additional information
A reference to this paper was reported in URBAN of 21 September 2004. The authors and editor have agreed that the extent of the report does not amount to prior publication of data.
Supplementary information
Additional information accompanies this article at: http://www.rcgp.org.uk/journal/index.asp
Funding body
This work was funded by the Danish Research Foundation for General Practice
Competing interests
None
REFERENCES
- 1.Miller WR. Motivational interviewing with problem drinkers. Behavioural Psychotherapy. 1983;11:147–172. [Google Scholar]
- 2.Miller WR, Rollnick S. Motivational interviewing, preparing people to change addictive behavior. New York: The Guildford Press; 1991. [Google Scholar]
- 3.Rogers CR. Client-centred therapy. Its current practice, implications, and theory. Boston: Houghton Mifflin; 1951. [Google Scholar]
- 4.Miller WR, Rollnick S. Motivational interviewing, preparing people to change addictive behavior. New York: The Guildford Press; 2002. [Google Scholar]
- 5.Anderson RM, Funnell MM, Butler PM, et al. Patient empowerment. Results of a randomised controlled trial. Diabetes Care. 1995;18:943–949. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 6.Chick J. Early intervention for hazardous drinking in the general hospital. Alcohol Alcohol Suppl. 1991;1:477–479. [PubMed] [Google Scholar]
- 7.Sanchez-Craig M, Davila R, Cooper G. A self-help approach for high-risk drinking: effect of an initial assessment. J Consult Clin Psychol. 1996;64:694–700. doi: 10.1037//0022-006x.64.4.694. [DOI] [PubMed] [Google Scholar]
- 8.Baker A, Kochan N, Dixon J, et al. Controlled evaluation of a brief intervention for HIV prevention among injecting drug users not in treatment. AIDS Care. 1994;6:559–570. doi: 10.1080/09540129408258670. [DOI] [PubMed] [Google Scholar]
- 9.Baker A, Heather N, Wodak A, et al. Evaluation of a cognitive-behavioural intervention for HIV prevention among injecting drug users. AIDS. 1993;7:247–256. doi: 10.1097/00002030-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Handmaker NS, Miller WR, Manicke M. Findings of a pilot study of motivational interviewing with pregnant drinkers. J Stud Alcohol. 1999;60:285–287. doi: 10.15288/jsa.1999.60.285. [DOI] [PubMed] [Google Scholar]
- 11.Colby SM, Monti PM, Barnett NP, et al. Brief motivational interviewing in a hospital setting for adolescent smoking: a preliminary study. J Consult Clin Psychol. 1998;66:574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- 12.Beresford SA, Curry SJ, Kristal AR, et al. A dietary intervention in primary care practice: the Eating Patterns Study. Am J Public Health. 1997;87:610–616. doi: 10.2105/ajph.87.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 14.Berg-Smith SM, Stevens VJ, Brown KM, et al. A brief motivational intervention to improve dietary adherence in adolescents. The Dietary Intervention Study in Children (DISC) Research Group. Health Educ Res. 1999;14:399–410. doi: 10.1093/her/14.3.399. [DOI] [PubMed] [Google Scholar]
- 15.Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. J Nerv Ment Dis. 1999;187:630–635. doi: 10.1097/00005053-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Harland J, White M, Drinkwater C, et al. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ. 1999;319:828–832. doi: 10.1136/bmj.319.7213.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stotts AL, Schmitz JM, Rhoades HM, Grabowski J. Motivational interviewing with cocaine-dependent patients: a pilot study. J Consult Clin Psychol. 2001;69:858–862. doi: 10.1037//0022-006x.69.5.858. [DOI] [PubMed] [Google Scholar]
- 18.Baker A, Boggs TG, Lewin TJ. Randomised controlled trial of brief cognitive-behavioural interventions among regular users of amphetamine. Addiction. 2001;96:1279–1287. doi: 10.1046/j.1360-0443.2001.96912797.x. [DOI] [PubMed] [Google Scholar]
- 19.Tappin DM, Lumsden MA, McIntyre D, et al. A pilot study to establish a randomised trial methodology to test the efficacy of a behavioural intervention. Health Educ Res. 2000;15:491–502. doi: 10.1093/her/15.4.491. [DOI] [PubMed] [Google Scholar]
- 20.Kuchipudi V, Hobein K, Flickinger A, Iber FL. Failure of a 2-hour motivational intervention to alter recurrent drinking behavior in alcoholics with gastrointestinal disease. J Stud Alcohol. 1990;51:356–360. doi: 10.15288/jsa.1990.51.356. [DOI] [PubMed] [Google Scholar]
