Abstract
Objective
To examine the influence of place of graduate medical education (GME), state licensure requirements, presence of established international medical graduates (IMGs), and ethnic communities on the initial practice location choices of new IMGs.
Data Sources
The annual Graduate Medical Education (GME) Survey of the American Medical Association (AMA) and the AMA Physician Masterfile.
Study Design
We identified 19,940 IMGs who completed GME in the United States between 1989 and 1994 and who were in patient care practice 4.5 years later. We used conditional logit regression analysis to assess the effect of market area characteristics on the choice of practice location. The key explanatory variables in the regression models were whether the market area was in the state of GME, the years of GME required for state licensure, the proportion of IMGs among established physicians, and the ethnic composition of the market area.
Principal Findings
The IMGs tended to locate in the same state as their GME training. Foreign-born IMGs were less likely to locate in markets with more stringent licensure requirements, and were more likely to locate in markets with higher proportions of established IMG physicians. The IMGs born in Hispanic or Asian countries were more likely to locate in markets with higher proportions of the corresponding ethnic group.
Conclusions
Policymakers may influence the flow of new IMGs into states by changing the availability of GME positions. IMGs tend to favor the same markets over time, suggesting that networks among established IMGs play a role in attracting new IMGs. Further, IMGs choose their practice locations based on ethnic matching.
Keywords: Physicians, international medical graduates, health economics, physician labor markets, ethnic matching
During the 1960s and early 1970s, there was a consensus that a growing shortage of physicians would soon bring the U.S. health care system to a state of crisis (e.g., Ginzberg et al. 1981), and physician workforce policy welcomed International Medical Graduate (IMG) physicians into the United States. Between 1963 and 1970, the number of IMGs in the United States increased by 85 percent (Haug and Martin 1971).
However, the favored status given to IMGs was short-lived. Responding to newly emerging fears of an impending physician surplus, Congress in 1976 passed legislation that restricted the ability of IMGs to remain in the United States after completion of graduate medical education (GME) (Eiler and Loft 1986). As a result, the inflow of new IMGs decreased in the late 1970s and remained stable throughout the 1980s. Between 1989 and 1994, however, the number of IMGs entering GME programs in the United States nearly doubled to about 25 percent (Council on Graduate Medical Education 1998). The sudden spurt in the number of new IMGs during the early 1990s refocused attention on the contribution of IMGs to the growth of the physician workforce. Motivated by concerns about an oversupply of physicians and the large government expenditures for GME, various policymaking organizations, including the Institute of Medicine (1996), the Pew Health Professions Commission (1995), and the Council on Graduate Medical Education (1998) have recently called for reductions in the number of IMGs in residency programs.
The health policy research community is divided about the role of IMGs in the health care delivery system (e.g., Iglehart 1996). Many analysts believe that the entry of new IMGs exacerbates a nationwide oversupply of physicians (Politzer et al. 1998; Mullan et al. 1995), while others contend that IMGs are especially likely to locate in communities that are underserved by U.S. medical graduates (Mick and Lee 1997; Baer et al. 1998). Mick et al. (2000) examined these issues by comparing the geographical distribution of IMGs and U.S. medical graduates. They found that IMGs were more likely than U.S. graduates to practice in locales characterized as high in medical need or medically underserved, but many IMGs clustered in areas with an already abundant supply of physicians. They concluded that IMGs serve a significant “safety net” role, while simultaneously exacerbating physician surpluses.
The existing research, however, has not directly examined the factors that affect IMGs’ choices of practice location. Numerous studies of the location choices of all new physicians have found that they are attracted to communities with affluent and well-educated populations, medical schools and residency training programs, mild climates, and low levels of health maintenance organization (HMO) penetration (e.g., Ernst and Yett 1985; Escarce et al. 1998). New physicians also tend to locate in communities with which they had prior contact, for example, during upbringing, medical school, or GME (e.g., Ernst and Yett 1985; Seifer et al. 1995).
However, the location choices of IMGs are likely to differ from those of U.S. medical graduates. International medical graduates, especially those from foreign countries, may be more geographically mobile because they are less likely to be connected through family or friends to particular communities in the United States. Differences in state licensure requirements for IMGs, compared with U.S. graduates, may affect their practice location choices. Networks of established IMG physicians may play an important role in helping new IMGs to start their practices. Finally, many foreign-born IMGs, in particular, may have cultural and language differences that are more easily overcome in communities with large numbers of people of the same ethnicity.
This article examines the initial practice location decisions of new IMG physicians who completed their GME between 1989 and 1994. Our study examines the extent to which new IMGs are attracted to market areas with large minority populations and whether this attraction varies with the physician's own ethnicity. We also examine whether new IMG physicians tend to choose practice locations close to where they received GME training, whether their location decisions are affected by state licensure requirements, and whether they are attracted to market areas with established IMGs.
Methods
Conceptual Framework
Our conceptual model views the physician services market as a set ofgeographically distinct, local market areas, with physicians confined to practice in only one of these markets (e.g., Newhouse et al. 1982). We assume that when new physicians choose the location of their first practices, they consider the overall utility, or well-being, attainable in different market areas (Ernst and Yett 1985; Newhouse et al. 1982). Utility, in turn, is influenced by earning opportunities and quality of life.
Earning opportunities depend on: sociodemographic characteristics of the population, which influence the level of demand for physician services; the number of established physicians in the same specialty, who may compete with new physicians but also help to create positions for them; the availability of physicians in other specialties, who may serve as referral sources or consultants; the presence of residency training programs; and the degree of HMO penetration (Escarce et al. 1998). Earning opportunities also depend on the costs of producing physician services, including the prices of nonphysician inputs needed to produce these services. Prior contact with a community (e.g., through GME training) may reduce the costs of acquiring information and other search costs associated with finding a position. Quality of life depends on various nonpecuniary amenities, including climate and proximity to friends and relatives.
