Abstract
Background
Opiate dependence is a major health and social issue in many countries. A mainstay of therapy has been methadone maintenance treatment, but other treatments, particularly buprenorphine, are increasingly being considered.
Aim
To conduct a systematic review to synthesise and critically appraise the evidence on the effectiveness of community maintenance programmes with methadone or buprenorphine in treating opiate dependence.
Method
A systematic review of databases, journals and the grey literature was carried out from 1990–2002. Inclusion criteria were: community-based, randomised controlled trials of methadone and/or buprenorphine for opiate dependence involving subjects who were aged 18 years old or over.
Results
Trials were set in a range of countries, employed a variety of comparators, and suffered from a number of biases. The evidence indicated that higher doses of methadone and buprenorphine are associated with better treatment outcomes. Low-dose methadone (20 mg per day) is less effective than buprenorphine (2–8 mg per day). Higher doses of methadone (>50–65 mg per day) are slightly more effective than buprenorphine (2–8 mg per day). There was some evidence that primary care could be an effective setting to provide this treatment, but such evidence was sparse.
Conclusion
The literature supports the effectiveness of substitute prescribing with methadone or buprenorphine in treating opiate dependence. Evidence is also emerging that the provision of methadone or buprenorphine by primary care physicians is feasible and may be effective.
Keywords: buprenorphine, methadone, opiate dependence, primary health care, systematic review
INTRODUCTION
Opiate dependence is a major health and social issue in many countries, as it is associated with increased morbidity and mortality, it adversely affects social circumstances, and it is accompanied by lost productivity and higher healthcare and law enforcement costs.1-3 The first (and still most common) drug used in community maintenance for opiate dependence is methadone. It is a full opioid agonist with a long half-life (less than 24 hours), has good oral bioavailability and reaches peak blood concentration 4 hours after oral administration. Methadone is useful in maintenance prescribing because ‘once daily’ dosing is possible. However, subjects need to take methadone on a daily basis and may experience withdrawal symptoms if a dose is missed. Moreover, as the level of respiratory depression or sedation that methadone can produce is not limited, a methadone overdose can be fatal.4 These negative characteristics have stimulated interest in buprenorphine and other alternative drugs.
Buprenorphine has only recently become more widely available and is now licensed in Austria, Belgium, Denmark, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, The Netherlands, Portugal, Sweden and the UK. Buprenorphine is a partial μ-opioid agonist, and therefore has both agonist and antagonist properties. It binds strongly to receptors — displacing other opiates — and thus can precipitate withdrawal, particularly when treatment is initiated. Buprenorphine has poor oral bioavailability and is generally administered sublingually, after which peak plasma concentration is reached in 1–1.5 hours. With a half-life of approximately 35 hours, 48- and 72-hour dosing is theoretically possible. Buprenorphine may be ‘safer’ in overdose compared to other opiates as it causes less respiratory depression — the main cause of death in overdose. However, when combined with other depressants, there is still a risk of respiratory depression. Given that co-dependence with alcohol and benzodiazepines is common, this may not necessarily confer any great safety benefit.
How this fits in
Treatment of opiate-dependent subjects has mainly consisted of methadone maintenance, but other drugs, in particular buprenorphine, are increasingly being considered. This article reviews the population groups and settings in which community maintenance with methadone or buprenorphine has been provided and examines the impact of intensity of treatment and additional aspects of programme delivery on the effectiveness of these two drugs.
The aim of this article is to evaluate the effectiveness of maintenance treatment with methadone or buprenorphine in treating opiate dependence. To this effect, an international systematic review of randomised controlled trials was carried out. Although a review of community maintenance with methadone or buprenorphine was published in the Cochrane Library,4 this article adds to the Cochrane review by investigating the population groups and settings in which community maintenance treatment has been provided, and by examining the impact of intensity of treatment and additional aspects of programme delivery on effectiveness. A number of policy recommendations are also identified.
METHOD
Search strategy
Studies were identified from a number of sources. The following electronic databases were searched: Medline, EMBASE, PsycINFO, CINAHL, SSCI, the Lindesmith Library database, the Controlled Trials Register of the Cochrane Library, ASSIA, EBSCO, and the British Library Catalogue. The search strategy was varied and adapted as necessary to suit particular databases. Search terms included ‘opiate’, ‘heroin’, ‘dependence’, ‘substance abuse’, ‘community maintenance’, ‘methadone’, ‘buprenorphine’, ‘clinical trial’, and ‘randomised controlled trial’ individually and in combination with each other. Additionally, journals in the field of addiction that were available on-line and electronic journals were searched. Journals that were not available electronically were hand searched for relevant studies.
The grey literature was included through hand searching of abstracts from the following conferences: International Conferences on the Reduction of Drug-Related Harm (1997–2000), Association of University Departments of General Practice (1997–2001), British Pharmaceutical Conference, and the professional newsletters of the Pharmacy Misuse Advisory Group and Substance Misuse Management Group, which list recent publications. The authors' national and international network of contacts was used to identify ongoing and unpublished studies.
The review focused on studies published between 1990 and 2002. Earlier studies were considered to be of limited practical relevance due to likely changes in the extent and patterns of heroin misuse and developments in maintenance treatments over time. Only English language studies were considered for practical reasons. The main searches were undertaken between December 2001 and April 2002. Existing reviews are not included in this paper because primary studies were analysed.
