Abstract
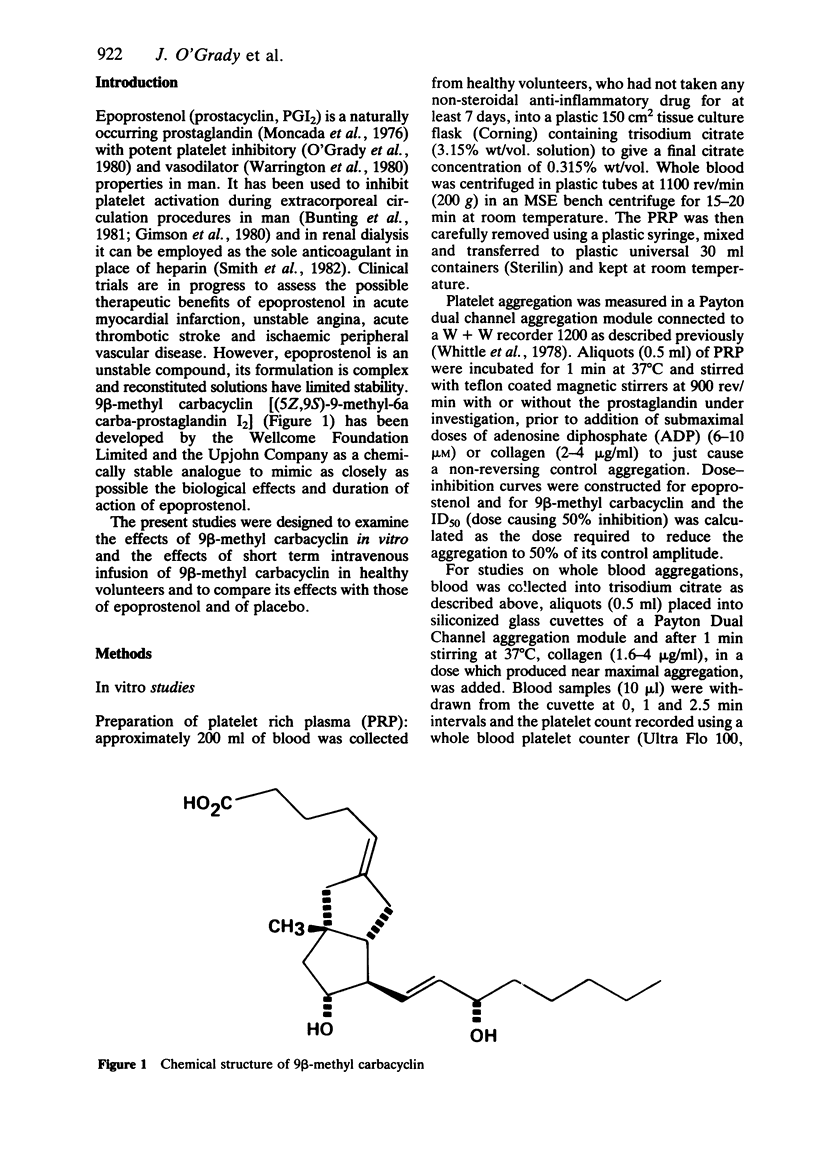
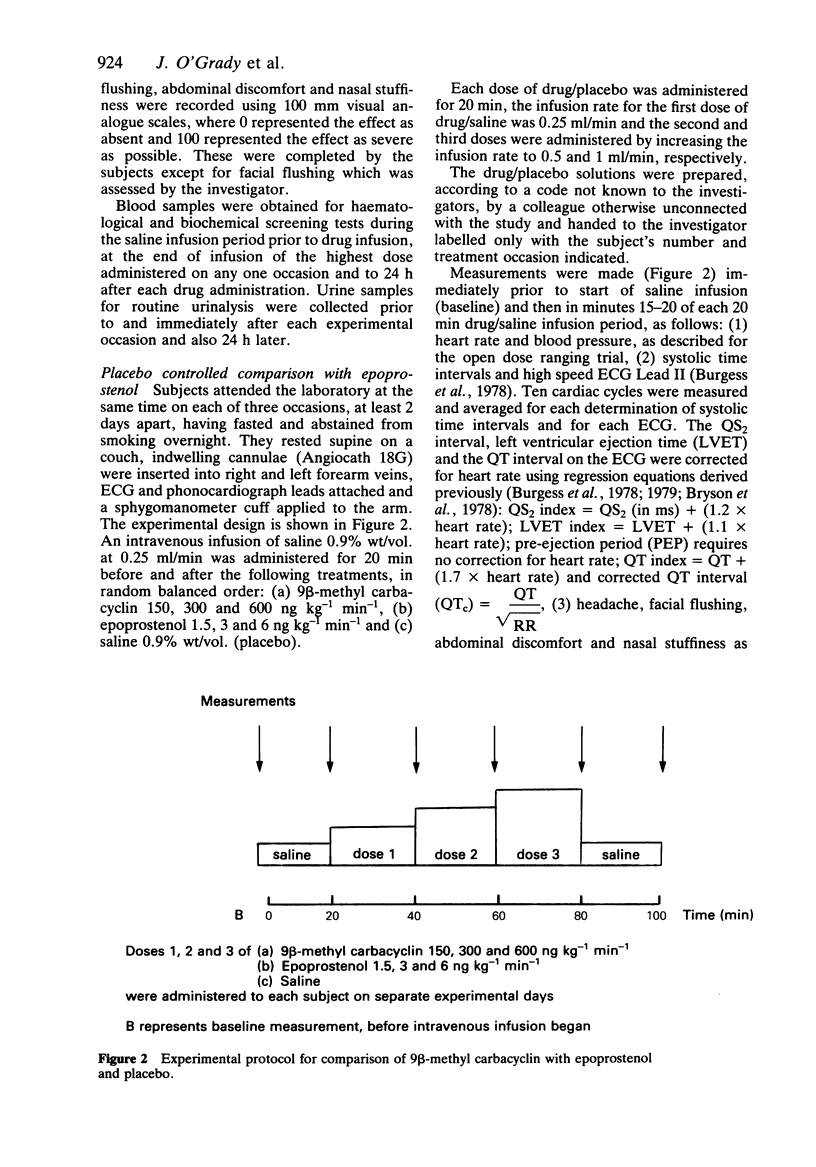
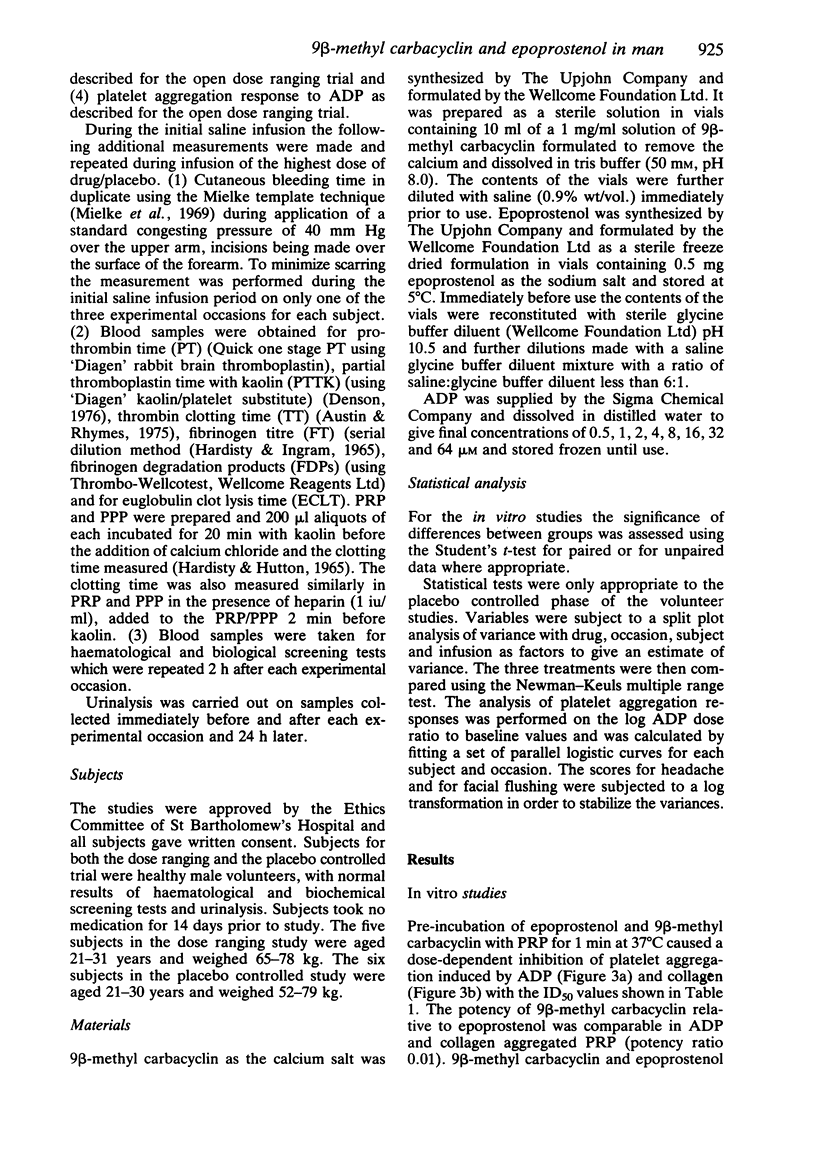
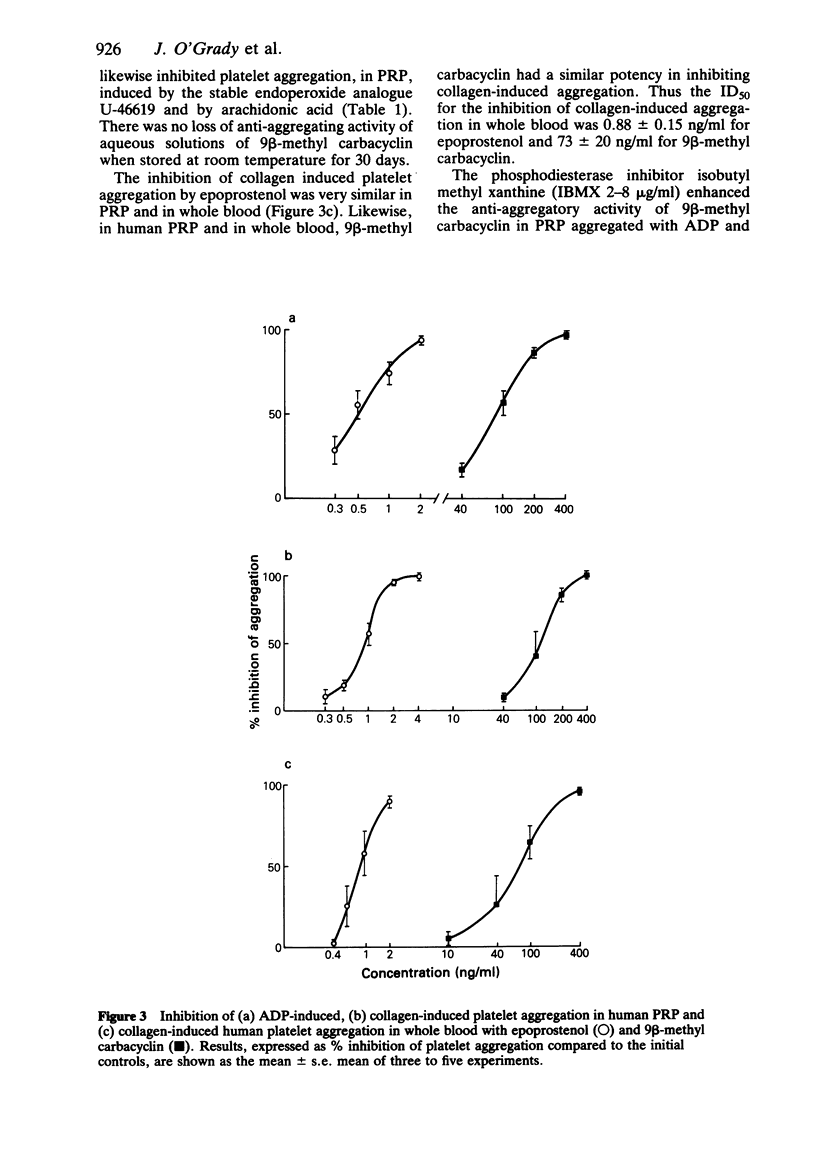
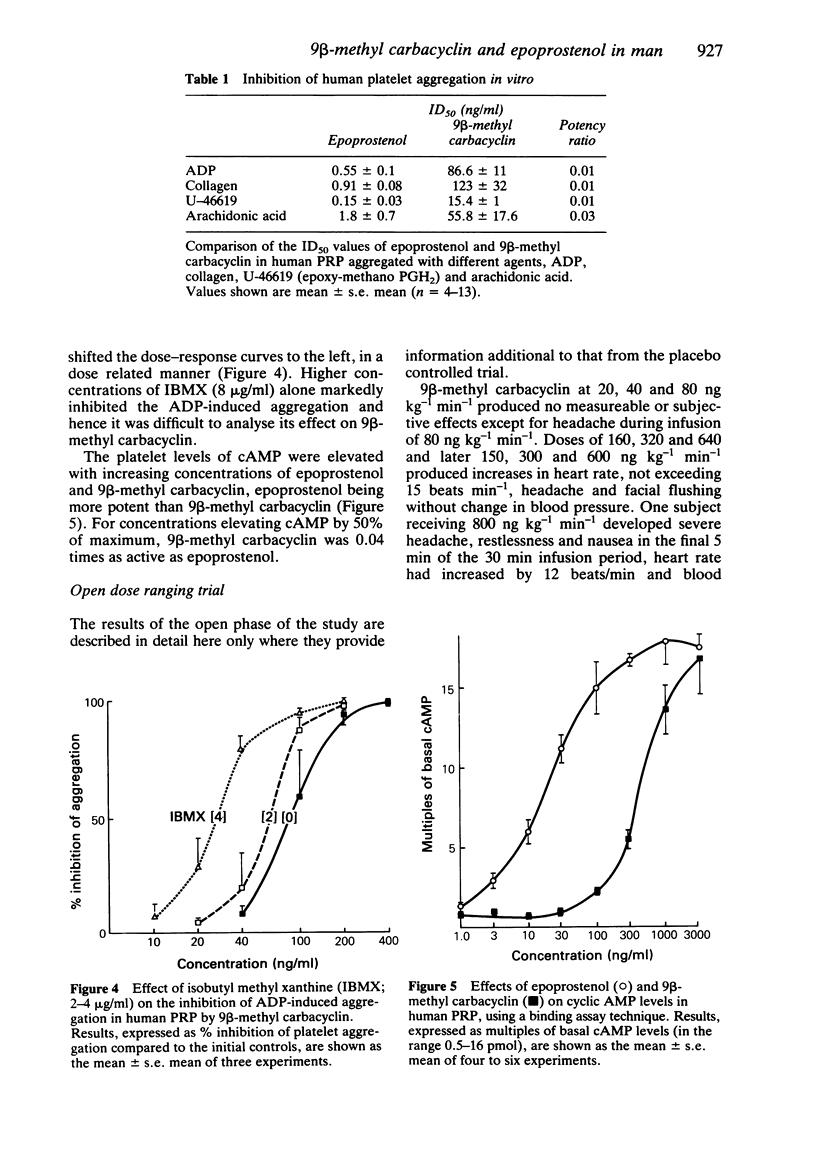
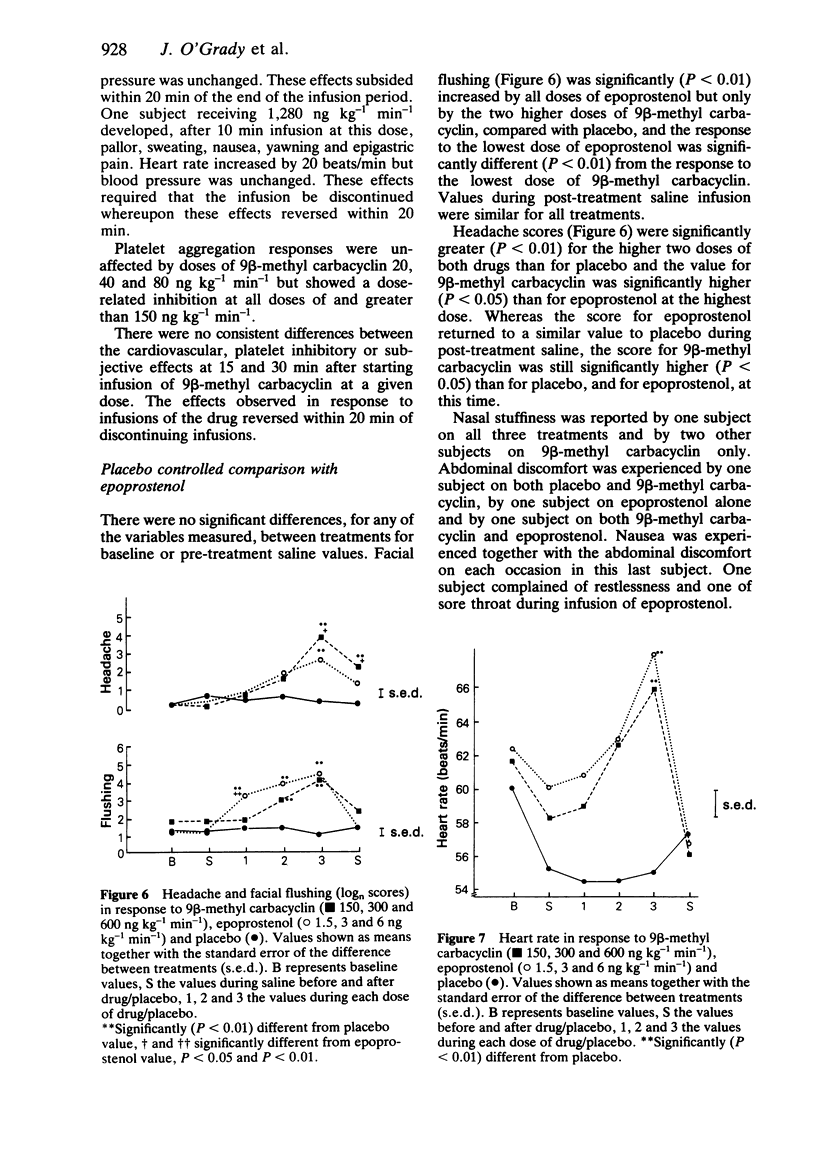
The effects of 9 beta-methyl carbacyclin, a chemically stable analogue of epoprostenol (prostacyclin, PGI2) were studied, in comparison with epoprostenol, both in vitro and in vivo in man. In vitro 9 beta-methyl carbacyclin and epoprostenol inhibited platelet aggregation induced by ADP, collagen, the endoperoxide analogue U46619 and arachidonic acid. The potency of 9 beta-methyl carbacyclin relative to epoprostenol was comparable in ADP and collagen-aggregated platelet rich plasma (PRP), 9 beta-methyl carbacyclin being 0.01 times as active as epoprostenol. The anti-aggregatory potencies of the two compounds were comparable in PRP and whole blood. The phosphodiesterase inhibitor isobutyl methyl xanthine enhanced the anti-aggregatory activity of both compounds in vitro. 