Abstract
Background
Due to clinical and non-clinical factors, considerable variation exists in the prescribing of antibiotics for respiratory tract infections (RTIs) by GPs based in the Netherlands.
Aims
To assess, in patients with RTIs in Dutch general practice: the prescribing rates of antibiotics; the relationship between GP characteristics and antibiotic prescribing; and the type of antibiotics prescribed.
Design of study
Descriptive and prognostic.
Setting
Eighty-four GPs in the middle region of the Netherlands.
Method
All patient consultations for RTIs were registered by 84 GPs during 3 weeks in autumn and winter 2001 and 2002. In addition, all GPs completed a questionnaire related to individual and practice characteristics.
Results
The mean proportion of consultations in which GPs prescribed antibiotics was 33% (95% CI = 29 to 35%) of all RTIs. This proportion varied from 21% for patients with upper RTIs or an exacerbation of asthma/COPD, to about 70% when patients had sinusitis-like complaints or pneumonia. Amoxycillin and doxycycline were the most frequently prescribed antibiotics, while 17% of the antibiotics prescribed were macrolides. Multiple linear regression analysis showed that the longer GPs had practised, the more frequently they prescribed antibiotics, especially in combination with relatively little knowledge about RTIs or the less time GPs felt they had available per patient. The final model, with seven factors, explained 29% of the variance of antibiotic prescribing.
Conclusion
The prescribing behaviour of Dutch GPs might be improved with regard to choice of type and indication of antibiotics.
Keywords: antibiotics, prescribing rates, respiratory tract infections
INTRODUCTION
In the Netherlands, 20% of all complaints presented to a GP are related to respiratory tract infections (RTIs).1 In 34% of consultations for upper RTI2 and in 30% of consultations for lower RTI3 an antibiotic is prescribed, despite evidence that antibiotics do not shorten the duration of RTIs.4-6 Even though antibiotic prescribing rates in the Netherlands are low in comparison with other European countries, about half of these prescriptions are estimated to be unnecessary.4 Furthermore, the last 10 years has seen a shift towards costlier, broad-spectrum antibiotic usage in outpatient care.7,8
There is considerable variation in prescribing antibiotics for RTIs between GPs (FM Haaijer-Ruskamp, unpublished data, 1984).2,9-14 This variation can partly be attributed to clinical reasoning,9-11 but non-clinical factors, such as GP characteristics (for example: years of practice; medical knowledge about RTIs; personal attitude towards RTIs and antibiotics; list size) have also been shown to play an important role (FM Haaijer-Ruskamp, unpublished data).2,9,12-14
In order to develop feasible and successful strategies to optimise antibiotic prescribing, there is a need for more detailed and up-to-date insight in antibiotic management and associated GP characteristics. Therefore, this study aims to assess the prescribing rates of the different types of antibiotics in patients with RTIs in Dutch general practice, and to describe the relationship between GP characteristics and antibiotic prescribing.
METHOD
Eighty-four GPs from the middle region of the Netherlands participated in this study. These GPs registered all patient consultations for RTIs during 3 weeks in autumn or winter (2001 and 2002). GPs interpreted signs and symptoms in their usual manner, aiming to describe everyday practice, using the ICPC codes.15 Additional information on patient characteristics (such as age, sex, and insurance type), symptoms and medications was gathered from the electronic patient records after the 3 weeks of registration. The consultations were grouped into upper or lower respiratory tract clinical entities and a distinction was made between symptoms and diagnoses (Table 1). Medication was classified according to the Anatomical Therapeutical Chemical (ATC) classification system.16
Table 1.
Categories of symptoms and diagnoses per clinical entity (with International Classification of Primary Care code).