Several market characteristics may have an especially important influence on the earning opportunities and quality of life of new IMG physicians. Licensure requirements for IMGs vary by state, causing differences across states in the costs of starting a medical practice. The presence of established IMGs in a market area may help new IMGs start successful practices. In particular, networks of established IMGs may reduce the costs of searching for positions, help to create new positions, and serve as sources of referrals and consultations. Foreign-born IMGs who have a different language or cultural background from the majority of the U.S. population may be attracted to market areas in which many people are of an ethnic background similar to their own. Such markets may offer higher demand for the services of foreign-born IMGs and, consequently, facilitate the development of their practices.
Study Population
The American Medical Association's (AMA) Annual GME Survey collects names and training information for physicians receiving GME training from the directors of all accredited residency and fellowship training programs in the United States. We used this database to identify physicians who completed their most recent GME (residency or fellowship) in the United States between 1989 and 1994. These data were linked with the AMA Physician Masterfile, which provided information on the physicians’ age, sex, birthplace, and medical school, as well as their major professional activity and practice address after the completion of GME.1
From this group, we selected physicians who graduated from medical schools outside the United States or Canada and whose main professional activity 4.5 years after completing GME was direct patient care. Each physician's first practice location was defined as the practice address reported in the year-end Masterfile 4.5 years after completion of GME.2
There are several reasons for using a 4.5-year interval between completion of GME and the date for determining the initial practice location. First, foreign nationals who come to the United States for GME training often do so with an exchange visitor visa, which requires participants to go back to their home countries after completion of GME for at least two years before they can return to the United States as permanent residents (Mullan et al. 1995). The 4.5-year interval allowed time for these individuals to comply with the regulations and then return to the United States to set up their practices. Second, many IMGs have H-1B visas, which allow them to work for three years in the United States after finishing GME, before returning to their home countries. The 4.5-year interval enabled us to exclude from the study physicians who had to go back to their home countries after their H-1B visas expired. Third, the 4.5-year interval allowed the analysis to bypass the temporary jobs many physicians hold while searching for stable practice opportunities (Willke 1991).
We divided the study population into the following 16 specialty groups: general internal medicine, general pediatrics, family medicine, general practice, internal medicine subspecialties (e.g., cardiology, gastroenterology, etc.), pediatric subspecialties, dermatology, neurology, general surgery, obstetrics/gynecology, surgical subspecialties (e.g., ophthalmology, orthopedic surgery, etc.), psychiatry, emergency medicine, radiology, anesthesiology, and pathology. We excluded from the analysis a small number of physicians in other miscellaneous specialties and physicians whose first practice location was outside the 48 contiguous states of the United States.
Statistical Approach
When IMGs choose a market area in which to practice, they make a single choice from among a set of alternatives after considering the attributes of all the alternatives. Our statistical analysis of IMGs’ practice location choices was based on the conditional logit regression model, which was developed to analyze this type of decision making (McFadden 1973; Maddala 1983).
According to the conditional logit model used in this study, the probability that a physician locates in a particular market area is a function of the characteristics of the area relative to the values of these characteristics in other market areas. Specifically, the probability, Pim, that physician i locates in market area m is:
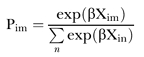 |
where Xin is a vector of market area characteristics for market n as perceived byphysician i, β is a vector of regression coefficients to be estimated, and the summation is over all the market areas where the physician could have located. An important advantage of the conditional logit model is that, in estimating the regression coefficients, it explicitly accounts for the characteristics of the rejected alternatives as well as the one that was chosen, thereby capturing a fundamental aspect of real-life decision making.
The market areas used in the study were the 316 metropolitan areas and the 45 nonmetropolitan portions of states within the contiguous United States.3 The key explanatory variables in the regression model enabled us to assess the importance of market area characteristics in IMGs’ selection of initial practice locations. To assess the effect of prior contact with a community, we included an indicator variable for whether the market area was in the state of most recent GME training. To assess the effect of state licensure requirements, we included a variable measuring the number of years of GME required for IMGs to become licensed in the state.4 To assess the importance of established IMG physicians in the market area, we included the proportion of practicing physicians in 1985 who were IMGs.
Lastly, to assess the effect of the ethnic composition of the market area, we included the proportion of the population with a non-English first language and the proportions of the population who were black, Asian, and Hispanic. In addition, for foreign-born IMGs, we included the interactions between indicator variables for physicians’ own ethnicity (black, Asian, and Hispanic) and the corresponding proportion of the population who were black, Asian, or Hispanic. These interaction terms allowed the model to determine the extent to which the initial location decisions on foreign-born IMGs are influenced by ethnic matching—that is, the tendency for physicians to locate in market areas in which a large proportion of the people are of an ethnic background similar to their own. The ethnicity of each foreign-born IMG was assigned using the physician's country of birth.5 Information on race and ethnicity was unavailable for IMGs who were born in the United States.
Additional market area characteristics used as covariates in the regression model included the logarithm of the population size; the proportion of the population 5 years of age or younger; the proportion 6 to 19 years old; the proportion older than 65 years old; the proportion female; the proportion of adults who finished high school; the proportion of adults who finished college; the poverty rate; and per capita income. Additional market characteristics in the model also included the level of HMO penetration, the physician-to-population ratio for established physicians in the same specialty, the physician-to-population ratio for established physicians in other specialties, an index of physician practice costs (i.e., office rents, wages of nonphysician personnel, and malpractice premiums), the number of hospitals with residency training programs, the mean January temperature in the market area, and an indicator variable for nonmetropolitan areas.
