Abstract
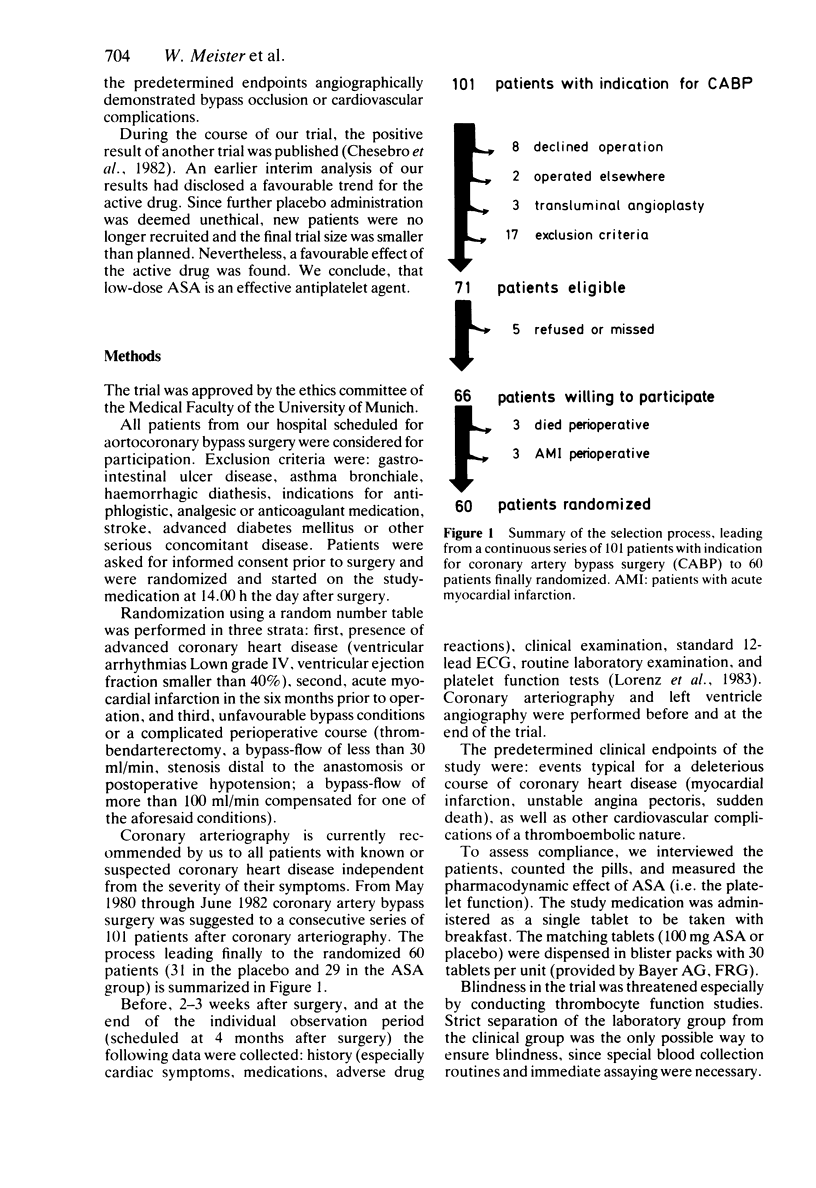
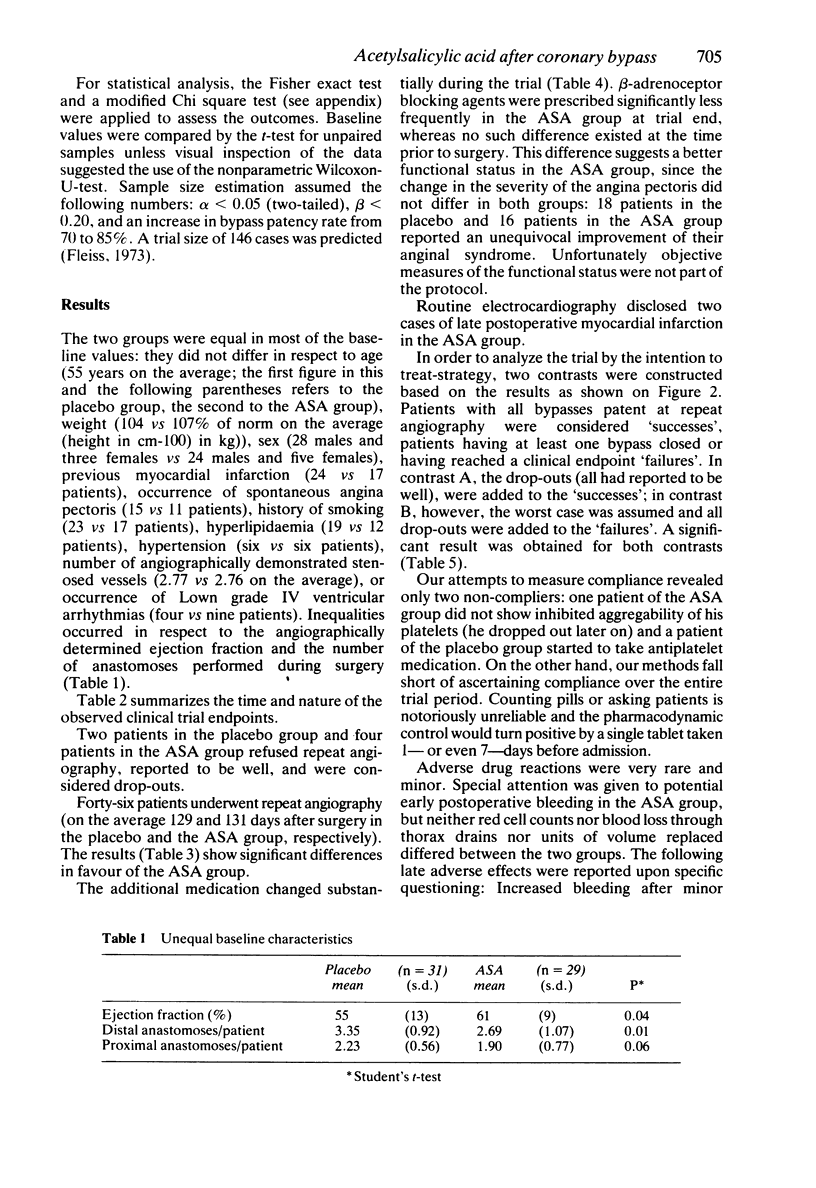
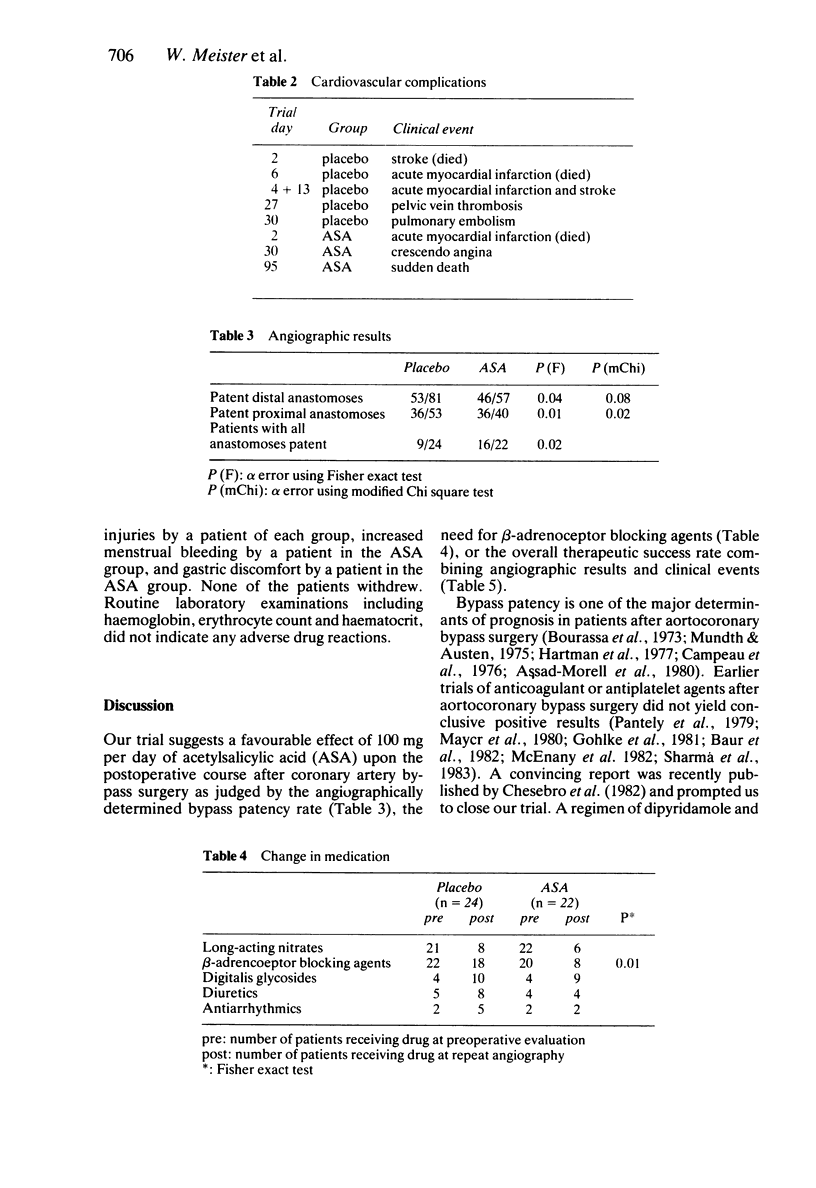
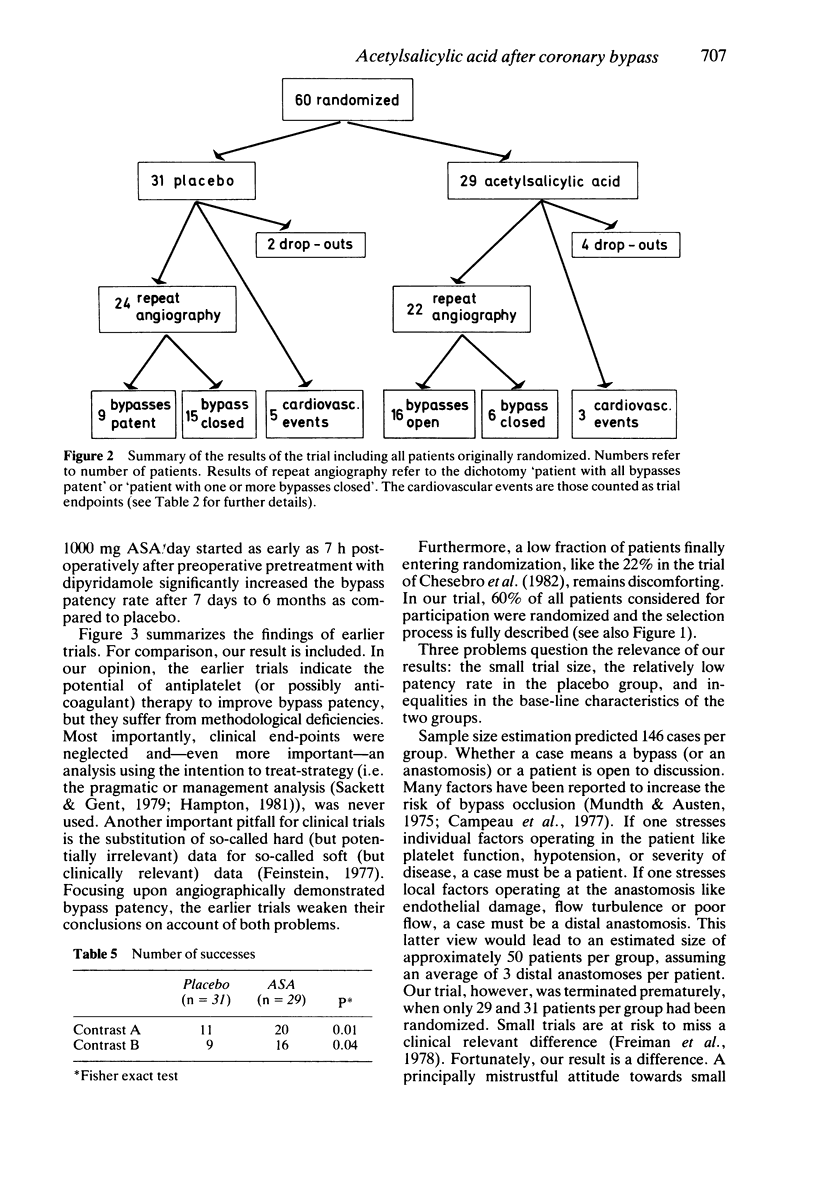
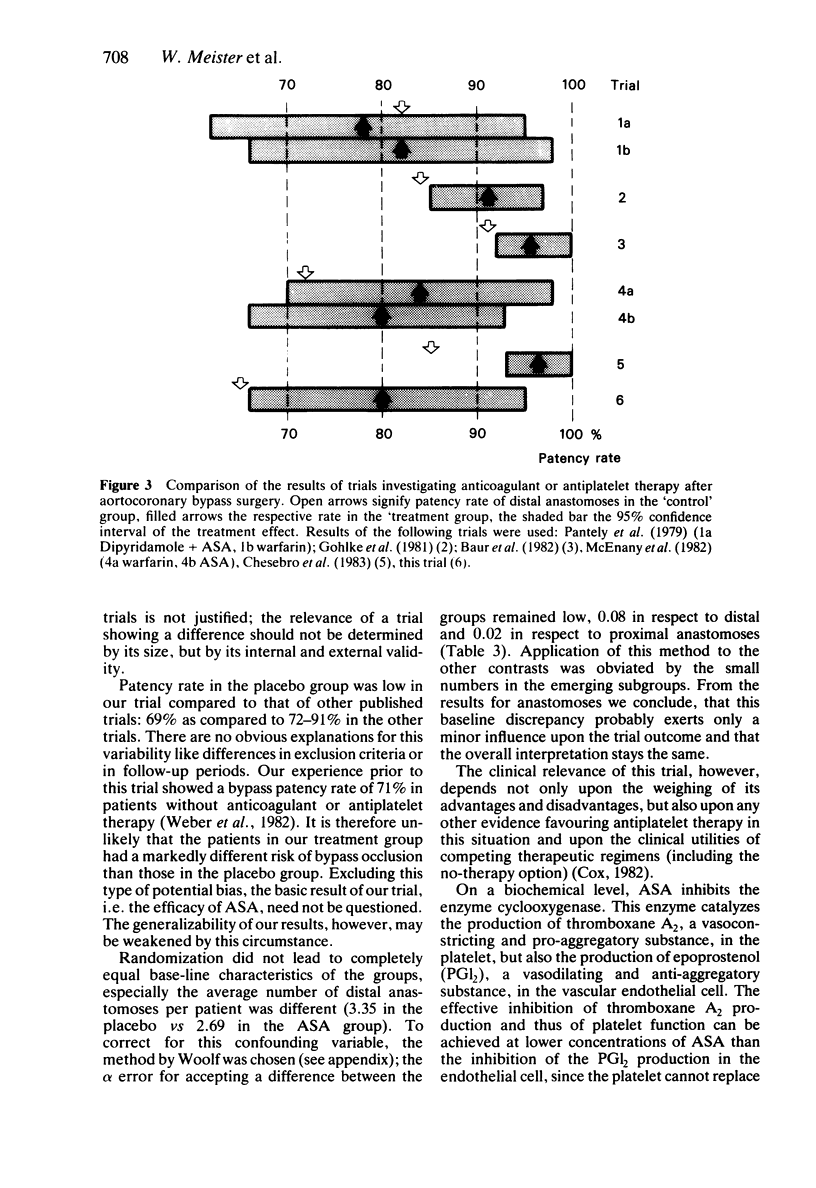
The effect of low-dose acetylsalicylic acid (100 mg/day) upon bypass patency-rate and clinical course after aortocoronary bypass surgery was investigated in a randomized, placebo-controlled clinical trial. Sixty patients with 143 distal anastomoses of bypasses were randomized, 46 underwent repeat angiography after 4 months. Using the intention to treat-strategy, treatment was superior to placebo as judged by bypass patency rate and occurrence of cardiovascular complications or death. Counting the six drop-outs as failures, only nine of the 31 patients of the placebo group, but 16 of the 29 patients of the treatment group were considered successes (P less than 0.04). Eighteen patients in the placebo group and eight patients of the treatment group received beta-adrenoceptor blockers postoperatively, suggesting again a favourable effect of the treatment. Adverse drug reactions were very rare and minor. Supported by pathophysiological insights and positive trends in similar trials, the positive result justifies the recommendation