Inclusion criteria
Community maintenance treatment was defined as any programme that purports to stabilise subjects, based in the community, on a substitute drug for as long as it is necessary to help them avoid returning to previous patterns of drug use. A longer-term aim of such programmes is to gradually reduce the quantity of the prescribed drug until the subject does not experience withdrawal symptoms and is drug-free. Although programme content varies across countries, trials were included in the review if the maintenance treatment under study consisted of the following components (albeit at varying levels of intensity): administration of methadone or buprenorphine, the provision of medical care, the delivery of counselling and support, health promotion and education, and linkage with other community-based services. The experimental group may have already been detoxified on an inpatient or outpatient basis prior to the start of the intervention treatment, may be treated pharmacologically and/or maintained in therapy. The control group may be treated pharmacologically, with placebo, or may have no treatment. Trials that examined the effectiveness of inpatient services were not included.
All randomised controlled trials involving subjects who were 18 years old or over, who were opiate dependent, and who participated in a community maintenance programme with methadone or buprenorphine were included in the review. Both subjects dependent on heroin alone and in combination with other drugs were included. Studies that examined subjects who were pregnant, suffered concurrent and major psychiatric illness, or participated in prison-based programmes were excluded.
Outcomes
The primary outcome measures studied were abstinence from illicit opiate use, reduction in illicit opiate use, withdrawal severity, and retention in treatment. Secondary outcome measures were changes in employment status, housing status, education, crime rates, quality of life, and level of injecting. Other relevant outcomes such as acceptability and social behaviour were discussed where appropriate.
Assessment of methodological quality
The methodological quality of each study was assessed according to the criteria outlined by the Cochrane Collaboration.5 The validity of studies was assessed in terms of the extent to which the design and conduct of the study are likely to prevent five sources of systematic errors, that is selection bias (systematic differences in comparison groups, knowledge of treatment assignment by staff or subjects), performance bias (systematic differences in care provided apart from the intervention being evaluated), attrition bias (systematic differences in withdrawals from the trial), detection bias (systematic differences in outcome assessment), and information bias (systematic differences in self-reported and objectively measured outcomes).
Data analysis
Studies were independently assessed by two reviewers (in agreement with Cochrane Collaboration guidelines). A standard inclusion and data extraction form was completed for each study. This form was developed following Cochrane Collaboration review requirements. Any disagreements between the two reviewers were to be resolved by a third reviewer and, if there was still no consensus, this was to be cleared through discussion within the research team. In practice, this was not required.
In light of the heterogeneity of primary studies as evidenced by the lack of uniformity in study design, participants, administered doses of methadone or buprenorphine, duration of maintenance treatment, and methods of reporting outcomes, a meta-analytic approach was abandoned in favour of a descriptive review. This is justified on the basis that previous reviews have found evidence of the heterogeneity of primary studies by, for example, detecting significant differences in effectiveness between trials that enrolled subjects with past methadone maintenance experience and trials that included subjects with no prior experience;6 and between trials that varied according to the dose of methadone or buprenorphine that was administered.4
Results
The number of studies identified by the literature search and excluded at each stage of the search process is illustrated in Figure 1. Of the 48 randomised controlled trials that evaluated the effectiveness of community maintenance treatment, 14 trials related to methadone,7-19 20 trials examined buprenorphine,20-37 and 14 trials contrasted methadone with buprenorphine.38-51
Figure 1.
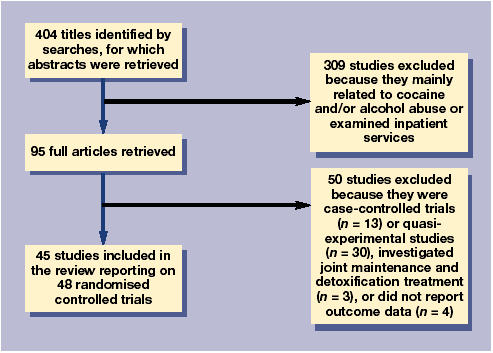
Flow chart of findings of literature search.
The majority of randomised controlled trials were carried out in the US, although the findings of trials set in Australia, Austria, Iran, Italy, Spain, Switzerland and the UK were also reported. No randomised controlled trials in other countries were identified. Care should be exercised when assessing the relevance of these findings to other countries because the subject population, the range of drug problems, and the sociological factors surrounding opiate dependence vary across countries. For example, maintenance studies from the US enrolled subjects with a higher mean age compared to the mean age in other countries.47,48,52 Moreover, differences are observed between countries in the funding, organisation, and regulation of community maintenance treatments. For example, supervised self-administration of both methadone and buprenorphine in community pharmacies is common in Australia, whereas take-home doses are standard in France.
Population groups
Trials on maintenance with methadone or buprenorphine generally enrolled subjects who were in good health, met Diagnostic and Statistical Manual III or IV criteria for opiate dependence, had no serious psychiatric or medical comorbidities, had not been involved in drug misuse treatment in the months prior to community maintenance, and were not pregnant. Hence, the results may not apply to the wider population of opiate-dependent subjects.
Variation exists between countries in the rules governing who may and who may not enter maintenance treatment and in the extent to which clinics and providers running maintenance programmes comply with these rules. In addition to this, trials have attracted subjects who were willing to participate and thus may have been more compliant with maintenance treatment than the wider population of opiate-dependent subjects.20,21,38 To date, the impact of the selection of subjects who enrol in trials on treatment effectiveness has not been investigated.