| Clinical entity | Symptoms | Diagnoses |
|---|---|---|
| Upper respiratory tract | ||
| Ear | Earache (H01) | Acute otitis media (H71) |
| Hearing complaints (H02) | Serous otitis media (H72) | |
| Discharge from ear (H04) | Eustachian salpingitis (H73) | |
| Other symptoms/complaints of ear (H29) | Chronic otitis media (H74) | |
| Perforation tympanic membrane (H77) | ||
| Upper respiratory tract | Sneezing/nasal congestion (R07) | Upper respiratory tract infection/head cold (R74) |
| Other symptoms of nose (R08) | Other infections respiratory system (R83) | |
| Sinus | Symptoms/complaints sinus (R09) | Sinusitis acute/chronic (R75) |
| Throat | Symptoms/complaints throat (R21) | Tonsillitis acute (R76) |
| Symptoms/complaints tonsils (R22) | Acute laryngitis/tracheitis/croup (R77) | |
| Hypertrophy/chronic infection tonsils (R90) | ||
| Lower respiratory tract | ||
| Pneumonia | Pneumonia (R81) | |
| Cough/bronchitisa | Pain attributed to respiratory system (R01) | Whooping cough (R71) |
| Dyspnea (R02) | Strep-throat/scarlet fever (R72) | |
| Wheezing (R03) | Acute bronchitis/bronchiolitis (R78) | |
| Cough (R05) | ||
| Abnormal sputum/phlegm (R25) | Chronic bronchitis (R79 or R91) | |
| Exacerbation asthma/COPD | Codes as stated above by cough/bronchitis in patients with asthma or COPD combined with codes COPD (R95) or asthma (R96) | |
In patients not diagnosed as having asthma or COPD.
All GPs completed a questionnaire related to individual and practice characteristics such as sex, years of practice, list size, medical knowledge of RTIs (14 items selected from the National Test of the National Centre for Evaluation of Postgraduate Training in General Practice [SVUH] in the Netherlands, with a score ranging from ‘very low’ [0] to ‘very well’ [10]), personal attitude towards RTIs and antibiotics (12 items, with a score ranging from ‘antibiotics not necessary’ [1] to ‘antibiotics necessary’ [5]), visits of drug representatives (number in the last 4 weeks) and perceived time available per patient (ranging from ‘too long’ [1] to ‘too short’ [5]). As mentioned previously, other studies have show these characteristics to be related to antibiotic prescribing.2,9,12-14
The mean proportion of consultations concerning respiratory tract symptoms and diagnoses in which antibiotics were prescribed was assessed per clinical entity, with 95% confidence intervals (CIs). Differences in antibiotic prescribing rates in relation to patient characteristics were analysed using one-way ANOVA.
The associations between GP characteristics and the proportion of consultations in which antibiotics were prescribed were assessed using multiple linear regression controlling for interaction. After selection of relevant factors (main factors and interaction terms) the best fitting model was assessed by means of an ‘enter’ model followed by a ‘backward’ strategy. To describe the strength of the associations, the standardised coefficients (95% CI) were presented, giving an indication of the relative importance of each independent variable. The final model was checked using multilevel analysis (MLWin) to control for practice clustering.
The types of antibiotics used were described per clinical entity. For lower respiratory tract conditions, the patients were divided into two groups: children (0–12 years) and adolescents/adults (above the age of 12 years), because indications and notable contraindications vary for these age groups. The data were analysed using SPSS version 10.0.
How this fits in
Previous research has shown considerable variation in prescribing antibiotics for respiratory tract infections, attributable to clinical and non-clinical factors. Recent antibiotic prescribing rates are lacking for the Netherlands. The variation in prescribing antibiotics for respiratory tract infections ranges from 21% for upper respiratory tract infections to 74% for sinusitis-like complaints. The proportion of antibiotics prescribed does not seem to have decreased in the last 10 years, while the proportion of macrolides prescribed increased from 4% to 17% of the antibiotics prescribed.
RESULTS
The GPs had practised for a mean of 16 years (range = 0–34 years) and almost three quarters (73%) had a partnership practice. In all, they registered 2630 consultations (mean = 31; range = 4–108). The mean patient age was 32 years (range = 0–98 years) (Table 2).
Table 2.
GP and consultation characteristics.
| GP characteristics (n = 84) | Number (%) | |
|---|---|---|
| Sex | Male | 57 (68) |
| Years of practice | 0–10 years | 27 (32) |
| 11–20 years | 39 (35) | |
| >20 years | 28 (33) | |
| Type of practice | Single | 23 (27) |
| Partnership practice | 61 (73) | |
| Urbanisation level | Rural | 30 (36) |
| Small town | 38 (45) | |
| City | 16 (19) | |
| % patients insured by the Dutch Sickness Fund | 0–60 | 44 (52) |
| >61 | 31 (37) | |
| List size (mean [SD]) | 2361 (504) | |
| Consultation characteristics (n = 2630) | ||
| Age of patient (years) | 0–4 | 518 (20) |
| 5–12 | 378 (14) | |
| 13–64 | 1360 (52) | |
| >65 | 372 (14) | |
| Sex of patient | Male | 1204 (46) |
| Insurance type | Dutch Sickness Fund | 1749 (67) |
| Private | 873 (33) | |
SD = standard deviation.