of prescribing 100 mg of acetylsalicylic acid once daily to all patients without contraindications after aortocoronary bypass surgery. The positive result of this trial warrants further clinical trials of low-dose acetylsalicylic acid for other indications in arterial diseases.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Assad-Morell J. L., Frye R. L., Connolly D. C., Davis G. D., Pluth J. R., Wallace R. B., Barnhorst D. A., Elveback L. R., Danielson G. K. Aorta-coronary artery saphenous vein bypass surgery: clinical and angiographic results. Mayo Clin Proc. 1975 Jul;50(7):379–386. [PubMed] [Google Scholar]
- Baur H. R., VanTassel R. A., Pierach C. A., Gobel F. L. Effects of sulfinpyrazone on early graft closure after myocardial revascularization. Am J Cardiol. 1982 Feb 1;49(2):420–424. doi: 10.1016/0002-9149(82)90519-7. [DOI] [PubMed] [Google Scholar]
- Chesebro J. H., Clements I. P., Fuster V., Elveback L. R., Smith H. C., Bardsley W. T., Frye R. L., Holmes D. R., Jr, Vlietstra R. E., Pluth J. R. A platelet-inhibitor-drug trial in coronary-artery bypass operations: benefit of perioperative dipyridamole and aspirin therapy on early postoperative vein-graft patency. N Engl J Med. 1982 Jul 8;307(2):73–78. doi: 10.1056/NEJM198207083070201. [DOI] [PubMed] [Google Scholar]