The feasibility and acceptance of methadone maintenance treatment has been demonstrated for subjects with a long history of illicit opiate use.12,14,15,19 Buprenorphine could be an important alternative because it is accepted by many drug users who are unwilling to receive methadone maintenance.36 Trials have also been able to induce subjects with concurrent opiate dependence and cocaine use onto maintenance treatment with either methadone8 or buprenorphine.49
Settings
Most trials were conducted in an outpatient clinic, although a number of trials were carried out in a laboratory setting.27-28,34,35 The delivery of maintenance treatment in these settings was characterised by random assignment to treatment, fixed doses of medications, no take-home medication, discharge of subjects who missed 3 consecutive days of medication, restricted and mandatory psychosocial treatment, no rewards for treatment compliance, limited length of treatment, no influence of urinary testing on treatment plan, and intense monitoring. Each of these features may not be replicated in routine practice and restrict the generalisability of the results to community settings.
There was little information about the providers who deliver maintenance treatment. The administration of methadone and buprenorphine was generally conducted and supervised by a physician and/or nurse. In addition to this, psychiatrists,11 counsellors,48 and social workers36 were involved in delivering additional medical and psychosocial services. The fact that the providers administering maintenance programmes in these trials are likely to be highly motivated and have received specific training, and that the delivery process was subject to close supervision and regulatory control, may have influenced outcomes.
In a recent development, opiate-dependent subjects have been receiving maintenance treatment with methadone or with buprenorphine in a primary care setting. For example, community maintenance has been extended to primary care in Australia, Canada, Scotland and Switzerland and has been tested in the US.53
One US trial contrasted methadone maintenance provided by primary care physicians in their office with methadone maintenance delivered in an outpatient clinic.10 The option of office-based care was only available to those clients who met criteria of sufficient clinical stability to participate. Seventy-seven per cent of office-based subjects were very satisfied with the care that they received and 55% of clinicians expressed their satisfaction with treating office-based patients. Treatment in primary care and in an outpatient clinic had comparable effectiveness as no differences were observed in illicit drug use and functional status. Another trial contrasted buprenorphine maintenance treatment delivered in a primary care clinic with its provision in an outpatient clinic.32 Primary care-based buprenorphine maintenance treatment was more effective than treatment in an outpatient clinic in terms of the rate of treatment retention (78% versus 52%), the proportion of opiate-positive urine samples (63% versus 85%) and the proportion of subjects who are abstinent from opiates for more than 3 weeks (43% versus 13%).
These findings suggest that primary care physicians who are interested in providing treatment for opiate-dependent subjects can be identified, and that maintenance treatment in this setting is acceptable to clients. However, the need to train and supervise primary care physicians, and the imposition of eligibility criteria for clients to enrol may restrict the potential of office-based maintenance by primary care physicians as a mechanism to achieve substantial treatment expansion.
None of the studies identified in the review used community pharmacies as a means of drug dispensing. This could be of considerable practical relevance because several countries, notably the UK, Australia and France rely on community pharmacies rather than clinics to dispense medication.
Intensity of treatment
Higher doses of methadone are more effective at enhancing treatment retention and reducing illicit opiate use than lower doses (Table 1). Trials have detected significant differences over a range from 20 to 90 mg of methadone per day. Although the most effective dose is as yet undetermined, the evidence suggests that maintenance doses as low as 20 mg per day are inadequate for suppressing opiate use, although they can be partially effective in retaining subjects in treatment.16 A minimal effective dose of methadone may be 50 mg per day. On the other hand, higher doses of methadone may increase craving for heroin and decrease subjective wellbeing.9
Table 1.
Effectiveness of maintenance treatment with methadone or buprenorphine.