9 beta-methyl carbacyclin and epoprostenol elevated platelet cyclic AMP, 9 beta-methyl carbacyclin being 0.04 times as active as epoprostenol. In a placebo controlled trial both drugs produces significant headache and facial flushing when compared with placebo. Nasal stuffiness, abdominal discomfort and nausea were reported on all three treatments. Both drugs caused significant and comparable increase in heart rate and decrease in pre-ejection (PEP) and PEP/left ventricular ejection time (LVET) ratio compared with placebo. Systolic and diastolic blood pressure, LVET and QS2 index were unchanged. Platelet aggregation responses to ADP were significantly inhibited by all three doses of both drugs compared with placebo. Bleeding time was significantly longer during epoprostenol infusion than either placebo or 9 beta-methyl carbacyclin infusion. Neither drug had significant effect, compared with placebo, on kaolin activated clotting time in PPP, PRP or in PRP in the presence of heparin, prothrombin time, partial thromboplastin time, thrombin clotting time, fibrinogen, fibrinogen degradation products or euglobulin clot lysis time. The pharmacodynamic effects and duration of action of 9 beta-methyl carbacyclin and of epoprostenol are similar; 9 beta-methyl carbacyclin is approximately 100 times less potent than epoprostenol in man.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bryson S. M., Whiting B., Lawrence J. R. Disopyramide serum and pharmacologic effect kinetics applied to the assessment of bioavailability. Br J Clin Pharmacol. 1978 Nov;6(5):409–419. doi: 10.1111/j.1365-2125.1978.tb04605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunting S., Simmons P. M., Moncada S. Inhibition of platelet activation by prostacyclin: possible consequences in coagulation and anticoagulation. Thromb Res. 1981 Jan 1;21(1-2):89–102. doi: 10.1016/0049-3848(84)90036-7. [DOI] [PubMed] [Google Scholar]
- Burgess C. D., Turner P., Wadsworth J. Cardiovascular responses to mianserin hydrochloride: a comparison with tricyclic antidepressant drugs. Br J Clin Pharmacol. 1978;5 (Suppl 1):21S–28S. [PMC free article] [PubMed] [Google Scholar]
- Burgess C. D., Wadsworth J., Warrington S. J. Evaluation of some non-invasive indices of cardiovascular function [proceedings]. Br J Clin Pharmacol. 1979 Apr;7(4):436P–437P. doi: 10.1111/j.1365-2125.1979.tb00980.x. [DOI] [PubMed] [Google Scholar]