Data on most of the market area characteristics were obtained from the Area Resource File. The index of physician practice costs was obtained from a published report (Zuckerman et al. 1990), and HMO penetration was obtained from Baker (1997). Information on state licensure requirements was obtained from the AMA (1992).
We estimated separate regression models for six analytic subgroups of IMGs, stratified by place of birth (foreign-born or U.S.-born) and specialty group (generalists, medical/surgical specialists, or hospital-based specialists).6 A significant positive value of a coefficient indicates that IMGs were more likely to locate in market areas with higher values of the particular characteristic, other things equal, whereas a significant negative value indicates that IMGs were less likely to choose market areas with higher values of the characteristic.7
Results
Descriptive Data
A total of 19,940 new IMG physicians met the criteria for inclusion in the study. These physicians represent 18.5 percent of the 107,867 physicians who completed GME between 1989 and 1994 and were in active medical practice in the United States 4.5 years later.
Table 1 reports descriptive data for the new IMG physicians and for new physicians who were U.S. medical graduates. The number of new IMG physicians finishing GME and later entering practice in the United States rose from 2,681 in the 1989 GME cohort to 4,373 in the 1994 GME cohort, an increase of 63 percent. At the end of GME training, 47.2 percent of IMGs were older than age 35, compared with 17.2 percent of U.S. graduates. The IMGs were more likely than U.S. medical graduates to be generalists (45.4 percent versus 32.6 percent),8 and they were less likely than U.S. medical graduates to locate their practices in nonmetropolitan areas or in the states where they completed GME training.9 About 82 percent of IMGs were born outside the United States or Canada. In comparison with U.S. medical graduates, IMGs were more likely to locate in the Northeast census region and less likely to locate in each of the other three census regions.
Table 1.
Patient Care Physicians Who Completed GME between 1989 and 1994 and Were in Practice 4.5 Years Later
| International Medical Graduates | U.S. Medical Graduates | |||
|---|---|---|---|---|
| Total number | 19,940 | 100.0% | 87,927 | 100.0% |
| Year in which completed GME | ||||
| 1989 | 2,681 | 13.4% | 14,222 | 16.2% |
| 1990 | 2,930 | 14.7% | 15,127 | 17.2% |
| 1991 | 2,827 | 14.2% | 13,903 | 15.8% |
| 1992 | 3,283 | 16.5% | 14,073 | 16.0% |
| 1993 | 3,846 | 19.3% | 15,440 | 17.6% |
| 1994 | 4,373 | 21.9% | 15,162 | 17.2% |
| Age | ||||
| 30 or younger | 2,026 | 10.2% | 25,156 | 28.6% |
| 31–35 | 8,922 | 44.7% | 47,600 | 54.2% |
| 36–40 | 6,455 | 32.4% | 12,206 | 13.9% |
| 41 or older | 2,537 | 12.7% | 2,856 | 3.3% |
| Male | 14,633 | 73.4% | 60,486 | 68.8% |
| Specialty group | ||||
| Generalist | 9,060 | 45.4% | 28,672 | 32.6% |
| Medical specialist | 8,684 | 43.6% | 42,758 | 48.6% |
| Hospital-based specialist | 2,196 | 11.0% | 16,497 | 18.8% |
| Practice located in state of GME | 9,704 | 48.7% | 46,700 | 53.1% |
| Practice located in nonmetropolitan Area | 1,521 | 7.6% | 8,014 | 9.1% |
| Census region of practice location | ||||
| Northeast | 6,738 | 33.8% | 19,452 | 22.1% |
| North Central | 3,975 | 19.9% | 19,249 | 21.9% |
| South | 6,252 | 31.4% | 30,639 | 34.8% |
| West | 2,975 | 14.9% | 18,577 | 21.1% |
| Country of birth | ||||
| U.S. or Canada | 3,665 | 18.4% | 78,776 | 89.6% |
| Africa/West Indies | 1,400 | 7.0% | 671 | 0.8% |
| Asia | 7,457 | 37.4% | 3,438 | 3.9% |
| Latin America | 2,253 | 11.3% | 2,116 | 2.4% |
| Other† | 5,165 | 25.9% | 2,926 | 3.3% |
Includes Europe, Russia, Israel, the Arab Nations, and South Africa.
Regression Results
Table 2 presents the estimated regression coefficients of the conditional logit models for each of the six analytic subgroups. The first three columns present the results for foreign-born IMGs; the latter three columns present results for U.S.-born IMGs.
Table 2.