- 21.Carroll KM, Libby B, Sheehan J, Hyland N. Motivational interviewing to enhance treatment initiation in substance abusers: an effectiveness study. Am J Addict. 2001;10:335–339. doi: 10.1080/aja.10.4.335.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emmons KM, Hammond SK, Fava JL, et al. A randomised trial to reduce passive smoke exposure in low-income households with young children. Pediatrics. 2001;108:18–24. doi: 10.1542/peds.108.1.18. [DOI] [PubMed] [Google Scholar]
- 23.Kelly AB, Halford WK, Young RM. Maritally distressed women with alcohol problems: the impact of a short-term alcohol-focused intervention on drinking behaviour and marital satisfaction. Addiction. 2000;95:1537–1549. doi: 10.1046/j.1360-0443.2000.951015378.x. [DOI] [PubMed] [Google Scholar]
- 24.Ershoff DH, Quinn VP, Boyd NR, et al. The Kaiser Permanente prenatal smoking-cessation trial: when more isn't better, what is enough? Am J Prev Med. 1999;17:161–168. doi: 10.1016/s0749-3797(99)00071-9. [DOI] [PubMed] [Google Scholar]
- 25.Longshore D, Grills C, Annon K. Effects of a culturally congruent intervention on cognitive factors related to drug-use recovery. Subst Use Misuse. 1999;34:1223–1241. doi: 10.3109/10826089909039406. [DOI] [PubMed] [Google Scholar]
- 26.Booth RE, Kwiatkowski C, Iguchi MY, et al. Facilitating treatment entry among out-of-treatment injection drug users. Public Health Rep. 1998;113(Suppl 1):116–128. [PMC free article] [PubMed] [Google Scholar]
- 27.Mhurchu CN, Margetts BM, Speller V. Randomised clinical trial comparing the effectiveness of two dietary interventions for patients with hyperlipidaemia. Clin Sci (Lond) 1998;95:479–487. [PubMed] [Google Scholar]
- 28.Rollnick S, Butler CC, Stott N. Helping smokers make decisions: the enhancement of brief intervention for general medical practice. Patient Educ Couns. 1997;31:191–203. doi: 10.1016/s0738-3991(97)01004-5. [DOI] [PubMed] [Google Scholar]
- 29.Smith DE, Heckemeyer CM, Kratt PP, Mason DA. Motivational interviewing to improve adherence to a behavioral weight-control program for older obese women with NIDDM. A pilot study. Diabetes Care. 1997;20:52–54. doi: 10.2337/diacare.20.1.52. [DOI] [PubMed] [Google Scholar]
- 30.Woollard J, Beilin L, Lord T, et al. A controlled trial of nurse counselling on lifestyle change for hypertensives treated in general practice: preliminary results. Clin Exp Pharmacol Physiol. 1995;22:466–468. doi: 10.1111/j.1440-1681.1995.tb02046.x. [DOI] [PubMed] [Google Scholar]
- 31.Saunders B, Wilkinson C, Phillips M. The impact of a brief motivational intervention with opiate users attending a methadone programme. Addiction. 1995;90:415–424. doi: 10.1046/j.1360-0443.1995.90341510.x. [DOI] [PubMed] [Google Scholar]
- 32.Pinto BM, Lynn H, Marcus BH, et al. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med. 2001;23:2–10. doi: 10.1207/S15324796ABM2301_2. [DOI] [PubMed] [Google Scholar]
- 33.Bien TH, Miller WR, Boroughs JM. Motivational interviewing with alcohol outpatients. Behavioural and Cognitive Psychotherapy. 1993;21:347–356. [Google Scholar]
- 34.Brown JM, Miller WR. Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychol Addict Behav. 1993;7:211–218. [Google Scholar]
- 35.Pill R, Stott NC, Rollnick SR, Rees M. A randomised controlled trial of an intervention designed to improve the care given in general practice to type II diabetic patients: patient outcomes and professional ability to change behaviour. Fam Pract. 1998;15:229–235. doi: 10.1093/fampra/15.3.229. [DOI] [PubMed] [Google Scholar]
- 36.Ockene JK, Kristeller J, Pbert L, et al. The physician-delivered smoking intervention project: can short-term interventions produce long-term effects for a general outpatient population? Health Psychol. 1994;13:278–281. doi: 10.1037//0278-6133.13.3.278. [DOI] [PubMed] [Google Scholar]
- 37.Ockene IS, Hebert JR, Ockene JK, et al. Effect of physician-delivered nutrition counseling training and an office-support program on saturated fat intake, weight, and serum lipid measurements in a hyperlipidemic population: Worcester Area Trial for Counseling in Hyperlipidemia (WATCH) Arch Intern Med. 1999;159:725–731. doi: 10.1001/archinte.159.7.725. [DOI] [PubMed] [Google Scholar]
- 38.Fleming MF, Barry KL, Manwell LB, et al. Brief physician advice for problem alcohol drinkers. A randomised controlled trial in community-based primary care practices. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- 39.Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473–480. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61:455–461. doi: 10.1037//0022-006x.61.3.455. [DOI] [PubMed] [Google Scholar]