- Data J. L., Molony B. A., Meinzinger M. M., Gorman R. R. Intravenous infusion of prostacyclin sodium in man: clinical effects and influence on platelet adenosine diphosphate sensitivity and adenosine 3':5'-cyclic monophosphate levels. Circulation. 1981 Jul;64(1):4–12. doi: 10.1161/01.cir.64.1.4. [DOI] [PubMed] [Google Scholar]
- FitzGerald G. A., Friedman L. A., Miyamori I., O'Grady J., Lewis P. J. A double blind placebo controlled crossover study of prostacyclin in man. Life Sci. 1979 Aug 20;25(8):665–672. doi: 10.1016/0024-3205(79)90507-1. [DOI] [PubMed] [Google Scholar]
- Gimson A. E., Langley P. G., Hughes R. D., Canalese J., Mellon P. J., Williams R., Woods H. F., Weston M. J. Prostacyclin to prevent platelet activation during charcoal haemoperfusion in fulminant hepatic failure. Lancet. 1980 Jan 26;1(8161):173–175. doi: 10.1016/s0140-6736(80)90661-3. [DOI] [PubMed] [Google Scholar]
- HARDISTY R. M., HUTTON R. A. THE KAOLIN CLOTTING TIME OF PLATELET-RICH PLASMA: A TEST OF PLATELET FACTOR-3 AVAILABILITY. Br J Haematol. 1965 May;11:258–268. doi: 10.1111/j.1365-2141.1965.tb06586.x. [DOI] [PubMed] [Google Scholar]