Conditional Logit Models of the Choice of First Practice Location for IMGs
| FOREIGN BORN IMGs | U.S. BORN IMGs | |||||
|---|---|---|---|---|---|---|
| Generalists (N=7,490) | Med/surg specialists (N=7,066) | Hosp specialists (N=1,719) | Generalists (N=1,570) | Med/surg specialists (N=1,618) | Hosp specialists (N=477) | |
| Key explanatory variables | ||||||
| Market area in same state as GME | 3.058* | 3.060* | 3.240* | 3.421* | 3.066* | 2.922* |
| Years of GME required for state licensure | −0.213* | −0.157* | −0.225* | −0.022 | −0.041 | −0.096 |
| Proportion of 1985 physicians who were IMGs | 1.905* | 1.914* | 2.474* | 0.814* | 0.829* | 0.934 |
| Proportion of population with non-English first language | 0.099 | 1.084* | −0.480 | 1.420 | 1.200 | 1.260 |
| Proportion of population black | 0.004 | −0.461 | −0.221 | −1.697* | 0.403 | 0.498 |
| Proportion of population Asian | −3.877* | −2.368* | −3.106 | −9.376* | −5.997* | −5.067 |
| Proportion of population Hispanic | −1.653* | −2.258* | 0.220 | −0.493 | 0.925 | 1.102 |
| Proportion of population black* Black IMG† | 0.433 | 0.438 | 1.178 | |||
| Proportion of population Asian* Asian IMG† | 3.097* | 0.618 | 1.100 | |||
| Proportion of population Hispanic* Hispanic IMG† | 3.273* | 3.298* | 1.701* | |||
| Covariates | ||||||
| Logarithm of population size | 1.053* | 1.080* | 1.389* | 0.987* | 1.013* | 0.952* |
| Proportion of population age 5 or younger | 14.793* | 4.628 | −20.710* | 16.049 | 4.809 | 27.250 |
| Proportion of population between ages 6 and 19 | −12.828* | −4.795* | −4.489 | −7.282 | −10.170* | −27.652* |
| Proportion of population age 65 or older | −5.100* | −4.323* | −7.844* | 3.988 | 0.879 | −8.978* |
| Proportion of population female | −1.088 | 12.116* | 7.924 | −3.643 | 3.514 | 26.584* |
| Proportion of adult population with high school degree | −1.815* | −1.673* | −0.598 | −1.155 | −0.509 | 6.466* |
| Proportion of adult population with college degree | 1.171 | 2.955* | 2.192 | −0.022 | −0.884 | −5.713* |
| Proportion of population below poverty level | 4.624* | 1.886* | 3.403* | 3.113 | −0.355 | 1.511 |
| Per capita income ($1000s) | 0.034* | −0.009 | 0.008 | 0.059* | 0.048* | 0.075* |
| HMO penetration | −0.551* | −0.844* | −0.158 | 0.057 | −1.500* | −1.617* |
| Generalists per thousand population | 0.090 | −0.515* | −1.459* | 0.478 | −0.858 | −1.131 |
| Medical/surgical specialists per thousand population | −0.417* | 0.234 | 0.269 | −0.179 | 0.879* | −0.604 |
| Hospital-based specialists per thousand population | 2.055* | 1.946* | 3.464* | 1.087 | 0.417 | 3.101* |
| Physician practice cost index | 0.003 | 0.000 | −0.006 | 0.000 | 0.002 | 0.010 |
| Number of hospitals with residency programs | −0.012* | −0.011* | −0.024* | −0.008 | −0.019* | −0.008 |
| Nonmetropolitan area | −0.200* | −0.480* | −0.892* | −0.182 | −0.416* | 0.641 |
| Mean January temperature | 0.019* | 0.016* | 0.004 | 1.428 | 1.200 | 1.265 |
For foreign-born IMGs only.
p <0.05.
Both foreign-born and U.S.-born IMGs were much more likely to choose practices in market areas located in the state where they had completed GME than in market areas located in other states. This finding is consistent with the notion that prior contact with a community reduces search costs and thus increases the probability of locating nearby. The IMGs also may develop other types of ties to the communities where they obtain their GME, by participating in professional and community organizations and developing personal relationships.
Foreign-born IMGs were significantly less likely to locate in states that required more years of GME before granting a license than in states requiring fewer years. By contrast, state licensure requirements did not affect the practice location decisions of U.S.-born IMGs.
Both new foreign-born and new U.S.-born IMGs were attracted to market areas in which a large proportion of established physicians were IMGs. However, the strength of this attraction was much greater for foreign-born IMGs. Further, the practice location choices of U.S.-born IMGs who were hospital-based specialists were unaffected by the proportion of established physicians who are IMGs. One interpretation of these findings is that networks of established IMGs help both foreign-born and U.S.-born IMGs who are starting their practices, but the benefit of these networks is greater for foreign-born IMGs.10 Foreign-born IMGs may have a more difficult time than U.S.-born IMGs obtaining positions in medical groups that are dominated by U.S. medical graduates or becoming incorporated into referral networks composed mainly of U.S. medical graduates.11
Finally, the ethnic composition of the market area population had complex relationships with the practice location decisions of new IMGs. Foreign-born IMGs who were not from Asian countries were less likely to locate in market areas with high proportions of Asians than in market areas with low proportions of Asians. Similarly, foreign-born IMGs who were not from Hispanic countries were less likely to locate in markets with high proportions of Hispanics than in markets with low proportions of Hispanics. However, foreign-born IMGs from Asian and Hispanic countries were attracted to market areas where the ethnic composition of the population matched their own ethnicity. The degree of ethnic matching was especially striking for foreign-born IMGs from Hispanic countries, who were significantly more likely to locate in market areas with high proportions of Hispanics than in market areas with low proportions of Hispanics. The proportion of the market area population who were black did not have a significant effect on the location choices of foreign-born IMGs, regardless of their ethnicity.
These findings indicate that ethnic matching plays an especially important role in the practice location choices of foreign-born IMGs, especially those born in Hispanic countries. This is consistent with the idea that foreign-born IMGs face lower cultural and language barriers, and enjoy higher demand for their services, in markets with high proportions of people whose ethnic background is similar to their own.12
International medical graduates born in the United States who were generalists were less likely to locate in market areas with large black populations and especially with large Asian populations. Similarly, U.S.-born IMGs who were medical/surgical specialists were much less likely to locate in market areas with large Asian populations. The location choices of U.S.-born IMGs were unaffected by the proportion of the market area population who were Hispanic. Because data on ethnicity or race were unavailable for U.S.-born IMGs, we were unable to examine the influence of ethnic matching on their practice location choices.
Other findings of the conditional logit regression analyses included a strong positive influence of population size on practice location for all the analytic subgroups in the study. The proportion of the population 6 to 19 years old, the proportion of the population older than 65, and HMO penetration had significant negative effects on practice location for most of the analytic subgroups, whereas per capita income had a significant positive effect. The poverty rate had a significant positive effect on practice location for foreign-born IMGs. The physician-to-population ratio for hospital-based specialists had a significant positive effect on practice location for most of the analytic subgroups, while the number of residency training programs had a significant negative effect. Lastly, IMGs were significantly less likely to locate in nonmetropolitan markets than in metropolitan markets, other things equal.