| Study reference number | Drug | Dose (mg) | Retention (%) | Illicit opiate use (% positive urine samples) |
|---|---|---|---|---|
| 16 | Methadone | 0 | 21 | 74 |
| Methadone | 20 | 41 | 68 | |
| Methadone | 50 | 52 | 56 | |
| 17 | Methadone | 40–50 | 56 | 62 |
| Methadone | 80–100 | 60 | 53 | |
| 20 | Buprenorphine | 1 | 34 | |
| Buprenorphine | 2 | 43 | ||
| Buprenorphine | 4 | 63 | ||
| 21 | Buprenorphine | 1 | 47 | |
| Buprenorphine | 2 | 58 | ||
| Buprenorphine | 4 | 71 | ||
| 30 | Buprenorphine | 0 | 28 | 96 |
| Buprenorphine | 2 | 62 | 76 | |
| Buprenorphine | 8 | 51 | 74 | |
| 31 | Buprenorphine | 1 | 40 | 94 |
| Buprenorphine | 4 | 51 | 90 | |
| Buprenorphine | 8 | 52 | 90 | |
| Buprenorphine | 16 | 61 | 86 | |
| 38 | Methadone | 30 | 61 | |
| Buprenorphine | 1 | 29 | ||
| Buprenorphine | 3 | 46 | ||
| Buprenorphine | 8 | 68 | ||
| 42 | Methadone | 20 | 20 | 71 |
| Methadone | 60 | 32 | 56 | |
| Buprenorphine | 8 | 42 | 47 | |
| 44 | Methadone | 35 | 82 | 48 |
| Methadone | 65 | 63 | 49 | |
| Buprenorphine | 2 | 54 | 73 | |
| Buprenorphine | 6 | 39 | 76 | |
| 45 | Methadone | 30 | 19 | 32 |
| Methadone | 80 | 31 | 21 | |
| Buprenorphine | 8 | 20 | 32 | |
| 46 | Methadone | Maximum 150 | 59 | |
| Buprenorphine | Maximum 32 | 50 | ||
| 49 | Methadone | 20 | 47 | 72 |
| Methadone | 65 | 64 | 45 | |
| Buprenorphine | 4 | 34 | 77 | |
| Buprenorphine | 12 | 55 | 58 | |
| 50 | Methadone | 50 | 56 | 48 |
| Buprenorphine | 8 | 56 | 55 | |
| 51 | Methadone | 60–120 | 90 | 59 |
| Buprenorphine | 8–16 | 56 | 62 |
Dosage of buprenorphine has an impact on treatment retention and illicit opiate use (Table 1). A comparison of buprenorphine dosages under 16 mg per day showed that a higher dose was associated with better treatment retention and a greater reduction in illicit opiate use. These trials suggested that the minimum effective daily maintenance dose of buprenorphine for reducing opiate use ranges from 8 to 16 mg per day. Higher doses of buprenorphine are more effective in attenuating heroin craving than low-dose buprenorphine.27,31,36
Trials examining the frequency of buprenorphine administration suggest that drug effects decrease and withdrawal effects increase as the time since the last active dose lengthens. This pattern is observed with 48-, 72-, 96-, and 120-hour buprenorphine dosing regimens.23,24,26,29,33-35 Two trials noted that the administration of buprenorphine three times weekly is just as effective as its daily administration for retaining subjects in treatment.25,37 There is some evidence that the maximum effective dosing interval may be limited to 120 hours.29,35 However, some subjects are willing and able to endure the withdrawal symptoms associated with less-than-daily dosing regimens and actually prefer less frequent dosing regimens with multiples of the daily dose.23,34
A number of trials have examined the dosage at which methadone becomes more effective in both reducing illicit opiate use and retaining subjects in treatment than low doses of buprenorphine (2–8 mg per day). Table 1 suggests that methadone doses exceeding 65 mg per day are more effective at retaining people in treatment and reducing illicit drug use than buprenorphine 2–8 mg per day. There were no comparisons between buprenorphine at higher daily doses (12–24 mg) and methadone.
Additional aspects of programme delivery
A number of additional services can be provided in the context of a community maintenance programme. These include medical and psychosocial services, the offer of take-home incentives contingent on certain behaviours by subjects, and the provision of behavioural skills sessions intended to reinforce abstinence. The provision of such additional services has been investigated in the context of methadone maintenance treatment, although the evidence is limited by the lack of standardisation in interventions. No evidence relating to buprenorphine maintenance treatment was identified. Although most trials comparing methadone with buprenorphine incorporated additional services in their maintenance programmes, these services were present in each treatment arm, which makes it impossible to assess their effectiveness.40-42,44,45,47-50
Evidence is emerging that medical and psychosocial services are valued by opiate-dependent subjects and that they increase the effectiveness of methadone maintenance treatment. One trial found that subjects who received medical and psychosocial services in addition to methadone maintenance treatment had a higher rate and number of weeks of opiate-free urine samples.12 Comparing different types of medical and psychosocial services, another trial observed that patients receiving supportive-expressive psychotherapy and those receiving drug counselling had similar proportions of opiate-positive urine samples, but the benefits of psychotherapy persisted for at least 6 months after the end of therapy, whereas those of drug counselling were not sustained.18
Another aspect of programme delivery is the offer of take-home incentives contingent on certain behaviours by clients. Contingent reinforcement has been shown to be an effective method by which methadone maintenance can reduce illicit opiate use8,13,14 and promote client attendance of other services that may prove effective in treating some of the problems of illicit opiate use.11 These trials demonstrated that the potency of take-home reinforcement was directly related to the size of reward and that relatively immediate delivery of take-home rewards following initiation of abstinence and long-term treatment were necessary conditions for achieving therapeutic benefit.
A third aspect of programme delivery is the community reinforcement approach. This refers to the provision of behavioural skills sessions intended to reinforce abstinence. A US trial of mainly Hispanic clients with comorbid psychiatric and drug disorders observed that subjects who participated in the methadone maintenance plus community reinforcement programme were more likely to abstain from opiates for more than 3 weeks (89% versus 78%) than subjects on methadone alone.7 No differences were found in terms of treatment retention.
Outcomes
Maintenance treatment with methadone or with buprenorphine has been proven to be effective in reducing illicit opiate use, stimulating abstinence, and promoting retention in treatment. Illicit opiate use as measured by the proportion of opiate-positive urine samples ranged from 21% to 72% with methadone and from 32% to 94% with buprenorphine (Table 1). The proportion of subjects who are abstinent from opiates for more than 3 weeks varied between 23% and 67% with methadone and between 14% and 41% with buprenorphine.44,49 The rate of treatment retention ranged from 19% to 90% with methadone and from 20% to 78% with buprenorphine (Table 1).