- Hassan S., Pickles H., Fish A., Burke C., Warrington S., O'Grady J. The cardiovascular and platelet effects of epoprostenol (prostacyclin, PGI2) are unaffected by beta-adrenoceptor blockade in man. Br J Clin Pharmacol. 1982 Sep;14(3):369–377. doi: 10.1111/j.1365-2125.1982.tb01993.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielke C. H., Jr, Kaneshiro M. M., Maher I. A., Weiner J. M., Rapaport S. I. The standardized normal Ivy bleeding time and its prolongation by aspirin. Blood. 1969 Aug;34(2):204–215. [PubMed] [Google Scholar]
- Moncada S., Gryglewski R., Bunting S., Vane J. R. An enzyme isolated from arteries transforms prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation. Nature. 1976 Oct 21;263(5579):663–665. doi: 10.1038/263663a0. [DOI] [PubMed] [Google Scholar]
- O'Grady J., Warrington S., Moti M. J., Bunting S., Flower R., Fowle A. S., Higgs E. A., Moncada S. Effects of intravenous infusion of prostacyclin (PGI2) in man. Prostaglandins. 1980 Feb;19(2):319–332. doi: 10.1016/0090-6980(80)90030-1. [DOI] [PubMed] [Google Scholar]
- Orchard M. A., Ritter J. M., Shepherd G. L., Lewis P. J. Cardiovascular and platelet effects in man of BW 245C, a stable mimic of epoprostenol (PGI2). Br J Clin Pharmacol. 1983 May;15(5):509–511. doi: 10.1111/j.1365-2125.1983.tb02083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickles H., Fish A., Hassan S., Burke C., Warrington S., O'Grady J. Effects of intravenous epoprostenol on platelets and the cardiovascular system are not potentiated by dipyridamole. Clin Pharmacol Ther. 1983 Feb;33(2):178–182. doi: 10.1038/clpt.1983.27. [DOI] [PubMed] [Google Scholar]
- Pickles H., O'Grady J. Side effects occurring during administration of epoprostenol (prostacyclin, PGI2), in man. Br J Clin Pharmacol. 1982 Aug;14(2):177–185. doi: 10.1111/j.1365-2125.1982.tb01959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah A., Pickles H., Joshi M., Webster A., O'Grady J. Effects of single oral dose administration of a hydantoin prostaglandin analogue BW 245C in man. Life Sci. 1984 Jun 4;34(23):2281–2286. doi: 10.1016/0024-3205(84)90218-2. [DOI] [PubMed] [Google Scholar]