Relative Risks
To better understand the magnitudes of the effects expressed by the conditional logit regression coefficients, we estimated relative risks for the key explanatory variables (Table 3). To interpret the relative risks consider two market areas that are identical in every respect except that one of the market areas has a particular characteristic and the other market area lacks the characteristic. The relative risk represents the likelihood a physician chooses the market area with the particular characteristic in preference to the market area without the characteristic. For example, foreign-born IMGs who were generalists were 21.28 times more likely to choose a market area located in the state where they had completed GME than they were to choose an otherwise identical market area located in a different state. The relative risks are consistent with our earlier discussion of the regression results.
Table 3.
Relative Risks of Choosing a Market Area with a Particular Characteristic in Preference to a Market Area without the Characteristic
| FOREIGN BORN IMGs | U.S. BORN IMGs | |||||
|---|---|---|---|---|---|---|
| Generalists (N=7,490) | Med/surg specialists (N=7,066) | Hosp specialists (N=1,719) | Generalists (N=1,570) | Med/surg specialists (N=1,618) | Hosp specialists (N=477) | |
| Characteristic | ||||||
| Market area is in same state as GME | 21.28* | 21.33* | 25.53* | 30.60* | 21.46* | 18.58* |
| One more year of GME is required for state licensure | 0.81* | 0.85* | 0.80* | 0.98 | 0.96 | 0.91 |
| Proportion of 1985 physicians who were IMGs is 10% higher | 1.21* | 1.21* | 1.28* | 1.08* | 1.09* | 1.10 |
| Proportion of population with non-English first language is 10% higher | 1.01 | 1.11* | 0.95 | 1.15 | 1.13 | 1.13 |
| Proportion of population black is 10% higher | 1.00 | 0.95 | 0.98 | 0.84* | 1.04 | 1.05 |
| Proportion of population Asian is 10% higher | 0.68* | 0.79* | 0.73 | 0.39* | 0.55* | 0.60 |
| Proportion of population Hispanic is 10%higher | 0.85* | 0.80* | 1.02 | 0.95 | 1.10 | 1.12 |
| Proportion of population black is 10%higher* Black IMG† | 1.04 | 1.04 | 1.13 | |||
| Proportion of population Asian is 10%higher* Asian IMG† | 1.36* | 1.06 | 1.12 | |||
| Proportion of population Hispanic is 10%higher* Hispanic IMG† | 1.39* | 1.39* | 1.19* | |||
For foreign-born IMGs only.
p <0.05.
Sensitivity Analysis
We were concerned that some IMGs may choose their GME site based on where they hope to establish their practices. This may be especially likely to occur for U.S.-born IMGs, who are much more likely than foreign-born IMGs to be familiar with a variety of communities in the United States. To the degree this occurs, the indicator variable for whether the market area was in the state of GME would be endogenous. As a result, the statistical association between practice location and this variable would be biased upward by reverse causation and the coefficients on the other variables could be biased as well. To assess the potential impact of endogeneity on the coefficients of the other variables, we reestimated the conditional logit regression models after excluding from the model the indicator variable for whether the market area was in the state of GME (Table 4). Although most of the coefficients were insensitive to removing state of GME from the specification, the estimated effect of licensure requirements changed. The negative impact of more stringent licensure requirements on the practice location decisions of foreign-born IMGs was reduced in magnitude, and more stringent licensure requirements actually exhibited a significant positive association with the location decisions of U.S.-born IMGs. This analysis reveals that the number of years of GME required for state licensure are positively correlated with the availability of GME positions for IMGs. More stringent licensure requirements may have evolved as a policy response in states where large numbers of IMGs receive GME.
Table 4.
Conditional Logit Models of the Choice of First Practice Location for IMGs (Sensitivity Analysis)
| FOREIGN BORN IMGs | U.S. BORN IMGs | |||||
|---|---|---|---|---|---|---|
| Generalists (N=7,490) | Med/surg specialists (N=7,066) | Hosp specialists (N=1,719) | Generalists (N=1,570) | Med/surg specialists (N=1,618) | Hosp specialists (N=477) | |
| Key explanatory variables | ||||||
| Years of GME required for state licensure | −0.079* | −0.007 | −0.090* | 0.171* | 0.170* | 0.132 |
| Proportion of 1985 physicians who were IMGs | 3.576 | 3.256* | 4.013* | 2.008* | 2.200* | 2.839* |
| Proportion of population with non-English first language | −0.748 | 0.362 | −0.856 | −0.304 | −0.245 | 0.117 |
| Proportion of population black | −0.590* | −1.219* | −1.911* | −1.671* | −0.845 | −1.260 |
| Proportion of population Asian | −2.212* | −0.934 | −2.961 | −6.873* | −4.308* | −2.555 |
| Proportion of population Hispanic | −1.779* | −2.468* | −0.233 | 0.242 | 0.819 | 0.457 |
| Proportion of population black* Black IMG† | 0.318* | 0.197 | 1.197 | |||
| Proportion of population Asian* Asian IMG† | 4.228* | 2.274* | 2.770 | |||
| Proportion of population Hispanic* Hispanic IMG† | 3.544* | 3.432* | 1.715* | |||
| Covariates | ||||||
| Logarithm of population size | 0.983 | 1.026* | 1.323* | 0.922* | 0.935* | 0.863* |
| Proportion of population age 5 or younger | 5.923* | −2.144 | −29.895* | 6.021 | −5.085 | 17.188 |
| Proportion of population between ages 6 and 19 | −5.440* | −0.382 | 2.526 | −1.002 | −5.201 | −19.503* |
| Proportion of population age 65 or older | −3.017 | −3.372* | −6.887* | 6.817* | 2.005 | −7.799 |
| Proportion of population female | −3.226* | 9.082* | 5.048 | −5.690 | −0.872 | 22.675 |
| Proportion of adult population with high school degree | −1.491 | −1.121* | −0.918 | −2.669* | −0.448 | 6.692* |
| Proportion of adult population with college degree | −0.260* | 1.350* | 1.489 | −1.303 | −3.098* | −8.273* |