Comparing methadone with buprenorphine, their effectiveness is similar in terms of reduction in illicit opiate use,39,42,47,50,51 reduction in cocaine use,39,42,47,49,50 retention in treatment,38-42,47,50 withdrawal severity,41,47 and quality of life.47 Although several trials found that methadone was superior to buprenorphine in terms of treatment retention,40,44,48 this finding may have been due to the comparison of non-equivalent doses of methadone and buprenorphine or buprenorphine doses that were too low for those subjects with higher levels of dependence.
Quality of the evidence
The quality of the randomised controlled trials was variable. Although the majority of trials have employed randomisation and stratification, and have blinded the people providing and receiving care to treatment assignment, individual studies still suffered from a variety of biases. Systematic differences in the characteristics of treatment groups were not adequately controlled for and may have contributed to differences in effectiveness results (that is, selection bias).9,10,13 Although most trials employed fixed doses of medication, several trials compared variable dose schemes.17-46,48,50 This complicates the interpretation of dose effects and may lead to performance bias. However, a flexible dosing schedule more closely simulates clinical practice and improves the transferability of the results to a community setting. The risk of attrition bias related to high drop-out rates in the group on buprenorphine. This usually reflected inadequate induction doses of buprenorphine.47,48
Additionally, the sample size may have been too small to be able to show statistically significant differences in a number of studies.8,9,11,13,23,33-35 Despite the fact that community maintenance therapies with methadone or buprenorphine often require a prolonged period to achieve maximal effect, the duration of treatment in some trials was too short to be able to fully assess the effectiveness of the maintenance programme.13,19,23,33-35
DISCUSSION
Summary of main findings
There was an extensive amount of literature investigating the effectiveness of community maintenance with methadone or buprenorphine. This body of evidence supports its effectiveness in a range of specific population groups, subject to the caveat that trials enrolled subjects who volunteered to participate and were not necessarily representative of the wider population of opiate-dependent subjects. Evidence is emerging that the provision of methadone or buprenorphine by primary care physicians is feasible and may be effective. Higher doses of methadone and buprenorphine are more effective at enhancing treatment retention and reducing illicit opiate use. Low-dose methadone (20 mg per day) is less effective than buprenorphine (2–8 mg per day). Higher doses of methadone (>50 mg per day) are slightly more effective than buprenorphine (2–8 mg per day). Less-than-daily buprenorphine dosing regimens are effective, although the frequency of buprenorphine dosing regimens is limited to five times the maintenance dose every 120 hours. The few trials evaluating additional services provided in the context of methadone maintenance treatment showed that methadone maintenance without additional services may be a pragmatic, but not a sufficient medical response to opiate dependence.
Implications for clinical practice
Given that current policy in many countries places heavy emphasis on substitute prescribing, the most important question is whether community maintenance therapies are effective. The evidence strongly suggests that maintenance prescribing for opiate dependence is indeed effective using methadone or buprenorphine.
With respect to community maintenance with methadone, guidelines like those used in the UK54,55 need to clearly reinforce a recommendation that higher doses of methadone are more effective. This is important because surveys of current prescribing practices of GPs in the UK suggest that methadone may still be underdosed.56 The fact that the administration of methadone doses needs to be supervised should also be emphasised in guidelines. In many of the US-based studies of methadone maintenance, subjects were required to attend clinics daily and the drug administration was supervised by a nurse or pharmacist. Current UK guidelines suggest that methadone supervision occurs for a minimum 3 months after initiation of treatment as part of a stabilisation phase.54,55
As an alternative to methadone maintenance, the evidence suggests that buprenorphine can be effectively used and that buprenorphine may even be more effective than methadone, depending on dose. There may be reluctance to use buprenorphine due to its potential and historical experience for misuse. However, it is possible to prescribe buprenorphine daily or even less frequently, so that pharmacy supervision (as used in the UK, Australia, and New Zealand) is still possible, although perhaps more challenging than supervising methadone consumption, due to its sublingual formulation.
Finally, the review indicated that evidence is emerging in favour of primary care treatment with methadone and buprenorphine. However, this is perhaps only feasible for subjects who meet criteria of sufficient clinical stability. Moreover, appropriate training of primary care physicians is essential. This is in line with advice in current UK guidelines.54,55
Implications for future research
The review of the literature highlighted a number of gaps in the evidence base relating to the effectiveness of community maintenance with methadone or buprenorphine. Future research needs to evaluate the effectiveness of maintenance treatment in primary care settings and identify the sub-population of opiate-dependent subjects for whom primary care-based treatment may be suitable. In terms of the intensity of treatment, any further studies need to investigate the most appropriate starting dose of methadone and buprenorphine, examine a more extensive range of dosages, explore the effectiveness of less frequent dosing regimens with multiples of the daily dose of buprenorphine, and determine optimal treatment length and the long-term effectiveness of community maintenance with methadone or buprenorphine. Another avenue for future research is to determine what type and intensity of medical, psychosocial and behavioural services provided in the context of community maintenance is most effective. Finally, more information is required about the effectiveness of community maintenance in terms of secondary outcome measures (employment status, housing, education, crime rates, quality of life, and level of injecting).