- Cox D. R. Statistical significance tests. Br J Clin Pharmacol. 1982 Sep;14(3):325–331. doi: 10.1111/j.1365-2125.1982.tb01987.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein A. R. Clinical biostatistics. XLI. Hard science, soft data, and the challenges of choosing clinical variables in research. Clin Pharmacol Ther. 1977 Oct;22(4):485–498. doi: 10.1002/cpt1977224485. [DOI] [PubMed] [Google Scholar]
- Freiman J. A., Chalmers T. C., Smith H., Jr, Kuebler R. R. The importance of beta, the type II error and sample size in the design and interpretation of the randomized control trial. Survey of 71 "negative" trials. N Engl J Med. 1978 Sep 28;299(13):690–694. doi: 10.1056/NEJM197809282991304. [DOI] [PubMed] [Google Scholar]
- Hampton J. R. Presentation and analysis of the results of clinical trials in cardiovascular disease. Br Med J (Clin Res Ed) 1981 Apr 25;282(6273):1371–1373. doi: 10.1136/bmj.282.6273.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley S. P., Bevan J., Cockbill S. R., Heptinstall S. Differential inhibition by low-dose aspirin of human venous prostacyclin synthesis and platelet thromboxane synthesis. Lancet. 1981 May 2;1(8227):969–971. doi: 10.1016/s0140-6736(81)91733-5. [DOI] [PubMed] [Google Scholar]