- 41.Miller WR, Meyers RJ, Tonigan JS. Engaging the unmotivated in treatment for alcohol problems: a comparison of three strategies for intervention through family members. J Consult Clin Psychol. 1999;67:688–697. doi: 10.1037//0022-006x.67.5.688. [DOI] [PubMed] [Google Scholar]
- 42.Rosal MC, Ockene JK, Ma Y, et al. Coronary Artery Smoking Intervention Study (CASIS): 5-year follow-up. Health Psychol. 1998;17:476–478. doi: 10.1037//0278-6133.17.5.476. [DOI] [PubMed] [Google Scholar]
- 43.O'Neill K, Baker A, Cooke M, et al. Evaluation of a cognitive-behavioural intervention for pregnant injecting drug users at risk of HIV infection. Addiction. 1996;91:1115–1125. doi: 10.1046/j.1360-0443.1996.91811154.x. [DOI] [PubMed] [Google Scholar]
- 44.Fleming MF, Mundt MP, French MT, et al. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. 2002;26:36–43. [PubMed] [Google Scholar]
- 45.Fleming MF, Manwell LB, Barry KL, et al. Brief physician advice for alcohol problems in older adults: a randomised community-based trial. J Fam Pract. 1999;48:378–384. [PubMed] [Google Scholar]
- 46.Greene GW, Rossi SR. Stages of change for reducing dietary fat intake over 18 months. J Am Diet Assoc. 1998;98:529–534. doi: 10.1016/S0002-8223(98)00120-5. [DOI] [PubMed] [Google Scholar]
- 47.Stotts AL, DiClemente CC, Dolan-Mullen P. One-to-one: a motivational intervention for resistant pregnant smokers. Addict Behav. 2002;27:275–292. doi: 10.1016/s0306-4603(01)00174-5. [DOI] [PubMed] [Google Scholar]
- 48.Maisto SA, Conigliaro J, McNeil M, et al. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. J Stud Alcohol. 2001;62:605–614. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- 49.Murphy JG, Duchnick JJ, Vuchinich RE, et al. Relative efficacy of a brief motivational intervention for college student drinkers. Psychol Addict Behav. 2001;15:373–379. doi: 10.1037//0893-164x.15.4.373. [DOI] [PubMed] [Google Scholar]
- 50.Sellman JD, Sullivan PF, Dore GM, et al. A randomised controlled trial of motivational enhancement therapy (MET) for mild to moderate alcohol dependence. J Stud Alcohol. 2001;62:389–396. doi: 10.15288/jsa.2001.62.389. [DOI] [PubMed] [Google Scholar]
- 51.Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. J Consult Clin Psychol. 2000;68:728–733. [PubMed] [Google Scholar]
- 52.Holder HD, Cisler RA, Longabaugh R, et al. Alcoholism treatment and medical care costs from Project MATCH. Addiction. 2000;95:999–1013. doi: 10.1046/j.1360-0443.2000.9579993.x. [DOI] [PubMed] [Google Scholar]
- 53.Walters ST, Bennett ME, Miller JH. Reducing alcohol use in college students: a controlled trial of two brief interventions. J Drug Educ. 2000;30:361–372. doi: 10.2190/JHML-0JPD-YE7L-14CT. [DOI] [PubMed] [Google Scholar]
- 54.Kemp R, Kirov G, Everitt B, et al. Randomised controlled trial of compliance therapy. 18-month follow-up. Br J Psychiatry. 1998;172:413–419. doi: 10.1192/bjp.172.5.413. [DOI] [PubMed] [Google Scholar]
- 55.Butler CC, Rollnick S, Cohen D, et al. Motivational consulting versus brief advice for smokers in general practice: a randomised trial. Br J Gen Pract. 1999;49:611–616. [Google Scholar]
- 56.Walters ST, Martin JE, Noto J. A controlled trial of two feedback-based interventions for heavy-drinking college students. Alcohol Clin ExpRes. 1999;23(Suppl):45A. [Google Scholar]
- 57.Tappin DM, Mckay C, McIntyre D, et al. A practical instrument to document the process of motivational interviewing. Behavioural and Cognitive Psychotherapy. 2000;28:17–32. [Google Scholar]
- 58.Schmaling KB, Blume AW, Afari N. A randomised controlled pilot study of motivational interviewing to change attitudes about adherence to medications for asthma. J Clin Psychol Med Settings. 2001;8:167–172. [Google Scholar]
- 59.Lennox AS, Bain N, Taylor RJ, et al. Stages of change training for opportunistic smoking intervention by the primary health care team. Part I: randomised controlled trial of the effect of training on patient smoking outcomes and health professional behaviour as recalled by patients. Health Educ J. 1998;57:140–149. [Google Scholar]
- 60.Kenardy J, Mensch M, Bowen K, et al. Group therapy for binge eating in type 2 diabetes: a randomised trial. Diabet Med. 2002;19:234–239. doi: 10.1046/j.1464-5491.2002.00679.x. [DOI] [PubMed] [Google Scholar]