Supplementary Material
Acknowledgments
This paper was based on a report Effectiveness of treatment for opiate dependent drug users: an international systematic review of the evidence commissioned by the Effective Interventions Unit of the Scottish Executive in 2002 (https://www.scotland.gov.uk/library5/health/isrem-00.asp). During the writing process of this paper, the findings of the report have been substantially extended and updated. The views expressed in this paper are those of the authors and not the Effective Interventions Unit. The authors would like to thank the two anonymous referees for their useful comments on an earlier version of this paper.
Funding body
Effective Interventions Unit of the Scottish Executive
Competing interests
None
REFERENCES
- 1.Davoli M, Perucci CA, Rapiti E, et al. A persistent rise in mortality among injection drug users in Rome, 1980 through 1992. Am J Public Health. 1997;87:851–853. doi: 10.2105/ajph.87.5.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hagan H, Thiede H, Weiss NS, et al. Sharing of drug preparation equipment as a risk factor for hepatitis C. Am J Public Health. 2001;91:42–46. doi: 10.2105/ajph.91.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mark TL, Woody GE, Juday T, Kleber HD. The economic costs of heroin addiction in the United States. Drug Alcohol Depend. 2001;61:195–206. doi: 10.1016/s0376-8716(00)00162-9. [DOI] [PubMed] [Google Scholar]
- 4.Mattick RP, Kimber J, Breen C, Davoli M. The Cochrane Library. Issue 4. Oxford: Update Software; 2003. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence (Cochrane Review) In: Cochrane Collaboration. [DOI] [PubMed] [Google Scholar]
- 5.Cochrane Collaboration. Cochrane reviewers' handbook 4.1.4. Updated October 2001. http://www.cochrane.org/resources/handbook/index.htm (accessed 22 December 2004.)
- 6.West SL, O'Neal KK, Graham CW. A meta-analysis comparing the effectiveness of buprenorphine and methadone. J Subst Abuse. 2000;12:405–414. doi: 10.1016/s0899-3289(01)00054-2. [DOI] [PubMed] [Google Scholar]
- 7.Abbott PJ, Weller SB, Delaney HD, Moore BA. Community reinforcement approach in the treatment of opiate addicts. Am J Drug Alcohol Abuse. 1998;24:17–30. doi: 10.3109/00952999809001696. [DOI] [PubMed] [Google Scholar]
- 8.Chutuape MA, Silverman K, Stitzer ML. Use of methadone take-home contingencies with persistent opiate and cocaine abusers. J Subst Abuse Treat. 1999;16:23–30. doi: 10.1016/s0740-5472(97)00318-8. [DOI] [PubMed] [Google Scholar]
- 9.Curran HV, Bolton J, Wanigaratne S, Smyth C. Additional methadone increases craving for heroin: a double-blind, placebo-controlled study of chronic opiate users receiving methadone substitution treatment. Addiction. 1999;94:665–674. doi: 10.1046/j.1360-0443.1999.9456654.x. [DOI] [PubMed] [Google Scholar]
- 10.Fiellin DA, O'Connor PG, Chawarski M, et al. Methadone maintenance in primary care. A randomised controlled trial. JAMA. 2001;286:1724–1731. doi: 10.1001/jama.286.14.1724. [DOI] [PubMed] [Google Scholar]
- 11.Kidorf M, Stitzer ML, Brooner RK, Goldberg J. Contingent methadone take-home doses reinforce adjunct therapy attendance of methadone maintenance patients. Drug Alcohol Depend. 1994;36:221–226. doi: 10.1016/0376-8716(94)90148-1. [DOI] [PubMed] [Google Scholar]
- 12.McLellan AT, Arndt IO, Metzger DS, et al. The effects of psychosocial services in substance abuse treatment. JAMA. 1993;269:1953–1959. [PubMed] [Google Scholar]
- 13.Preston KL, Umbricht A, Epstein DH. Methadone dose increase and abstinence reinforcement for treatment of continued heroin use during methadone maintenance. Arch Gen Psychiatry. 2000;57:395–404. doi: 10.1001/archpsyc.57.4.395. [DOI] [PubMed] [Google Scholar]
- 14.Preston KL, Umbricht A, Epstein DH. Abstinence reinforcement maintenance contingency and one-year follow up. Drug Alcohol Depend. 2002;67:125–137. doi: 10.1016/s0376-8716(02)00023-6. [DOI] [PubMed] [Google Scholar]
- 15.Sees KL, Delucchi KL, Masson C, et al. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence. JAMA. 2000;283:1303–1310. doi: 10.1001/jama.283.10.1303. [DOI] [PubMed] [Google Scholar]
- 16.Strain EC, Stitzer ML, Liebson IA, Bigelow GE. Dose-response effects of methadone in the treatment of opioid dependence. Ann Intern Med. 1993;119:23–27. doi: 10.7326/0003-4819-119-1-199307010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Strain EC, Bigelow GE, Liebson IA, Stitzer ML. Moderate- vs high-dose methadone in the treatment of opioid dependence: a randomised trial. JAMA. 1999;281:1000–1005. doi: 10.1001/jama.281.11.1000. [DOI] [PubMed] [Google Scholar]