Antibiotic prescribing
Overall, GPs prescribed antibiotics in one out of three consultations concerning RTIs (mean = 33%, 95% CI = 29 to 35%) (Table 3). In a consultation where a diagnosis was registered (for example, otitis media, sinusitis, bronchitis) GPs prescribed an antibiotic in almost half (47%) of the cases, compared to one in eight (12%) when the GP only registered a symptom (such as earache or cough).
Table 3.
Antibiotic prescribing rates according to clinical entities (n = 84 GPs).
| Proportion antibiotics prescribed (mean per GP [95% CI]) | Number of consultations | |
|---|---|---|
| Diagnoses | 47 (42 to 52) | 1664 |
| Symptoms | 12 (9 to 16) | 966 |
| Ear | 35 (28 to 42) | 408 |
| Upper respiratory tract | 21 (15 to 27) | 573 |
| Sinus | 74 (67 to 81) | 272 |
| Throat | 37 (29 to 45) | 255 |
| Pneumonia | 67 (54 to 80) | 108 |
| Cough/bronchitis | 27 (22 to 32) | 669 |
| Exacerbation of asthma/COPD | 21 (14 to 28) | 345 |
| Mean/Total | 33 (29 to 35) | 2630 |
Prescription rates varied considerably between clinical entities. As many as 70% of consultations with patients presenting sinusitis-like complaints or pneumonia resulted in antibiotic prescribing, against 21% of consultations with patients suffering upper RTIs or with an exacerbation of asthma/COPD. In cases of ear and throat complaints or cough/bronchitis, an antibiotic was prescribed in one third of cases.
Patient characteristics and antibiotic prescribing
Children (0–12 years) received antibiotics less frequently (29%) than older patients (36%) (one-way ANOVA = P <0.001). Further inspection of data showed this to be the case for all clinical entities except for ear complaints: in children with ear complaints below the age of 5 years, more antibiotics were prescribed than in patients above the age of 5 years (on average 44% versus 26%, one-way ANOVA = P <0.001). There were no differences in antibiotic prescribing in relation to patient sex and insurance type.
GP characteristics and antibiotic prescribing
For RTIs, seven factors were independently correlated with antibiotic prescribing rates, explaining 29% of the variation in antibiotic prescribing (Table 4). Years of practice was shown to be a main factor, especially when in interaction with medical knowledge on RTIs and perceived time available per patient. Medical knowledge on RTIs and perceived time available per patient were also independently associated with antibiotic prescribing rates, as well as the interaction terms ‘sex × list size’ and ‘years of practice × visits from drug representatives’, but these latter associations were weaker (Table 4). Sex, list size and visits from drug representatives were not independently correlated with these prescribing rates. Other factors, such as personal attitude towards RTIs and antibiotics, were not correlated with antibiotic prescribing at all. Multilevel analysis, controlling for practice clustering, resulted in similar findings.
Table 4.
The association between GP characteristics and mean antibiotic prescribing in RTIs by means of linear regression analysis.
| 95% CI | ||
|---|---|---|
| GP characteristics | ||
| Sex | – | |
| Years of practice | 3.60 | 1.20 to 6.00 |
| List size | – | |
| Medical knowledge on RTIs | 0.63 | 0.01 to 1.26 |
| Visits from drug representatives | – | |
| Perceived time per patient | 0.71 | 0.18 to 1.24 |
| Interaction terms | ||
| Sex × list sizea | 0.34 | 0.09 to 0.59 |
| Years of practice × medical knowledge on RTIsb | −2.37 | −4.3 to −0.42 |
| Years of practice × visits from drug representativesc | 0.25 | −0.00 to 0.51 |
| Years of practice × perceived time per patientd | −1.32 | −2.48 to −0.17 |
Explained variance: 0.29.
Female GPs having more patients enlisted, prescribe antibiotics more frequently.
The longer the years of practice and the less a GP knows about RTIs, the more frequently a GP prescribes antibiotics.
The longer the years of practice and the more drug representatives seen by a GP, the more frequently a GP prescribes antibiotics.