- Harter H. R., Burch J. W., Majerus P. W., Stanford N., Delmez J. A., Anderson C. B., Weerts C. A. Prevention of thrombosis in patients on hemodialysis by low-dose aspirin. N Engl J Med. 1979 Sep 13;301(11):577–579. doi: 10.1056/NEJM197909133011103. [DOI] [PubMed] [Google Scholar]
- Hartman C. W., Kong Y., Margolis J. R., Warren S. G., Peter R. H., Behar V. S., Oldham H. N. Aortocoronary bypass surgery: Correlation of angiographic symptomatic and functional improvement at 1 year. Am J Cardiol. 1976 Mar 4;37(3):352–357. doi: 10.1016/0002-9149(76)90283-6. [DOI] [PubMed] [Google Scholar]
- Lewis H. D., Jr, Davis J. W., Archibald D. G., Steinke W. E., Smitherman T. C., Doherty J. E., 3rd, Schnaper H. W., LeWinter M. M., Linares E., Pouget J. M. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1983 Aug 18;309(7):396–403. doi: 10.1056/NEJM198308183090703. [DOI] [PubMed] [Google Scholar]
- Lorenz R., Siess W., Weber P. C. Effects of very low versus standard dose acetyl salicylic acid, dipyridamole and sulfinpyrazone on platelet function and thromboxane formation in man. Eur J Pharmacol. 1981 Apr 9;70(4):511–518. doi: 10.1016/0014-2999(81)90362-9. [DOI] [PubMed] [Google Scholar]