- 18.Woody GE, McLellan AT, Luborsky L, O'Brien CP. Psychotherapy in community methadone programs: a validation study. Am J Psychiatry. 1995;152:1302–1308. doi: 10.1176/ajp.152.9.1302. [DOI] [PubMed] [Google Scholar]
- 19.Yancovitz SR, Des Jarlais DC, Peyser NP, et al. A randomised trial of an interim methadone maintenance clinic. Am J Public Health. 1991;81:1185–1191. doi: 10.2105/ajph.81.9.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmadi J. Buprenorphine maintenance treatment of heroin dependence: the first experience from Iran. J Subst Abuse Treat. 2002;22:157–159. doi: 10.1016/s0740-5472(02)00222-2. [DOI] [PubMed] [Google Scholar]
- 21.Ahmadi J. A controlled trial of buprenorphine treatment for opium dependence: the first experience from Iran. Drug Alcohol Depend. 2002;66:111–114. doi: 10.1016/s0376-8716(01)00202-2. [DOI] [PubMed] [Google Scholar]
- 22.Amass L, Bickel WK, Higgins ST, Badger GJ. Alternate-day dosing during buprenorphine treatment of opioid dependence. Life Sci. 1994;54:1215–1228. doi: 10.1016/0024-3205(94)00848-5. [DOI] [PubMed] [Google Scholar]
- 23.Amass L, Bickel WK, Crean JP, et al. Alternate-day buprenorphine dosing is preferred to daily dosing by opioid-dependent humans. Psychopharmacology. 1998;136:217–225. doi: 10.1007/s002130050559. [DOI] [PubMed] [Google Scholar]
- 24.Bickel WK, Amass L, Crean JP, Badger GJ. Buprenorphine dosing every 1, 2, or 3 days in opioid-dependent patients. Psychopharmacology. 1999;146:111–118. doi: 10.1007/s002130051096. [DOI] [PubMed] [Google Scholar]
- 25.Perez de los Cobos JP, Martin S, Etcheberrigaray A, et al. A controlled trial of daily versus thrice-weekly buprenorphine administration for the treatment of opioid dependence. Drug Alcohol Depend. 2000;59:223–233. doi: 10.1016/s0376-8716(99)00122-2. [DOI] [PubMed] [Google Scholar]
- 26.Eissenberg T, Bigelow GE, Strain EC, et al. Dose-related efficacy of levomethadyl acetate for treatment of opioid dependence. A randomised clinical trial. JAMA. 1997;277:1945–1951. [PubMed] [Google Scholar]
- 27.Greenwald MK, Johanson CE, Schuster CR. Opioid reinforcement in heroin dependent volunteers during outpatient buprenorphine maintenance. Drug Alcohol Depend. 1999;56:191–203. doi: 10.1016/s0376-8716(99)00032-0. [DOI] [PubMed] [Google Scholar]
- 28.Greenwald MK, Schuh KJ, Hopper JA, et al. Effects of buprenorphine sublingual tablet maintenance on opioid drug-seeking behaviour by humans. Psychopharmacology. 2002;160:344–352. doi: 10.1007/s00213-001-0975-0. [DOI] [PubMed] [Google Scholar]
- 29.Gross A, Jacobs EA, Petry NM, Badger GJ, Bickel WK. Limits to buprenorphine dosing: a comparison between quintuple and sextuple the maintenance dose every 5 days. Drug Alcohol Depend. 2001;64:111–116. doi: 10.1016/s0376-8716(00)00227-1. [DOI] [PubMed] [Google Scholar]
- 30.Johnson RE, Eissenberg T, Stitzer ML, et al. A placebo controlled clinical trial of buprenorphine as a treatment for opioid dependence. Drug Alcohol Depend. 1995;40:17–25. doi: 10.1016/0376-8716(95)01186-2. [DOI] [PubMed] [Google Scholar]
- 31.Ling W, Charuvastra C, Collins JF, et al. Buprenorphine maintenance treatment of opiate dependence: a multicenter, randomised clinical trial. Addiction. 1998;93:475–486. doi: 10.1046/j.1360-0443.1998.9344753.x. [DOI] [PubMed] [Google Scholar]
- 32.O'Connor PG, Oliveto AH, Shi JM, et al. A randomised trial of buprenorphine maintenance for heroin dependence in a primary care clinic for substance users versus a methadone clinic. Am J Med. 1998;105:100–105. doi: 10.1016/s0002-9343(98)00194-6. [DOI] [PubMed] [Google Scholar]
- 33.Petry NM, Bickel WK, Badger GJ. A comparison of four buprenorphine dosing regimens in the treatment of opioid dependence. Clin Pharmacol Ther. 1999;66:306–314. doi: 10.1016/S0009-9236(99)70039-1. [DOI] [PubMed] [Google Scholar]
- 34.Petry NM, Bickel WK, Badger GJ. A comparison of four buprenorphine dosing regimens using open-dosing procedures: is twice-weekly dosing possible? Addiction. 2000;95:1069–1077. doi: 10.1046/j.1360-0443.2000.95710698.x. [DOI] [PubMed] [Google Scholar]
- 35.Petry NM, Bickel WK, Badger GJ. Examining the limits of the buprenorphine interdosing interval: daily, every-third-day and every-fifth-day dosing regimens. Addiction. 2001;96:823–834. doi: 10.1046/j.1360-0443.2001.9668234.x. [DOI] [PubMed] [Google Scholar]
- 36.Resnick RB, Galanter M, Pycha C, et al. Buprenorphine: an alternative to methadone for heroin dependence treatment. Psychopharmacol Bull. 1992;28:109–113. [PubMed] [Google Scholar]