- 61.Connors GJ, Walitzer KS, Dermen KH. Preparing clients for alcoholism treatment: effects on treatment participation and outcomes. J Consult Clin Psychol. 2002;70:1161–1169. doi: 10.1037//0022-006x.70.5.1161. [DOI] [PubMed] [Google Scholar]
- 62.Baker A, Lewin T, Reichler H, et al. Evaluation of a motivational interview for substance use within psychiatric in-patient services. Addiction. 2002;97:1329–1337. doi: 10.1046/j.1360-0443.2002.00178.x. [DOI] [PubMed] [Google Scholar]
- 63.Lincourt P, Kuettel TJ, Bombardier CH. Motivational interviewing in a group setting with mandated clients: a pilot study. Addict Behav. 2002;27:381–391. doi: 10.1016/s0306-4603(01)00179-4. [DOI] [PubMed] [Google Scholar]
- 64.Beich A, Gannik D, Malterud K. Screening and brief intervention for excessive alcohol use: qualitative interview study of the experiences of general practitioners. BMJ. 2002;325:870. doi: 10.1136/bmj.325.7369.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.DiIorio C, Resnicow K, McDonnell M, et al. Using motivational interviewing to promote adherence to antiretroviral medications: a pilot study. J Assoc Nurses AIDS Care. 2003;14:52–62. doi: 10.1177/1055329002250996. [DOI] [PubMed] [Google Scholar]
- 66.Blanchard KA, Morgenstern J, Morgan TJ, et al. Motivational subtypes and continuous measures of readiness for change: concurrent and predictive validity. Psychol Addict Behav. 2003;17:56–65. doi: 10.1037/0893-164x.17.1.56. [DOI] [PubMed] [Google Scholar]
- 67.Curry SJ, Ludman EJ, Graham E, et al. Pediatric-based smoking cessation intervention for low-income women: a randomised trial. Arch Pediatr Adolesc Med. 2003;157:295–302. doi: 10.1001/archpedi.157.3.295. [DOI] [PubMed] [Google Scholar]
- 68.Davis TM, Baer JS, Saxon AJ, Kivlahan DR. Brief motivational feedback improves post-incarceration treatment contact among veterans with substance use disorders. Drug Alcohol Depend. 2003;69:197–203. doi: 10.1016/s0376-8716(02)00317-4. [DOI] [PubMed] [Google Scholar]
- 69.Miller WR, Yahne CE, Tonigan JS. Motivational interviewing in drug abuse services: a randomised trial. J Consult Clin Psychol. 2003;71:754–763. doi: 10.1037/0022-006x.71.4.754. [DOI] [PubMed] [Google Scholar]
- 70.Baer JS, Kivlahan DR, Blume AW, et al. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. Am J Public Health. 2001;91:1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carey MP, Maisto SA, Kalichman SC, et al. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. J Consult Clin Psychol. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Marlatt GA, Baer JS, Kivlahan DR, et al. Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. J Consult Clin Psychol. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- 73.Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68:898–908. [PubMed] [Google Scholar]
- 74.Treasure JL, Katzman M, Schmidt U, et al. Engagement and outcome in the treatment of bulimia nervosa: first phase of a sequential design comparing motivation enhancement therapy and cognitive behavioural therapy. Behav Res Ther. 1999;37:405–418. doi: 10.1016/s0005-7967(98)00149-1. [DOI] [PubMed] [Google Scholar]
- 75.Project MATCH Research Group. Mattson ME, Del Boca FK, Carroll KM, et al. Matching Alcoholism Treatments to Client Heterogeneity: project MATCH three-year drinking outcomes. Alcohol Clin Exp Res. 1998;22:1301–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- 76.Miller WR, Sovereign RG, Krege B. Motivational Interviewing with problem drinkers: II. The drinker's check-up as a preventive intervention. Behavioural Psychotherapy. 1988;16:251–268. [Google Scholar]
- 77.Wertz J. Virginia: Virginia Polytechnic Institute and State University; 1994. The effect of motivational interviewing on treatment participation, self-efficacy, and alcohol use at follow-up in inpatient alcohol dependent adults; pp. 1–178. [Thesis/Dissertation.] [Google Scholar]
- 78.Alderson P, Green S, Higgins JPT. Cochrane reviewers' handbook 4.2.1. Chichester: John Wiley & Sons Ltd; 2004. Updated December 2003. [Google Scholar]
- 79.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomised clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 80.Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. 1998;352:609–613. doi: 10.1016/S0140-6736(98)01085-X. [DOI] [PubMed] [Google Scholar]
- 81.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