The longer the years of practice and the less time perceived by the GP to be available per patient, the more frequently a GP prescribes antibiotics. RTI = respiratory tract infection.
Type of antibiotics
The type of antibiotics prescribed per clinical entity is shown in Figure 1. For ear complaints amoxicillin was prescribed most frequently (in 76% of consultations in which antibiotics were prescribed). For patients with upper RTIs or sinusitis-like complaints doxycycline was most frequently prescribed (41% and 63%, respectively), as were narrow-spectrum penicillins for patients with throat complaints (43%). More specific inspection of data showed that in cases of sore throat (R21), tonsil complaints (R22) and acute tonsillitis (R76), narrow-spectrum penicillins accounted for 51% of the consultations in which antibiotics were prescribed, while broad-spectrum penicillins accounted for 27% and macrolides for 10%.
Figure 1.
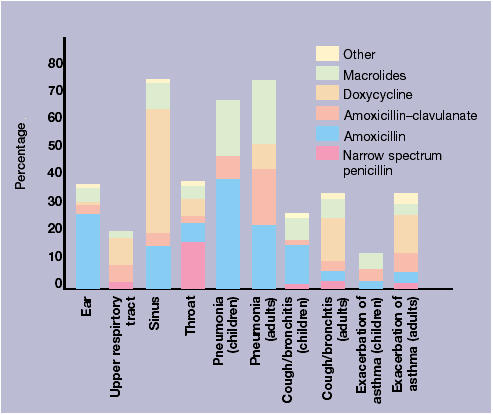
Clinical entities and type of antibiotics (n = 2630 consultations)
In cases of children with pneumonia or cough/bronchitis, amoxicillin was prescribed in more than half of the consultations in which antibiotics were prescribed (59% and 55% respectively). Antibiotics were rarely prescribed for children with exacerbations of asthma. None of the children in the study received doxycycline. Adults with cough/bronchitis or exacerbation of asthma/COPD received doxycycline in almost half of the consultations in which antibiotics were prescribed (48% and 49% respectively), while macrolides and amoxicillin-clavulanate together were prescribed in about 40% of cases. In adults with pneumonia, amoxicillin, amoxicillin–clavulanate or macrolides were prescribed in about 30% of the consultations in which antibiotics were prescribed.
DISCUSSION
The participating GPs prescribed antibiotics in one-third of consultations concerning RTIs. There was considerable variation between the clinical entities. Years of practice was the most important factor in explaining the variation in prescribing antibiotics; the longer GPs had practiced, the more antibiotics they prescribed, especially if they had relatively little knowledge about RTIs or felt they had relatively less time available per patient.
Strengths and limitations of the study
The results were based on data from 84 GPs, with 2630 patient consultations. Our findings reliably describe antibiotic prescription rates in cases of RTIs, as the data analysed was taken from electronic patient records, which accurately reflect drug prescriptions.17 Further, a previous and similar registration showed that the variety of registered consultations between GPs across time was consistent with claims data.18
GPs participated in this study by way of self-selection, as is the case with all kinds of sentinel studies. The sex of GPs, years of practice, and urbanisation level accurately reflected the whole Dutch GP population. Single-handed GPs were under-represented, but as type of practice was not associated with the frequency of antibiotic prescribing, this is unlikely to have influenced antibiotic prescribing rates. Time constraints during consultation may have influenced registration of consultations concerning RTIs. This is unlikely to have biased the registration as the antibiotic prescribing rates differed little from those found during another nationwide sentinel (AE Akkerman et al, unpublished data, 2004). We therefore believe that the associations between GP characteristics and antibiotic prescribing rates were unbiased.
Comparison with the existing literature
The mean prescription rates for RTIs in this study are similar to those found in the first Dutch National Survey of General Practice 10 years ago.2,3
More than three quarters of the antibiotic prescriptions for patients with ear and sinusitis-like complaints were in accordance with the first choice antibiotics advocated by the guidelines of the Dutch College of General Practitioners, that is, amoxicillin for ear infections and amoxicillin or doxycycline for sinusitis-like complaints. For throat complaints half of the antibiotic prescriptions were in accordance to the guidelines, that is, narrow-spectrum penicillins. Amoxicillin was most commonly prescribed in cases of lower RTIs in children, and doxycycline in adults. This was in line with the available national pharmacotherapeutic sources.19 A national guideline for acute cough was lacking at the time of the study.