| Proportion of population below poverty level | 2.013* | 1.147 | 1.746 | −1.873 | −2.549 | −0.352 |
| Per capita income ($1000s) | 0.031* | −0.007 | 0.022 | 0.063* | 0.047* | 0.075* |
| HMO penetration | 0.040 | −0.155 | 0.659 | 0.644 | −0.721 | −1.051 |
| Generalists per thousand population | 0.220 | −0.345 | −1.272* | 0.139 | −0.406 | −0.417 |
| Medical/surgical specialists per thousand population | 0.139* | 0.773* | 0.755* | 0.336 | 1.739* | 0.564 |
| Hospital-based specialists per thousand population | 0.882 | 0.598 | 2.105* | 0.394 | −2.018* | 0.139 |
| Physician practice cost index | 0.005* | 0.003 | −0.009* | 0.010* | 0.009* | 0.010 |
| Number of hospitals with residency programs | 0.009* | 0.005 | −0.001 | 0.008 | 0.002 | 0.018 |
| Nonmetropolitan area | −0.197 | −0.536* | −1.005* | −0.184 | −0.477* | 0.546 |
| Mean January temperature | −0.749 | 0.362 | −0.856 | 0.008 | 0.007 | 0.019* |
For foreign-born IMGs only.
p <0.05.
Discussion
This study examined the impact of various market area characteristics on the practice location choices of new IMGs who completed GME between 1989 and 1994. The study had four principal results. First, the location of GME was a strong predictor of new IMGs’ choices of practice location. Second, more years of GME required for state licensure had a negative effect on the practice location choices of new foreign-born IMGs. Third, there was strong persistence over time in the location choices of foreign-born IMGs, probably mediated by the effects of networks of established IMG physicians. Fourth, foreign-born IMGs were attracted to markets where the ethnic composition of the population matched their own ethnicity.
Our findings suggest that policymakers may influence the distribution across market areas of new IMGs by changing the availability of GME positions for IMGs. Numerous influential organizations have recently called for a reduction in the number of residency positions for IMGs at the national level (Institute of Medicine 1996; Pew Health Professions Commission 1995; Council on Graduate Medical Education 1998). However, some observers have criticized these proposals on the grounds that limiting the influx of IMGs into the United States could hurt populations in areas of medical underservice (Mick and Lee 1997), including rural areas. Mick et al. (2000) found that IMGs are more likely than U.S. medical graduates to practice in counties that are medically underserved, although they are simultaneously more likely than U.S. graduates to locate in states with large numbers of physicians. Further, Mick and Pfahler (1995) found that, on the whole, IMGs are no more likely than U.S. graduates to practice in rural areas. Therefore, an alternative to reducing GME positions for IMGs nationally would be to increase or reduce positions in particular states according to the level of medical underservice and medical need.
Additional concerns regarding a reduction in the number of residency positions for IMGs have been based on the notion that a decrease in IMGs would adversely affect access to generalist physicians. Our finding that IMGs were more likely than U.S. graduates to enter generalist fields supports this contention. On the other hand, the specialty choices of IMGs have varied substantially over time (Mick and Pfahler 1995) and the stability of their relative preferences for generalist fields is difficult to predict.
During the period of our study, when IMGs were required to pass the Federal Licensing Exam (FLEX) in order to become licensed, policymakers might also have influenced the geographical distribution of new IMGs through changes in state licensure requirements for IMGs. However, the FLEX has recently been replaced by the U.S. Medical Licensing Exam (USMLE), which has made state licensure requirements more uniform (American Medical Association 2000). The increased uniformity associated with the introduction of the USMLE has effectively eliminated licensure requirements as a state policy instrument.13
Of course, the prospect of using policy to affect the distribution of IMGs is tempered by the strong persistence over time in the location choices of IMGs. This persistence, which is likely to be mediated by the role of established IMGs in helping new IMGs to start successful practices, may make it difficult to start an influx of IMGs into new areas.
The finding that IMGs born in Hispanic and Asian countries were more likely to locate in markets with large Hispanic and Asian populations, respectively, suggests an opportunity to increase access to physician care for underserved minority populations. The role of Hispanic physicians in serving Hispanic populations has been documented by previous research (e.g., Komaromy et al. 1996), and is supported by a recent survey of Hispanic physicians in California, which found that 40 percent of Hispanic IMGs were located in heavily Hispanic zip codes, whereas only 27 percent of non-Hispanic IMGs practiced in these zip codes (Hayes-Bautista et al. 2000). Hayes-Bautista etal. (2000) also documented a drop in new physicians into Hispanic areas after a policy to reduce the number of IMGs in California was instituted. A national policy increasing the number of permanent visas awarded to physicians from countries of the same ethnicity as underserved U.S. populations could help to redistribute physicians into underserved areas, particularly underserved minority communities.
Our study was limited by lack of information on the citizenship of foreign-born IMG physicians. Many policy issues regarding IMGs are related to visa status, but the majority of foreign-born IMGs are either U.S. citizens or permanent residents (Mullan et al. 1995). Further, we had no informationon how long foreign-born IMGs had lived in the United States, or whether they had previous ties to particular communities other than through GME.