- Majerus P. W. Arachidonate metabolism in vascular disorders. J Clin Invest. 1983 Nov;72(5):1521–1525. doi: 10.1172/JCI111110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus A. J. Aspirin as an antithrombotic medication. N Engl J Med. 1983 Dec 15;309(24):1515–1517. doi: 10.1056/NEJM198312153092410. [DOI] [PubMed] [Google Scholar]
- Mayer J. E., Jr, Lindsay W. G., Castaneda W., Nicoloff D. M. Influence of aspirin and dipyridamole on patency of coronary artery bypass grafts. Ann Thorac Surg. 1981 Mar;31(3):204–210. doi: 10.1016/s0003-4975(10)60927-7. [DOI] [PubMed] [Google Scholar]
- McEnany M. T., Salzman E. W., Mundth E. D., DeSanctis R. W., Harthorne J. W., Weintraub R. M., Gates S., Austen W. G. The effect of antithrombotic therapy on patency rates of saphenous vein coronary artery bypass grafts. J Thorac Cardiovasc Surg. 1982 Jan;83(1):81–89. [PubMed] [Google Scholar]
- Moncada S. Prostacyclin and arterial wall biology. Arteriosclerosis. 1982 May-Jun;2(3):193–207. doi: 10.1161/01.atv.2.3.193. [DOI] [PubMed] [Google Scholar]
- Mundth E. D., Gerald Austen W. Surgical measures for coronary heart disease (second of three parts). N Engl J Med. 1975 Jul 10;293(2):75–80. doi: 10.1056/NEJM197507102930205. [DOI] [PubMed] [Google Scholar]