- 37.Schottenfeld RS, Pakes JR, O'Connor P, et al. Thrice-weekly versus daily buprenorphine maintenance. Biol Psychiatry. 2000;47:1072–1079. doi: 10.1016/s0006-3223(99)00270-x. [DOI] [PubMed] [Google Scholar]
- 38.Ahmadi J. Methadone versus buprenorphine maintenance for the treatment of heroin-dependent outpatients. J Subst Abuse Treat. 2003;24:217–220. doi: 10.1016/s0740-5472(03)00024-2. [DOI] [PubMed] [Google Scholar]
- 39.Eder H, Fischer G, Gombas W, et al. Comparison of buprenorphine and methadone maintenance in opiate addicts. Eur Addict Res. 1998;4:3–7. doi: 10.1159/000052034. [DOI] [PubMed] [Google Scholar]
- 40.Fischer G, Gombas W, Eder H, et al. Buprenorphine versus methadone maintenance for the treatment of opioid dependence. Addiction. 1999;94:1337–1347. doi: 10.1046/j.1360-0443.1999.94913376.x. [DOI] [PubMed] [Google Scholar]
- 41.Johnson RE, Fudala PJ, Jaffe JH. Outpatient comparison of buprenorphine and methadone maintenance. I. Effects on opiate use and self-reported adverse effects and withdrawal symptomatology. NIDA Res Monogr. 1991;105:585–586. [PubMed] [Google Scholar]
- 42.Johnson RE, Jaffe JH, Fudala PJ. A controlled trial of buprenorphine treatment for opioid dependence. JAMA. 1992;267:2750–2755. [PubMed] [Google Scholar]
- 43.Johnson R, Chutuape M, Strain E, et al. A comparison of levomethadyl acetate, buprenorphine and methadone for opioid dependence. N Engl J Med. 2000;343:1290–1297. doi: 10.1056/NEJM200011023431802. [DOI] [PubMed] [Google Scholar]
- 44.Kosten TR, Schottenfeld R, Ziedonis D, Falcioni J. Buprenorphine versus methadone maintenance for opioid dependence. J Nerv Ment Dis. 1993;181:358–364. doi: 10.1097/00005053-199306000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Ling W, Wesson DR, Charuvastra C, Klett CJ. A controlled trial comparing buprenorphine and methadone maintenance in opioid dependence. Arch Gen Psychiatry. 1996;53:401–407. doi: 10.1001/archpsyc.1996.01830050035005. [DOI] [PubMed] [Google Scholar]
- 46.Mattick RP, Ali R, White JM, et al. Buprenorphine versus methadone maintenance therapy: a randomized double-blind trial with 405 opioid-dependent patients. Addiction. 2003;98:441–452. doi: 10.1046/j.1360-0443.2003.00335.x. [DOI] [PubMed] [Google Scholar]
- 47.Pani PP, Maremmani I, Pirastu R, et al. Buprenorphine: a controlled clinical trial in the treatment of opioid dependence. Drug Alcohol Depend. 2000;60:39–50. doi: 10.1016/s0376-8716(99)00140-4. [DOI] [PubMed] [Google Scholar]
- 48.Petitjean S, Stohler R, Deglon JJ, et al. Double-blind randomised trial of buprenorphine and methadone in opiate dependence. Drug Alcohol Depend. 2001;62:97–104. doi: 10.1016/s0376-8716(00)00163-0. [DOI] [PubMed] [Google Scholar]
- 49.Schottenfeld RS, Pakes JR, Oliveto A, et al. Buprenorphine vs methadone maintenance treatment for concurrent opioid dependence and cocaine abuse. Arch Gen Psychiatry. 1997;54:713–720. doi: 10.1001/archpsyc.1997.01830200041006. [DOI] [PubMed] [Google Scholar]
- 50.Strain EC, Stitzer ML, Liebson IA, Bigelow GE. Comparison of buprenorphine and methadone in the treatment of opioid dependence. Am J Psychiatry. 1994;151:1025–1030. doi: 10.1176/ajp.151.7.1025. [DOI] [PubMed] [Google Scholar]
- 51.Uehlinger C, Deglon JJ, Livoti S, et al. Comparison of buprenorphine and methadone in the treatment of opioid dependence. Eur Addict Res. 1998;4:13–18. doi: 10.1159/000052036. [DOI] [PubMed] [Google Scholar]
- 52.Information and Statistics Division. Drug Misuse Statistics, 2001. Edinburgh: Scottish Executive; 2002. [Google Scholar]
- 53.Krantz MJ, Mehler PS. Treating opioid dependence. Growing implications for primary care. Arch Intern Med. 2004;164(3):277–288. doi: 10.1001/archinte.164.3.277. [DOI] [PubMed] [Google Scholar]
- 54.Department of Health, Scottish Home and Health Department, Welsh Office. Drug misuse and dependence: guidelines on clinical management. London: The Stationery Office; 1999. [Google Scholar]
- 55.Royal College of General Practitioners. Royal College of General Practitioners Guidance for the use of buprenorphine for the treatment of opioid dependence in primary care. London: Royal College of General Practitioners; 2004. [Google Scholar]
- 56.Matheson C, Pitcairn J, Bond CM, et al. General practice management of illicit drug users in Scotland: a national survey. Addiction. 2003;98:119–126. doi: 10.1046/j.1360-0443.2003.00263.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