A second limitation was that we used the number of years of GME required for licensure as our only measure of the stringency of state licensure requirements. Other requirements were either correlated with the number of years of GME required or did not vary enough to use in the analyses.
Finally, we did not know the race or ethnicity of the new IMGs in the study. For foreign-born IMGs we used country of birth as a proxy for ethnicity, but we were unable to include race or ethnicity in the analyses for U.S.-born IMGs. Nonetheless, the findings on ethnic matching for foreign-born Asian and Hispanic physicians are compelling. It is possible that the findings for black physicians would have been as strong if specific information on physician race had been available for use in the analyses.
Despite these limitations, our study provides new insights into the practice location decisions of new IMGs. In particular, the effects of state licensure requirements, established IMGs, and ethnic communities on new IMGs’ practice location choices have not been previously documented. These findings further our understanding of the roles that IMGs play in the U.S. physician workforce, and address the potential for state policies to influence the geographical distribution of IMGs.
Acknowledgments
We are indebted to Laurence C. Baker, Ph.D., for allowing us to use his HMO penetration data. We also thank Tamara Smith and Kris Parker for their skilled secretarial assistance.
Notes
The Masterfile is the only database with information on all allopathic physicians in the United States. It is continuously updated with information collected from medical schools, hospitals, state licensing agencies, medical societies, specialty certification boards, and periodic surveys of physicians.
For example, the first practice location for physicians who completed GME in 1994 (typically in June) was based on the reported practice address in December 1998.
Rhode Island, Connecticut, and New Jersey do not have any nonmetropolitan counties.
During the period of our study, IMGs were required to pass the Federal Licensing Exam (FLEX). States differed in when IMGs were allowed to take the FLEX and in how the exam was administered (AMA 1992). For example, some states required candidates to take both parts of the FLEX at the same time, and some had limits on how many attempts could be made to pass the exam. States also differed in whether physicians who completed a “Fifth Pathway” program were qualified licensure candidates, whether personal interviews were required, and whether the state endorsed a Canadian certificate when held by an IMG. The number of years of GME required to become licensed in a state was correlated with several of these other licensure requirements and was used as a proxy for the general stringency of these requirements. Recently, the FLEX was replaced by the U.S. Medical Licensing Exam (USMLE).
Physicians were categorized as black if they were born in Africa (excluding Northern Africa and South Africa) or on an island in the West Indies with a predominant population of African descent. Physicians were categorized as Hispanic if they were born in Central or South America or on a Spanish-speaking Caribbean Island. Physicians were categorized as Asian if they were born in Asia, excluding Russia, Israel, and the Arab nations.
Generalists included physicians in general internal medicine, general pediatrics, family medicine, and general practice; medical/surgical specialists included physicians in internal medicine subspecialties, pediatric subspecialties, dermatology, neurology, general surgery, obstetrics/gynecology, surgical subspecialties, and psychiatry; and hospital-based specialists included physicians in emergency medicine, radiology, anesthesiology, and pathology.
The conditional logit model assumes that the ratio of the probabilities of choosing any two market areas is independent of the other areas included in the analysis, a property known as the independence of irrelevant alternatives (IIA) (McFadden 1973; Maddala 1983). Escarce et al. (1998) found that the IIA assumption did not lead to serious bias in the analysis of the location patterns of new physicians.
The specialty choices of IMGs have changed substantially over time. Consistent with our data, Mick and Pfahler (1995) found a notable surge in the proportion of IMGs entering generalist fields in the early 1990s.
Mick and Pfahler (1995) found that IMGs nationally do not practice disproportionately in rural areas, although analysis of smaller geographical units revealed variations in the pattern.
An alternative possibility is that the proportion of IMGs among established physicians captures unmeasured but enduring attributes of market areas that make them attractive to IMGs. Although we cannot rule out this possibility, the regression models included numerous relevant covariates to minimize the possibility of omitted variable bias.
Shortell (1974) found that patterns of referrals among physicians were influenced by physicians’“status” in the medical community, and that “high-status” physicians rarely referred patients to “low-status” physicians. Many physicians are likely to view IMGs as having lower status than U.S. medical graduates.
There is evidence that black and Hispanic patients perceive that black and Hispanic physicians, respectively, provide care of higher quality than do other physicians (Saha et al. 1999). Further, black and Hispanic patients seek care from physicians of their own race and ethnicity because of personal preference and language irrespective of geographic accessibility or socioeconomic factors (Gray and Stoddard 1997; Saha etal. 2000). These patterns of demand may partly explain the finding that black and Hispanic physicians care for more black and Hispanic patients, respectively, than do other physicians (e.g., Komaromy et al. 1996).
We are grateful to an anonymous reviewer for pointing this out.
This research was supported by a grant from the Robert Wood Johnson Foundation under its Health Care Financing and Organization initiative.