These results are somewhat similar to those found 10 years previously,2,3 with two noteworthy exceptions. Firstly, the use of narrow-spectrum penicillins in throat infections has declined. The proportion of narrow-spectrum penicillins among all antibiotic prescriptions for sore throat, tonsil complaints and acute tonsillitis fell from 64% 10 years ago,2 to 51%. The proportion of broad-spectrum penicillins, which are not indicated in cases of throat infections, remained the same, while the proportion of macrolides, which were rarely prescribed for these cases 10 years ago, increased. Secondly, the overall use of macrolides was 17% of all consultations in which antibiotics were prescribed, mainly for lower RTIs. This percentage was less than 4% 10 years ago.2 These trends are noteworthy because these types of antibiotics are not a first choice treatment in Dutch general practice and are linked to a risk of growing resistance of relevant bacterial pathogens.20
The explained variance was 29%, which is comparable to explained variances found in a previous study (FM Haaijer-Ruskamp, unpublished data).12 Two studies found that years of practice are associated with higher prescribing rates.12,14 This factor correlates both with the time expired after training for general practice and with developing habits over time. It is likely that GPs maintain the policy learned during their vocational training. In addition, the results show that antibiotic prescribing in RTIs does not correlate with personal attitudes, as far as measured in this study.
It can be concluded that some aspects of prescribing antibiotics by Dutch GPs could be improved, despite the relatively low rates of antibiotics prescribed compared to other European Union countries,21 the US22 and Canada.23
GPs who trained some time ago should be a target group for quality assurance in this field. Reduction of antibiotic prescribing for RTIs is possible, as shown by Welschen et al by means of a multiple intervention strategy. This consists, in part, of group education meetings, monitoring and feedback on prescribing behaviour.18 However, changing clinical practice is difficult, as shown by other studies.24,25 Increasing the proportion of first choice antibiotics seems to be easier than reducing the number of antibiotic prescriptions (I Welschen et al unpublished data, 2004).
Implications for future research
There is a need for further study involving more GPs to allow for detailed subgroup analyses, as well as studies that look at both GP and patient characteristics that are a risk for unnecessary antibiotic prescriptions. We recently began a study to address these issues with 150 GPs. Findings from both types of studies are needed to develop strategies to further optimise the use of antibiotics in general practice.
Acknowledgments
We thank the GPs who voluntarily participated in this study. We acknowledge Frances Verheij for all her administrative assistance, Peter Zuithoff for his statistical assistance, and Gerrit Hofmeijer and Tom van Goor for extracting data from the electronic patient records in general practices.
Funding body and reference number
The Health Care Insurance Board (College voor Zorgverzekeringen) (Reference number 451/001/2001)
Ethics committee reference number
Ethics committee of UMC Utrecht, reference number protocol 01/304
Competing interests
None
REFERENCES
- 1.Van de Lisdonk EH, van den Bosch WJHM, Huygen FJA. Lagro-Janssen ALM (redactie). Ziekten in de huisartspraktijk. Maarssen: Elsevier/Bunge; 1999. [Diseases in General Practice.] [Google Scholar]
- 2.De Melker RA, Kuyvenhoven MM. Management of upper respiratory tract infections in Dutch family practice. J Fam Pract. 1994;38:353–357. [PubMed] [Google Scholar]
- 3.Kuyvenhoven MM, Verheij TJM, de Melker RA, van der Velden J. Antimicrobial agents in lower respiratory tract infections in Dutch general practice. Br J Gen Pract. 2000;50:133–134. [PMC free article] [PubMed] [Google Scholar]
- 4.De Melker RA. Effectiviteit van antibiotica bij veel voorkomende luchtweginfecties in de huisartspraktijk. [Efficacy of antibiotics in frequently occurring airway infections in family practice.] Ned Tijdschr Geneeskd. 1998;142:452–456. [PubMed] [Google Scholar]