- Smith M. C., Danviriyasup K., Crow J. W., Cato A. E., Park G. D., Hassid A., Dunn M. J. Prostacyclin substitution for heparin in long-term hemodialysis. Am J Med. 1982 Nov;73(5):669–678. doi: 10.1016/0002-9343(82)90409-0. [DOI] [PubMed] [Google Scholar]
- Tateson J. E., Moncada S., Vane J. R. Effects of prostacyclin (PGX) on cyclic AMP concentrations in human platelets. Prostaglandins. 1977 Mar;13(3):389–397. doi: 10.1016/0090-6980(77)90019-3. [DOI] [PubMed] [Google Scholar]
- Warrington S. J., Smith P. R., O'Grady J. Noninvasive assessment of the cardiovascular effects of prostacyclin (PGI2) in man. Eur J Cardiol. 1980;12(2):73–80. [PubMed] [Google Scholar]
- Webster J., Rees A. J., Lewis P. J., Hensby C. N. Prostacyclin deficiency in haemolytic-uraemic syndrome. Br Med J. 1980 Jul 26;281(6235):271–271. doi: 10.1136/bmj.281.6235.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle B. J., Moncada S., Vane J. R. Comparison of the effects of prostacyclin (PGI2), prostaglandin E1 and D2 on platelet aggregation in different species. Prostaglandins. 1978 Sep;16(3):373–388. doi: 10.1016/0090-6980(78)90216-2. [DOI] [PubMed] [Google Scholar]