References
- American Medical Association. U.S. Medical Licensure Statistics and Current Licensure Requirements by State 1992. Chicago: AMA Press; 1992. [Google Scholar]
- American Medical Association. State Medical Licensure Requirements and Statistics 2000–2001. Chicago: AMA Press; 2000. [Google Scholar]
- Baer LD, Ricketts TC, Konrad TR, Mick SS. “Do International Medical Graduates Reduce Rural Physician Shortages?”. Medical Care. 1998;36(11):1534–44. doi: 10.1097/00005650-199811000-00003. [DOI] [PubMed] [Google Scholar]
- Baker LC. “The Effect of HMOs on Fee-for-Service Health Care Expenditures Evidence from Medicare”. Journal of Health Economics. 1997;16:453–81. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- Council on Graduate Medical Education. Eleventh Report: International Medical Graduates, the Physician Workforce, and GME Payment Reform. Rockville, MD: U.S. Department of Health and Human Services; 1998. [Google Scholar]
- Eiler MA, Loft JD. Foreign Medical Graduates. Chicago, IL: American Medical Association; 1986. [Google Scholar]
- Ernst RL, Yett DE. “Econometric and Statistical Studies of the Geographic Distribution of Physicians”. In: Ernst RL, Yett DE, editors. Physician Location and Specialty Choice. Ann Arbor MI: Health Administration Press; 1985. pp. 179–226. [Google Scholar]
- Escarce JJ, Polsky D, Wozniak GD, Pauly MV, Kletke PR. “Health Maintenance Organization Penetration and the Practice Location Choices of New Physicians: A Study of Large Metropolitan Areas in the U.S”. Medical Care. 1998;36(11):1555–66. doi: 10.1097/00005650-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Ginzberg E, Brann E, Hiestand D, Ostow M. “Physician Supply and Health Policy: The Clouded Outlook”. Milbank Quarterly. 1981;59(4):508–41. [PubMed] [Google Scholar]
- Gray B, Stoddard JJ. “Patient–Physician Pairing: Does Racial and Ethnic Congruity Influence Selection of a Regular Physician?”. Journal of Community Health. 1997;22:247–59. doi: 10.1023/a:1025148302636. [DOI] [PubMed] [Google Scholar]
- Hayes-Bautista DE, Hsu P, Hayes-Bautista M, Stein RM, Dowling P, Beltran R, Villagomez J. “Latino Physician Supply in California: Sources, Locations, and Projections”. Academic Medicine. 2000;75(7):727–36. doi: 10.1097/00001888-200007000-00018. [DOI] [PubMed] [Google Scholar]
- Haug JN, Martin BC. Foreign Medical Graduates in the United States, 1970. Chicago, IL: American Medical Association; 1971. [Google Scholar]
- Iglehart JK. “The Quandary over Graduates of Foreign Medical Schools in the United States”. New England Journal of Medicine. 1996;334(25):1679–83. doi: 10.1056/NEJM199606203342521. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. The Nation's Physician Workforce: Options for Balancing Supply and Requirements. Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]
- Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, Bindman AB. “The Role of Black and Hispanic Physicians in Providing Health Care for Underserved Populations”. New England Journal of Medicine. 1996;334(20):1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- Maddala GS. Limited-Dependent and Qualitative Variables in Econometrics. New York: Cambridge University Press; 1983. [Google Scholar]
- McFadden D. Zarembka P. Frontiers in Econometrics. New York: Academic Press; 1973. “Conditional Logit Analysis of Qualitative Choice Behavior”; pp. 105–42. [Google Scholar]
- Mick SS, Lee SD, Wodchis WP. “Variations in Geographical Distribution of Foreign and Domestically Trained Physicians in the United States: ‘Safety Nets’ or ‘Surplus Exacerbation’?”. Social Science Medicine. 2000;50:185–202. doi: 10.1016/s0277-9536(99)00183-5. [DOI] [PubMed] [Google Scholar]
- Mick SS, Lee SD. “The Safety Net Role of International Medical Graduates”. Health Affairs. 1997;16(4):141–50. doi: 10.1377/hlthaff.16.4.141. [DOI] [PubMed] [Google Scholar]
- Mick SS, Pfahler MN. Review and Synthesis of the Literature on Foreign Medical Graduates/International Medical Graduates. Ann Arbor, MI: University of Michigan School of Public Health; 1995. Report to the U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions [P.O. HRSA 94-961(P)] [Google Scholar]
- Mullan F, Politzer RM, Davis CH. “Medical Migration and the Physician Workforce”. Journal of the American Medical Association. 1995;273(19):1521–7. doi: 10.1001/jama.1995.03520430057039. [DOI] [PubMed] [Google Scholar]
- Newhouse JP, Williams AP, Bennett BW, Schwartz WB. “Does the Geographical Distribution of Physicians Reflect Market Failure?”. Bell Journal Economics. 1982;13:493–506. [Google Scholar]
- Pew Health Professions Commission. Critical Challenges: Revitalizing the Health Professions for the Twenty-first Century. San Francisco: University of California at San Francisco, Center for Health Professions; 1995. [Google Scholar]
- Politzer RM, Cultice JM, Meltzer AJ. “The Geographic Distribution of Physicians in the United States and the Contribution of International Medical Graduates”. Medical Care Research and Review. 1998;55(1):116–30. doi: 10.1177/107755879805500107. [DOI] [PubMed] [Google Scholar]
- Saha S, Taggart SH, Komaromy M, Bindman AB. “Do Patients Choose Physicians of Their Own Race?”. Health Affairs. 2000;19(4):76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. “Patient–Physician Racial Concordance and the Perceived Quality and Use of Health Care”. Archives of Internal Medicine. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Seifer SD, Vranizan K, Grumbach K. “Graduate Medical Education and Physician Practice Location: Implications for Physician Workforce Policy”. Journal of the American Medical Association. 1995;274(9):685–91. [PubMed] [Google Scholar]
- Shortell SM. “Determinants of physician referral rates: an exchange theory approach”. Medical Care. 1974;12(1):13–31. doi: 10.1097/00005650-197401000-00002. [DOI] [PubMed] [Google Scholar]
- Willke RJ. “Practice Mobility among Young Physicians”. Medical Care. 1991;29(10):977–88. doi: 10.1097/00005650-199110000-00004. [DOI] [PubMed] [Google Scholar]
- Zuckerman S, Welch WP, Pope G. “A Geographic Index of Physician Practice Costs”. Journal of Health Economics. 1990;9:39–69. doi: 10.1016/0167-6296(90)90040-a. [DOI] [PubMed] [Google Scholar]