- 5.Butler CC, Rollnick S, Pill R, et al. Understanding the culture of prescribing: qualitative study of general practitioners' and patients' perceptions of antibiotics for sore throats. BMJ. 1998;317:637–42. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott JG, Cohen D, DiCicco-Bloom B, et al. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Pract. 2001;50:853–858. [PubMed] [Google Scholar]
- 7.Bruinsma N, Stobberingh E, de Smet P, van den Bogaard A. Antibiotic use and the prevalence of antibiotic resistance in bacteria from healthy volunteers in the Dutch community. Infection. 2003;31:9–14. doi: 10.1007/s15010-002-3035-8. [DOI] [PubMed] [Google Scholar]
- 8.Kuyvenhoven MM, van Balen FAM, Verheij TJM. Outpatient antibiotic prescription from 1992 till 2001 in The Netherlands. J Antimicrob Chemother. 2003;52:675–678. doi: 10.1093/jac/dkg412. [DOI] [PubMed] [Google Scholar]
- 9.De Sutter AI, de Meyere MJ, de Maeseneer JM, Peersman WP. Antibiotic prescribing in acute infections of the nose or sinuses: a matter of personal habit? Fam Pract. 2001;18:209–213. doi: 10.1093/fampra/18.2.209. [DOI] [PubMed] [Google Scholar]
- 10.Coenen S, Michiels B, van Royen P, et al. Antibiotics for coughing in general practice: a questionnaire study to quantify and condense the reasons for prescribing. BMC Family Practice. 2002;3:16–25. doi: 10.1186/1471-2296-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S, Little P, Britten N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ. 2003;326:138. doi: 10.1136/bmj.326.7381.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuyvenhoven MM, de Melker RA, van der Velden K. Prescription of antibiotics and prescribers' characteristics. A study into prescription of antibiotics in upper respiratory tract infections in general practice. Fam Pract. 1993;10:366–370. doi: 10.1093/fampra/10.4.366. [DOI] [PubMed] [Google Scholar]
- 13.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–904. [PubMed] [Google Scholar]
- 14.Lam TP, Lam KF. Management of upper respiratory tract infection by family doctors. Int J Clin Pract. 2001;55:358–60. [PubMed] [Google Scholar]
- 15.Anonymous. ICPC-2: International Classification of Primary Care. Oxford: World Organization of National Colleges, Academies, and Academic Associations of General Practitioners/Family Physicians; 1998. [Google Scholar]
- 16.WHO Collaborating Centre for Drug Statistics Methodology. Complete ATC index. 2004 www.whocc.no/atcddd (accessed 7 Jan 2005)
- 17.Thiru K, Hassey A, Sullivan F. Systematic review of scope and quality of electronic patient record data in primary care. BMJ. 2003;326:1070. doi: 10.1136/bmj.326.7398.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Welschen I, Kuyvenhoven MM, Hoes AW, Verheij TJ. Effectiveness of a multiple intervention to reduce antibiotic prescribing for respiratory tract symptoms in primary care: randomised controlled trial. BMJ. 2004;329:431. doi: 10.1136/bmj.38182.591238.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Loenen AC. Farmacotherapeutisch Kompas: medisch farmaceutische voorlichting/uitgave van de Commissie Farmaceutische Hulp van het College voor Zorgverzekeringen. Utrecht: Roto Smeets Utrecht; 2003. (redacteur) [Pharmacotherapeutic Compass: medical pharmaceutical advice/publication of committee Pharmaceutical Help of the Health Care insurance Board.] [Google Scholar]
- 20.De Neeling AJ, Overbeek BP, Horrevorts AM, et al. Antibiotic use and resistance of Streptococcus pneumoniae in The Netherlands during the period 1994-1999. JAC. 2001;48:441–444. doi: 10.1093/jac/48.3.441. [DOI] [PubMed] [Google Scholar]
- 21.Cars O, Mölstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001;357:1851–1853. doi: 10.1016/S0140-6736(00)04972-2. [DOI] [PubMed] [Google Scholar]
- 22.Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991–1999. Ann Intern Med. 2003;138:525–533. doi: 10.7326/0003-4819-138-7-200304010-00008. [DOI] [PubMed] [Google Scholar]
- 23.Hutchinson JM, Jelinski S, Hefferton D, et al. Role of diagnostic labeling in antibiotic prescription. Can Fam Physician. 2001;47:1217–1224. [PMC free article] [PubMed] [Google Scholar]
- 24.Zwar N, Henderson J, Britt H, et al. Influencing antibiotic prescriber feedback and management guidelines: a 5 year follow-up. Fam Pract. 2002;19:12–17. doi: 10.1093/fampra/19.1.12. [DOI] [PubMed] [Google Scholar]
- 25.Jewell D. How to change clinical behaviour: no answers yet. Br J Gen Pract. 2003;53:266–267. [PMC free article] [PubMed] [Google Scholar]