- O'Grady J., Moncada S. Aspirin: A paradoxical effect on bleeding-time. Lancet. 1978 Oct 7;2(8093):780–780. doi: 10.1016/s0140-6736(78)92661-2. [DOI] [PubMed] [Google Scholar]
- Pantely G. A., Goodnight S. H., Jr, Rahimtoola S. H., Harlan B. J., DeMots H., Calvin L., Rösch J. Failure of antiplatelet and anticoagulant therapy to improve patency of grafts after coronary-artery bypass: a controlled, randomized study. N Engl J Med. 1979 Nov 1;301(18):962–966. doi: 10.1056/NEJM197911013011803. [DOI] [PubMed] [Google Scholar]
- Porter J., Jick H. Drug-induced anaphylaxis, convulsions, deafness, and extrapyramidal symptoms. Lancet. 1977 Mar 12;1(8011):587–588. doi: 10.1016/s0140-6736(77)92011-6. [DOI] [PubMed] [Google Scholar]
- Sackett D. L., Gent M. Controversy in counting and attributing events in clinical trials. N Engl J Med. 1979 Dec 27;301(26):1410–1412. doi: 10.1056/NEJM197912273012602. [DOI] [PubMed] [Google Scholar]
- Weksler B. B., Pett S. B., Alonso D., Richter R. C., Stelzer P., Subramanian V., Tack-Goldman K., Gay W. A., Jr Differential inhibition by aspirin of vascular and platelet prostaglandin synthesis in atherosclerotic patients. N Engl J Med. 1983 Apr 7;308(14):800–805. doi: 10.1056/NEJM198304073081402. [DOI] [PubMed] [Google Scholar]


